Abstract
Obesity is an essential health issue leading to noncommunicable diseases (NCDs) as well as atherosclerotic cardiovascular diseases. We aimed to determine the trends in obesity prevalence among Royal Thai Army (RTA) personnel and their associated factors using the health examination of RTA personnel database. A series of cross-sectional studies were conducted from 2017 to 2021. A self-report guide was created using a standardized case report form to obtain demographic characteristics and determine behavioral risk factors. Obesity was defined as BMI \(\ge\) 25 kg/m2, and a total of 512,476 RTA personnel nationwide were included. Obesity prevalence rose from 42.1% (95% CI 41.7–42.4) in 2017 to 44.2% (95% CI 43.9–44.5) in 2021 (p for trend < 0.001). A significant surge was observed in obesity prevalence among young RTA personnel aged 18–24 years from 23.7% in 2017 to 28.4% in 2021 (p for trend < 0.001). Higher age individuals, male participants and RTA personnel residing in Bangkok tended to have a significantly higher risk for obesity. Further, regular exercise was a protective factor for obesity. Our data emphasized that obesity among the RTA personnel has been continuously rising over one half-decade, especially among young adults.
Similar content being viewed by others
Introduction
Obesity is one of the essential causes of noncommunicable diseases (NCDs) including type 2 diabetes (T2D), cancer, hypertension (HT) as well as atherosclerotic cardiovascular diseases (ASCVD)1,2,3,4,5. In addition, obesity was associated with an increase in the number of chronic diseases as a dose–response relationship6. According to the World Health Organization (WHO) report in 2016, globally, adults aged 18 years and older with body mass index (BMI) > 25 kg/m2 totaled approximately more than 1.9 billion; moreover, of these over 650 million had BMI > 30 kg/m27. The 5th National Health Examination Survey (NHES V) in 2014 indicated that obesity prevalence (BMI ≥ 25 kg/m2) in a Thai population aged ≥ 15 years was 32.9% and 41.8% among males and females, respectively8. Additionally, a recent study among young Thai men provided crucial evidence of rising trends in obesity prevalence from 2009 to 20164.
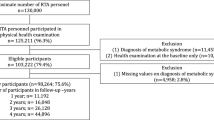
Yearly, Nationwide, approximately 80,000 to 120,000 Royal Thai Army (RTA) personnel individuals participate in the yearly health examination provided by the RTA Medical Department (RTAMED). In the present study, we investigated the trends in obesity prevalence among RTA personnel using the physical health examination of RTA personnel database from 2017 to 2021. Furthermore, we also determined the associations between obesity and age, geographic region, and behavioral factors.
Methods
Study design and subjects
A series of cross-sectional studies were conducted from 2017 to 2021. The dataset was retrieved from the annual health examination database of RTA personnel after obtaining permission from the RTAMED in Bangkok, Thailand. The RTAMED provides annual health examinations for RTA personnel through the Army Institute of Pathology (AIP), Armed Forces Research Institute of Medical Sciences (AFRIMS) and 37 RTA hospitals nationwide; then the records are reported to the RTAMED in Bangkok. Approximately 80,000 to 120,000 RTA personnel access the health examination, annually. The inclusion criteria for this study included active-duty RTA personnel aged 18 to 60 years nationwide. Participants without health examination records each year were excluded.
Data collection
Annually, AIP, AFRIMS and 37 RTA hospitals provide health examinations for RTA personnel. The RTA personnel’s body weight and height were measured to calculate BMI. A self-report guide was created using a standardized case report form to obtain demographic characteristics and behavioral risk factors. The participant’s body weight was measured in kilograms, and the height in centimeters. BMI was calculated as body weight in kilograms divided by height in meters squared (kg/m2).
Outcome variables
BMI was classified in six groups, including < 18.50 kg/m2, 18.5 to 22.99 kg/m2, 23.00–24.99 kg/m2, 25.00 to 29.99 kg/m2, 30.00–34.99 kg/m2 and \(\ge\) 35.00 kg/m2. Obesity was defined as BMI \(\ge\) 25 kg/m9. The age variable of study participants was categorized in eight groups presented in Table 1. The geographic region of residence consisted of Bangkok, north, northeast, central and south. The health scheme of the study participants included Civil Servant Medical Benefit, Social Security and Universal Coverage. Smoking status was categorized in three groups, including (1) never smoked, (2) ex-smoker defined as being smoke-free for 12 months and (3) current smoker. Alcohol consumption was divided in three groups including (1) never consumed, (2) ex-drinker defined as alcohol-free for 12 months and (3) current consumer. Regular exercise was defined as exercise 30 min/day and at least 3 days/week.
Statistical analysis
Statistical analyses were performed using StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. Baseline characteristics were calculated using descriptive statistics. Due to the nature of an observational study, some data of some variables were missing, including smoking status (3.2%), alcohol consumption (2.8%) and exercise (3.6%). Although we were aware of missing data, the study comprised a large sample size; thus, the existing data would be included in the analysis. Categorical variables including sex, age groups, regions, health scheme, smoking status, history of alcohol consumption, a history of exercise and BMI categories were presented as percentage. Continuous variables including age and BMI were presented as mean, standard deviation (SD). The outcome of the study was obesity prevalence among RTA personnel presented as a percentage and 95% confidence interval (CI). P for trend was calculated using chi-square statistics for trends. To determine the association between covariates and obesity, binary logistic regression analysis was performed, and the magnitude of association was presented as crude odds ratio (ORs) with 95% CI. A multiple logistic regression model was used to determine independent factors associated with obesity among RTA personnel. The variables in the final model included year, sex, age, regions, health scheme, smoking status, alcohol consumption and exercise. The magnitude of association was presented as adjusted odds ratio (AORs) with 95% CI. A p-value less than 0.05 was considered statistically significant.
Ethics consideration
The study was reviewed and approved by the Institutional Review Board, RTA Medical Department in compliance with international guidelines such as the Declaration of Helsinki, the Belmont Report, CIOMS Guidelines and the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use—Good Clinical Practice (ICH-GCP) (approval number S067h/64). Due to using secondary data, a waiver of documentation of informed consent was used, and the waiver for informed consent was granted by the Institutional Review Board, RTA Medical Department.
Results
Demographic characteristics
A total of 512,476 RTA personnel were included in the study from 2017 to 2021. Demographic data of participants are presented in Table 1. The average age of participants was 38.2 ± 11.4 years. In all, 467,780 participants (91.3%) were males. One third of all participants resided in the central region. Almost all participants were under the Civil Servant Medical Benefit scheme, approximately 98%. The prevalence of current smokers was 28.5% in 2017 while it reached 33.3% in 2021. In terms of alcohol consumption, approximately two thirds of participants were current drinkers over 5 years. Participants with a history of regular exercise were 39.2% in 2017, and rose to 47.3% in 2021. The average BMI of participants was 24.7 ± 3.7 kg/m2 in 2017, 24.8 ± 3.8 kg/m2 in 2018, 24.9 ± 3.8 kg/m2 in 2019, 24.9 ± 3.9 kg/m2 in 2020 and 25.0 ± 3.9 kg/m2 in 2021.
Trends in obesity prevalence among the RTA personnel from 2017 to 2021
The proportion of the RTA personnel with BMI 25.00 to 29.99 kg/m2 rose from 33.6% in 2017 to 33.8% in 2021 while the proportion of the RTA personnel with BMI 30.00 to 34.99 kg/m2 significantly increased from 7.1 in 2017 to 8.6% in 2021. Furthermore, the prevalence of RTA personnel having BMI \(\ge\) 35 kg/m2 was continuously incremental from 1.3% in 2017 to 1.8% in 2021. Figure 1 demonstrates the proportion of BMI groups among RTA personnel from 2017 to 2021.
From 2017 to 2021, the overall obesity prevalence among RTA personnel increased significantly by the year of the study. Table 2 illustrates the trends in obesity prevalence among RTA personnel by sex, age groups and regions over 5 years. Obesity prevalence rose from 42.1% (95% CI 41.7–42.4) in 2017 to 42.5% (95% CI 42.1–42.8) in 2018, 43.0% (95% CI 42.8–43.3) in 2019, 43.2% (95% CI 43.0–43.5) in 2020 and 44.2% (95% CI 43.9–44.5) in 2021 (p for trend < 0.001). Figure 2 presents obesity prevalence among RTA personnel by sex from 2017 to 2021. Obesity prevalence among male participants was higher than that among females over five years. Among males, obesity prevalence significantly increased from 43.1% in 2017 to 45.3% in 2021 (p for trend < 0.001) while, among females, it rose from 30.2% in 2017 to 31.4% in 2021 (p for trend = 0.010). In addition, obesity prevalence among ages 18 to 49 years significantly rose from 2017 to 2021 (p for trend < 0.05); moreover, a dramatic increase was noted in obesity prevalence among young RTA personnel aged 18 to 24 years by 4.7% over one half-decade (p for trend < 0.001). In terms of geographic region, obesity prevalence among RTA personnel residing in all regions, except in the south, significantly increased over five years (p for trend < 0.05).
Associated factors of obesity among RTA personnel
Univariable and multiple logistic regression analyses were performed to determine the associated factors of obesity among RTA personnel (Table 3). The final model was adjusted for survey year, sex, age, geographic region, health scheme, smoking status, alcohol consumption and history of regular exercise. After adjusting for potential confounders, the results indicated a significant increase in annual obesity prevalence. Male participants had an increased risk of obesity compared with females (AOR 1.96 95% CI 1.89–2.00). Higher-aged participants tended to present obesity when compared with younger participants. RTA personnel in the central, northeast, northern and southern regions had a lower risk for obesity compared with those residing in Bangkok (AOR 0.97, 0.94, 0.91, and 0.81, respectively). Regarding behavioral factors, ex-smokers were more likely to be obese compared with participants who never smoked (AOR 1.14; 95% CI 1.12–1.16) while no association was observed between alcohol consumption and obesity. Moreover, RTA personnel who regularly exercised were at a significantly lower risk of obesity (AOR 0.82; 95% CI 0.81–0.83) than those having no history of regular exercise.
Discussion
To our knowledge, this study represented the largest epidemiologic study of obesity prevalence and its associated factors among RTA personnel in Thailand over one half decade. These data provide crucial evidence of rising trends in obesity prevalence among RTA personnel from 2017 to 2021. Factors associated with obesity included being male, higher age, geographic region, smoking status and no regular exercise.
The average BMI among RTA personnel ranged from 24.7 in 2017 to 25.0 kg/m2 in 2021 increasing at an average of 0.6 kg/m2 per decade. This finding was comparable with the trends in adult BMI in a pooled analysis of 1698 population-based measurement studies from 200 countries10. Compared with the related study among Iranian military personnel, obesity prevalence in the current study was relatively high11. The present study reported the overall obesity prevalence among RTA personnel rose by 2.1% over five years which was compatible with the civilian trends in Thailand showing an increasing obesity prevalence from 37.5 in 20148 to 42.2% in 201912. Similarly, a related study among active-duty military personnel in the US illustrated that combined overweight and obesity (BMI \(\ge\) 25 kg/m2) continuously increased from 50.6% in 1995 to 60.8% in 200813.
Several studies have indicated that obesity prevalence among females was relatively high when compared with that among males6,8,10,12. In this study, male participants tended to present a higher risk for obesity approximately twice that of females corresponding to the obesity situation among military personnel in the US in that overweight and obesity prevalence among males was significantly higher13.
The present study emphasized that a significant rising obesity prevalence among RTA personnel aged 18 to 49 years over 5 years, especially among young RTA personnel aged 18 to 24 years, surged from 23.7 to 28.4% over one half decade. However, among older age groups, a deceleration was observed of rising obesity prevalence during the study period. Correspondingly, the NHES V and VI surveys showed rising trends in obesity prevalence in a Thai population aged 15 to 29 years approximately 7% over 5 years while remaining relatively lower among older Thai adults8,12. In addition, one study in the US demonstrated active-duty military personnel aged less than 25 years having BMI ≥ 25 kg/m2 rose by approximately 8.6% from 1995 to 2008 while it remained slowly incremental among those with higher age13. This could be due to the transformation of Thai society to being more industrial; thus, fast food and high-energy food is more available4,14. The dietary behavior and lifestyle of young adults may facilitate increasing BMI in this age group.
The current study presented that higher age participants tended to have obesity as a dose–response relationship, peaking at 40 to 44 years and dropping at age \(\ge\) 50 years. This pattern was consistent with related studies in the US and China illustrating that obesity prevalence was greater among middle-aged individuals and declined among older people13,15. This phenomenon may be explained by reduced lean muscle mass associated with higher age16.
We found that the RTA personnel residing in Bangkok and the central region were inclined to exhibit obesity when compared with those in other regions. This occurrence was similar to a recent report that the BMI level of people residing in Bangkok and the central region of Thailand was relatively high17. In this area, several agriculture businesses facilitate more than sufficient dietary products combined with inappropriate patient dietary behaviors that might have encouraged increasing weight17. In addition, the NHES VI survey in 2019 reported the proportion of Thai populations aged ≥ 15 years in Bangkok and the central region consuming fast food was relatively high when compared with those in other regions. Moreover, Thais in Bangkok and the central region consumed less dietary fiber including fruits and vegetables among both males and females12.
Our study reported that ex-smokers were inclined to exhibit obesity. Related evidence indicated that weight gain usually occurred after smoking cessation leading to declined metabolic rate, increased caloric intake and changes in food preferences18. Furthermore, one related study in the US reported that weight gain among smokers who quit was more than that gained among current smokers, approximately 4.4 kg among males and 5.0 kg among females over a 10-year period19. Conversely, a recent study reported that smoking status was unassociated with obesity4. However, the finding was outweighed by the advantages of smoking cessation, which are much greater than the superfluous risk granted by the weight gain.
Finally, we found that regular exercise was a protective factor for obesity among RTA personnel similar to a related study among young Thai men4. Therefore, our study suggested that regular exercise, such as increased physical activity, running and weight training, should be encourage among RTA personnel to decrease BMI and alleviate the progression of NCDs including ASCVD20,21. However, the intensity of exercise should be modified appropriately for personal characteristics, especially among individuals with heart disease and elderly people22,23. Our findings emphasized that modifiable risk factors for obesity such as no regular exercise should be improved among RTA personnel. Among young RTA personnel ages 18 to 24 years, obesity prevalence speedily rose over five years; therefore, health interventions including raising awareness regarding reducing their weight and associated further complications such as T2D and HT, should be facilitated in these age groups. Further, modifying dietary behaviors and regular self-weighing can also play an essential role to control BMI level24,25,26.
Several limitations were encountered in this study. First, the study employed a serial cross-sectional design; therefore, the results could demonstrate only the association between factors and outcomes. Second, the present study was conducted among RTA personnel comprising a greater proportion of male participants accounting for 91.3%; however, the results reported the real situation in this study population. According to the observational study using the health examination database, behavioral risk variables were collected very broadly, e.g., total number of alcohol drinks, total number of cigarettes and smoking frequency and intensity of exercise were not recorded. However, the associations between factors and outcomes were able to be presented. Our study also exhibited significant strengths, including a representative, large sample of RTA personnel. Thus, our findings provided valuable insights regarding the prevalence, demographics and behavioral risk factors of obesity in Thailand. Furthermore, these data may contribute to strategies for the primary prevention of metabolic syndrome, T2D, HT and ASCVD in this population.
Conclusion
Our data emphasized that obesity among RTA personnel has been continuously rising from 2017 to 2021, especially among young adults. RTA personnel residing in Bangkok and the central region tended to present a greater obesity prevalence. Regular exercise should be encouraged to alleviate the process of obesity, and dietary behaviors should be modified concurrently.
Data availability
Data cannot be shared publicly because the data set contains identifying information; additionally, the data belong to the Royal Thai Army Medical Department. Thus, ethics restrictions exist concerning the data set. Data are available from the Royal Thai Army Medical Department, Bangkok, Thailand for researchers meeting the criteria to access confidential data.
Abbreviations
- NCDs:
-
Noncommunicable diseases
- T2D:
-
Type 2 diabetes
- HT:
-
Hypertension
- ASCVD:
-
Atherosclerotic cardiovascular diseases
- BMI:
-
Body mass index
- RTA:
-
The Royal Thai Army
- RTAMED:
-
The Royal Thai Army Medical Department
- AIP:
-
Army Institute of Pathology
- AFRIMS:
-
Armed Forces Research Institute of Medical Sciences
- NHES:
-
National Health Examination Survey
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- SD:
-
Standard deviation
References
Hall, J. E., do Carmo, J. M., da Silva, A. A., Wang, Z. & Hall, M. E. Obesity-induced hypertension: Interaction of neurohumoral and renal mechanisms. Circ. Res. 116, 991–1006 (2015).
DeMarco, V. G., Aroor, A. R. & Sowers, J. R. The pathophysiology of hypertension in patients with obesity. Nat. Rev. Endocrinol. 10, 364–376 (2014).
Sakboonyarat, B., Rangsin, R., Kantiwong, A. & Mungthin, M. Prevalence and associated factors of uncontrolled hypertension among hypertensive patients: A nation-wide survey in Thailand. BMC Res. Notes 12, 380 (2019).
Hatthachote, P., Rangsin, R., Mungthin, M. & Sakboonyarat, B. Trends in the prevalence of obesity among young Thai men and associated factors: From 2009 to 2016. Mil. Med. Res. 6, 13 (2019).
Iyengar, N. M., Gucalp, A., Dannenberg, A. J. & Hudis, C. A. Obesity and cancer mechanisms: Tumor microenvironment and inflammation. J. Clin. Oncol. 34, 4270 (2016).
Sakboonyarat, B. et al. Trends, prevalence and associated factors of obesity among adults in a rural community in Thailand: Serial cross-sectional surveys, 2012 and 2018. BMC Public Health 20, 850 (2020).
World Health Organization. Obesity and Overweight (World Health Organization, 2021).
Aekplakorn, W. Thai National Health Examination V (NHES V) (2014).
World Health Organisation. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment (World Health Organisation, 2000).
NCDRF Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants LK. The Lancet (2016). https://maastrichtuniversity.on.worldcat.org/oclc/8100887452. Accessed 11 Jan 2022.
Salimi, Y., Taghdir, M., Sepandi, M. & Karimi Zarchi, A. A. The prevalence of overweight and obesity among Iranian military personnel: A systematic review and meta-analysis. BMC Public Health 19, 162 (2019).
Wichai Aekplakorn. Thai National Health Examination VI (NHES VI) (2019). https://online.fliphtml5.com/bcbgj/znee/#p=187. Accessed 11 Jan 2022.
Reyes-Guzman, C. M., Bray, R. M., Forman-Hoffman, V. L. & Williams, J. Overweight and obesity trends among active duty military personnel: A 13-year perspective. Am. J. Prev. Med. 48, 145 (2015).
Wallinga, D. Today’s food system: How healthy is it? J. Hunger Environ. Nutr. 4, 251–281 (2009).
Wang, R. et al. Prevalence of overweight and obesity and some associated factors among adult residents of northeast China: A cross-sectional study. BMJ Open 6, e010828 (2016).
Gallagher, D. et al. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am. J. Epidemiol. 143, 228 (1996).
Sakboonyarat, B. & Rangsin, R. Prevalence and associated factors of ischemic heart disease (IHD) among patients with diabetes mellitus: A nation-wide, cross-sectional survey. BMC Cardiovasc. Disord. 18, 151 (2018).
Filozof, C., Fernández Pinilla, M. C. & Fernández-Cruz, A. Smoking cessation and weight gain. Obes. Rev. 5, 95 (2004).
Flegal, K. M., Troiano, R. P., Pamuk, E. R., Kuczmarski, R. J. & Campbell, S. M. The influence of smoking cessation on the prevalence of overweight in the United States. N. Engl. J. Med. 333, 1165 (1995).
Tanasescu, M. et al. Exercise type and intensity in relation to coronary heart disease in men. J. Am. Med. Assoc. 288, 1994 (2002).
Ko, I.-G. & Choi, P.-B. Regular exercise modulates obesity factors and body composition in sturdy men. J. Exerc. Rehabil. 9, 256 (2013).
World Health Organization. Global Recommendations on Physical Activity for health (World Health Organization, 2010).
Mittleman, M. A. et al. Triggering of acute myocardial infarction by heavy physical exertion—Protection against triggering by regular exertion. N. Engl. J. Med. 329, 1677 (1993).
Kruger, J., Blanck, H. M. & Gillespie, C. Dietary and physical activity behaviors among adults successful at weight loss maintenance. Int. J. Behav. Nutr. Phys. Act. 3, 17 (2006).
Stelmach-Mardas, M., Mardas, M., Warchol, W., Jamka, M. & Walkowiak, J. Successful maintenance of body weight reduction after individualized dietary counseling in obese subjects. Sci. Rep. https://doi.org/10.1038/srep06620 (2014).
Steinberg, D. M., Bennett, G. G., Askew, S. & Tate, D. F. Weighing every day matters: Daily weighing improves weight loss and adoption of weight control behaviors. J. Acad. Nutr. Diet. 115, 511–518 (2015).
Acknowledgements
The authors are exceedingly grateful to all those involved for successfully conducting the study, including staff of the Health Promotion and Preventive Medicine Division, the Royal Thai Army Medical Department. The authors thank all staff members of the Royal Thai Army Medical Department, the Armed Forces Research Institute of Medical Sciences, the Army Institute of Pathology and 37 RTA hospitals nationwide, for their support in completing this study.
Funding
This research was supported by (1) the FETP-NCD, Division of Epidemiology, Department of Disease Control, Ministry of Public Health, Thailand, and (2) the Research Unit for Military Medicine, Phramongkutklao College of Medicine, Bangkok, Thailand.
Author information
Authors and Affiliations
Contributions
The concept for study was developed by B.S., J.P., K.J., P.S., P.H., M.M. and R.R. B.S., J.P., K.J. and R.R. collected the data. B.S. analyzed the data. B.S. and J.P. wrote the first draft, and all authors contributed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakboonyarat, B., Poovieng, J., Jongcherdchootrakul, K. et al. Rising trends in obesity prevalence among Royal Thai Army personnel from 2017 to 2021. Sci Rep 12, 7726 (2022). https://doi.org/10.1038/s41598-022-11913-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-11913-2
- Springer Nature Limited
This article is cited by
-
Hospital admission and mortality rates for ischemic heart disease in Thailand: 2012–2021
BMC Research Notes (2024)
-
Association between obesity and new-onset heart failure among patients with hypertension in Thailand
Journal of Health, Population and Nutrition (2024)
-
Association between raised blood pressure and elevated serum liver enzymes among active-duty Royal Thai Army personnel in Thailand
BMC Cardiovascular Disorders (2023)
-
Relationship between pulse pressure and body mass index in active-duty Royal Thai Army personnel in Thailand
BMC Cardiovascular Disorders (2023)
-
Relationship between triglyceride-glucose index and aminotransferase among Royal Thai Army personnel 2017–2021: a serial cross-sectional study
Lipids in Health and Disease (2023)