Abstract
The cause of idiopathic sudden sensorineural hearing loss (idiopathic SSNHL)—diagnosed after excluding other causes of hearing loss, such as SSNHL associated with vestibular schwannoma (VS)—is unknown. The presumed pathogenesis of idiopathic SSNHL includes circulatory disorders (e.g., cochlear infarction). We tested the hypothesis that patients with SSNHL who are at high stroke risk will have a lower rate of VS compared to those with low stroke risk. The rationale is that the primary cause of SSNHL in patients with high stroke risk might be a circulatory disturbance. We conducted a retrospective study in six hospitals. Our sampling of SSNHL patients included those diagnosed with idiopathic SSNHL and VS-associated SSNHL. SSNHL patients who had a head MRI were stratified by severity of hearing loss and evaluated for differences in the detection rate of VS between the high-scoring CHADS2 (CHADS2-H-), an index of stroke risk, and low-scoring CHADS2 (CHADS2-L-) groups. We identified 916 patients who met the inclusion criteria. For severe hearing loss, the CHADS2-H group had a significantly lower rate of VS than the CHADS2-L group (OR 0 [95% CI 0.00–0.612]; P = 0.007). These results indirectly support the hypothesis that a primary cause of severe idiopathic SSNHL in those at high risk of stroke might be a circulatory disorder.
Similar content being viewed by others
Introduction
Idiopathic sudden sensorineural hearing loss (idiopathic SSNHL) is an abruptly appearing hearing loss that severely affects the quality of life of 11–77 per 100,000 people per year1. The hearing loss is often permanent and can be mild, total, or somewhere in between in severity. Idiopathic SSNHL is usually diagnosed after excluding other causes of SSNHL, such as vestibular schwannoma (VS). Although the exact cause of idiopathic SSNHL remains unknown, circulatory disorders, such as cochlear infarction, have been implicated in its pathogenesis2. This idea is consistent with findings from large cohort studies supporting the association of idiopathic SSNHL and stroke3,4. Moreover, comorbidities such as vertigo or dizziness and factors that increase risk of atherosclerosis, such as aging, diabetes mellitus, and history of cardiac disease, are reported to contribute to the severity of idiopathic SSNHL5,6. Despite these findings, there is still no definitive evidence that circulatory disturbances can cause idiopathic SSNHL.
SSNHL can be associated with a VS7. The prevalence of VS in patients with SSNHL is reported to be 0.8–3.7%8. Therefore, differentiation of retrocochlear pathology is necessary in the diagnosis of idiopathic SSNHL, and it is recommended that MRI or an auditory brainstem response test be conducted9,10.
Taken together, we formulated a hypothesis based on the following three steps. First, circulatory disturbances might be the primary cause of SSNHL in patients with high risk for stroke. Second, the cause of severe SSNHL in patients with high risk for stroke is even more likely to be circulatory disturbances, because a high risk of atherosclerosis contributes to the severity of SSNHL5,6. Third, therefore, severe SSNHL in patients at high risk of stroke are relatively less likely to have SSNHL caused by VS. In other words, we hypothesized that patients with severe SSNHL who are at high risk for stroke might have a lower rate of VS than those who are at low risk for stroke.
The CHADS2 score is one method for assessing stroke and atherosclerosis risk in patients with non-rheumatic atrial fibrillation11. CHADS2 is essentially a set of clinical prediction rules for estimating risk. CHADS2 stands for Congestive heart failure, Hypertension, Age, Diabetes mellitus, and S2 for prior stroke or transient ischemic attack. The CHADS2 score may be useful also as a predictor of cardiovascular/cerebrovascular events in patients with coronary artery disease lacking atrial fibrillation and as a prognosticator for patients with acute myocardial infarction12,13.
Thus, the present study tested this hypothesis by comparing the rate of VS in patients with SSNHL, who were stratified by CHADS2 score and severity of hearing loss. We then estimated the population of idiopathic SSNHL patients who are at risk for stroke and atherosclerosis by using CHADS2 scores and severity of hearing loss.
Methods
We conducted a retrospective chart review of patients treated at six tertiary hospitals in Japan as part of the Keio Academical Otolaryngology Research Unit (KAORU) Project7. Patients diagnosed with SSNHL and who had undergone a head MRI in the departments of otolaryngology and head and neck surgery were eligible. Data were collected from the medical records of patients at the following hospitals and from the indicated time periods: Keio University Hospital between January 2012 and March 2020; National Hospital Organization Tokyo Medical Center between January 2012 and December 2019; Saiseikai Utsunomiya Hospital between January 2016 and November 2018; Japanese Red Cross Shizuoka Hospital between January 2014 and June 2019; Kawasaki Municipal Hospital between April 2016 and March 2020; and Hiratsuka City Hospital between January 2012 and December 2019.
Our sampling of SSNHL patients included those diagnosed with idiopathic SSNHL and VS-associated SSNHL. Idiopathic SSNHL was defined using the criteria of the Sudden Deafness Research Committee of the Ministry of Health, Labour and Welfare (MHLW), Japan (2015) (Table 1)14. VS-associated SSNHL was also defined according to these criteria, except for cases listed having an “unknown etiology” as main symptoms.
Relevant data we collected were patient age, sex, affected ear (side), pure tone audiogram (PTA), presence of vertigo or dizziness symptoms, VS diagnosed by MRI; comorbidities (diabetes mellitus, hypertension, stroke/transient ischemic attack (TIA), congestive heart failure, vascular disease [e.g., myocardial infarction, angina pectoris, peripheral artery disease, aortic plaque], thromboembolism, hyperlipidemia, atrial fibrillation); and CHADS2 score. Scoring for CHADS2 was done by a physician; 1 point was assigned each for congestive heart failure, hypertension, age ≥ 75 years, or diabetes, and 2 points were assigned each for previous stroke and/or TIA11.
We excluded from analysis any patients diagnosed with bilateral simultaneous onset SSNHL. The first SSNHL post-onset PTA with complete values was used for analysis. The severity of PTA, which is the arithmetic mean of five hearing frequencies (250, 500, 1000, 2000, and 4000 Hz), was graded according to the criteria defined by the MHLW: Grade 1: PTA < 40 dB; Grade 2: 40 dB ≤ PTA < 60 dB; Grade 3: 60 dB ≤ PTA < 90 dB; and Grade 4: 90 dB ≤ PTA14.
For the first analysis, we classified SSNHL patients by presence/absence of VS and evaluated the two groups statistically according to various demographic and clinical characteristics. A receiver operating characteristic (ROC) curve was calculated with the CHADS2 scores for presence/absence of VS. The best cutoff value was determined using the Youden index15. With the ROC curve and Youden index analysis, we could identify the optimal cutoff value(s) that produced the best tradeoff between sensitivity and specificity.
Next, the patients were classified into a mild hearing-loss group (Grades 1 and 2) or a severe hearing-loss group (Grades 3 and 4). We evaluated the contribution of various risk factors for stroke and arteriosclerosis on the severity of SSNHL.
Finally, the patients were stratified by severity of hearing loss and evaluated for differences in the detection rate of VS between the CHADS2-H- and CHADS2-L-scoring groups.
The t-test and Fisher’s exact test were used for statistical analyses, as appropriate. P < 0.05 was defined as a statistically significant. We used EZR statistical software (Saitama Medical Center, Jichi Medical University, Saitama, Japan) for all analyses16. All methods of the present study were carried out in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement17.
All procedures were approved by the institutional review boards (IRBs) of the participating hospitals (IRB approval number): Keio University School of Medicine (20200033), National Hospital Organization Tokyo Medical Center (R20-046), Saiseikai Utsunomiya Hospital (2020-19), Japanese Red Cross Shizuoka Hospital (2020-15), Kawasaki Municipal Hospital (2020-9), and Hiratsuka City Hospital (02-003). The requirement of written informed consent was waived by the IRBs of Keio University School of Medicine, National Hospital Organization Tokyo Medical Center, Saiseikai Utsunomiya Hospital, Japanese Red Cross Shizuoka Hospital, Kawasaki Municipal Hospital, and Hiratsuka City Hospital, because of the retrospective design.
Results
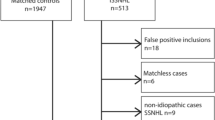
We identified 916 SSNHL patients (426 men [46.5%], 490 women [53.5%]) who met the inclusion criteria. Mean age ± standard deviation (SD) at the time of the initial examination was 59.4 ± 15.4 years.
Table 2 shows the demographic and clinical characteristics of included patients with SSNHL, stratified by presence/absence of VS. SSNHL patients with VS and those without VS showed no significant differences across any of their demographic and clinical characteristics. Using ROC curve analysis, we determined that the optimal cutoff values for the CHADS2 score were at two points (CHADS2-H, CHADS2-L) on the specificity-sensitivity curve. The area under the curve (AUC) was 0.551 (95% confidence interval (CI), 0.487–0.616). This categorization of CHADS2 scores into low and high groups by cutoff value has been reported in several reports11,13. We found no significant difference in the rate of CHADS2-H and CHADS2-L between SSNHL patients with VS and those without VS (p = 0.06) (odds ratio (OR), 0.38 [95% CI 0.099–1.066]).
Table 3 shows summaries of the analysis of patient characteristics associated with severity of SSNHL. We found no significant difference in the rate of VS between the Grade 1–2 severity group and Grade 3–4 severity group (p = 0.40) (OR 0.77 [95% CI 0.421–1.400]). Patients in the Grade 3–4 group were significantly older; had more vertigo or dizziness symptoms; were more likely to have diabetes mellitus, hypertension, congestive heart failure, vascular disease, and/or atrial fibrillation; and had higher CHADS2 scores compared with patients in the Grade 1–2 group.
Figure 1 shows the prevalence of VS in SSNHL patients, stratified by the severity of hearing loss and CHADS2 score. The CHADS2-H group had a lower prevalence rate of VS than the CHADS2-L group, although this difference was not statistically significant (p = 0.06) (OR, 0.38 [95% CI 0.099–1.066]). However, in the Grade 3–4 group, the CHADS2-H group had a significantly lower prevalence rate of VS than the CHADS2-L group (p = 0.007) (OR, 0 [95% CI 0.00–0.612]). In the Grade 1–2 group, CHADS2-H and CHADS2-L participants were statistically indistinguishable regarding rate of VS (p = 1) (OR 1.06 [95% CI 0.258–3.216]).
Discussion
Idiopathic SSNHL is an abruptly appearing and disabling inner ear disorder that presents mostly unilaterally. The pathogenesis of idiopathic SSNHL has not been identified. VS, viral infection (e.g. mumps virus), intralabyrinthine hemorrhage and rupture of the labyrinthine window have been reported as causes of SSNHL7,18,19,20. Previous studies have suggested that risk factors for cerebrovascular and cardiovascular disease can also be considered risk factors for idiopathic SSNHL21,22. Although previous studies have provided evidence for the hypothesis that idiopathic SSNHL is caused by a circulatory disturbance2,3,4, like cochlear infarction, no definitive conclusions have been reached. In the present study, we evaluated associations of stroke and atherosclerosis risk using patients’ CHADS2 scores and tested whether the rate of VS in SSNHL patients differed systematically according to CHADS2 score. Our aim was to determine the population of idiopathic SSNHL patients who had higher stroke and atherosclerosis risk by excluding from analysis SSNHL patients with VS.
We had two main findings. First, we found an association between CHADS2 scores and severity of hearing loss in SSNHL patients. CHADS2 scores of SSNHL patients with Grade 1–2 hearing loss were significantly different from those with Grade 3–4 hearing loss. Other significant differences were found in proportion with vertigo/dizziness; age; and comorbidities (diabetes mellitus, hypertension, congestive heart failure, vascular disease, and atrial fibrillation). These results suggest that patients with Grade 3–4 hearing loss severity were more likely to have higher risk factors for stroke/atherosclerosis, which is consistent with previous reports5,6. Furthermore, when stratifying SSNHL patients by hearing-loss grade and CHADS2 score, participants in the CHADS2-H group with Grade 3–4 severity were significantly less likely to have a VS than those Grade 3–4 severity participants in the CHADS2-L group. Indeed, no VS was detected in Grade 3–4 patients with high risk factors for stroke/atherosclerosis. This may be an important result to more clearly define the population of idiopathic SSNHL patients associated with stroke and atherosclerosis risk.
Second, the rate of VS in SSNHL patients was 5.8%, which was slightly higher than previously reported8. We speculate that this is because the criteria defined by the MHLW in Japan are strictly applied in the diagnosis of idiopathic SSNHL. In the present study, patients with acute low-frequency sensorineural hearing loss (ALHL) limited to 125 to 500 Hz were excluded. A past report indicates that the rate of VS in ALHL cases is lower than the rate of VS in all SSNHL cases23,24. In other words, the exclusion of SSNHL patients who did not meet this criterion, such as ALHL cases limited to 125 to 500 Hz, may have resulted in a slightly higher VS rate. Some reports suggest that all cases of SSNHL should be screened for VS by MRI25. However, our present results suggest that MRI screening for SSNHL of patients with a CHADS2 score of ≥ 2 accompanied by Grade 3–4 severity might not have higher priority. This population accounted for 10.6% of the SSNHL patients (97/916 cases).
The present study has three possible limitations. First, the study is retrospective, and therefore may have selection bias and information bias. Second, the factors and risks of VS are still largely unknown and could not be adjusted for in the analysis. Third, idiopathic SSNHL itself is a disorder whose pathogenesis is still unknown.
The present study also had at least two strengths. First, it was a multicenter study with a relatively large number of patients. Second, for the first time, our analysis allowed an indirect estimate of the presumed population of SSNHL patients associated with stroke and atherosclerosis risk according to severity of hearing loss and CHADS2 score.
In conclusion, patients with severe hearing loss (Grade 3–4) and high CHADS2 scores had a significantly lower rate of VS than SSNHL patients with low CHADS2 scores. By process of elimination, this suggests that the cause of severe idiopathic SSNHL in individuals at high risk of stroke and atherosclerosis might be a circulatory disorder. Thus, when determining whether the severe hearing loss in a patient is due to idiopathic SSNHL, clinicians should calculate the patient’s CHADS2 score and then decide whether the patient should undergo an MRI to rule out VS. If the CHADS2 score is high, the patient should undergo whole brain MRI and/or MR angiography. We hypothesize that the cause of severe SSNHL in patients with a high risk for stroke/atherosclerosis is a circulatory disturbance, which we will evaluate in the near future.
Data availability
The data analysed during this study are available from the corresponding author upon reasonable request.
References
Alexander, T. H. & Harris, J. P. Incidence of sudden sensorineural hearing loss. Otol. Neurotol. 34, 1586–1589 (2013).
Rasmussen, H. Sudden deafness. Acta Otolaryngol. 37, 65–70 (1949).
Kim, S. Y., Lim, J. S., Sim, S. & Choi, H. G. Sudden sensorineural hearing loss predicts ischemic stroke: A longitudinal follow-up study. Otol Neurotol. 39, 964–969 (2018).
Kim, J. Y., Hong, J. Y. & Kim, D. K. Association of sudden sensorineural hearing loss with risk of cardiocerebrovascular disease: A study using data from the Korea National Health Insurance Service. JAMA Otolaryngol. Head Neck Surg. 144, 129–135 (2018).
Kitoh, R. et al. Nationwide epidemiological survey of idiopathic sudden sensorineural hearing loss in Japan. Acta Otolaryngol. 137, S8–S16 (2017).
Fukui, M. et al. Idiopathic sudden hearing loss in patients with type 2 diabetes. Diabetes Res. Clin. Pract. 63, 205–211 (2004).
Wasano, K. et al. Sudden sensorineural hearing loss in patients with vestibular schwannoma. Sci. Rep. 11, 1624 (2021).
Friedman, R. A., Kesser, B. W., Slattery, W. H. 3rd., Brackmann, D. E. & Hitselberger, W. E. Hearing preservation in patients with vestibular schwannomas with sudden sensorineural hearing loss. Otolaryngol. Head Neck Surg. 125, 544–551 (2001).
Stachler, R. J. et al. Clinical practice guideline: Sudden hearing loss. Otolaryngol. Head Neck Surg. 146, S1-35 (2012).
Chandrasekhar, S. S. et al. Clinical practice guideline: Sudden hearing loss (update). Otolaryngol. Head Neck Surg. 161, S1–S45 (2019).
Gage, B. F. et al. Validation of clinical classification schemes for predicting stroke: Results from the National Registry of Atrial Fibrillation. JAMA 285, 2864–2870 (2001).
Huang, S. S. et al. Usefulness of the CHADS2 score for prognostic stratification of patients with acute myocardial infarction. Am. J. Cardiol. 114, 1309–1314 (2014).
Tabata, N. et al. Prognostic value of the CHADS2 Score for adverse cardiovascular events in coronary artery disease patients without atrial fibrillation-a multi-center observational cohort study. J. Am. Heart Assoc. 6, e006355 (2017).
Nakashima, T. et al. Idiopathic sudden sensorineural hearing loss in Japan. Acta Otolaryngol. 134, 1158–1163 (2014).
Youden, W. J. Index for rating diagnostic tests. Cancer 3, 32–35 (1950).
Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 48, 452–458 (2013).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. The Lancet 370, 1453–1457 (2007).
Cohen, B. E., Durstenfeld, A. & Roehm, P. C. Viral causes of hearing loss: A review for hearing health professionals. Trends Hear 18, 233126514541361 (2014).
Lee, J. W. et al. Clinical features and prognosis of sudden sensorineural hearing loss secondary to intralabyrinthine hemorrhage. J. Audiol. Otol. 20, 31–35 (2016).
Nagai, T. & Nagai, M. Labyrinthine window rupture as a cause of acute sensorineural hearing loss. Eur. Arch. Otorhinolaryngol. 269, 67–71 (2012).
Kuo, C. L., Shiao, A. S., Wang, S. J., Chang, W. P. & Lin, Y. Y. Risk of sudden sensorineural hearing loss in stroke patients: A 5-year nationwide investigation of 44,460 patients. Medicine 95, e4841 (2016).
Aimoni, C. et al. Diabetes, cardiovascular risk factors and idiopathic sudden sensorineural hearing loss: A case-control study. Audiol. Neurootol. 15, 111–115 (2010).
Hosokawa, K., Hosokawa, S., Takebayashi, S. & Mineta, H. Trough-shaped audiograms are common in patients with acoustic neuroma and sudden sensorineural hearing loss. Audiol. Neurootol. 23, 58–62 (2018).
Suzuki, M., Hashimoto, S., Kano, S. & Okitsu, T. Prevalence of acoustic neuroma associated with each configuration of pure tone audiogram in patients with asymmetric sensorineural hearing loss. Ann. Otol. Rhinol. Laryngol. 119, 615–618 (2010).
Sauvaget, E., Kici, S., Kania, R., Herman, P. & Tran Ba Huy, P. Sudden sensorineural hearing loss as a revealing symptom of vestibular schwannoma. Acta Otolaryngol. 125, 592–595 (2005).
Acknowledgements
We thank Prof. Kengo Nagashima for his advice on statistical analysis.
Funding
This work was supported by Grant-in-Aid for Clinical Research from the National Hospital Organization (H31-NHO(kankaku)-01).
Author information
Authors and Affiliations
Contributions
All authors contributed to the revision and approval of the final version of this paper. N.T. and K.W. contributed to the conception, study design, data acquisition, statistical analysis, and interpretation of the data, and first draft of this manuscript. N. O., K. H., M. S., T. N., Y. H., and S. S. contributed to data acquisition. K. O. contributed to the study design.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsuzuki, N., Wasano, K., Oishi, N. et al. Severe sudden sensorineural hearing loss related to risk of stroke and atherosclerosis. Sci Rep 11, 20204 (2021). https://doi.org/10.1038/s41598-021-99731-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99731-w
- Springer Nature Limited