Abstract
To investigate the longitudinal latent state-trait structure of the different dimensions of psychosis symptoms in clinical high-risk state (CHRS) and first episode psychosis (FEP) individuals over a one year time-span. This paper examines if the symptom clusters Positive Symptoms, Negative Symptoms, Affectivity, Resistance, Activation, and Excitement according to the Brief Psychiatric Rating Scale (BPRS) differ in their trait and state characters in 196 CHRS and 131 FEP individuals. Statistical analysis was performed using latent state-trait analysis. On average, trait differences accounted for 72.2% of Positive Symptoms, 81.1% of Negative Symptoms, 57.0% of Affectivity, and 69.2% of Activation, whereas 15.0% of the variance of Resistance and 13.2% of the variance of Excitement were explained by trait differences. Explorative analyses showed a trait components’ increase of 0.408 in Positive Symptoms from baseline up to the 9th month and an increase of 0.521 in Affectivity from baseline up to the 6th month. Negative Symptoms had the highest trait component levels of all subscales between baseline and 6 months. The finding that an increasing proportion of psychosis symptoms is persisting over time underlines the importance of early intervention programs in individuals with psychotic disorders.
Similar content being viewed by others
Introduction
Symptoms occurring in early stages of psychosis represent a heterogeneous psychopathological domain with symptom clusters ranging from hallucinations and thought disorder to emotional withdrawal, blunted affect, depression, and anxiety, and also including hostility, uncooperativeness, and excitement. This exemplary list underlines the diversity in the phenotype of psychotic disorders and hence supports the hypothesis of a multidimensional structure of psychotic symptomatology1. This applies not only to psychosis symptoms in the clinical population, but also to subclinical psychotic experiences in the general population2. Furthermore, previous research has shown that psychotic symptoms differ not only in their clinical expression but also in their longitudinal course: Van Os and colleagues for example showed that there is evidence for a psychosis continuum model ranging from subclinical psychotic experiences (observed experiences below the threshold of its clinical detection) in the general population to psychosis proneness/clinical high-risk state (describing people presenting with potentially prodromal symptoms3,4) and first episode psychosis called psychosis proneness-persistence-impairment model5. The majority of subclinical psychotic experiences seems to be episodic5. However, there is evidence, that these subclinical psychotic experiences (psychosis proneness) may become persistent and subsequently clinically relevant, depending on the degree of environmental exposure interacting with genetic risk. This approach is in line with the neurodevelopmental model of schizophrenia postulating that the mental disorder is the end state of abnormal neurodevelopmental processes that started years before the illness onset6. Rössler and colleagues also found that subclinical psychotic experiences are quite persistent in some individuals7. Another study of van Os and colleagues came to similar results: They found that subclinical psychotic experiences are transitory in about 80% of individuals, while around 20% go on to develop persistent psychotic experiences and 7% a psychotic disorder8. There is evidence that the clinical high-risk state is associated with an increased risk of psychotic disorders and its spectrum of related diagnostic categories such as schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder, brief psychotic disorder, depression/bipolar disorder with psychotic features, substance-induced psychotic disorder, psychotic disorder not otherwise classified9,10. A study of Rössler and colleagues differentiated between schizotypal signs (defined as the reduced capacity for close relationships as well as ideas of reference, odd beliefs, and suspicion/paranoid ideation) and schizophrenia nuclear symptoms (defined as thought insertion, thought-broadcasting, thought control, and hearing voices) and showed that the expression of these symptoms is predominantly influenced by stable traits around age 30, whereas the occasion-specific states are more influential at ages 20 and 5011. Thus, there might be clinical phenotypes with longitudinally more durable characteristics as well as occasion-specific states underlying psychoses.
The concept which these studies are based on is latent state-trait theory12,13, postulating that psychological constructs are not either a trait or a state but can be rather trait-like or rather state-like. Therefore, every characteristic comprises a state and a trait component but with differing proportions. According to the latent state-trait theory, a state represents systematic influences of the measurement situation (occasion-specific), whereas a trait represents temporally stable individual differences in the measured variables (consistent over occasions). A “situation” is defined as the bio-psycho-social conditions that are present in the measurements within a test occasion14. As an example of the differentiation between state and trait effects see Meyhöfer, Bertsch, Esser, and Ettinger (2016)15.
However, there are two questions that are unanswered at this point: (1) How is the proportion of occasion-specific states and stable traits in clinical high-risk state (CHRS) and first episode psychosis (FEP) individuals regarding psychosis symptoms? (2) Do the dimensions of psychotic psychopathology differ in their latent state-trait structure over time?
Our first hypothesis is that the dimensions of psychotic symptoms differ regarding their proportions of occasion-specific states and stable traits in CHRS and FEP individuals. Our second hypothesis is that the latent state-trait structure of the dimensions of psychotic psychopathology differs over time.
Aim of study
Our aim was to determine the proportion of variance related to latent states and traits in CHRS and FEP individuals over a 1 year time-span.
Methods
Context and sample
This study presents a post-hoc analysis of data from CHRS individuals included in the longitudinal research program on the early detection of psychotic disorders (FePsy) at the University of Basel Psychiatric Hospital from April 2000 to May 2017, and of FEP individuals presenting at the Psychosis Early Detection and Intervention Centre (PEDIC) at the Department of Psychiatry, University Medical Centre Hamburg-Eppendorf (UKE Hamburg, Germany) from January 2005 to December 2008. The FePsy and the PEDIC are comparable ongoing and well-established programs for the prevention, early detection, and early treatment of psychosis and are reference centers for these individuals in their catchment areas16,17,18. With their long-term clinical programs and accompanying research, they address this area from an integrated point of view.
To be included, CHRS individuals had to meet the criteria for an at risk mental state in psychosis, namely: attenuated psychotic symptoms or brief limited intermittent psychotic symptoms according to the PACE criteria19, familial aggregation of psychotic disorders in combination with at least two further risk factors similar to the PACE criteria, or a minimal amount and combination of certain risk factors according to the Basel Screening Instrument for Psychosis20. Exclusion criteria were age < 18 years, insufficient knowledge of German, IQ below 85, previous episode of schizophrenic psychosis, psychosis due to organic reasons or substance abuse, or psychotic symptomatology within affective psychosis or borderline personality disorder. Individuals who were treated with antipsychotics > 3 weeks or who had exceeded a 2500 mg cumulative chlorpromazine equivalent dose were also excluded21.
Inclusion criteria for FEP individuals were age 14–65, a schizophrenia spectrum disorder diagnosis according to DSM-IV22, no psychotic episode in the past, and absence of organic disorders presenting with a psychotic syndrome and of mental retardation.
For a more detailed description of the in- and exclusion criteria see Riecher-Rössler et al. (2007 and 2009)16,23 and Hochstrasser et al. (2017)24.
Individuals received treatment as usual, ranging from active surveillance to integrated psychiatric treatment with antipsychotic pharmacotherapy as deemed necessary by the treatment team. Data were collected from service entry every three months over one year (study visits: baseline as well as 3-months, 6-months, 9-months and 12-months follow-up). CHRS individuals were followed-up for transition for a maximum of five years (data from year two to five were not considered in the present study). Once a CHRS individual transitioned, it was counted as dropout. Four individuals were excluded from the analysis because of not showing up for any of the study visits. The final sample consisted of 327 individuals, 196 CHRS and 131 FEP individuals.
Study procedures were conducted in accordance with all local and national regulations, and the local ethics committees (the Ethics Committee of Northwestern and Central Switzerland (EKNZ) and the Ethics Committee of the Ärztekammer Hamburg) approved the study protocols (2465/05, 2515/05, OB-026/06, M12/99). Informed consent has been obtained from each participant. For participants under the age of 18 years, informed consent has been obtained from a parent and/or legal guardian.
Measures
Psychopathology was assessed by trained raters in the FePsy and PEDIC programs using the Brief Psychiatric Rating Scale25 (FePsy), and the Positive and Negative Syndrome Scale for Schizophrenia26 (PEDIC)17,18,27. The PANSS has been developed based on the BPRS, and therefore, all BPRS items can be derived from the corresponding PANSS items. In addition, there is broad evidence for the equivalence of the BPRS and the PANSS28. BPRS ratings for the PEDIC individuals could therefore be extracted from the PANSS ratings.
The BPRS subscales “Positive Symptoms” (items: unusual thought content, conceptual disorganization, hallucinatory behavior, and grandiosity), “Negative Symptoms” (items: blunted affect, emotional withdrawal, and motor retardation), “Affectivity” (items: anxiety, guilt feelings, depressive mood, and somatic concern), “Resistance” (items: hostility, uncooperativeness, and suspiciousness), and “Activation” (items: excitement, tension, and mannerisms-posturing) were calculated according to Shafer29. Furthermore, based on Huber et al. (2012), the BPRS Excited Component (BPRS-EC) (items: excitement, hostility, uncooperativeness, and tension) was calculated as an established measure of aggression and agitation constructed in accordance with the PANSS-EC17,30,31,32. As you can see here, there is a partial item overlap between the subscales Resistance, Activation and Excitement.
Concerning psychometric properties of the BPRS and the PANSS, Bell, et al. found high inter-rater reliabilities and good criterion validities33. The kappa coefficient of the PANSS total score in our data base is κ = 0.68. Kay, Opler and Lindenmayer (1988) found strong correlations of the PANSS and the Scale for the Assessment of Negative Symptoms (SANS) and the Assessment of Positive Symptoms (SAPS), which indicates a good construct validity34.
Statistical analysis
Descriptive statistics are given in total numbers and percentages for nominal scaled variables as well as mean, standard deviation (SD), median (MDN), and range for ordinal and interval scaled variables.
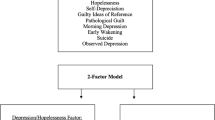
The main analyses consisted of latent state-trait models decomposing the variance of the observed BPRS subscores into variance due to stable individual differences (trait component), variance due to the current study visit (state component), and error variance by using structural equation modeling35. Hence the latent state-trait model implies that the observed variables are affected by the individual and stable characteristics of the person, measurement errors and also situational factors as well as effects of the person-situation interaction14. For each symptom cluster, a latent state-trait model incorporating five lower order state factors (i.e. one for each study visit) and one higher order trait factor was fitted (see Fig. 1)36.
A consistency coefficient r2 was calculated for every subscale and each study visit indicating the proportions of variance explained by trait differences in BPRS subscales. As fit indices, the posterior-predictive p-value (PPP) and the difference between the observed and the replicated chi-square values (Δχ2) were used. PPPs as close as possible to 0.5 and positive upper levels of the CI indicate good fit37. In a first step, we performed the models without indicator-specific trait factors, but since these models did not fit the data, we included indicator-specific trait factors, which resulted in a good model fit. Indicator-specific trait factors (also called method-specific factors) are integrated in the latent state-trait model to take account of temporally stable components of the indicators not shared with the other indicators of the construct by allowing each indicator to load onto its own latent trait factor38.
Group differences (CHRS vs. FEP) regarding the extent of the trait component were directly tested within the structural equation modelling framework by regressing the group variable on the latent trait factor. To verify the assumptions of regression analyses we examined diagnostic residual plots, histograms and Q-Q-Plots. Furthermore, we controlled our analysis for the potential confounders age and gender by regressing these variables on the latent trait factor. All models were fitted in Mplus 739 using Bayesian estimation and handled missing values using the Bayesian parametric multiple imputation approach, which is similar to the full information maximum likelihood estimation approach40,41,42,43.
In contrast to the frequentist inference approach, Bayesian analysis assumes that model parameters are random quantities, not constants, and thus can incorporate prior knowledge. Hence, Bayes combines prior distributions for parameters with the data likelihood to form posterior distributions for the parameter estimates. An important advantage of Bayesian analysis is the acquirement of more balanced results through using previous information mitigating the effect of a small sample size or/and many dropouts44,45.
Ethics committee approval
Study procedures were conducted in accordance with all local and national regulations, and the local ethics committees (the Ethics Committee of Northwestern and Central Switzerland (EKNZ) and the Ethics Committee of the Ärztekammer Hamburg) approved the study protocols (2465/05, 2515/05, OB-026/06, M12/99).
Results
Descriptive statistics of the sample
Of the 327 individuals comprising the final study population, 175 (53.5%) were female and the mean age was 25.0 years (SD: 7.1, range: 14–57). 43 (21.9%) of the 196 CHRS individuals transitioned to first episode psychosis within the follow-up period for transition. Of the 131 FEP individuals, 53 (40.5%) individuals were diagnosed with schizophrenia, 37 (28.2%) with schizophreniform disorder, 12 (9.2%) with schizoaffective disorder, 11 (8.4%) with psychotic disorder not otherwise specified, 6 (4.6%) with delusional disorder and 12 (9.2%) with other schizophrenia-spectrum disorders. 96 (49.0%) of the 196 CHRS individuals and 124 (94.7%) of the 131 FEP individuals received medication (antipsychotics, antidepressants, anxiolytics, and/or mood stabilizers) at any time within the observation period.
Missing data
147 (45.0%) of the participants could be retained over the whole study duration. To control for the effect of dropouts, the latent state-trait analysis was repeated for the subsample without dropouts and yielded qualitatively identical results. Additionally, we performed subgroup analyses for dropouts vs. non-dropouts comparing the sociodemographic variables gender, age, CHRS vs. FEP and BPRS at baseline. Gender, age and BPRS at baseline did not differ regarding dropout status, indicating that the data were missing at random concerning these variables. However, there were significantly more CHRS individuals (134; 74.4%) that dropped out during the observation period than FEP (46; 25.6%) individuals.
Descriptive statistics of BPRS baseline scores
Descriptive statistics of BPRS baseline subscores for CHRS and FEP individuals are shown in Table 1.
Latent state-trait analyses
The results of the latent state-trait analyses showing the proportions of variance explained by trait differences (consistency coefficient r2) in BPRS subscales are presented in Table 2 and visualized in Fig. 2.
On average, 57% to 81.1% of the variance of Positive Symptoms (72.2%), Negative Symptoms (81.1%), Affectivity (57.0%) and Activation (69.2%) across the five different time points was explained by trait differences. However, only 15.0% of the variance in Resistance and 13.2% of the variance in BPRS-EC was explained by trait differences across the five study visits.
Explorative analyses
Explorative analyses showed a trait component increase of 40.8% for Positive Symptoms from baseline (53.9%) up to 9-months follow-up (98.4%) and an increase of 52.1% in Affectivity from baseline (31.1%) up to 6-month follow-up (83.2%). Negative Symptoms had the highest trait component of all subscales between baseline and 6-months follow-up, and the second highest apart from Positive Symptoms at 9-months and 12-months follow-up. PPPs ranged from 0.384 to 0.514 and upper levels of CI were all positive indicating a good fit of the latent state-trait models.
Linear regression analysis
The examination of diagnostic residual plots, histograms and Q–Q-Plots revealed that the assumptions of linearity, homoscedasticity, independence and normality were met.
The results of the linear regression analysis comparing trait components of CHRS and FEP individuals are shown in Table 3.
Subgroup analyses showed all subscales except Excitement to have lower scores on the trait component in CHRS than in FEP individuals. PPPs ranged from 0.161 to 0.504 and upper levels of CI were all positive indicating a good fit.
Discussion
To the best of the authors’ knowledge, this is the first study to assess to what extent the psychopathological syndromes associated with CHRS and FEP are related to latent states and traits over a 1 year time-span.
The dimensions of psychopathological symptoms assessed with the BPRS differ in their latent state-trait structure: Whereas Positive Symptoms, Negative symptoms, Affectivity, and Activation show a relatively high trait component, Resistance and BPRS-EC present with low trait and relatively high state components. Negative Symptoms were the most consistent syndrome. Over all individuals, there is a development indicating an increasing proportion of trait components in psychosis syndromes over time. FEP individuals in general show a higher trait symptom severity than CHRS individuals with the exception of BPRS-EC.
The finding that Negative Symptoms have the highest trait component levels, is in line with previous literature discussing a predominant deficit component of schizophrenia and with clinical experience leading to a persistently impaired course of psychotic and negative symptoms throughout the illness46. For instance, a study of Strauss, et al.46 examining periods of recovery of individuals with and without deficit syndrome over 20 years found that individuals without a deficit syndrome showed more periods of global recovery than individuals with a deficit syndrome47. Another article of Millan, Fone, Steckler, and Horan (2014) gives an integrative overview of Negative Symptoms and discusses possible reasons for their persistence and treatment options47. The difference between CHRS and FEP individuals concerning the trait character of symptomatology is also consistent with the definition of these two groups: CHRS individuals are supposed to have more fluctuating symptoms while FEP individuals should show rather consolidated symptoms19. Furthermore, the finding of higher trait components in FEP than in CHRS individuals is compatible with van Os et al.5 postulating two concepts of psychosis, the psychosis continuum model and the psychosis-proneness-persistence-impairment model. Excitement and Resistance being more episodic supports the evidence from several studies showing that aggressive symptoms change over time as a function of the underlying illness and occur mostly during early treatment correlating with florid psychotic symptoms48,49. As Excitement showed the lowest trait component, this subscale should be used to monitor agitation and aggression in clinical practice.
The result that Positive Symptoms, Negative Symptoms, Affectivity, and Activation seem to be more persistent, while Excitement and Resistance seem to be more episodic, can be interpreted in different ways: On one hand, this finding supports the more common and deficit-oriented view that there may be some persisting symptom clusters, remaining after an acute psychotic episode as residual symptoms. Studies investigating community samples found that the positive symptoms delusional ideation and isolated hallucinations are relatively prevalent (15% to 16%) in the general population and pose a high risk for the development of a psychotic disorder50,51,52,53,54. In addition, negative symptoms can resist control even when positive symptoms are well treated47. The review of Lang et al. showed remission rates of around 50% and rather stable psychopathological symptom patterns with residual symptoms55. Following this line of thought, an adequate treatment of psychosis would mean to focus especially on these persevering symptom clusters.
On the other hand, the rather trait-characterized symptom clusters Positive Symptoms, Negative symptoms, Affectivity, and Activation can be seen as structural types of the disorder. This phenomenological approach, based on the Gestalt theory and described by Parnas56, considers that a psychosis symptom always appears in a holistic context and is part of a “whole” of mutually implicative, interpenetrating experiences, feelings, beliefs, expressions, and actions, influenced by the biographical background of the individual. Even if the conceptualization in the common diagnosis systems DSM-5 and ICD-10 is an important tool helping to communicate among healthcare professionals and ensuring a standardized documentation, it captures only a fragment of the clinical core of schizophrenia-spectrum disorders. As an example, the representatives name the drastically decreased number of cases diagnosed with hebephrenia, while the borderline personality disorder diagnosis increased since the ICD-10 was introduced, hinting on a degree of arbitrariness of the current operationalization of schizophrenia spectrum disorders56. Furthermore, there is evidence that psychopathology is not necessarily related to an impairment in subjective wellbeing: a study examining individuals with first episode psychosis showed no associations between subjective wellbeing and the PANSS subscales Negative Symptoms, Positive Symptoms, Disorganization and Excitement24, supporting a rather resource-oriented point of view and discouraging a perspective focused on residual symptoms. Following this line of thought, our results could provide a basis to disentangle the heterogeneity in the psychopathological presentation of schizophrenia-spectrum disorders and for the investigation of endophenotypes linked to risk factors and biological correlates57.
Strengths of the current post-hoc analysis include the relatively large sample size for this difficult-to-study sample and the equality of time between study visits, avoiding an inequality related bias.
Concerning the composition of the study sample, there are a few more aspects to discuss. The adequate sample size of both subsamples (CHRS, FEP) and the naturalistic nature of the study sample recruited from two established psychosis early detection and treatment programs constitute strengths of this study and enhance the generalizability of the results. On the other hand, only a limited common set of variables on socio-demographic and clinical parameters was available reducing the richness of detail of the sample description and limiting the possibilities of variables to control for (e.g. ethnicity, socio-economic status, intelligence quotient). Furthermore, data was extracted from a treatment as usual (TAU) population including psychopharmacological treatment in some cases. In addition, data on non-pharmacological treatment was unfortunately not available and could not be controlled for. Nevertheless, examining an untreated population would not have been possible due to ethical reasons, making a naturalistic design the best feasible solution. Additionally, there was a relatively high percentage of dropouts, what could have biased our results in the direction of underestimation of trait-components.
Another issue is the broad spectrum of diagnoses included in our analysis, especially the question if the findings could have been influenced by the inclusion of FEP individuals with schizoaffective psychosis. Due to the relatively small percentage of individuals with a schizoaffective psychosis (8.4%) and the similar trait component of Affectivity compared to the subscales Positive Symptoms, Negative symptoms, and Activation, we assume that this effect can be neglected.
Several further limitations of the current study have to be taken into account. The BPRS is based on observations of the individuals’ behaviour over the last fourteen days. As we assessed our patients every three months, potential symptom fluctuations between assessments could not be accounted for. In general, the BPRS and the PANSS focus on symptoms without taking psychosocial functioning into account what leads to a rather limited view of psychopathology. Further studies could integrate measures including the level of functioning to ensure a more comprehensive assessment of the latent state-trait structure of psychosis. In addition, psychopathology was measured using two different psychometric tools: CHRS individuals were assessed using the BPRS, and FEP individuals were assessed using the PANSS with post-hoc extraction of BPRS scores. However, the items of the BPRS and the PANSS have a large overlap and there is evidence showing their equivalence20. Furthermore, although psychopathology was assessed by trained raters in all cases, and although the FePsy and PEDIC programs are similar in their structure and have comparable inclusion and exclusion criteria, systematic differences depending on study centre cannot be completely ruled out, possibly influencing the comparison between CHRS and FEP data. Further monocentric studies are therefore needed to assess if differences found in the current analyses can also be replicated in a more homogeneous population.
Further studies should examine the latent state-trait structure of psychosis symptoms over a larger period of time and could include moderating factors like specific diagnoses (e.g. personality disorders).
To conclude, even if there are several methodological limitations, the current study contributes to a deeper understanding of psychosis and its symptom clusters. Additionally, our results are relevant for clinical practice: an increasing proportion of psychosis symptoms is persisting over time, underlining the importance of the early detection and treatment of psychosis symptoms. Furthermore, differentiating psychosis symptom clusters regarding their stability may help to set priorities, especially in the beginning of treatment.
References
Tonna, M. et al. Dimensional structure of first episode psychosis. Early Interv. Psychiatry 13, 1431–1438. https://doi.org/10.1111/eip.12789 (2019).
Shevlin, M., Boyda, D., Houston, J. & Murphy, J. Measurement of the psychosis continuum: Modelling the frequency and distress of subclinical psychotic experiences. Psychosis 7, 108–118. https://doi.org/10.1080/17522439.2014.931451 (2015).
Fusar-Poli, P. et al. The psychosis high-risk state: A comprehensive state-of-the-art review. JAMA Psychiat. 70, 107–120. https://doi.org/10.1001/jamapsychiatry.2013.269 (2013).
Yung, A. R. et al. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophr. Res. 60, 21–32. https://doi.org/10.1016/s0920-9964(02)00167-6 (2003).
van Os, J., Linscott, R. J., Myin-Germeys, I., Delespaul, P. & Krabbendam, L. A systematic review and meta-analysis of the psychosis continuum: Evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol. Med. 39, 179–195. https://doi.org/10.1017/S0033291708003814 (2009).
Rapoport, J. L., Giedd, J. N. & Gogtay, N. Neurodevelopmental model of schizophrenia: Update 2012. Mol. Psychiatry 17, 1228–1238. https://doi.org/10.1038/mp.2012.23 (2012).
Rossler, W. et al. Psychotic experiences in the general population: A twenty-year prospective community study. Schizophr. Res. 92, 1–14. https://doi.org/10.1016/j.schres.2007.01.002 (2007).
van Os, J. & Reininghaus, U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry 15, 118–124. https://doi.org/10.1002/wps.20310 (2016).
Radua, J. et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 17, 49–66. https://doi.org/10.1002/wps.20490 (2018).
van Os, J., Reininghaus, U. & Meyer-Lindenberg, A. The search for environmental mechanisms underlying the expression of psychosis: Introduction. Schizophr. Bull. 43, 283–286. https://doi.org/10.1093/schbul/sbw178 (2017).
Rossler, W., Hengartner, M. P., Ajdacic-Gross, V., Haker, H. & Angst, J. Deconstructing sub-clinical psychosis into latent-state and trait variables over a 30-year time span. Schizophr. Res. 150, 197–204. https://doi.org/10.1016/j.schres.2013.07.042 (2013).
Steyer, R., Ferring, D. & Schmitt, M. J. States and traits in psychological assessment. Eur. J. Psychol. Assess. 8, 79–98 (1992).
Steyer, R., Geiser, C. & Fiege, C. APA Handbook of Research Methods in Psychology. Data Analysis and Research Publication. Vol. 3. 291–308. (American Psychological Association, 2012).
Hermes, M. & Stelling, D. Context matters, but how much? Latent state-trait analysis of cognitive ability assessments. Int. J. Sel. Assess. 24, 285–295 (2016).
Meyhofer, I., Bertsch, K., Esser, M. & Ettinger, U. Variance in saccadic eye movements reflects stable traits. Psychophysiology 53, 566–578. https://doi.org/10.1111/psyp.12592 (2016).
Riecher-Rössler, A. et al. The Basel early-detection-of-psychosis (FEPSY)-study-design and preliminary results. Acta Psychiatr. Scand. 115, 114–125. https://doi.org/10.1111/j.1600-0447.2006.00854.x (2007).
Huber, C. G., Hochstrasser, L., Meister, K., Schimmelmann, B. G. & Lambert, M. Evidence for an agitated-aggressive syndrome in early-onset psychosis correlated with antisocial personality disorder, forensic history, and substance use disorder. Schizophr. Res. 175, 198–203. https://doi.org/10.1016/j.schres.2016.04.027 (2016).
Lambert, M. et al. Assertive community treatment as part of integrated care versus standard care: A 12-month trial in patients with first- and multiple-episode schizophrenia spectrum disorders treated with quetiapine immediate release (ACCESS trial). J. Clin Psychiatr. 71, 1313–1323. https://doi.org/10.4088/JCP.09m05113yel (2010).
Yung, A. R. et al. Prediction of psychosis. A step towards indicated prevention of schizophrenia. Br. J. Psychiatry Suppl. 172, 14–20 (1998).
Riecher-Rössler, A. et al. The Basel screening instrument for psychosis (BSIP): Development, structure, reliability and validity. Fortschr. Neurol. Psychiatr. 76, 207–216. https://doi.org/10.1055/s-2008-1038155 (2008).
Studerus, E. et al. Can neuropsychological testing facilitate differential diagnosis between at-risk mental state (ARMS) for psychosis and adult attention-deficit/hyperactivity disorder (ADHD)?. Eur. Psychiatry 52, 38–44. https://doi.org/10.1016/j.eurpsy.2018.02.006 (2018).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th edn., text rev.). (2000).
Riecher-Rössler, A. et al. Efficacy of using cognitive status in predicting psychosis: A 7-year follow-up. Biol. Psychiatry 66, 1023–1030. https://doi.org/10.1016/j.biopsych.2009.07.020 (2009).
Hochstrasser, L. et al. The association of psychopathology with concurrent level of functioning and subjective well-being in persons with schizophrenia spectrum disorders. Eur. Arch. Psychiatry Clin. Neurosci. https://doi.org/10.1007/s00406-017-0780-3 (2017).
Overall, J. E. Psychological Measurements in Psychopharmacology: Modern Problems in Psychopharmacology. Vol. 7. 67–78. (Karger, 1974).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276. https://doi.org/10.1093/schbul/13.2.261 (1987).
Huber, C. G. et al. Evidence for an agitated-aggressive syndrome predating the onset of psychosis. Schizophr. Res. 157, 26–32. https://doi.org/10.1016/j.schres.2014.06.014 (2014).
Leucht, S. et al. Linking the PANSS, BPRS, and CGI: Clinical implications. Neuropsychopharmacology 31, 2318–2325. https://doi.org/10.1038/sj.npp.1301147 (2006).
Shafer, A. Meta-analysis of the brief psychiatric rating scale factor structure. Psychol. Assess. 17, 324–335. https://doi.org/10.1037/1040-3590.17.3.324 (2005).
Huber, C. G. et al. Brief Psychiatric Rating Scale-Excited Component (BPRS-EC) and neuropsychological dysfunction predict aggression, suicidality, and involuntary treatment in first-episode psychosis. Schizophr. Res. 134, 273–278. https://doi.org/10.1016/j.schres.2011.12.002 (2012).
Huber, C. G. et al. Applicability of the clinical global impressions-aggression (CGI-A) scale for use in file audit trials. Pharmacopsychiatry 44, 189–192. https://doi.org/10.1055/s-0031-1280816 (2011).
Huber, C. G. et al. Validation of a clinical global impression scale for aggression (CGI-A) in a sample of 558 psychiatric patients. Schizophr. Res. 100, 342–348. https://doi.org/10.1016/j.schres.2007.12.480 (2008).
Bell, M., Milstein, R., Beamgoulet, J., Lysaker, P. & Cicchetti, D. The positive and negative syndrome scale and the brief psychiatric rating-scale—Reliability, comparability, and predictive-validity. J. Nerv. Ment. Dis. 180, 723–728. https://doi.org/10.1097/00005053-199211000-00007 (1992).
Kay, S. R., Opler, L. A. & Lindenmayer, J. P. Reliability and validity of the positive and negative syndrome scale for schizophrenics. Psychiatry Res. 23, 99–110 (1988).
Steyer, R., Schmitt, M. & Eid, M. Latent state-trait theory and research in personality and individual differences. Eur. J. Pers. https://doi.org/10.1002/%28SICI%291099-0984%28199909/10%2913:5%3C389:A (1999).
Steyer, R. & Schmitt, M. J. Latent state-trait models in attitude research. Qual. Quant. 24, 427–445. https://doi.org/10.1007/Bf00152014 (1990).
Fong, T. C. & Ho, R. T. Factor analyses of the Hospital Anxiety and Depression Scale: A Bayesian structural equation modeling approach. Qual. Life Res. 22, 2857–2863. https://doi.org/10.1007/s11136-013-0429-2 (2013).
Geiser, C. & Lockhart, G. A comparison of four approaches to account for method effects in latent state-trait analyses. Psychol. Methods 17, 255–283 (2012).
Geiser, C. Datenanalyse mit Mplus. 2 edn. (VS Verlag für Sozialwissenschaften, 2011).
Bartlett, J. W., Seaman, S. R., White, I. R. & Carpenter, J. R. Alzheimer’s Disease Neuroimaging, I. Multiple imputation of covariates by fully conditional specification: Accommodating the substantive model. Stat. Methods Med. Res. 24, 462–487. https://doi.org/10.1177/0962280214521348 (2015).
Enders, C. K., Baraldi, A. N. & Cham, H. Estimating interaction effects with incomplete predictor variables. Psychol. Methods 19, 39–55. https://doi.org/10.1037/a0035314 (2014).
Kim, S., Sugar, C. A. & Belin, T. R. Evaluating model-based imputation methods for missing covariates in regression models with interactions. Stat. Med. 34, 1876–1888. https://doi.org/10.1002/sim.6435 (2015).
Seaman, S. R., Bartlett, J. W. & White, I. R. Multiple imputation of missing covariates with non-linear effects and interactions: An evaluation of statistical methods. BMC Med. Res. Methodol. 12, 46. https://doi.org/10.1186/1471-2288-12-46 (2012).
Muthén, B. Bayesian Analysis in Mplus: A Brief Introduction. Vol. 203. Unpublished manuscript. https://www.statmodel.com/download/IntroBayesVersion. (2010).
Gelman, A. et al. Bayesian Data Analysis (CRC Press, 2013).
Strauss, G. P., Harrow, M., Grossman, L. S. & Rosen, C. Periods of recovery in deficit syndrome schizophrenia: A 20-year multi-follow-up longitudinal study. Schizophr. Bull. 36, 788–799. https://doi.org/10.1093/schbul/sbn167 (2010).
Millan, M. J., Fone, K., Steckler, T. & Horan, W. P. Negative symptoms of schizophrenia: Clinical characteristics, pathophysiological substrates, experimental models and prospects for improved treatment. Eur. Neuropsychopharmacol. 24, 645–692. https://doi.org/10.1016/j.euroneuro.2014.03.008 (2014).
Lion, J. R., Synder, W. & Merrill, G. L. Underreporting of assaults on staff in a state hospital. Hosp. Commun. Psychiatry 32, 497–498 (1981).
Krakowski, M., Czobor, P. & Chou, J. C. Course of violence in patients with schizophrenia: Relationship to clinical symptoms. Schizophr. Bull. 25, 505–517 (1999).
Johns, L. C., Hemsley, D. & Kuipers, E. A comparison of auditory hallucinations in a psychiatric and non-psychiatric group. Br. J. Clin. Psychol. https://doi.org/10.1348/014466502163813 (2002).
van Os, J., Hanssen, M., Bijl, R. V. & Ravelli, A. Strauss (1969) revisited: A psychosis continuum in the general population?. Schizophr. Res. 45, 11–20 (2000).
Van Os, J. Is there a continuum of psychotic experiences in the general population?. Epidemiol. Psichiatr. Soc. https://doi.org/10.1017/S1121189X0000306714968483 (2003).
Poulton, R. et al. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: A 15-year longitudinal study. Arch. Gen. Psychiatry. https://doi.org/10.1001/archpsyc.57.11.105311074871 (2000).
Malla, A. & Payne, J. First-episode psychosis: Psychopathology, quality of life, and functional outcome. Schizophr. Bull. 31, 650–671. https://doi.org/10.1093/schbul/sbi031 (2005).
Lang, F. U., Kosters, M., Lang, S., Becker, T. & Jager, M. Psychopathological long-term outcome of schizophrenia – A review. Acta Psychiatr. Scand. 127, 173–182. https://doi.org/10.1111/acps.12030 (2013).
Parnas, J. A disappearing heritage: The clinical core of schizophrenia. Schizophr. Bull. 37, 1121–1130. https://doi.org/10.1093/schbul/sbr081 (2011).
Braff, D. L., Freedman, R., Schork, N. J. & Gottesman, I. I. Deconstructing schizophrenia: An overview of the use of endophenotypes in order to understand a complex disorder. Schizophr. Bull. https://doi.org/10.1093/schbul/sbl04917088422 (2007).
Funding
This work was supported by the Swiss Academy of Medical Sciences (SAMS), the Gottfried and Julia Bangerter-Rhyner foundation (CGH) and the research fund of the UPK Basel (LH and CGH). The funding body had no role in the design, collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
C.G.H., E.S. and L.H. designed the study, and L.H. and C.G.H. wrote the initial draft of the paper. C.G.H., E.S., A.R., B.G.S. and M.L. collected the data. L.H., E.S., and C.G.H. analyzed and interpreted the data. C.G.H., L.H., E.S., A.R., B.G.S., M.L., U.E.L., S.B. and R.S. have contributed to, read and approved the final version of the manuscript. L.H. and C.G.H. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hochstrasser, L., Studerus, E., Riecher-Rössler, A. et al. Latent state-trait structure of BPRS subscales in clinical high-risk state and first episode psychosis. Sci Rep 12, 6652 (2022). https://doi.org/10.1038/s41598-022-10207-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10207-x
- Springer Nature Limited
This article is cited by
-
Psychosis superspectrum I: Nosology, etiology, and lifespan development
Molecular Psychiatry (2024)
-
Comparing the latent state–trait structure of the PANSS in cariprazine-medicated and placebo-controlled patients with acute schizophrenia
European Archives of Psychiatry and Clinical Neuroscience (2024)