Abstract
To date, no study has reported the objective metabolic laboratory findings worldwide or the comorbidities for Ménière’s disease (MD) using a population-based design in Asian populations. The aim of this study was to investigate the comorbidities and associated factors for MD using the Korean National Health Insurance Service database. This retrospective population-based study was conducted using a data from the National Sample Cohort database from 2009 to 2015. We only enrolled patients whose records showed a prescription for MD medicine and audiometry findings as well as an appropriate diagnostic code. We also included a matched cohort without MD who were enrolled randomly and matched for sex, age, year of diagnosis, income level, and residential area with the MD group with a ratio of 10:1. We evaluated comorbidities including autoimmune, allergic, metabolic diseases and cancer and the health screening data including general characteristics (height, weight, waist circumference, body mass index, and blood pressure), laboratory findings (fasting glucose, cholesterol, triglyceride, high-density lipoproteintryglyceride (HDL) cholesterol, low-density lipoproteintryglyceride cholesterol, hemoglobin, creatinine, aspartate aminotransferase and alanine aminotransferase, and gamma-glutamyltrans- peptidase (rGT)), and general health behaviors (smoking, alcohol, and exercise) of the MD group, and compared these characteristics with those of the MD-free control group. A total of 2,013 and 20,130 participants were included in the MD and MD-free control groups (1,640 and 15,458 for health screening data). We found the increase in incidence of allergic rhinitis and allergic asthma, decrease in systolic blood pressure, HDL cholesterol, and rGT, and less frequent alcohol consumption and less prevalent smoking in the MD group. No significant differences were observed between the groups in the incidence of autoimmune diseases, and cerebro- and cardiovascular disease as well as health screening data and objective laboratory findings. Inconsistence with published studies, the results of this study suggest that the autoimmunity and metabolic disorder, and skeletal growth might not be associated with the onset of MD. Another well-designed study for other races will be needed to the generalization of this study results.
Similar content being viewed by others
Introduction
Ménière’s disease (MD) is a multifactorial disorder of the inner ear characterized by vertigo, tinnitus, and sensorineural hearing loss1. Due to changes in diet and an increase in the aging population, the incidence of MD has rapidly increased2,3. In recent population-based studies, the incidence of MD was 13–118 per 100,000 persons2,3.
MD is a complex heterogeneous disorder, with multiple factors reported to contribute to its development, 4 including age (older than 60 years), sex (female) 2,3, genetics5,6, race (white people)7, stature and leg length (short)8, metabolic disorder9,10, autoimmunity10,11,12,13,14,15,16,17, anatomy18, allergies19, migraines20, weather (high humidity and low atmospheric pressure)21, diets, and stress22. However, the majority of studies are limited by a lack of population-based cohorts and low number of cases; therefore, the underlying disease pathological pathways remain unclear. Furthermore, despite the recent rapid increase in the incidence of MD in Asian populations23, few studies have reported the comorbidities of MD in Asian countries.
To the best of our knowledge, to date, no study has reported the objective metabolic laboratory findings worldwide or the comorbidities for MD using a population-based design in Asian populations. The aim of this study was to investigate the comorbidities and associated factors for MD over 7 years in South Korea using the Korean National Health Insurance Service (NHIS) database (Table 1).
Result
Baseline characteristics of participants
Finally, 2,013 participants with MD and 20,130 controls (1,640 and 15,458 for health screening data) were enrolled in the analysis. No significant differences in age, sex, year of diagnosis, income level, and residential area were observed between the two cohorts (Table 2).
Comorbidities associated with MD
Of the autoimmune diseases, we found no significant association between MD and rheumatoid arthritis, ankylosing spondylitis, type 1 diabetes mellitus (DM), Grave’s disease, and Hashimoto’s thyroiditis. Due to the limited number of patients with each autoimmune disease, we also compared the total number of autoimmune rheumatic diseases (systemic lupus erythematous, dermatomyositis/polymyositis, systemic sclerosis, Sjogren’s syndrome, ankylosing spondylitis, and rheumatoid arthritis) and autoimmune non-rheumatic diseases (type 1 DM, Grave’s disease, Hashimoto’s thyroiditis, Crohn’s disease, ulcerative colitis, autoimmune hepatitis), and no significant differences were observed between the two groups. Among the allergic diseases, the patients with MD were at increased risk of allergic rhinitis (odds ratio [OR] 2.000, 95% CI 1.790–2.240) and allergic asthma (OR 1.469, 95% CI 0.992–2.101) compared with the controls. Regarding the incidence of cerebro- and cardiovascular diseases and cancer, there were no significant differences between the two groups (Table 3).
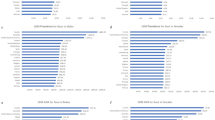
Health screening data
Among the general characteristics studied, we found no significant differences in height, weight, body mass index (BMI), and waist circumference between the patients with MD and controls. Systolic BP was significantly lower in the patients with MD. Laboratory findings showed that HDL cholesterol and rGT levels significantly decreased in the patients with MD. We found no significant differences in fasting glucose, total cholesterol, triglyceride, LDL cholesterol, hemoglobin, creatinine, AST, and ALT levels between the patients with MD and controls. Of the general health behaviors, alcohol intake and smoking history were less frequent in the patients with MD, whereas there were no differences in exercise frequency (Table 4).
Discussion
In this large population-based study, we investigated comorbidities including autoimmune, allergic and metabolic diseases, cancer, as well as health screening data (including general characteristics, laboratory findings, and general health behaviors of patients with MD), and compared these characteristics to those of matched MD-free controls.
We found an increase in the incidence of allergic rhinitis and allergic asthma in patients with MD, similar to that in previous studies that reported a higher number of patients with a history of allergy and the prevalence of allergic diseases, a higher positive rate of the allergic skin test, and elevated Immunoglobulin E levels in patients with MD compared with those in controls3,24,25,26. Randomized controlled studies regarding the treatment of allergy and its association with MD attacks would be helpful to achieve confirmative conclusions.
We further found less frequent alcohol consumption and less prevalent smoking in patients with MD, consistent with the findings of previous studies that reported a lower OR in current smokers and alcohol drinkers10 and low prevalence of smoking and alcohol consumption among MD cases3. For alcohol consumption in patients with MD, there are positive aspects, such as alcohol consumption has inhibitory effects on hypothalamic vasopressin production, leading to an increase of diuresis and reduction of endolymphatic pressure27. This might be a possible cause for less frequent alcohol consumption in the MD population. However, there is a negative aspect that alcohol has toxic effects on the cochlear and labyrinth28, therefore, clinicians should not guide their patients to consume more alcohol before more confirmatory studies are conducted. There are no studies that reported a direct association between smoking and MD; however, there is a retrospective study that reported that smoking cessation contributes to the prevention of new peripheral vestibular disorders among males29. Further, smoking is known to cause vasoconstriction and a decrease in blood flow. Since alcohol consumption and smoking have a positive correlation30, alcohol consumption might be a confounder in the association between smoking and MD.
Moreover, no significant differences in the incidence of autoimmune diseases and cerebro- and cardiovascular disease were observed between patients with MD and controls. In health screening data, body weight, waist circumference, BMI, and objective laboratory findings (fasting glucose, cholesterol, triglyceride, LDL cholesterol, AST, and ALT levels) were not significantly different between patients with MD and controls. Moreover, systolic BP, HDL cholesterol, and rGT levels were lower in patients with MD.
The exact mechanism of MD remains unclear, although several etiologies including autoimmune, allergic, genetic, traumatic, or infectious (viral) conditions have been proposed1. The association between autoimmunity and MD has been supported by the high prevalence of systemic autoimmune diseases in patients with MD10,13,14,15. The relationship between metabolic disorder and MD has also been suggested. Previous studies have reported that DM is associated with severe hearing loss and frequent vertigo in cases of MD9 and higher BMI and systolic BP are related to MD10. Therefore, the present study results are not consistent with those of previous studies.
The primary disadvantage of administrative database-based research is the risk of inaccurate cohort identification, which can lead to selection bias. Therefore, definitions of specific diseases determine the quality of the population-based study31. Previous studies used the definition of diseases only based on diagnostic code, not including specific tests or treatments, used self-reported diagnosis, or did not match the control cohort with patient cohort10,13,14,15. In this study, MD was defined not only based on diagnostic code but also based on the audiometry findings and medications2. Moreover, to select accurate comorbidities, we applied a registration program code that requires many tests or prescription history or used prescription history, refers to the previous studies. Therefore, selection bias might be the reason for the heterogeneity between the results of previous studies and this study. However, elevated levels of serum autoantibodies16,17, cytokines, and chemokines12 in patients with MD have also been reported in Italian and Spain studies. Therefore, there is a possibility that the lack of significance in autoimmune diseases might be due to racial characteristics.
A previous UK study reported that tall stature and high leg length are associated with the prevalence of MD, suggesting that early life environmental exposures may influence skeletal growth and onset of MD8. However, inconsistent with the previous study, height was not significantly different between the two groups in this study. This may be due to the self-reported diagnosis of MD in the previous study8 or racial differences.
In conclusion, this study observed the comorbidities and conditions of patients with MD using a national population database, multiple diagnostic criteria, and stratified matched control group. To the best of our knowledge, this study is the first globally to observe objective laboratory findings and to compare height, weight, BMI, waist circumference, BP, and many comorbidities using population-based design in Asian countries. Some of the results are not consistent with those of previous studies; therefore, other well-designed studies for other races will be needed to generalize the results of this study.
Conclusions
We investigated the comorbidities including autoimmune, allergic, metabolic diseases and cancer and the health screening data including general characteristics (height, weight, waist circumference, body mass index, and blood pressure), laboratory findings (fasting glucose, cholesterol, triglyceride, HDL cholesterol, low-density LDL cholesterol, hemoglobin, creatinine, AST, ALT, and rGT), and general health behaviors (smoking, alcohol, and exercise) of patients with MD using a national population database. We found the increase in incidence of allergic rhinitis and allergic asthma, decrease in systolic blood pressure, HDL cholesterol, and rGT, and less frequent alcohol consumption and less prevalent smoking in the MD group. Inconsistence with published studies, the results of this study suggest that the autoimmunity and metabolic disorder, and skeletal growth might not be associated with the onset of MD. In this study, we applied a registration program code, used multiple diagnostic criteria, and stratified matched control group to minimize the selection bias; however, previous studies used the definition of diseases only based on diagnostic code, not including specific tests or treatments, used self-reported diagnosis, or did not match the control cohort with patient cohort. Therefore, selection bias might be the reason for the heterogeneity between the results of previous studies and this study. Another well-designed study for other races will be needed to the generalization of this study results.
Methods
Data source
In South Korea, 97% of the population is covered by national health insurance, and the remaining 3% is covered by the medical aid program. The Korean NHIS includes all claims of both these programs; thus, it can be used as a data source to identify the health status of the whole nation. Using the sub-datasets, we selected a National Sample Cohort (NSC) database (DB), which has been used in previous studies32,33. The NHIS-NSC DB is an approximately 2% random sample (n = 1,000,000) of all citizens stratified according to age, sex, income level, and residential area. The DB includes data on the participants’ insurance eligibility, medical treatment history, health care provider’s institution, and general health screening data from 2002 to 2015. In this study, we used NHIS-NSC data from 2009 to 2015. A more detailed description of these data is provided in a previous study34. All methods were performed in accordance with the relevant guidelines and were approved by the Institutional Review Board (IRB) of the Kyung Hee University Hospital at Gangdong (IRB No.2020-03-007). Informed consent was unnecessary because this study involved minimal risk to human subjects, and its requirement was waived by the IRB of the Kyung Hee University Hospital at Gangdong (IRB No.2020-03-007).
Study population
In the present study, a patient with MD was operationally defined as a person who had a diagnostic code of MD (International Classification of Diseases 10th revision [ICD-10] codes: H810 or H810.002) as the primary or secondary diagnosis code, had a record of pure-tone audiometry (codes E6931 and F6341), and who had been prescribed betahistine, referring to the diagnostic criteria established by the American Academy of Otolaryngology-Head and Neck Surgery35,36 and Barany Society37 and previous UK and Korea nationwide population-based study of MD2,3 (washout period was from 2002 to 2004). As in other previous population-based studies, because of the limitation of the administrative database, the degree or type of hearing loss and the frequency of vertigo could not be applied to the definition of the disease. A matched cohort without MD was enrolled randomly by matching patients by sex, age, year of diagnosis, income level, and residential area to the MD group at a ratio of 10:1.
Comorbidities based on medical treatment history
The South Korean government has enhanced benefit coverage and established a registration program for four major conditions (cancer, cardiovascular disease, cerebrovascular disease, and rare diseases). The patients must meet the diagnostic criteria related to the imaging, cultivation, genetic, histologic test, or clinical diagnosis, which is applied differently to each condition, to be registered in this program. In this study, comorbidity data were extracted using the V code from the registration program or prescription history combined with ICD-10 diagnosis code (comorbidities that cannot apply V code) to identify patients more accurately with comorbidities. We evaluated four types of comorbidities: (i) autoimmune diseases (rheumatic and non-rheumatic), (ii) allergic diseases, (iii) metabolic diseases, and (iv) cancer. The details of the diagnostic criteria are presented in Table 1. We included the comorbidities which could refer to the definition of disease according to the previous population based Korean studies. We also referred to the comorbidities in the other disorder in previous population based Korean studies38,39.
Health screening data
All insured Koreans older than 40 years undergo a biannual health checkup supported by the NHIS, and employees older than 20 years are required to undergo health checkups once a year. We used general health screening data between 2009 and 2015 in the NHIS-NSC DB. Regarding general health screening data, weight, height, waist circumference, and blood pressure (BP) were measured. Fasting blood glucose, total cholesterol, triglyceride, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, hemoglobin, serum creatinine, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and gamma-glutamyl transferase (rGT) levels were also measured in a fasting state. Information on general health behaviors such as alcohol consumption, smoking, and exercise was obtained using self-report questionnaires40.
Statistical analysis
We evaluated associations between MD and comorbidities using univariate logistic regression after adjusting for age, sex, and socioeconomic status. Continuous variables are expressed as number of participants analyzed, mean, standard deviation, median, minimum, and maximum values and categorical variables as frequency and percentage. All statistical analyses were performed using R version 3.5.1. (Foundation for Statistical Computing, Vienna, Austria).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Girasoli, L. et al. Update on vertigo in autoimmune disorders, from diagnosis to treatment. J. Immunol. Res. 2018, 5072582. https://doi.org/10.1155/2018/5072582 (2018).
Kim, M. H. & Cheon, C. Epidemiology and seasonal variation of Meniere’s disease: data from a population-based study. Audiol. Neurootol. 25, 224–230. https://doi.org/10.1159/000506921 (2020).
Bruderer, S. G., Bodmer, D., Stohler, N. A., Jick, S. S. & Meier, C. R. Population-based study on the epidemiology of Meniere’s Disease. Audiol. Neurootol. 22, 74–82. https://doi.org/10.1159/000475875 (2017).
Nakashima, T. et al. Meniere’s disease. Nat. Rev. Dis. Primers 2, 16028. https://doi.org/10.1038/nrdp.2016.28 (2016).
Gallego-Martinez, A., Requena, T., Roman-Naranjo, P. & Lopez-Escamez, J. A. Excess of rare Missense variants in hearing loss genes in Sporadic Meniere disease. Front. Genet https://doi.org/10.3389/fgene.2019.00076 (2019).
Roman-Naranjo, P. et al. Rare coding variants involving MYO7A and other genes encoding stereocilia link proteins in familial meniere disease. Hear. Res. 409, 108329 (2021).
Vrabec, J. T. Genetic investigations of Meniere‘s disease. Otolaryngol. Clin. N. Am. 43, 1121–1132 (2010).
Tyrrell, J. S., Taylor, M. S., Whinney, D. & Osborne, N. J. Associations of leg length, trunk length, and total adult height with Meniere’s: cross-sectional analysis in the UK biobank. Ear Hear. 36, e122-128. https://doi.org/10.1097/AUD.0000000000000132 (2015).
Pieska, T., Kotimaki, J., Mannikko, M., Sorri, M. & Hietikko, E. Concomitant diseases and their effect on disease prognosis in Meniere’s disease: diabetes mellitus identified as a negative prognostic factor. Acta Otolaryngol. 138, 36–40. https://doi.org/10.1080/00016489.2017.1373850 (2018).
Tyrrell, J. S., Whinney, D. J., Ukoumunne, O. C., Fleming, L. E. & Osborne, N. J. Prevalence, associated factors, and comorbid conditions for Meniere’s disease. Ear Hear. 35, e162-169. https://doi.org/10.1097/AUD.0000000000000041 (2014).
Huang, C. et al. Up-regulated expression of interferon-gamma, Interleukin-6 and tumor necrosis factor-alpha in the endolymphatic sac of Meniere’s disease suggesting the local inflammatory response underlies the mechanism of this disease. Front. Neurol. 13, 781031–781031 (2022).
Moleon, M.-D.-C. et al. Clinical and cytokine profile in patients with early and late onset Meniere disease. J. Clin. Med. 10, 4052 (2021).
Kim, S. Y. et al. Association between Meniere’s disease and thyroid diseases: a nested case-control study. Sci. Rep. 10, 18224. https://doi.org/10.1038/s41598-020-75404-y (2020).
Hahn, H. J., Kwak, S. G., Kim, D. K. & Kim, J. Y. A nationwide, population-based cohort study on potential autoimmune association of Meniere disease to atopy and vitiligo. Sci. Rep. 9, 4406. https://doi.org/10.1038/s41598-019-40658-8 (2019).
Gazquez, I. et al. High prevalence of systemic autoimmune diseases in patients with Meniere’s disease. PLoS One 6, e26759. https://doi.org/10.1371/journal.pone.0026759 (2011).
Chiarella, G. et al. Proteomics in Meniere disease. J. Cell. Physiol. 227, 308–312. https://doi.org/10.1002/jcp.22737 (2012).
Nacci, A. et al. Elevated antithyroid peroxidase and antinuclear autoantibody titers in Meniere’s disease patients: more than a chance association?. Audiol. Neurootol. 15, 1–6. https://doi.org/10.1159/000218357 (2010).
Lucinda, L. R., Cristoff, D. D., Coelho, L. O. M., Zanini, O. P. L. & Guimaraes, R. C. C. Anatomical variations in patients with Meniere disease: a tomography study. Int. Arch. Otorhinolaryngol. 22, 231–238. https://doi.org/10.1055/s-0037-1604463 (2018).
Weinreich, H. M. & Agrawal, Y. The link between allergy and Meniere’s disease. Curr. Opin. Otolaryngol. Head Neck Surg. 22, 227–230. https://doi.org/10.1097/MOO.0000000000000041 (2014).
Tabet, P. & Saliba, I. Meniere’s disease and vestibular Migraine: updates and review of the literature. J. Clin. Med. Res. 9, 733–744. https://doi.org/10.14740/jocmr3126w (2017).
Schmidt, W. et al. The weather and Meniere’s disease: A longitudinal analysis in the UK. Otol. Neurotol. 38, 225 (2017).
Kirby, S. E. & Yardley, L. Physical and psychological triggers for attacks in Ménière’s disease. Psychother. Psychosom. 81, 396–398 (2012).
Kim, M. H. & Cheon, C. Epidemiology and seasonal variation of Ménière’s disease: data from a population-based study. Audiol. Neurotol. 25, 224–230 (2020).
Derebery, M. J. Allergic management of Meniere’s disease: an outcome study. Otolaryngol. Head Neck Surg. 122, 174–182. https://doi.org/10.1016/S0194-5998(00)70235-X (2000).
Keles, E. et al. Meniere’s disease and allergy: allergens and cytokines. J. Laryngol. Otol. 118, 688–693. https://doi.org/10.1258/0022215042244822 (2004).
Savastano, M., Giacomelli, L. & Marioni, G. Non-specific immunological determinations in Meniere’s disease: any role in clinical practice?. Eur. Arch. Otorhinolaryngol. 264, 15–19. https://doi.org/10.1007/s00405-006-0147-2 (2007).
Allen, C. D. et al. Exposure to alcohol during adolescence exerts long-term effects on stress response and the adult brain stress circuits. Neuroscience 339, 64–71 (2016).
Verma, R. K., Panda, N. K., Basu, D. & Raghunathan, M. Audiovestibular dysfunction in alcohol dependence. Are we worried?. Am. J. Otolaryngol. 27, 225–228 (2006).
Wada, M. et al. Association between smoking and the peripheral vestibular disorder: a retrospective cohort study. Sci. Rep. 7, 16889. https://doi.org/10.1038/s41598-017-17294-1 (2017).
Shiffman, S. & Balabanis, M. Do drinking and smoking go together?. Alcohol Health Res. World 20, 107 (1996).
Gavrielov-Yusim, N. & Friger, M. Use of administrative medical databases in population-based research. J. Epidemiol. Commun. Health 68, 283–287 (2014).
Kim, S. Y., Chanyang, M., Oh, D. J. & Choi, H. G. Association between depression and rheumatoid arthritis: two longitudinal follow-up studies using a national sample cohort. Rheumatology 59, 1889–1897 (2020).
Yoon, S. Y., Shin, J., Kim, Y. W., Chang, J. S. & Won Kim, H. The mortality rate of Parkinson’s disease and related comorbidities: a nationwide population-based matched cohort study in Korea. Age Ageing https://doi.org/10.1093/ageing/afaa250 (2020).
Lee, J., Lee, J. S., Park, S.-H., Shin, S. A. & Kim, K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 46, e15–e15 (2017).
Goebel, J. A. 2015 Equilibrium Committee amendment to the 1995 AAO-HNS guidelines for the definition of Meniere’s disease. Otolaryngol. Head Neck Surg. 154, 403–404 (2016).
Committee on Hearing and Equilibrium. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. Otolaryngol. Head Neck Surg. 113, 181–185 (1995).
Lopez-Escamez, J. A. et al. Diagnostic criteria for Menière’s disease. J. Vestib. Res. 25, 1–7 (2015).
Kim, B. R., Yang, S., Choi, J. W., Choi, C. W. & Youn, S. W. Epidemiology and comorbidities of patients with chronic urticaria in Korea: a nationwide population-based study. J. Dermatol. 45, 10–16 (2018).
Lee, J., Kwon, H., Jung, H., Kim, G. & Bae, J. Prevalence and comorbidities associated with hidradenitis suppurativa in Korea: a nationwide population-based study. J. Eur. Acad. Dermatol. Venereol. 32, 1784–1790 (2018).
Kim, Y.-H. et al. Waist circumference and all-cause mortality independent of body mass index in Korean population from the National Health Insurance Health Checkup 2009–2015. J. Clin. Med. 8, 72 (2019).
Bae, E. H. et al. Trend of prevalence and incidence of systemic lupus erythematosus in South Korea, 2005 to 2015: a nationwide population-based study. Korean J. Intern. Med. 35, 652 (2020).
Cho, S.-K. et al. Incidence and prevalence of idiopathic inflammatory myopathies in Korea: a nationwide population-based study. J. Korean Med. Sci. 34, e55 (2019).
Kang, G. et al. Incidence, prevalence, mortality and causes of death in systemic sclerosis in Korea: a nationwide population-based study. Br. J. Dermatol. 178, e37–e39 (2018).
Kim, H. J. et al. Incidence, mortality, and causes of death in physician-diagnosed primary Sjögren’s syndrome in Korea: a nationwide, population-based study. Semin Arthritis Rheum. 47(2), 222–227 (2017).
Jang, H.-D. et al. Relationship between dementia and ankylosing spondylitis: a nationwide, population-based, retrospective longitudinal cohort study. PLoS One 14, e0210335 (2019).
Eun, Y. et al. Menopausal factors and risk of seropositive rheumatoid arthritis in postmenopausal women: a nationwide cohort study of 136 million women. Sci. Rep. 10, 1–9 (2020).
Bae, J. M., Lee, J. H., Yun, J. S., Han, B. & Han, T. Y. Vitiligo and overt thyroid diseases: a nationwide population-based study in Korea. J. Am. Acad. Dermatol. 76, 871–878 (2017).
Yang, B. R. et al. Prevalence of extraintestinal manifestations in Korean inflammatory bowel disease patients. PLoS One 13, e0200363. https://doi.org/10.1371/journal.pone.0200363 (2018).
Kim, B. H. et al. Population-based prevalence, incidence, and disease burden of autoimmune hepatitis in South Korea. PLoS ONE 12, e0182391 (2017).
Shin, J.-Y. et al. Changing patterns of adult asthma incidence: results from the National health insurance service-national sample cohort (NHIS-NSC) database in Korea. Sci. Rep. 8, 1–7 (2018).
Acknowledgements
I would like to thank to the Healthcare Big-Data Center, Medical Science Research Institute, Kyung Hee University Hospital at Gangdong for the assistance with statistical analysis used in this research.
Author information
Authors and Affiliations
Contributions
M.H.K. designed the project, carried out the study, interpreted the results, wrote and revised the paper.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, M.H. Population-based study for the comorbidities and associated factors in Ménière’s disease. Sci Rep 12, 8266 (2022). https://doi.org/10.1038/s41598-022-12492-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-12492-y
- Springer Nature Limited
This article is cited by
-
Ménière’s disease and allergy: Epidemiology, pathogenesis, and therapy
Clinical and Experimental Medicine (2023)