Abstract
Asthma and rhinitis often co-exist in the same patient. Although some authors observed a higher prevalence and/or greater severity of asthma in patients with rhinitis, this view is not homogeneous and the debate continues. The aim of our study is to describe the prevalence of rhinitis in children and adolescents and to analyse their relationship with the prevalence of asthma. A multicentre study was conducted using the methodology of the International Study of Asthma and Allergies in Childhood (ISAAC). The target population of the study was all those school children aged 6–7 and 13–14 years from 6 of the main health catchment areas of Galicia (1.9 million inhabitants). The schools required were randomly selected, and all children in the targeted age ranges were included. Multiple logistic regression was used to obtain adjusted prevalence odds ratios (OR) between asthma symptoms of the schoolchildren and rhinitis prevalence. The results were adjusted for parental smoking habits, maternal education level, cat and dog exposure, and obesity. A total of 21,420 valid questionnaires were finally obtained. Rhinitis was associated with a significant increase in the prevalence of asthma in both age groups. The highest OR were 11.375 for exercise induced asthma (EIA) for children with recent rhinoconjunctivitis and 9.807 for children with recent rhinitis in 6–7 years old group. The prevalence OR’s are higher in EIA and severe asthmatics. Rhinitis in children and adolescents is associated with a higher prevalence and severity of asthma.
Similar content being viewed by others
Introduction
Asthma is a chronic inflammatory disease that often affects children and adolescents. Its prevalence varies widely between different geographic zones, being around 2%–4% in Asia, Northern Africa, Eastern Europe, and Eastern Mediterranean regions, whilst in other countries in Southeast Asia, North America, and Latin America it reaches 29%–32%1. Our community, Galicia, in the Northwest of Spain, has a medium prevalence compared to the rest of the world, being between 11.4% and 15.7% in children and between 8.8% and 18.8% in adolescents2. It is one of the most common causes of Disability-adjusted life years in children and young adults1. The mortality due to asthma in this age group has gradually reduced in the last few years, although with significant differences between different countries1,3.
Rhinitis is diagnosed based on the presence of typical symptoms, such as rhinorrhoea, nasal obstruction, sneezing, or itching. In order to define chronic rhinitis, two of these symptoms must be present for at least one hour per day for 12 weeks a year. It is a very common illness in the paediatric population, with a prevalence that reaches 45% in some areas4.
Asthma prevalence varies significantly worldwide and even between regions closely related geographically and ethnically2,5,6.
Asthma and rhinitis often co-exist in the same patient, in children as well as in adults. Asthma is found in up to 38% of patients with allergic rhinitis (AR) and nasal symptoms are present in 6% to 85% patients with asthma7. However, although some authors observed a higher prevalence and/or greater severity of asthma in patients with rhinitis8,9, this was not confirmed by other studies10,11. Likewise, although different studies appear to support the atopic course, as such that allergic diseases occur following a time-based order from atopic dermatitis and food allergy to asthma and allergic rhinitis12,13, other authors say that the typical atopic course does not occur in their populations, possibly in relation to environmental factors14,15. The results of previous studies seem to support that the atopic march is less frequent than classically considered. In a UK cohort study, including more than 9000 children, it was observed that less than 7% of children with eczema follow the trajectory of the classic atopic march16. In another study, it has been shown that a fifth of children with asthma without food allergy or atopic dermatitis ended up developing the dermatological disease, which we could be considered as a reverse atopic march17.
The aim of the present study is to describe the prevalence of rhinitis in children and adolescents in this community and to analyse the relationship with the prevalence and severity of asthma.
Materials and methods
Study population
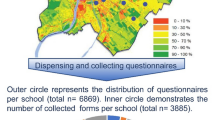
A multicentre study was conducted using the methodology of the International Study of Asthma and Allergies in Childhood (ISAAC)18. Written questionnaires, previously translated and validated in Spanish, were used19. The study was approved by the Clinical Research Ethics Committee of Galicia (code number 2005/116). All research was performed in accordance with relevant guidelines/regulations, and in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects before inclusion.
The target population of the study was all those school children aged 6–7 and 13–14 years from 6 of the main health catchment areas of Galicia, which includes a total of 1.9 million inhabitants, sixty nine percent of the population in this Autonomous Region19. At these ages, schooling is mandatory by law, thus it can be assumed that the schooling rate is quite close to 100%. In each area, a research team leaded by a Medical Doctor specialist in Paediatrics or Respiratory Medicine was set up to carry-out the study.
Following the ISAAC protocol, a minimum sample size of 1000 valid questionnaires was established for each age group and for each area studied in order to obtain the levels of prevalence, and to also detect the possible differences between the areas analysed18.
The schools required from each health area were randomly selected, and all children in the targeted age ranges were included. The schools that refused to take part in the study were replaced with others. Permission was sought from parents or guardians, who also completed the questionnaires for the 6–7 years age group, whereas in the older age group the responses to the questionnaires were made by the children themselves.
Fieldwork was conducted between October 2006 and February 2007. The questionnaire data was introduced manually into a data base, using double entry with subsequent validation, in accordance with the ISAAC protocols. The environmental questionnaire included questions about asthma and rhinitis symptoms, self-reported height and weight, exposure to pets, smoking habits of parents, and mother’s education level. Obesity and overweight were defined in accordance with the Body Mass Index (BMI) cut-off points suggested by Cole et al.20 for each age group and gender. The educational level of the mother was classified into 3 categories: (1) No education or only primary school education; (2) Secondary school education; (3) University education. Four mutually exclusive categories of passive smoking were established for each child: neither parent smoked, the father only, the mother only, and both. The presence of a dog or cat in the home was classified based on the questionnaire questions corresponding to having a cat or dog in the home during the first year of life or during the past year.
For the purpose of this study several definitions of rhinitis were taken into account as independent variables. “Rhinitis ever” was defined as a positive answer to the question “Have you (has your child) ever had a problem with sneezing or a runny or blocked nose, when you (he or she) DID NOT have a cold or the flu?”. "Recent rhinitis" was determined by a positive response to question “In the past 12 months, have you (has your child) had a problem with sneezing or a runny or blocked nose, when you (he or she) DID NOT have a cold or the flu?”. "Recent rhinoconjunctivitis" determined by a combination of positive responses to questions: “In the past 12 months, have you (has your child) had a problem with sneezing or a runny or blocked nose, when you (he or she) DID NOT have a cold or the flu?”, and “In the past 12 months, has this nose problem been accompanied by itchy-watery eyes?”.
"Severe rhinoconjunctivitis" included children and adolescents with “Recent rhinoconjunctivitis” and, with the answer “a lot” to question “In the past 12 months, how much did this nose problem interfere with your (child´s) daily activities? (Not at all/a little/a moderate amount/a lot)”19.
As primary dependent variables, some definitions of asthma were considered. “Wheezing ever” was defined as a positive answer to the question “Has your child ever had wheezing or whistling in the chest at any time in the past?”. “Current asthma” was defined as a positive answer to the question “Has your child had wheezing or whistling in the chest during the last 12 months?”. “Severe asthma” was defined as a combination of the three questions assessing the severity of asthma: “How many attacks of wheezing has your child had during the last 12 months? (none, 1–3, 4–12, > 12)”, “In the last 12 months, how often on average has your child’s sleep been disturbed due to wheezing? (never, < 1 night/week, > = 1 nights/week)”, and “In the last 12 months, has wheezing been severe enough to limit your child’s speech to only one or two words at a time between breaths?”. Children were considered to have current severe asthma when there were > = 4 asthma attacks or when sleep was disturbed > = 1 nights/week or when there had been an episode of speech limitation. “Exercise induced asthma (EIA)” was defined as a positive answer to the question, “In the last 12 months, has your child's chest sounded wheezy during or after exercise?”20.
Data analysis
Children with rhinitis were considered as exposed, while those with asthma were considered as having the outcome of interest. Binary variables were compared using the Chi-squared test.
Adjusted Prevalence ORs and 95%CI were estimated using multivariate logistic regression models. For all statistical models, adjustment for potential confounders was carried out using the change-in-estimate method21. Covariables with p-value < 0.2 were introduced consecutively into the model, and those that modified the value of the measure of effect by at least 10% were retained in the final model. We consider as potential confounders the following variables and all of them were retained in the final model: gender, parental smoking habits, maternal education level, cat and dog exposure, and obesity.
The children with incomplete data were excluded from the study. The statistical analysis was performed using IBM SPSS statistics 24 software.
Results
In the 6–7 year-old group, 284 centers were randomly selected, out of which 253 agreed to take part in the study. In the 13–14 year-old group, 143 schools were randomly selected, out of which 123 collaborated.
A total of 10,690 valid questionnaires were finally obtained in the 6–7 years age group, and 10,730 in the 13–14 years group, with a response rate of 72.4% and 84.4%, respectively.
The prevalence of rhinitis in the 6–7 years age group was: 29.4% for rhinitis ever, 24% for recent rhinitis, 11.5% for rhinoconjunctivitis, and 0.1% for severe rhinoconjunctivitis. In the group aged 13–14 years, the prevalence was 46.2%, 34.5%, 16.2%, and 0.2%, respectively. The prevalence of wheezing ever in the lower age group was 39.0%, that of current asthma was 13.5%, severe asthma 4.9%, and EIA 6.4%. In the 13–14 years old group, these prevalence’s were 23.0%, 13.2%, 5.8%, and 20.0%, respectively (Table 1). The general characteristics of the children, parental smoking, maternal education level, cat and dog exposure are shown in Table 2.
Univariate analysis shows that the prevalence of asthma symptoms was significantly elevated in the patients with any of the forms of rhinitis analysed (Table 3). Considering the low prevalence of severe rhinoconjunctivitis, the relationship with asthma symptoms were not analysed in these cases. The highest prevalence of asthma symptoms was observed in the patients with recent rhinoconjunctivitis, while there was wheezing ever in 74.4% of children in the 6–7 years group, and in 45.1% of the 13–14 years old group (Table 3).
In the multivariate analysis it was confirmed that rhinitis was associated with a significant increase in the prevalence of asthma, achieving an OR of 11.375 (9.233–14.014) for EIA in 6–7 years old children with recent rhinoconjunctivitis and 9.807 (7.612–12.635) for children of this same age group with recent rhinitis. In general, the prevalence OR’s are higher in the 6–7 years old group than in the 13–14 years old group, especially for EIA and severe asthma (Table 4).
Discussion
The prevalence of rhinitis is elevated in the community studied, exceeding that present in most Western Europe countries that have available data obtained with the same methodology18. In the studied population, rhinitis is clearly more prevalent in the adolescents, unlike what happens in asthma in this same population, where a higher prevalence is observed in the 6–7 years old group, except for EIA20. In our area, asthma is a disease with an elevated prevalence in children and adolescents with rhinitis, as more than half of the 6–7 years old children and more than one-third of the 13–14 years old group have asthma symptoms. This agrees with the results of a recent meta-analysis that showed a strong association between both diseases22. The impact seems particularly relevant in severe asthma, as the presence of rhinitis appears to increase the prevalence of severe asthma by between 3 and 6 times in the older aged group, and more than 9 times in the younger age group. This relationship between rhinitis and more severe forms of asthma has been noted in children as well as adults by other authors8,9,23,24,25; although other authors did not observe any relationship between the rhinitis and the severity of the asthma11,26,27.
This association between rhinitis and asthma may be due to several factors. On the one hand, the rhinitis, by itself, may aggravate the asthma since the asthmatics with rhinitis have a higher FeNO, a lower FEV1, and greater bronchial hyper-reactivity23,25,28. On the other hand, there could be factors, both genetic and environmental, that may contribute to aggravating both the asthma and the rhinitis. It is known that allergic sensitisation, filaggrin loss-of-function mutations and other genetic alterations, treatments, maternal nutrition during pregnancy, and environmental exposure12,29,30,31,32,33,34,35,36.
Another aspect to consider is the concept of ‘united airway diseases (UAD), as such that the upper airway and the lower airway form a single organ, and the symptomatology would be a reflection of the same underlying process with some clinical, epidemiological, and pathophysiological differences37. Some mechanisms have been established that appear to support the pathophysiological interactions between the upper and lower airway, by conditioning the air that we breathe, common inflammatory processes and neural reflexes. The exposure to allergens produces a series of IgE reactions mediated by the release of mastocyte and basophil mediators that would produce rhinorrhoea and sneezing in the upper airway, as well as a cough, oedema, mucosa secretion in the lower airway. At the same time, in the post-mortems of humans that have died due to asthma, it has been demonstrated that there is eosinophilic inflammation in the whole respiratory tract from the nasal mucosa to the lung tissue. Furthermore, the nasal-bronchial reflex is well documented in animal models, which produces an increase in the resistance in the lower airway after nasal provocation with cold air or allergens12.
In conclusion, there is an elevated prevalence of rhinitis in children and adolescents in our community, and it seems to be associated with higher prevalence and severity of the asthma.
References
Serebrisky, D. & Wiznia, A. Pediatric asthma: a global epidemic. Ann. Glob. Health. 85(1), 6 (2019).
López-Silvarrey-Varela, A. et al. Prevalence and geographic variations in asthma symptoms in children and adolescents in Galicia (Spain). Arch. Bronconeumol. 47(6), 274–282 (2011).
Gonzalez-Barcala, F. J. et al. Trends of asthma mortality in Galicia from 1993 to 2007. J. Asthma. 49(10), 1016–1020 (2012).
Doulaptsi, M. et al. Differentiating rhinitis in the paediatric population by giving focus on medical history and clinical examination. Med. Sci. (Basel) 7(3), 38 (2019).
Khoo, S. K. et al. No simple answers for the Finnish and Russian Karelia allergy contrast: methylation of CD14 gene. Pediatr. Allergy Immunol. 27(7), 721–727 (2016).
Ruokolainen, L. et al. Significant disparities in allergy prevalence and microbiota between the young people in Finnish and Russian Karelia. Clin. Exp. Allergy. 47(5), 665–674 (2017).
Brożek, J. L. et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines-2016 revision. J. Allergy Clin. Immunol. 140(4), 950–958 (2017).
Machluf, Y., Farkash, R., Rotkopf, R., Fink, D. & Chaiter, Y. Asthma phenotypes and associated comorbidities in a large cohort of adolescents in Israel. J. Asthma. 57(7), 722–735 (2020).
Pongracic, J. A. et al. Distinguishing characteristics of difficult-to-control asthma in inner-city children and adolescents. J. Allergy Clin. Immunol. 138(4), 1030–1041 (2016).
Albataineh, E. et al. Asthma control and its predictive factors in adult asthma patients. J. Clin. Med. Res. 11(12), 807–817 (2019).
Chen, W., FitzGerald, J. M., Lynd, L. D., Sin, D. D. & Sadatsafavi, M. Long-term trajectories of mild asthma in adulthood and risk factors of progression. J. Allergy Clin. Immunol. Pract. 6(6), 2024-2032.e5 (2018).
Yang, L., Fu, J. & Zhou, Y. Research progress in atopic march. Front. Immunol. 27(11), 1907 (2020).
Yii, A. C. A. et al. Precision medicine in united airways disease: a “treatable traits” approach. Allergy 73(10), 1964–1978 (2018).
Lule, S. A. et al. Life-course of atopy and allergy-related disease events in tropical sub-Saharan Africa: a birth cohort study. Pediatr. Allergy Immunol. 28(4), 377–383 (2017).
González-Barcala, F. J., Martínez-Torres, A. E., Méndez-Brea, P. & García-Marcos, L. With the torch in the mist of the United airway disease: atopic march and other arguments in the search for evidence. Arch. Bronconeumol. https://doi.org/10.1016/j.arbres.2021.09.017 (2022).
Belgrave, D. C. et al. Developmental profiles of eczema, wheeze, and rhinitis: two population-based birth cohort studies. PLoS Med. 11(10), e1001748 (2014).
Barberio, G. et al. Does a “reverse” atopic march exist?. Allergy 63(12), 1630–1632 (2008).
Asher, M. I. et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet 368(9537), 733–743 (2006).
Faraldo-García, A. et al. Cross-sectional study about impact of parental smoking on rhinitis symptoms in children. Clin. Otolaryngol. 42(6), 1275–1280 (2017).
Gonzalez-Barcala, F. J. et al. Exposure to paracetamol and asthma symptoms. Eur. J. Public Health. 23(4), 706–710 (2013).
Greenland, S. Modeling and variable selection in epidemiologic analysis. Am. J. Public Health. 79(3), 340–349 (1989).
Tohidinik, H. R., Mallah, N. & Takkouche, B. History of allergic rhinitis and risk of asthma; a systematic review and meta-analysis. World Allergy Organ J. 12(10), 100069 (2019).
Oka, A. et al. Ongoing allergic rhinitis impairs asthma control by enhancing the lower airway inflammation. J. Allergy Clin. Immunol. Pract. 2(2), 172–178 (2014).
To, M. et al. Persistent asthma from childhood to adulthood presents a distinct phenotype of adult asthma. J. Allergy Clin. Immunol. Pract. 8(6), 1921–1927 (2020).
Deliu, M. et al. Impact of rhinitis on asthma severity in school-age children. Allergy 69(11), 1515–1521 (2014).
Boulay, M. È. et al. Comparative features of Asthma with frequent or infrequent exacerbations: a longitudinal study of retrospective and prospective events. J. Asthma. 55(3), 231–243 (2018).
Hamouda, S., Karila, C., Connault, T., Scheinmann, P. & de Blic, J. Allergic rhinitis in children with asthma: a questionnaire-based study. Clin. Exp. Allergy. 38(5), 761–766 (2008).
de Groot, E. P., Nijkamp, A., Duiverman, E. J. & Brand, P. L. Allergic rhinitis is associated with poor asthma control in children with asthma. Thorax 67(7), 582–587 (2012).
Ramírez González N. Thirdhand smoke: a ubiquitous hidden threat in pandemic times. Arch. Bronconeumol. (Engl. Ed). 2021
Licari, A. et al. The nose and the lung: united airway disease?. Front. Pediatr. 5, 44 (2017).
Chan, A. et al. Filaggrin mutations increase allergic airway disease in childhood and adolescence through interactions with eczema and aeroallergen sensitization. Clin. Exp. Allergy. 48(2), 147–155 (2018).
Yan, Z. et al. Bioinformatics analysis and identification of underlying biomarkers potentially linking allergic rhinitis and asthma. Med. Sci. Monit. 26, e924934 (2020).
Blöndal, V. et al. Study of atopic multimorbidity in subjects with rhinitis using multiplex allergen com-ponent analysis. Clin. Transl. Allergy. 10, 6 (2020).
Bai, X. F. et al. Maternal oral contracep-tive pill use and the risk of atopic diseases in the offspring: a systematic review and me-ta-analysis. Med. (Baltimore) 99(16), e19607 (2020).
Ellie, A. S. et al. Prevalence of child-hood asthma and allergies and their associations with perinatal exposure to home environmental factors: a cross-sectional study in Tianjin, China. Int. J. Environ. Res. Public Health. 18(8), 4131 (2021).
Long, A., Bunning, B., Sampath, V., DeKruyff, R. H. & Nadeau, K. C. Epigenetics and the environment in airway disease: asthma and allergic rhinitis. Adv. Exp. Med. Biol. 1253, 153–181 (2020).
Tiotiu, A. et al. Manifesto on united airways diseases (UAD): an interasma (global asthma association—GAA) document. J. Asthma. 5, 1–16 (2021).
Acknowledgements
This work was funded by the Maria Jose Jove Foundation.
Author information
Authors and Affiliations
Contributions
AAP, TSP, ALSV, FJS, MJC, AFG, JJNF, SPD, JSL, MASJG, LBR, LGS, TPC, MSC, FJGB, contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript. All authors approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Gonzalez-Barcala Francisco-Javier has received speaker fees, consulting fees or research grants from ALK, Astra-Zeneca, Bial, Boehringer-Ingelheim, Chiesi, Gebro Pharma, GlaxoSmithKline, Laboratorios Esteve, Menarini, Mundipharma, Novartis, Rovi, Roxall, Sanofi, Stallergenes-Greer and Teva.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Acevedo-Prado, A., Seoane-Pillado, T., López-Silvarrey-Varela, A. et al. Association of rhinitis with asthma prevalence and severity. Sci Rep 12, 6389 (2022). https://doi.org/10.1038/s41598-022-10448-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10448-w
- Springer Nature Limited