Abstract
Tobacco smoking is an important risk factor for peripheral artery disease (PAD), but it remains unknown whether smokeless tobacco, such as Swedish snuff (snus), is also associated with this disease. We used data from the Cohort of Swedish Men including 24,085 men. Individuals were grouped into never, past, and current snus dippers as well as never, past quitting ≥ 10 years, past, quitting < 10 years, and current smokers. Incident PAD cases were defined by linkage of the cohort with the Swedish National Patient Register. Cox proportional hazards regression was used to analyze the data. Over a mean follow-up period of 9.1 years (from July 1, 2009 to December 31, 2019), 655 incident PAD cases were ascertained. Cigarette smoking but not Swedish snus dipping was associated with an increased risk of PAD. Compared with never snus dippers, the hazard ratio of PAD was 0.95 (95% confidence interval [CI] 0.73–1.24) for past snus dippers and 0.88 (95% CI 0.66–1.17) for current snus dippers. Compared to never smokers, the hazard ratio of PAD was 1.38 (95% CI 1.14–1.68) for past smoker who stopped smoking for ≥ 10 years, 2.61 (95% CI 1.89–3.61) for past smoker who stopped smoking for < 10 years, and 4.01 (95% CI 3.17, 5.08) for current smoker. In conclusion, cigarette smoking but not Swedish snus dipping increases the risk of PAD.
Similar content being viewed by others
Introduction
Peripheral artery disease (PAD) is a common atherosclerotic cardiovascular disease with a global prevalence of 5.6%1. It was estimated that PAD affected around 237 million individuals aged above 25 years worldwide in 20151. Traditional cardiovascular risk factors, like smoking, diabetes, dyslipidemia, and hypertension, and several metabolic and inflammatory factors have been associated with PAD risk in populations in Western countries2. Among these factors, tobacco smoking is an important modifiable risk factor for PAD3, and the causality of the association has been strengthened in recent Mendelian randomization studies4,5. Nicotine is one of the detrimental chemicals in tobacco and has the potential of impairing cardiovascular system via unfavorable impacts on heart rate, blood lipids, blood pressure, blood viscosity, and vasoconstriction as well as on endothelial function6,7,8.
Oral snuff is a smokeless tobacco product containing nicotine but limited other detrimental components from cigarette smoking. Studies have suggested that snuff dippers are exposed to similar or higher doses of nicotine than smokers9. Snuff in different countries and areas may be largely varying in addiction potential and patterns of usage10 and have different impacts on cardiovascular disease11. In Sweden, approximately 11–13% of the population used Swedish snuff (snus) and 7–12% of the population smoked daily in a recent decade12. Previous studies on snus revealed that snus dipping was not associated with risk of overall heart disease13, stroke14, acute myocardial infarction15 or ischemic heart disease16 but associated with an increased risk of cardiovascular mortality17. However, limited data are available on the effect of Swedish snus dipping on PAD risk. Here, we aimed to explore the association between snus dipping and incident PAD using data from a cohort of middle-aged and older men. We also examined the association for tobacco smoking as a positive control.
Materials and methods
Study population
We included individuals from the Cohort of Swedish Men (COSM) that was initiated in the late autumn of 1997 by inviting 100,303 Swedish men aged 45 to 79 living in Västmanland or Örebro county18. Around 49% of invited individuals (48,850) responded the questionnaire in 1997. The second surveys were conducted in 2008 and 2009 when 37,861 and 29,068 COSM members who were still alive and residing in the study areas received questionnaires about health status (2008) and modifiable risk factors (2009), respectively. Around 78% (29,531) and 90% (26,161) of men completed the 2008 and 2009 questionnaires, respectively. A total of 29,597 men participated in at least one survey in 2008 and 2009. After removal of individuals who died before July 1, 2009, those with a prior diagnosis of PAD, and those with missing information on snus dipping (in the analysis of snus dipping), 24,085 men were included in the analysis. The flow chart of the final study population is presented in Fig. 1. Data used in this study were permitted under Project simpl2020002. The study has been approved by the Swedish Ethical Review Authority (Dnr: 2019-03986). All participants have provided informed consent. The research was performed in accordance with the Declaration of Helsinki.
Assessment of snus dipping and tobacco smoking
Snus dipping and tobacco smoking were measured by a self-administrated questionnaire in 2009. Participants were asked to answer the question “mark if you have used snus regularly (more than 5 servings per week)” by choosing one of three predefined categories, including “No, I have never used snus regularly”, “Yes, I use snus” and “Yes, but I stopped using snus”19. Three statuses (never, past, and current snus dippers) were defined based on this question. Likewise, tobacco smoking was defined using corresponding information on “mark if you have smoked cigarettes regularly (more than 5 cigarettes per week)”. Four categories (never, past with quitting time ≥ 10 years, past with quitting time < 10 years and current smoker) were defined when taking time of stopping smoking into consideration. Individuals without smoking information (n = 1172) were grouped into one category named “missing” in the analysis. Never snus dipper and never smoker were defined as the reference groups in the analysis of snus dipping and tobacco smoking, respectively, in relation to PAD risk.
Ascertainment of cases and follow-up
Incident PAD cases were ascertained by the clinical diagnosis based on codes from the 9th (440.0, 440.2, 440.3, 440.4, 440.9, 443.9) and 10th (I70.0, I70.2, I70.3, I70.4, I70.5, I70.6, I70.7, I70.9, I703.9) International Classification of Disease revision with information identified by linkage of the cohorts to the Swedish Patient Register. The register has an nearly complete coverage of hospital-based inpatient and outpatient care20. Individuals were followed up from July 1, 2009 until the date of diagnosis of PAD, date of death, or end of follow-up (i.e., 31 December 2019), whichever came first. Death information was obtained from the Swedish Death Registry.
Assessment of covariables
Information on age, body mass index, highest education attainment, history of hypertension, hypercholesterolemia, and diabetes mellitus, physical activity (walking/cycling and exercise combined), diet quality (measured by modified Dietary Approaches to Stop Hypertension) and coffee consumption was reported in the 2008 and 2009 questionnaires. The modified Dietary Approaches to Stop Hypertension diet included fruits, vegetables, nuts and legumes, whole grains, and low‐fat dairy products as healthy components and red and processed meat and sweetened beverages as unhealthy components21. Individuals were assigned a score from 1 to 5 according to the quintiles of consumption of each food and the scores were summed to create a diet score (7–35). A high score indicates a high adherence to the modified Dietary Approaches to Stop Hypertension diet pattern.
Statistical analysis
The Kaplan–Meier method and log-rank test were used to compare the probability of being free of PAD diagnosis across snus dippers and cigarette smokers. Cox proportional hazard regression was used to estimate the associations of snus dipping and tobacco smoking with risk of incident PAD with age as the underlying time scale. The assumption of proportionality was verified using Schoenfeld residuals. We obtained estimates from an age-adjusted model and a multivariable-adjusted model with adjustment for age, body mass index (underweight, normal, overweight and obesity), education levels (≤ 9, 10–12, > 12 years), history of hypertension, hypercholesterolemia, and diabetes mellitus (yes or no), tobacco smoking in the analysis of snus dipping, snus dipping in the analysis of tobacco smoking, physical activity (0–10, 11–30 and 31–60 and > 60 min per day), and diet score (continuous). The proportion of missing data was 3.32% for body mass index, 0.24% for education level, 16.9% for smoking status, and 11.9% for physical activity. A separate group was created for each variable with missing values. All statistical tests were two-sided, and the analyses were performed in Stata/SE (version 15.0; StataCorp, Texas, USA). An association with a p value below 0.05 was deemed as statistically significant.
Results
The mean age of the population at baseline was 70.2 ± 8.3 years. A total of 655 incident PAD cases were ascertained during a mean follow-up period of 9.1 years and 220,127 person-years (from July 1, 2009 to December 31, 2019). The age of PAD onset was 78.2 ± 8.0 years, and the incidence rate was 3.0 per 1000 person-years. The age-standardized baseline characteristics by snus dipping are displayed in Table 1. Snus dippers were more likely to be younger men with low education level, low physical activity, and with a history of hypertension, hypercholesterolemia, diabetes, and past or current cigarette smokers.
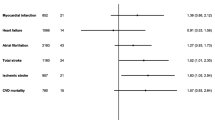
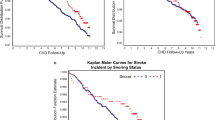
The Kaplan–Meier survival curve showed that past snus dippers had higher probability of being free of PAD diagnosis compared to never snus dippers (Fig. 2, p for log-rank test = 0.02). However, snus dipping was not associated with the risk of PAD in either the age-adjusted or the multivariable-adjusted model (Table 2). Compared with never snus dippers, the multivariable-adjusted hazard ratio of PAD was 0.95 (95% confidence interval (CI) 0.73, 1.24) for past snus dippers and 0.88 ((95% CI 0.66, 1.17) for current snus dippers.
In Kaplan–Meier analysis, never smokers had higher probability of being free of PAD diagnosis compared to past or current smokers (Fig. 2, p for log-rank test < 0.001). Tobacco smoking also showed a robust and strong association with incident PAD in Cox regression (Table 2). Hazard ratios of PAD were 1.38 (95% CI 1.14, 1.68), 2.61 (95% CI 1.89, 3.61) and 4.01 (95% CI 3.17, 5.08) for past smoker who stopped smoking for ≥ 10 years, past smoker who stopped smoking for < 10 years, and current smoker, compared to never smoker. The direction and magnitude of associations remained stable in the analysis excluding individuals without smoking information (data not shown).
Discussion
The present study found that cigarette smoking, but not Swedish snus dipping was associated with an increased risk of PAD in a cohort of middle-aged and older Swedish men. This is the first study examining the association between snus dipping and incident PAD.
Previous studies on snuff dipping in relation to other cardiovascular diseases showed no association with risk of atrial fibrillation or heart failure22,23, but reported conflicting results for myocardial infarction and stroke11,13,14,15,16,24,25. A recent cohort study found that Swedish snus dipping was not associated with risk of major heart and valvular diseases, abdominal aortic aneurysm, or cardiovascular mortality, but possibly with an increased risk of stroke19. The discrepancy in these studies may be caused by residual confounding (e.g., weight gain after starting dipping snus since snus is often used to quit smoking), varying ways of treating smoking status (adjusting for it as confounders or restricting analysis to never smokers), different baseline age, inadequate statistical power, and diverse effects of snus (nicotine) on different cardiovascular diseases. Given that obesity is not an important risk factor for PAD2 and that many important cofounders were adjusted for in our analyses, our findings is less likely to be biased by confounding from weight change and other lifestyle factors. Nevertheless, the association may be challenged by inadequate power caused by a small number of cases despite of a long follow-up of this study. However, we observed that the hazard ratios of PAD for past and current snus dippers were below one.
Tobacco smoking has been identified as an important modifiable risk factor for PAD and the magnitude of the association was larger than that for coronary artery disease2,3,4,5,26. Even though nicotine has been proposed to affect the cardiovascular systems in an unfavorable manner6,7,8, our study did not support a detrimental role of snus (rich in nicotine) dipping in PAD. Considering a comparably reduced risk of PAD in past smoker versus current smoker, the nicotine replacement therapy to help cessation appears to be a practical strategy for PAD prevention after the assessment of potential side-effects. As for the different associations of snus dipping and cigarette smoking with PAD risk, the difference in components of snus and tobacco may convey the clues that certain chemical components contained in tobacco or generated in cigarette smoking, such as arsenic27 and carbon monoxide28 but not nicotine elevate the risk of developing PAD.
There are several underlying mechanisms explaining the positive association between tobacco smoking and PAD risk. Smoking is associated with high risk of developing metabolic disorders, such as type 2 diabetes29, hypertension5, and obesity5, which are risk factors for PAD. In addition, smoking may increase PAD risk through systemic inflammation30,31, endothelial dysfunction32, and coagulation factors33. The null finding on the association between Swedish snuff dipping and PAD risk may be explained by limited peripheral arterial atherosclerosis effects of nicotine which is rich in snus products.
There are strengths and limitations of the present study. Strength includes a large sample size, a long follow-up period, and accurate diagnostic information from register. We used tobacco smoking as the positive control and a strong association between tobacco smoking and PAD risk validated the case definition. Snus dipping and tobacco smoking information was obtained from a self-reported questionnaire, which may lead to misclassification of the exposure. Over the follow-up period, individuals may change their tobacco and snus use, which may also introduce misclassification of the exposure. Even though we adjusted for important lifestyle factors in the analysis, we could not completely rule out the possibility that our results might be affected by residual confounding caused by unadjusted factors, like sleep features34 and mental factors35, although these factors have not been robustly associated with the development of PAD. This study included middle-aged and elderly men only. Thus, whether findings can be generalized to younger individuals and to women needs assessment. The power of the study was generally confined by a small number of PAD cases. In addition, we could not assess the association between Swedish snus dipping and PAD risk in never smokers also due to few cases (2 cases and 4 cases in past and current snus dippers in never smoker, respectively). However, any residual confounding from cigarette smoking cannot explain our null finding for snus dipping and PAD risk.
In conclusion, cigarette smoking but not Swedish snuff dipping likely increases the risk of PAD. Along with previous null findings on the associations of snus dipping with stroke and coronary heart diseases13,14,15,16,19, our findings indicate that Swedish snus dipping is unlikely to have an important impact on the development of vascular diseases.
Data availability
De-identified SIMPLER data are available for researchers upon application (http://www.simpler4health.se/). Data can be accessed by a reasonable request to the corresponding author.
References
Song, P. et al. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: An updated systematic review and analysis. Lancet Glob. Health 7, e1020–e1030. https://doi.org/10.1016/s2214-109x(19)30255-4 (2019).
Criqui, M. H. & Aboyans, V. Epidemiology of peripheral artery disease. Circ. Res. 116, 1509–1526. https://doi.org/10.1161/circresaha.116.303849 (2015).
Lu, L., Mackay, D. F. & Pell, J. P. Meta-analysis of the association between cigarette smoking and peripheral arterial disease. Heart 100, 414–423. https://doi.org/10.1136/heartjnl-2013-304082 (2014).
Larsson, S. C. et al. Genetic predisposition to smoking in relation to 14 cardiovascular diseases. Eur. Heart. J. 41, 3304–3310. https://doi.org/10.1093/eurheartj/ehaa193 (2020).
Levin, M. G. et al. Genetics of smoking and risk of atherosclerotic cardiovascular diseases: A Mendelian randomization study. JAMA Netw. Open 4, e2034461. https://doi.org/10.1001/jamanetworkopen.2020.34461 (2021).
Kilaru, S. et al. Nicotine: A review of its role in atherosclerosis. J. Am. Coll. Surg. 193, 538–546. https://doi.org/10.1016/s1072-7515(01)01059-6 (2001).
Rohani, M. & Agewall, S. Oral snuff impairs endothelial function in healthy snuff users. J. Intern. Med. 255, 379–383. https://doi.org/10.1046/j.1365-2796.2003.01279.x (2004).
Fant, R. V., Henningfield, J. E., Nelson, R. A. & Pickworth, W. B. Pharmacokinetics and pharmacodynamics of moist snuff in humans. Tob. Control 8, 387–392. https://doi.org/10.1136/tc.8.4.387 (1999).
Holm, H., Jarvis, M. J., Russell, M. A. & Feyerabend, C. Nicotine intake and dependence in Swedish snuff takers. Psychopharmacology 108, 507–511. https://doi.org/10.1007/bf02247429 (1992).
Seidenberg, A. B., Ayo-Yusuf, O. A. & Rees, V. W. Characteristics of “American Snus” and Swedish Snus Products for Sale in Massachusetts, USA. Nicotine Tob. Res. 20, 262–266. https://doi.org/10.1093/ntr/ntw334 (2018).
Vidyasagaran, A. L., Siddiqi, K. & Kanaan, M. Use of smokeless tobacco and risk of cardiovascular disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 23, 1970–1981. https://doi.org/10.1177/2047487316654026 (2016).
Folkhälsomyndigheten. Statistics & reporting. https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/ (2021).
Lee, P. N. Summary of the epidemiological evidence relating snus to health. Regul. Toxicol. Pharmacol. 59, 197–214. https://doi.org/10.1016/j.yrtph.2010.12.002 (2011).
Hansson, J. et al. Snus (Swedish smokeless tobacco) use and risk of stroke: Pooled analyses of incidence and survival. J. Intern. Med. 276, 87–95. https://doi.org/10.1111/joim.12219 (2014).
Hansson, J. et al. Use of snus and acute myocardial infarction: Pooled analysis of eight prospective observational studies. Eur. J. Epidemiol. 27, 771–779. https://doi.org/10.1007/s10654-012-9704-8 (2012).
Lee, P. N. Epidemiological evidence relating snus to health—an updated review based on recent publications. Harm. Reduct. J. 10, 36. https://doi.org/10.1186/1477-7517-10-36 (2013).
Byhamre, M. L. et al. Swedish snus use is associated with mortality: A pooled analysis of eight prospective studies. Int. J. Epidemiol. 49, 2041–2050. https://doi.org/10.1093/ije/dyaa197 (2021).
Harris, H. et al. The Swedish mammography cohort and the cohort of Swedish men: Study design and characteristics of two population-based longitudinal cohorts. OA Epidemiol. 2, 1 (2013).
Titova, O. E., Baron, J. A., Michaëlsson, K. & Larsson, S. C. Swedish snuff (snus) and risk of cardiovascular disease and mortality: Prospective cohort study of middle-aged and older individuals. BMC Med. 19, 111. https://doi.org/10.1186/s12916-021-01979-6 (2021).
Ludvigsson, J. F. et al. External review and validation of the Swedish national inpatient register. BMC Public Health 11, 450. https://doi.org/10.1186/1471-2458-11-450 (2011).
Yuan, S., Bruzelius, M., Håkansson, N., Åkesson, A. & Larsson, S. C. Lifestyle factors and venous thromboembolism in two cohort studies. Thromb. Res. https://doi.org/10.1016/j.thromres.2021.03.024 (2021).
Arefalk, G. et al. Smokeless tobacco (snus) and risk of heart failure: Results from two Swedish cohorts. Eur. J. Prev. Cardiol. 19, 1120–1127. https://doi.org/10.1177/1741826711420003 (2012).
Hergens, M. P. et al. Use of Scandinavian moist smokeless tobacco (snus) and the risk of atrial fibrillation. Epidemiology 25, 872–876. https://doi.org/10.1097/ede.0000000000000169 (2014).
Hergens, M. P. et al. Long-term use of Swedish moist snuff and the risk of myocardial infarction amongst men. J. Intern. Med. 262, 351–359. https://doi.org/10.1111/j.1365-2796.2007.01816.x (2007).
Janzon, E. & Hedblad, B. Swedish snuff and incidence of cardiovascular disease. A population-based cohort study. BMC Cardiovasc. Disord. 9, 21. https://doi.org/10.1186/1471-2261-9-21 (2009).
Yuan, S., Damrauer, S. M., Håkansson, N., Åkesson, A. & Larsson, S. C. A prospective evaluation of modifiable lifestyle factors in relation to peripheral artery disease risk. Eur. J. Vasc. Endovasc. Surg. https://doi.org/10.1016/j.ejvs.2022.04.004 (2022).
Wang, C. H. et al. A review of the epidemiologic literature on the role of environmental arsenic exposure and cardiovascular diseases. Toxicol. Appl. Pharmacol. 222, 315–326. https://doi.org/10.1016/j.taap.2006.12.022 (2007).
Chen, Y. G. et al. Risk of peripheral artery disease in patients with carbon monoxide poisoning: A population-based retrospective cohort study. Medicine (Baltimore) 94, e1608. https://doi.org/10.1097/md.0000000000001608 (2015).
Yuan, S. & Larsson, S. C. A causal relationship between cigarette smoking and type 2 diabetes mellitus: A Mendelian randomization study. Sci. Rep. 9, 19342. https://doi.org/10.1038/s41598-019-56014-9 (2019).
Goncalves, R. B. et al. Impact of smoking on inflammation: Overview of molecular mechanisms. Inflamm. Res. 60, 409–424. https://doi.org/10.1007/s00011-011-0308-7 (2011).
Yuan, S. et al. Anti-inflammatory diet and incident peripheral artery disease: Two prospective cohort studies. Clin. Nutr. 41, 1191–1196. https://doi.org/10.1016/j.clnu.2022.04.002 (2022).
Münzel, T. et al. Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur. Heart J. 41, 4057–4070. https://doi.org/10.1093/eurheartj/ehaa460 (2020).
Lee, K. W. & Lip, G. Y. Effects of lifestyle on hemostasis, fibrinolysis, and platelet reactivity: A systematic review. Arch. Intern Med. 163, 2368–2392. https://doi.org/10.1001/archinte.163.19.2368 (2003).
Nagayoshi, M. et al. Association of sleep apnea and sleep duration with peripheral artery disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 251, 467–475. https://doi.org/10.1016/j.atherosclerosis.2016.06.040 (2016).
Heikkilä, K. et al. Job strain as a risk factor for peripheral artery disease: A multi-cohort study. J. Am. Heart Assoc. 9, e013538. https://doi.org/10.1161/jaha.119.013538 (2020).
Acknowledgements
We want to acknowledge the participants and investigators of SIMPLER for provisioning of facilities and experimental support. SIMPLER receives funding through the Swedish Research Council under Grant number 2017-00644. The computations were performed on resources provided by SNIC through Uppsala Multidisciplinary Center for Advanced Computational Science (UPPMAX) under Project simpl2020002. SIMPLER data can be applied via an application to https://www.simpler4health.se/.
Funding
Open access funding provided by Karolinska Institute. Funding for this study came from the Karolinska Institutet’s Research Foundation Grants (Grant number 2020-01842), the Swedish Research Council (Vetenskapsrådet; Grant Number 2019-00977), the Swedish Research Council for Health, Working Life and Welfare (Forte; 2018-00123) and the Swedish Heart-Lung Foundation (Hjärt-Lungfonden; Grant number 20210351). S.M.D. is supported by IK2-CX001780.
Author information
Authors and Affiliations
Contributions
S.Y. and S.C.L. conceived and designed the study. S.Y. undertook the statistical analyses and wrote the first draft of the manuscript. All authors provided important comments to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yuan, S., Titova, O.E., Damrauer, S.M. et al. Swedish snuff (snus) dipping, cigarette smoking, and risk of peripheral artery disease: a prospective cohort study. Sci Rep 12, 12139 (2022). https://doi.org/10.1038/s41598-022-16467-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16467-x
- Springer Nature Limited