Abstract
This study aims to investigate the reliability and efficacy of rear 4-min Schirmer test, as a supplement indicator, in assessing tear secretion and diagnosing dry eye. 180 participants were enrolled in this study. Schirmer test I without anaesthesia was performed once on both eyes to determine the value of normal Schirmer test. The values of tear secretion were recorded at each minute. Other examinations included the following: the ocular surface disease index (OSDI), the standard patient evaluation of eye dryness (SPEED), fluorescein stain, tear film break-up time (BUT), and Meibomian gland (MG) secretion grading. The participants were divided into dry eye (DE) group and non-dry eye (ND) group. The values of the 2-min Schirmer test, rear 3-min Schirmer test, rear 4-min Schirmer test, and 5-min Schirmer test were 5.36 ± 4.63, 5.57 ± 2.11, 7.21 ± 4.13, and 10.93 ± 6.30, respectively, in the DE group. These indicators were 8.25 ± 6.80, 2.73 ± 2.31, 7.36 ± 3.42, and 11.84 ± 6.16, respectively, in the ND group. The rear 4-min Schirmer test had a significant correlation with OSDI and SPEED in the DE group (r = − 0.242/ − 0.183) and in the ND group (r = − 0.316/ − 0.373). Meanwhile, the rear 4-min Schirmer test had a stronger connection with fBUT (r = 0.159) and MG secretion (r = − 0.162) in the DE group and also had higher accuracy in diagnosing severe DE and borderline DE. In conclusion, the rear 4-min Schirmer test may be a supplement indicator in assessing tear secretion and diagnosing DE.
Similar content being viewed by others
Introduction
Dry eye (DE) is a common disorder on the ocular surface, and its prevalence is increasing rapidly. The incidence of DE varies from 5 to 35%1,2 due to geographical and ethnic differences. Approximately 30 million people worldwide have DE3. The International Dry Eye Workshop in 2017 defined DE as “a multifactorial disease of the ocular surface characterised by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles”4.
A stable tear film is key to a healthy ocular surface because it can protect the lubricated environment for the eyes5. When the tear film becomes abnormal, patients often have six main symptoms: dryness, gritty or sandy sensation, burning, redness, crust on lashes, and eyelids stuck shut in the morning6. The assessment of people’s symptoms is a major component in the diagnosis of DE. However, the signs of the disease do not always correlate with symptoms, thus necessitating objective ocular examinations. The most common diagnostic tests include the Schirmer test (ST)7,8, tear break-up time (BUT)4, corneal fluorescein staining (CFS)9, tear meniscus height10.
ST was first used as a diagnostic test for DE syndrome in 1903, and it can help to evaluate tear volume11. It is performed by placing a special filter paper at the middle and lateral thirds of the lower fornix with or without anaesthetic8. After 5 min, a person’s tear secretion can be measured using wetting paper. ST is always performed just once in clinical practice. However, ST has several serious disadvantages, such as discomfort, irritation, low reproducibility, requiring a long time, and inconvenience12,13. Because of these limitations, many efforts were made to improve the ST’s efficiency and comfort, just like to be performed this test after using anaesthesia or changing the filter paper14. However, these changes may not make significant improvements. With anaesthesia, a reflex component was still alive, and it may mislead physicians to judge the situation of the examinee.
The measure of tear secretion is always affected by paper irration, especially in first minute of ST15. Because of an adaptation of nervous system16, the speed of tear secretion slowed over time. This sign attracted our attention and we had a idea about how to increase the applicability and convenience of the ST. If we can remove the value of the first minute with a large difference, and then perform a weighted calculation based on the results obtained in the rear 4-min to obtain a theoretical five-minute test value, the value may be used as a supplementary data to make up for the partial shortcomings of classical ST. Our purpose was to investigate the reliability and efficacy of rear 4-min Schirmer test to help ophthalmologists diagnose DE.
Materials and methods
Subjects
This prospective study was performed at the outpatient clinic of the Second Affiliated Hospital of Zhejiang University School of Medicine in September 2019. The way we recruited volunteers was based on sampling of convenience. Participants attending the outpatient department of a teaching hospital attached to a medical college were enrolled in the study. The multiple rate comparison method performed with PASS version 15 was used to estimate sample size. The final sample size also included 10% dropout rate.
All participants were divided into DE and non-dry eye (ND) groups. The criteria of DE diagnosis were OSDI > 13 points and fBUT < 10 s; patients not meeting these criteria was classified into the ND group. Both eyes of per participant were included in this study. The exclusion criteria were as follows: age < 18 years; current pregnancy; eye allergies, conjunctival inflammation, corneal ulcer, eyelid inflammation, palsy, valgus, and other ocular lesions; history of wearing contact lenses within 30 days; history intraocular operation within 6 months; severe blepharitis; or severe systemic disease. This study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (NO. 2019-307). All participants provided written informed consent after an explanation of the nature and possible consequences of the study.
DE symptom questionnaires
Ocular surface disease index
The ocular surface disease index (OSDI) was a validated dry eye questionnaire that can measure the severity of DE, symptoms, functional problems, and environmental triggers queried for the past week17. The OSDI have been regarded as an established standard questionnaire4. Each OSDI answer in 12 questions was graded on a scale of 0–4. A total OSDI scores ranged from 0 to 100. The results were interpreted as follows: normal (scores 0–12) and dry eye (scores 13–100)18.This study used Chinese version and validated in previous studies19,20.
Standard patient evaluation of eye dryness questionnaire
The standard patient evaluation of eye dryness (SPEED) questionnaire was administered to grade the level of DE symptomology21. And the SPEED questionnaire is also useful in assessing dry eye symptoms in a nonclinical sample22. The assessment standard of the SPEED questionnaire is derived by summing the scores from the frequency and severity parts of the questionnaire for 3 months. The values of frequency and severity in the SPEED questionnaire were obtained by summing the scores of the eight items (with each rated from 0 to 4), and the total SPEED scores ranged from 0 to 28. The results were interpreted as follows: normal (scores 0) and dry eye (scores 1–28). We uesd a Chinese language version and validated in previous study23.
DE symptom examinations
ST I
ST was performed once without topical anaesthesia, and both eyes were evaluated at the same time. The filter paper (Showa Yakuhin Kako, Tokyo, Japan) was folded and placed between the lower eyelid and the globe at the junction between the middle and lateral thirds of the eyelid. The participants were asked to close their eyes, as ST with close eyes may be more reliable in DE24. The test lasted 5 min, and the length of the wetted paper was directly read off the scale on the paper. Wetting was measured at 1, 2, 3, 4, and 5 min. The participants were excluded from the study if any of the scores exceeded 30 mm (the whole paper was wetted) because of the inability to give an exact measurement of the amount of wetting. The results were interpreted as follows: ≤ 5 mm: severe DE, ≤ 10 mm: borderline DE, and > 10 mm: normal tear secretion25. We observed multiple indicators of ST, as follows:
-
(1)
ST1: The value of the normal (5-min) ST.
-
(2)
2-min ST: the value of the first 2 min of ST.
-
(3)
Rear 3-min ST: the value of normal ST minus that of first 2 min of ST.
-
(4)
Rear 4-min ST: the value of normal ST minus that of first min of ST.
Tear film BUT
Tear film instability was assessed using BUT measurements, which were obtained using the following method. TBUT tests include fluorescein tear film break-up time (fBUT) and noninvasive tear film break-up time (NIBUT). fBUT: Fluorescein was added to the tear film for both eyes, and the patients were asked to blink several times to ensure uniform distribution. The time from the last blink of the eye to the first dry spot on the tear film was measured. Three consecutive measurements were made and recorded. The average values of the three measurements were recorded. NIBUT: NIBUT was measured using Keratograph 5 M (Oculus Optikgerate GmbH, Wetzlar, Germany). The participants placed the lower jaw on the jaw rest and keep both eyes open. After successful focusing, they were asked to blink twice and look at the red point in the centre, keeping the eye open as much as possible until the next blink. Then, the device automatically detected the tear film distribution map and displayed the measured values. BUT was categorised as moderate (5–10 s) or severe (< 5 s)26,27.
Meibomian gland secretion quality grading
The quality of the Meibomian gland (MG) secretion grading was briefly assessed using a Meibomian Gland Evaluator (TearScience, Morrisville, NC, USA). A total of 15 Meibomian glands (in the nasal, middle, and temporal parts of the lower tarsus) were selected. The quality of meibum was graded as follows: 0, clear fluid; 1, thick and cloudy dropout; 2, inspissated and congealed dropout with the consistency of toothpaste; and 3, no dropout. The total scores ranged from 0 to 45.
CFS score
For CFS, the participants’ cornea was divided equally into five quadrants, and the score for each quadrant was recorded after fluorescein staining, as follows: 0, no punctate staining; 1, less than 30 stained points; 2, more than 30 stained points but no fusion; and 3, entirely stained with fusion. A total score of five parts was given as 0–15.
Sequence of DE tests
Participants completed the tests in the following order: first, each participant signed informed consent forms, completed the OSDI and SPEED questionnaires, and provided general information. Second, a Keratograph 5 M measurement was performed to obtain the NIBUT. Third, fBUT, CFS, and Schirmer I tests were performed. Finally, MG secretion was measured using MG evaluators. A ≥ 10-min intertest interval was set during which the patients were asked to rest with their eyes closed.
Statistics
All statistical analyses were performed using SPSS (version 24, IBM, Armonk, NY, USA) for Mac. A Kolmogorov–Smirnov test and P-P plot were used to assess the normality of the continuous variables. An independent samples t test was used to compare the parameters of the ST indicators and the demographic characteristics between the two groups. The chi-square test was used to compare the sex distribution between the two groups. Pearson’s rank-order correlation was used to identify the correlation between ST, BUT, OSDI, SPEED, MG secretion grading, and CFS. One-way ANOVA test was uesd to compare the values of four indicators of ST.
In order to investigate the reliability and efficacy of four indicators of ST, true positive rate and true negative rate were used and the chi-square test was used to compare the efficacy of four indicators of ST. The true positive rate is equal to true positive/(true positive + false negative) × 100%. The definition of true positive rate is the proportion of patients who are actually dry eye in the total number of patients who are just judged to be dry eye according to the criteria of test. The definition of patients who are actually dry eye is that their tear secretion is less than the cut-off.The true negative rate is equal to true negative/(true negative + false positive) × 100%. The true negative rate is the proportion of patients who are actually normal in the total number of persons who are just judged to be normal according to the criteria of test. The definition of normal person is that their tear secretion is more than the cut-off. The figures were created using SPSS and GraphPad Prism, version 8 (San Diego, CA). The datas are presented as mean ± standard deviation. p < 0.05 was considered statistically significant.
Results
Participants’ demographics and baseline characteristics
We included 360 eyes of 180 participants; of them, 240 eyes of 120 participants had DE and 120 eyes of 60 participants did not. Table 1 presents the participants’ baseline characteristics (age, sex, subjective questionnaires, and objective examinations). The objective examination results of NIBUT, fBUT, MG secretion grading, and CFS were 4.70 ± 2.28, 3.69 ± 2.22, 22.51 ± 11.68, and 0.88 ± 0.25, respectively, in the DE group and 8.43 ± 3.31, 4.22 ± 2.20, 16.32 ± 9.60, and 0.35 ± 0.06,respectively, in the ND group. The OSDI and SPEED scores were 30.12 ± 12.91 and 12.59 ± 4.63, respectively in the DE group and 6.62 ± 3.35 and 5.27 ± 2.87, respectively, in the ND group.Age was not significantly different between the two groups.Other DE-related indicators had significant differences between the two groups (p < 0.05). The normal and abnormal test results were in the Supplementary Table 1.
ST and DE group
Comparison among the different values of ST
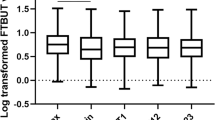
The four ST indicators were significantly different from each other in both groups. Figure 1 summarises four indicators of ST in the DE group. The values of ST1, 2-min ST, rear 3-min ST, and rear 4-min ST were 10.93 ± 6.30, 5.36 ± 4.63, 5.57 ± 2.11, and 7.21 ± 4.13, respectively, in the DE group. The four indicators were significantly different from each other (p < 0.01). Significant positive correlations were observed between ST1, 2-min ST, rear 3-min ST, and rear 4-min ST. The details about the relationships with the four indicators are listed in Table 2. We also recorded the ST results at each minute. However, we noticed a sign of tear secretion when the patients were performed ST. The speed of mean wetting per minute had been slowed down in ST. The speed was approximately 1.25–4.56 mm/min in the test, including in the DE and ND groups (Fig. 2). We observed that the speed of wetting paper in the first minute was unstable and casual in different participants. Therefore, we focused on the other indicators of ST, which removed the data from the first minute. We observed that the value of the rear of 4-min was approximately 3/5 of ST1.
Different values of ST and DE symptom questionnaires
We analysed the relationship between four indicators and DE symptom questionnaires. We observed that these indicators all had a correlation with the OSDI or SPEED. Table 3 presents the details. We observed that both ST1 and rear 4-min ST had relationships with the other indicators. As we expected, ST had a weak correlation with the questionnaire scores. However, the rear 4-min ST had a higher correlation with OSDI and SPEED than ST1.
Different values of ST and other DE examinations
The BUT was the most convenient diagnostic test used in clinical practice. The participants performed three consecutive fBUT tests and one-time NIBUT. In addition to BUT, MG secretion grading and CFS were performed. All four tests had statistical significance between the DE group and the ND group. However, we investigated the correlation between different values of ST and the other four tests. The results revealed the relationship between different ST and fBUT, MG secretion grading, and CFS in Table 3. In Table 3, we can see that the rear 4-min ST had a higher correlation with other examinations than the other three sorts of ST.
ST and non-DE group
The values of ST1, 2-min ST, rear 3-min ST, and rear 4-min ST were 11.84 ± 6.16, 8.25 ± 6.80, 2.73 ± 2.31, and 7.36 ± 3.42, respectively, in the ND group (Fig. 3). The four indicators were significantly different from each other (p < 0.01) in the ND group. The OSDI and SPEED scores were 6.62 ± 3.35 and 5.27 ± 2.87. Other DE tests, such as NIBUT, fBUT, MG secretion grading, and CFS, were 8.43 ± 3.31, 4.22 ± 2.20, 16.32 ± 9.60, and 0.35 ± 0.06, respectively. Table 4 shows the correlation between ST and other examinations in the ND group. We noticed the same sign in the ND group as in the DE group. The rear 4-min ST had the highest correlation with all examinations compared to the other three types of ST.
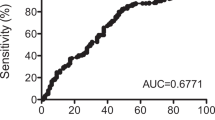
Rear 4-min ST may be a suitable supplement for DE diagnosis
To evaluate the four indicators in diagnosing DE, the true positive rate (TPR) was compared. The TPR of ST1, 2-min ST, rear 3-min ST, and rear 4-min ST was 101 eyes (42.08%), 75 eyes (31.25%), 68 eyes (28.33%), and 145 eyes (60.41%). We also calculated the true negative rate (TNR) in the ND group. We observed that the TNR of ST1, 2-min ST, rear 3-min ST, and rear 4-min ST was 50 eyes (41.67%), 47 eyes (39.17%), 48 eyes (40.00%), and 54 eyes (45.00%). The TPR of the four indicators showed a significant difference (p < 0.001). Based on the above results, we chose one indicator, rear 4-min ST, to be a reliable supplement for ST. We observed that the number of patients in theory whose tear secretions were less than 10 mm in 5 min accounted for 74.62% of people whose value of rear 4-min ST was lower than 6 mm. To provide the reference for the clinical diagnosis, we divided the patients into severe DE (ST ≤ 5 mm) and borderline DE (ST 5–10 mm). The value of tests in severe dry eye and borderline dry eye was in the supplementary Table 2. We compared rear 4-min ST with ST1 in subjective questionnaires and objective examinations. As shown in Table 5, the relationship between rear 4-min ST and other examinations in patients with severe DE was higher than that in patients with borderline DE. This means that in patients with severe DE, DE may be more easily diagnosed through the rear 4-min ST than classical ST.
Discussion
No consensus exists on the diagnostic criteria for DE in different areas, even though the International Dry Eye Workshop proposed the criteria for DE diagnosis. Most ocular examinations are not a perfect means to diagnose DE28, and suffer from low sensitivity and specificity in detecting symptoms. One of the major reasons may be the heterogeneity of DE. However, there is no single existing test to reliably diagnose DE, and two or three tests are often required, making the process time and labor intensive. Therefore, it is crucial to simplify the process and improve the accuracy of the tests.
ST is one of the most commonly used tests for assessing tear production ability due to its low cost and simplicity. However, the value of diagnosing DE has not yet been unified with the improvements of ST over decades. Jones’12 prospective of basal ST was that the cut-point should be set at 10 mm/5 min; however, Van Bijsterveld29 thought the length of wetting paper less than 5.5 mm should be defined as deficient aqueous production. A cutoff of 5.0 mm/5 min is recommended as meaningful4,30. Even though ST without topical anaesthesia may cause patients discomfort, we think that reflex tear secretion is an indispensable indicator.
ST is easily influenced by many factors, such as reflex tear, paper irritation, temperature, and humidity31,32. Therefore, doctors have strived to improve the accuracy of ST in clinical practice. Schulze suggested altering the ST to strip meniscometry because of its rapid performance of the procedure (5 s per eye)33. As we know, ST without topical anaesthesia may induce reflex tearing, and reflex tear secretion is unstable. To decrease the disadvantage of irritation of filter paper, a new strip named K-Schirmer was developed in Korea, and its reliability of repeated measurements was higher than ST34. In Vasileios Karampatakis' research, he compared the 2- and 5-min test and evaluated the reliability and the tear secretion of the Schirmer test I in 2 min15. In his study, he noticed that the speed of wetting paper slowed over time. And we saw a similar sign about the speed of wetting. During the initial 1 min, the speed of tear production was faster than in the next min; this phenomenon suggested an adaptation of the central nervous system16. Another reason was that a few remaining tears may exist in the low fornix. For that matter, the doctor should make sure that there are no tears before the test. However, we realised that the technique and process of dipping tears were not convenient for doctors and patients. In our study, we took the ST once as usual and recorded the values of each minute to determine the elements that may be more reliable for assessing tear secretion. Our study included both patients and normal people. Therefore, we had enough samples to verify whether our selected indicator really worked.
In the long term, ST is implemented only once in clinical practice. Only one test may impair the accuracy of the results and the validity of the test. To increase the accuracy of examinations, we should take care of more than one indicator. Telles suggested measuring several dynamic wetting lengths when we gauge human tear production35. Therefore, we selected four indicators: ST1, 2-min ST, rear 3-min ST, and rear 4-min ST. In our study, the ST values were consistent with the OSDI and SPEED. However, the relevance was low. This was consistent with a previous report36. At the same time, we valued ST with other examinations, such as BUT, MG secretion grading, and CFS. BUT is considered to be the most common statistical pattern to value the stability of tear film37. MG secretion grading is used to assess the extent of gland obstruction38. The fluorescein staining score is a test that values the environment of the cornea. Similar to the results above, ST was correlated to the fBUT and MG secretion grading in the DE group. Besides ST1, we noticed an interesting phenomenon: rear 4-min ST were correlated to the fBUT and MG secretion grading in the DE group. However, it was also correlated with the fBUT and MG secretion grading in the ND group. Finally, rear 4-min ST had higher TPRin diagnosing DE. It suggested that participants in our study, regardless of which group, rear 4-min ST may be a reliable indicator in assessing tear secretion. The reasons may include adaptation of irritation, the stable speed of tear secretion and reduction in the eye’s pain of patients. For doctors, it just needs a few seconds to record the value of the first minute and fifth minute of ST, and it is able to give reliable data to evaluate tear secretion. However, some participants may be sensitive about the paper and have massive tear secretion. These people do not fit this measurement and need other tests.
In conclusion, our study found that rear 4-min ST seemed to be a better assessment of tear production. Our data indicate that rear 4-min ST < 6 mm and 5-min ST < 10 mm likely indicates DE. One of the limitations of this study is that we did not account for the drainage and evaporation of tears.
References
Chen, W., Li, J. & Zheng, Q. Prevalence and risk factors of dry eye disease among a hospital-based population. Invest. Ophthalmol. Vis. Sci. 54, 935. https://doi.org/10.1097/ICL.0000000000000064 (2013).
Hashemi, H. et al. Prevalence of dry eye syndrome in an adult population. Clin. Exp. Ophthalmol. 42(3), 242–248. https://doi.org/10.1111/ceo.12183 (2014).
Phadatare, S. P., Momin, M., Nighojkar, P., Askarkar, S. & Singh, K. K. A comprehensive review on dry eye disease: Diagnosis, medical management, recent developments, and future challenges. Adv Pharm. 2015, 704946. https://doi.org/10.1155/2015/704946 (2015).
Craig, J. P. et al. TFOS DEWS II definition and classification report. Ocul. Surf. 15(3), 276–283. https://doi.org/10.1016/j.jtos.2017.05.008 (2015).
King-Smith, P. E., Begley, C. G. & Braun, R. J. Mechanisms, imaging and structure of tear film breakup. Ocul. Surf. 16(1), 4–30. https://doi.org/10.1016/j.jtos.2017.09.007 (2018).
Bandeen-Roche, K., Muñoz, B., Tielsch, J. M., West, S. K. & Schein, O. D. Self-reported assessment of dry eye in a population-based setting. Invest. Ophthalmol. Vis. Sci. 38(12), 2469–2475 (1997).
Saleh, T. A., McDermott, B., Bates, A. K. & Ewings, P. Phenol red thread test vs. Schirmer’s test: A comparative study. Eye (London). 20(8), 913–935. https://doi.org/10.1038/sj.eye.6702052 (2006).
Bawazeer, A. M. & Hodge, W. G. One-minute Schirmer test with anesthesia. Cornea 22(4), 285–287. https://doi.org/10.1097/00003226-200305000-00001 (2003).
Feenstra, R. P. G. & Tseng, S. C. G. Comparison of fluorescein and rose bengal staining. Ophthalmology 99(4), 605–617. https://doi.org/10.1016/s0161-6420(92)31947-5 (1992).
García-Resúa, C., Santodomingo-Rubido, J., Lira, M., Giraldez, M. J. & Vilar, E. Y. Clinical assessment of the lower tear meniscus height. Ophthalmic. Physiol. Opt. 29(5), 487–496. https://doi.org/10.1111/j.1475-1313.2009.00634x (2009).
Schirmer, O. Studien zur Physiologie und Pathologie der Tranenabsonderung und Tranenabfuhr. Graefes Arch Clin Exp Ophthalmol. 56, 197–291 (1903).
Jones, L. T. The lacrimal secretory system and its treatment. Am. J. Ophthalmol. 62(1), 47–60. https://doi.org/10.1016/0002-9394(66)91676-x (1966).
Masmali, A., Alqahtani, T. A., Alharbi, A. & El-Hiti, G. A. Comparative study of repeatability of phenol red thread test versus schirmer test in normal adults in Saudi Arabia. Eye Contact Lens. 40(3), 127–131. https://doi.org/10.1097/ICL.0000000000000025x (2014).
Halberg, G. P. & Behrens, C. Standardized Schirmer tear test kit. Am. J. Ophthalmol. 51, 840–842. https://doi.org/10.1016/0002-9394(61)91827-x (1963).
Karampatakis, V., Karamitsos, A., Skriapa, A. & Pastiadis, G. Comparison between normal values of 2- and 5-minute schirmer test without anesthesia. Cornea 29(5), 497–501. https://doi.org/10.1097/ICO.0b013e3181c2964c (2010).
Rhoades, R. A. & Tanner, G. A. Medical Physiology (Lippincott, Williams & Wilkins, Philadelphia, 2003).
The epidemiology of dry eye disease: Report of the Epidemiology Subcommittee of the International Dry Eye Work Shop (2007). Ocul. Surf. 5(2):93–107. https://doi.org/10.1016/s1542-0124(12)70082-4 (2007).
Schiffman, R. M. et al. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 118(5), 615–621. https://doi.org/10.1001/archopht.118.5.615 (2000).
Fu, Y. et al. Prospective trial of a 2940 nm Er:YAG laser for the treatment of meibomian gland dysfunction. Graefes Arch. Clin. Exp. Ophthalmol. 259(8), 2269–2278. https://doi.org/10.1007/s00417-021-05170-8 (2021).
Fan, F., Li, X., Li, K. & Jia, Z. To find out the relationship between levels of glycosylated hemoglobin with meibomian gland dysfunction in patients with type 2 diabetes. Ther. Clin. Risk Manag. 17, 797–807. https://doi.org/10.2147/TCRM.S324423 (2021).
Ngo, W. et al. Psychometric properties and validation of the Standard Patient Evaluation of Eye Dryness questionnaire. Cornea 32(9), 1204–1210. https://doi.org/10.1097/ICO.0b013e318294b0c0 (2013).
Asiedu, K. et al. Ocular surface disease index (OSDI) versus the standard patient evaluation of eye dryness (SPEED): A study of a nonclinical sample. Cornea 35(2), 175–180. https://doi.org/10.1097/ICO.0000000000000712 (2016).
Lu, F. et al. Evaluation of reliability and validity of three common dry eye questionnaires in Chinese. J. Ophthalmol. 27, 2401213. https://doi.org/10.1155/2018/2401213 (2018).
Serin, D., Karsloğlu, S., Kyan, A. & Alagöz, G. A Simple approach to the repeatability of the schirmer test without anesthesia: Eyes open or closed?. Cornea 26(8), 903–906. https://doi.org/10.1097/ICO.0b013e3180950083 (2007).
Vashisht, S. & Singh, S. Evaluation of phenol red read test versus Schirmer test in dry eyes: A comparative study. Int. J. Appl. Basic Med. Res. 1(1), 40–42. https://doi.org/10.4103/2229-516X.81979 (2011).
Kashkouli, M. B. et al. Subjective versus objective dry eye disease in patients with moderate-severe thyroid eye disease. Ocul. Surf. 16(4), 458–462. https://doi.org/10.1016/j.jtos.2018.07.003 (2018).
Sang, X. et al. Lipid layer thickness and tear meniscus height measurements for the differential diagnosis of evaporative dry eye subtypes. Int. J. Ophthalmol. 11(9), 1496–1502. https://doi.org/10.18240/ijo.2018.09.11 (2018).
Lin, P. Y. et al. Association between symptoms and signs of dry eye among an elderly Chinese population in Taiwan: The Shihpai Eye Study. Invest. Ophthalmol. Vis. Sci. 46(5), 1593–1598. https://doi.org/10.1167/iovs.04-0864 (2005).
Van Bijsterveld, O. P. Diagnostic tests in the sicca syndrome. Arch Ophthalmol. 82(1), 10–14. https://doi.org/10.1001/archopht.1969.00990020012003 (1969).
Danjo, Y. Diagnostic usefulness and cutoff value of Schirmer’s I test in the Japanese diagnostic criteria of dry eye. Graefes Arch. Clin. Exp. Ophthalmol. 235(12), 761–766. https://doi.org/10.1007/BF02332860 (1997).
Kallarackal, G. U. et al. A comparative study to assess the clinical use of fluorescein meniscus time (FMT) with tear break up time (TBUT) and Schirmer’s tests (ST) in the diagnosis of dry eyes. Eye (London). 16(5), 594–600. https://doi.org/10.1038/sj.eye.6700177 (2002).
Tsubota, K. The importance of the Schirmer test with nasal stimulation. Am. J. Ophthalmol. 111(1), 106–108. https://doi.org/10.1016/s0002-9394(14)76908-9 (1991).
Schulze, K., Großjohann, R., Paul, S., Bossaller, L. & Tost, F. Schirmer’s test and strip meniscometry : Comparative consideration in the diagnostics of dry eye. Ophthalmologe. 118(6), 561–568. https://doi.org/10.1007/s00347-020-01208-0 (2021).
Park, J. E. et al. Development of K-Schirmer strip and evaluation of clinical availability. Korean J. Vis. Sci. 20(1), 37–47. https://doi.org/10.17337/JMBI.2018.20.1.37 (2018).
Telles, R., Li, W., Dursch, T. J., Lin, M. C. & Radke, C. J. Human tear-production rate from closed-eye Schirmer-strip capillary dynamics. Colloids Surfaces A Physicochem. Eng. Aspects. 521, 61–68. https://doi.org/10.1016/j.colsurfa.2016.08.027 (2017).
Samuel, K. et al. Association between dry eye symptoms and signs. J. Curr. Ophthalmol. 30(4), 321–325. https://doi.org/10.1016/j.joco.2018.05.002 (2018).
Mcmonnies, C. W. Tear instability importance, mechanisms, validity and reliability of assessment. J. Optom. 11(4), 203–210. https://doi.org/10.1016/j.optom.2017.11.004 (2018).
Pucker, A. D. & Nichols, J. J. Analysis of meibum and tear lipids. Ocul Surf. 10(4), 230–250. https://doi.org/10.1016/j.jtos.2012.07.004 (2012).
Funding
This study was funded by Xiaodan Huang (2020C03035).
Author information
Authors and Affiliations
Contributions
Conception and design: X.J., X.W. Provision of study materials or patients: X.F. Collection and assembly of data: X.W., Y.W., Y.M., J.M. Data analysis and interpretation: X.W. Manuscript writing: X.W. Final version of the manuscript: All authors. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Fan, X., Wu, Y. et al. Rear 4-min Schirmer test, a modified indicator of Schirmer test in diagnosing dry eye. Sci Rep 12, 6272 (2022). https://doi.org/10.1038/s41598-022-09791-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09791-9
- Springer Nature Limited
This article is cited by
-
New advances in medical management of dry eye: optimizing treatment strategies for enhanced relief
International Ophthalmology (2024)