Abstract
Dysregulation of ion flux across membranes and glutamate-induced excitotoxicity appear to be important pathophysiologic abnormalities in bipolar illness. Understanding ion control and responses to ionic stress is important to decipher the pathogenesis of this disorder. Monensin alone significantly increased [Na]i in ONPs from bipolar individuals (5.08 ± 0.71 vs baseline 3.13 ± 0.93, P = 0.03) and AP5 had no effect (2.0 ± 1.2 vs baseline 3.13 ± 0.93, P = 0.27). However, the combination of AP5 and monensin resulted in normalization of [Na]i (3.25 ± 1.28 vs baseline 3.13 ± 0.93, P = 0.89). This effect was not observed in cells from non-bipolar individuals (monensin alone, 1.72 ± 1.10 vs baseline 2.42 ± 1.80, P = 0.25; AP5 alone, 1.37 ± 0.74 vs baseline 2.42 ± 1.80; AP5 combined with monensin, 1.53 ± 0.98 vs baseline 2.42 ± 1.80, P = 0.31). Sodium regulation is central to neuronal function and may be disturbed in patients with bipolar disorder. Monensin is an ionophore, meaning that it incorporates itself into the membrane and allows sodium to enter independent of cellular membrane proteins. While the mechanism remains obscure, the observation that the NMDA receptor antagonist, AP5, normalizes [Na]i only in olfactory neuroepithelial precursors obtained from bipolar illness may provide novel insights into ion regulation in tissues from subjects with bipolar illness.
Similar content being viewed by others
Introduction
Bipolar disorder (BD) is a severe mental illness that afflicts about 1–3% of the population1,2, or about 3 to 5 million people in United States3. It has suboptimal outcomes regarding both disease and its treatment4,5. Better understanding of pathophysiologic processes would improve treatment development.
Neuroelectrical genes account for some 74% of all known susceptibility loci6. Furthermore, ion regulatory abnormalities are among the most reproducible findings in studies of BD7. Most important is the elevation of intracellular sodium ([Na]i) and dysfunction of ion transport systems7,8. Several ion regulatory systems have been shown to be uniquely disrupted in bipolar patients versus controls7,8,9,10. Furthermore, bipolar patients have been found to have excessive levels of the precursor glutamine in certain parts of their brain, as well as higher numbers of glutamate receptors9,10,11,12,13. These findings imply an abnormality of glutamate signaling in bipolar.
The aim of the present study was to further examine the role of the ionotropic N-methyl-D-aspartate (NMDA) glutamate receptor in the regulation of [Na]i. We utilized a sodium ionophore, monensin, to increase [Na]i to bypass other cellular proteins and focus on NMDA receptor function.
Methods
The olfactory neuroepithelial precursor (ONP) cells used have been previously described (BD n = 3; nonBD n = 6)14. Briefly, the BP subjects were a lithium-responsive 22 year-old male (on lithium for 5 years), a lithium-responsive 47 year-old male (on divalproex for 22 years), and a 56 year-old woman who had never received lithium (on divalproex for 34 years)14. Controls were age and gender matched. ONP cells are known to have functional NMDA receptors14,15,16. We used cells that were at passage number 15–20. ONPs were treated with the sodium ionophore monensin at 1 µM to model the elevation of [Na]i present in bipolar patients. The dose and duration of treatment was based on previous work that specifically modelled the doubling of intracellular sodium concentrations seen in manic bipolar patients7. Specifically, treatment with 0.1 M glutamate for 6 h16, or 1 µM of monensin for 2 h17 double the [Na]i in ONPs. The NMDA receptor antagonist AP5 (D-2-amino-5-phosphonopentanoate) was used to examine the role of NMDA receptor in normalizing this non-glutamate ionic stress, and was used as a pretreatment.
ONPs, which were initially obtained by olfactory epithelial biopsy after the subjects signed an informed consent; we followed all of the guidelines and regulations for human studies that is outlined in the Declaration of Helsinki and were overseen by our institutional review board (the University of Louisville Human Subjects Protection Program Office [HSPPO], protocol number 485.04). The cells were frozen in liquid nitrogen and for the experiments they were cultured in minimum essential media (MEM [content of media may be found at https://www.thermofisher.com/us/en/home/technical-resources/media-formulation.201.html; importantly, the sodium concentration is 0.84% which is similar to saline and has 2 mM L-glutamine but no glutamate]), gentamycin 0.1 mg/mL, and FBS 10%, in 5% CO2 as previously described14. They were treated with 1 µM monensin for 6.5 h, 0.1 mM AP5 for 6.5 h, or pretreated AP5 30 min followed by adding monensin to AP5 for an additional 6 h. This latter point was, in part, to ensure that depolarization with monensin does not activate the NMDA receptor. Each experiment was repeated 3–5 times. [Na]I, obtained in triplicate for each experiment, was measured with flame spectroscopy and expressed as concentration per protein as measured by Lowry methodology ([Na]i × 10–5 M/mg protein). Statistical analysis employed unpaired, 2-tailed t-tests. Since sodium concentration was the only outcome measure, and only 10 comparisons made, multiple-comparison corrections were not necessary.
Ethics approval and consents
The ONP cells were obtained by biopsy over two decades ago under a grant from the Brain and Behavior Research Foundation. At that time, all participants provided informed consent and the protocol was approved by the institution’s Human Subjects Protection Program.
Results
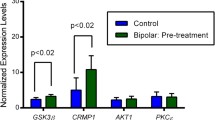
Monensin alone significantly increased [Na]i in ONPs from bipolar individuals (5.08 ± SD 0.71 vs baseline 3.13 ± 0.93 10−5 M/mg protein , P = 0.03) and AP5 alone had no effect (2.0 ± 1.2 vs baseline 3.13 ± 0.93, P = 0.27) (Fig. 1). The combination of AP5 and monensin normalized [Na]i (3.25 ± 1.28 vs baseline 3.13 ± 0.93, P = 0.89). This effect was not observed in cells from non-bipolar individuals (monensin alone, 1.72 ± 1.10 vs baseline 2.42 ± 1.80, P = 0.25; AP5 alone, 1.37 ± 0.74 vs baseline 2.42 ± 1.80; AP5 + monensin, 1.53 ± 0.98 vs baseline 2.42 ± 1.80, P = 0.31) (Fig. 1).
Intracellular sodium concentration with monensin treatment significantly increases only in ONPs from BD patients, but not non-bipolar controls, treated with monensin 1 µm for 6 h (*P < 0.05). BD ONPs pretreated by AP5 for 30 min followed by monensin for 6 h treatment were protected from the increase of intracellular sodium concentration.
Discussion
ONPs derived from BD individuals appear to be more susceptible to [Na]i elevations induced by monensin than nonBD controls. Despite the absence of glutamate in the experimental system, when the NMDA glutamate receptors are blocked, elevations of [Na]i are blocked. NonBD cells appear to be able to compensate for monensin-induced elevations of [Na]i in an NMDA receptor-independent manner. In this model, NMDA receptor appears necessary for bipolar-specific sodium ion dysregulation.
We utilized monensin, a sodium ionophore, to model the doubling of the intracellular sodium concentrations that have been documented in living humans with active mania18,19. Monensin can regulate the activity of NMDA receptor sodium channel20,21, and has been show to increase sodium pump activity22,23, regulate transport of sodium, potassium and calcium, and stimulate sodium-proton exchanger activity24. These changes appear to result from the elevation of intracellular sodium induced by monensin and have been demonstrated in a wide variety of cell types. The current study focused on the NMDA receptor, and we did not investigate other compensatory mechanisms in our ONP cells.
We did demonstrate a bipolar-specific abnormality in ion regulation, but have not determined the specific nature of the anomaly. We utilized an experimental dose that doubled the intracellular sodium concentration in cells obtained from bipolar patients. That same concentration did not increase sodium in control ONPs. We do not know if the lack of increase is related to a unique sensitivity to monensin in ONPs from bipolar individuals, or other unidentified compensatory mechanisms in ONPs from controls. However, at this concentration of monensin, an active NMDA receptor appears to play an important role in mediating the observed elevations of intracellular sodium in cells with the genetic heritage of bipolar illness (Fig. 1).
The use of a small number of diagnosis-specific cell lines is a limitation to this study, but is an acceptable practice given the labor-intensive nature of these investigations25. Replication of these findings in other cellular models would be important.
Sodium ion regulation appears to be altered in BD. Several systems have been implicated including the sodium pump26, cytoskeletal proteins27, and NMDA receptors28. The current study suggests that when the NMDA receptor is rendered dysfunctional with AP5, non-glutamate-mediated [Na]i elevation is prevented. In nonBD ONPs the dose of monensin used does not increase [Na]i even in the absence of NMDA dysfunction (Fig. 1). This suggests a central role of the NMDA receptor, and might explain why some NMDA antagonists, such as lamotrigine, memantine, and ketamine, are effective in the treatment of bipolar disorder.
We have previously demonstrated at 0.1 M glutamate treated for 6 h increased intracellular sodium ([Na]i) concentration twice that of untreated ONPs9. Similarly, ONPs derived from BD were more susceptible to glutamate-induced apoptosis17. The diagnosis-specific abnormalities related to ion regulation, along with the unique effectiveness of medications that alter ion function in bipolar disorder29 support ongoing investigation of these mechanisms.
Conclusions
Sodium regulation is central to neuronal function and may be disturbed in patients with bipolar disorder. Monensin is an ionophore, meaning that it incorporates itself into the membrane and allows sodium to enter independent of cellular membrane proteins. While the mechanism remains obscure, the observation that the NMDA receptor antagonist, AP5, normalizes [Na]i only in olfactory neuroepithelial precursors obtained from individuals with bipolar illness suggests that the NMDA receptor may play an important role in the ion dysregulation of excitable tissues of people with bipolar illness.
Data availability
All the data for this project are presented in this paper.
Abbreviations
- AP5:
-
D-2-amino-5-phosphonopentanoate
- BP:
-
Bipolar disorder
- MEM:
-
Minimum essential media
- NMDA:
-
N-methyl-D-aspartate
- [Na]i :
-
Intracellular sodium concentration
- ONP:
-
Olfactory neuroepithelial precursor
References
Grant, B. F. et al. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: Results from the national epidemiologic survey on alcohol and related conditions. J. Clin. Psychiatry. 66(10), 1205–1215 (2005).
Merikangas, K. R. et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 64(5), 543–552. https://doi.org/10.1001/archpsyc.64.5.543 (2007) ((Erratum in Arch Gen Psychiatry. 2007:64(9):1039.)).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry. 62(6), 593–602 (2005).
Cipriani, G., Danti, S., Carlesi, C., Cammisuli, D. M. & Di Fiorino, M. Bipolar disorder and cognitive dysfunction: A complex link. J. Nerv. Ment. Dis. 205(10), 743–756. https://doi.org/10.1097/NMD.0000000000000720 (2017).
Dome, P., Rihmer, Z. & Gonda, X. Suicide risk in bipolar disorder: A brief review. Medicina (Kaunas). 55(8), E403. https://doi.org/10.3390/medicina55080403 (2019).
Askland, K. D. Toward a biaxial model of “bipolar” affective disorders: Further exploration of genetic, molecular and cellular substrates. J. Affect. Disord. 94(1–3), 35–66 (2006).
El-Mallakh RS, Yff T, Gao Y. Ion dysregulation in the pathogenesis of bipolar illness. Ann Depress Anxiety. 2016;3(1):1076. https://austinpublishinggroup.com/depression-anxiety/fulltext/depression-v3-id1076.php
El-Mallakh, R. S., Gao, Y. & You, P. Role of endogenous ouabain in the etiology of bipolar disorder. Int. J. Bipolar Disord. 9(1), 6. https://doi.org/10.1186/s40345-020-00213-1 (2021).
Gao, Y., Lohano, K., Delamere, N. A., Lei, Z. & El-Mallakh, R. S. Ethanol normalizes glutamate-induced elevation of intracellular sodium in olfactory neuroepithelial progenitors from subjects with bipolar illness but not bipolar controls: Biologic evidence for the self-medication hypothesis. Bipolar Disord. 21(2), 179–181. https://doi.org/10.1111/bdi.12737 (2019).
Beneyto, M., Kristiansen, L. V., Oni-Orisan, A., McCullumsmith, R. E. & Meador-Woodruff, J. H. Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology 32(9), 1888–1902. https://doi.org/10.1038/sj.npp.1301312 (2007).
Öngür, D. et al. Abnormal glutamatergic neurotransmission and neuronal-glial interactions in acute mania. Biol. Psychiatry. 64(8), 718–726. https://doi.org/10.1016/j.biopsych.2008.05.014 (2008).
Gigante, A. D. et al. Brain glutamate levels measured by magnetic resonance spectroscopy in patients with bipolar disorder: A meta-analysis. Bipolar Disord. 14(5), 478–487. https://doi.org/10.1111/j.1399-5618.2012.01033.x (2012).
Kubo, H. et al. 1H-magnetic resonance spectroscopy study of glutamate-related abnormality in bipolar disorder. J. Affect. Disord. 208, 139–144. https://doi.org/10.1016/j.jad.2016.08.046 (2017).
Gao, Y. et al. Olfactory neuroepithelial neural progenitor cells from subjects with bipolar I disorder. J. Cent. Nerv. Sys. Dis. 9, 1179573517694529. https://doi.org/10.1177/1179573517694529 (2017).
Khalyfa, A. et al. Gene expression profiling for adult human olfactory neuroepithelial-derived progenitors. Gene Ther. Mol. Biol. 11, 203–218 (2007).
Gao, Y., Lei, Z., Lu, C., Roisen, F. J. & El-Mallakh, R. S. Effect of ionic stress on apoptosis and the expression of TRPM2 in human olfactory neuroepithelial-derived progenitors. World J. Biol. Psychiatry. 11(8), 972–984. https://doi.org/10.3109/15622975.2010.507784 (2010).
Hu, M., Gao, Y. & El-Mallakh, R. S. Bipolar disorder-derived olfactory neuroepithelial progenitors more susceptible to glutamate induced apoptosis and lithium rescue than cells from non- bipolar subjects. J. Affect Disord. 294, 568–573. https://doi.org/10.1016/j.jad.2021.07.064 (2021).
Coppen, A., Shaw, D. M., Malleson, A. & Costain, R. Mineral metabolism in mania. Br. Med. J. 1(5479), 71–75. https://doi.org/10.1136/bmj.1.5479.71 (1966).
Shaw, D. M. Mineral metabolism, mania, and melancholia. Br. Med. J. 2(5508), 262–267. https://doi.org/10.1136/bmj.2.5508.262 (1966).
Yu, X. M. & Salter, M. W. Gain control of NMDA-receptor currents by intracellular sodium. Nature 396(6710), 469–474. https://doi.org/10.1038/24877 (1998).
Xin, W. K. et al. A functional interaction of sodium and calcium in the regulation of NMDA receptor activity by remote NMDA receptors. J. Neurosci. 25(1), 139–148. https://doi.org/10.1523/JNEUROSCI.3791-04.2005 (2005).
Efendiev, R., Bertorello, A. M., Zandomeni, R., Cinelli, A. R. & Pedemonte, C. H. Agonist-dependent regulation of renal Na+, K+-ATPase activity is modulated by intracellular sodium concentration. J. Biol. Chem. 277(13), 11489–11496. https://doi.org/10.1074/jbc.M108182200 (2002).
Tsuchida, K. et al. Monensin-induced increase in intracellular Na+ induces changes in Na+ and Ca2+ currents and regulates Na+-K+ and Na+-Ca2+ transport in cardiomyocytes. Pharmacology 106(1–2), 91–105. https://doi.org/10.1159/000510576 (2021).
Miraglia, E. et al. Na+/H+ exchanger activity is increased in doxorubicin-resistant human colon cancer cells and its modulation modifies the sensitivity of the cells to doxorubicin. Int. J. Cancer. 115(6), 924–929. https://doi.org/10.1002/ijc.20959 (2005).
Mertens, J. et al. Differential responses to lithium in hyperexcitable neurons from patients with bipolar disorder. Nature 527(7576), 95–99. https://doi.org/10.1038/nature15526 (2015).
Lichtstein, D. et al. Na+, K+-ATPase signaling and bipolar disorder. Int. J. Mol. Sci. 19(8), 2314. https://doi.org/10.3390/ijms19082314 (2018).
Leussis, M. P., Madison, J. M. & Petryshen, T. L. Ankyrin 3: Genetic association with bipolar disorder and relevance to disease pathophysiology. Biol. Mood Anxiety Disord. 2, 18. https://doi.org/10.1186/2045-5380-2-18 (2012).
Rapoport, S. I., Basselin, M., Kim, H. W. & Rao, J. S. Bipolar disorder and mechanisms of action of mood stabilizers. Brain Res. Rev. 61(2), 185–209. https://doi.org/10.1016/j.brainresrev.2009.06.003 (2009).
El-Mallakh, R. S. & Huff, M. O. Mood stabilizers and ion regulation. Harv. Rev. Psychiatry. 9, 23–32 (2001).
Funding
This work was supported by the Jesse H. Wright, M.D. Endowment for Mood Disorders Research at the University of Louisville Depression Center.
Author information
Authors and Affiliations
Contributions
Y.G., design, performance, supervision, statistics, and writing. A.A.M., performance, statistics, writing. Carleigh Litteral, writing. N.A.D., sodium measurement, writing. R.S.E.-M., design, supervision, writing.
Corresponding author
Ethics declarations
Competing interests
Dr. El-Mallakh is a speaker for the following pharmaceutical companies: Eisai, Indivior, Intra-Cellular, Janssen, Lundbeck, Otsuka, Sunovion, and Teva. None of the other authors have any potential conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, Y., Mack, A.A., Litteral, C. et al. NMDA receptor inhibition prevents intracellular sodium elevations in human olfactory neuroepithelial precursors derived from bipolar patients. Sci Rep 12, 10437 (2022). https://doi.org/10.1038/s41598-022-14187-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-14187-w
- Springer Nature Limited