Abstract
Studies on the effects of dual tasking in patients with chronic inflammatory rheumatic diseases are limited. The aim of this study was to assess dual tasking while walking in patients with axial spondyloarthritis (axSpA) in comparison to healthy controls. Thirty patients with axSpA and thirty healthy controls underwent a 10-m walk test at a self-selected comfortable walking speed in single- and dual-task conditions. Foot-worn inertial sensors were used to compute spatiotemporal gait parameters. Analysis of spatiotemporal gait parameters showed that the secondary manual task negatively affected walking performance in terms of significantly decreased mean speed (p < 0.001), stride length (p < 0.001) and swing time (p = 0.008) and increased double support (p = 0.002) and stance time (p = 0.008). No significant interaction of group and condition was observed. Both groups showed lower gait performance in dual task condition by reducing speed, swing time and stride length, and increasing double support and stance time. Patients with axSpA were not more affected by the dual task than matched healthy controls, suggesting that the secondary manual task did not require greater attention in patients with axSpA. Increasing the complexity of the walking and/or secondary task may increase the sensitivity of the dual-task design to axial spondyloarthritis.
Similar content being viewed by others
Introduction
Walking while concurrently performing motor and/or cognitive tasks, such as carrying an object, talking with someone, calling or texting on a smartphone, or other attention-demanding tasks, is the norm rather than the exception during everyday life1. Maintaining a safe, stable and efficient gait pattern under such dual task conditions relies on the successful interaction between neural mechanisms that regulate balance and gait control and those that regulate the execution of concurrent motor and/or cognitive task2.
There is a plethora of literature reporting that gait pattern is adversely affected during dual-task walking. This is the case for young healthy individuals2,3,4,5,6, who generally presented reduced gait speed, shorter stride length, and increased time spent in double limb support in dual-task walking condition compared to single-task walking condition., The negative effect of dual tasks on gait is greater in older adults (e.g., see for reviews7,8,9,10) and patients populations (patients with neurologic disorders (e.g., see for review11,12,13,14), suggesting that walking requires greater cognitive resources in these populations versus young and/or healthy adults. At this point, it is important to mention that interpreting changes in dual-task walking performance is rather difficult15. It is indeed recognised that dual-task interference during walking does depend on a wide variety of factors (e.g., see for reviews8,10,12,15), including among others the gait capabilities of the individuals. In fact, what the above mentioned older adults and patient populations seem to have in common is gait disorders. For instance, compared to young adults, older adults walked with slower walking, with shorter steps and prolonged double support (see for review16). These age-related changes in spatiotemporal gait parameters are recognised as indicating as the adoption of a more conservative or less destabilising gait, to avoid falls and/or reduce the energetic cost of mobility16. Note that this so-called “cautious gait pattern” has also been observed in patients with neurologic disorders (patients after a stroke17, patients with sensory or cerebellar ataxia18, patients with subcortical disequilibrium19).
To the best of our knowledge, no studies have examined dual-task walking in patients with chronic inflammatory rheumatic diseases. However, recent studies have reported similar gait disorders in patients with axSpA20 than those observed in the above-mentioned older and patient populations9,17,18,19,21,22. Along these lines, considering also as others7,8,9,10,11,12,13,14 that dual task paradigms can provide important insights into the interactions between cognition and the control of walking, the purpose of this study was to assess dual tasking while walking in patients with axSpA in comparison to healthy matched controls.
We hypothesized that (1) the concurrent performance of a secondary manual task would negatively affect spatiotemporal gait parameters during walking (hypothesis 1), and (2) spatiotemporal gait parameters would be more affected by dual-tasking in patients with axSpA as compared to healthy matched controls (hypothesis 2).
Methods
Study design
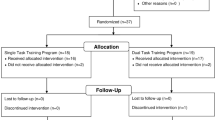
The present study takes part of a larger prospective study called “FOLOMI (Function, Locomotion, Measurement, Inflammation)”23, registered in Clinical Trials (NCT03761212), which has been approved by local ethic committee CPP Ile De France 1, RCB: 2017-A03468-45, date of agreement: July 17th, 2018, Last version: V6.0, June 17th, 2020). All research was performed in accordance with the relevant guidelines and regulations. Written signed informed consent was required for all participants of the study to participate in the FOLOMI prospective study23.
Data of the present study for the single task condition have been already presented in a previous publication20. These data are included only as reference for the dual task walking condition, insofar as the present study focused on the effects of a secondary task on spatiotemporal gait parameters in axSpA. Dual task data have not been published previously in any form.
Participants
To calculate the number of subjects required for this study, we used results presented in Zebouni et al. study24 regarding stride length differences between patients and healthy controls. With a standard deviation of 0.12 and an expected difference of 0.14, and a significance level and a power set respectively at 0.05 and 80%, sample size was estimated at 12 in each group using Sample Size Calculator25,26 and was brought to 30 to allow the use of parametric tests.
The first thirty patients with axSpA included in FOLOMI study were age and sex matched to thirty healthy controls. Inclusion and non-inclusion criteria are listed in Table 123.
Clinical characteristics of the participants
Clinical characteristics including age, sex, weight, height and pain intensity were gathered for both patients with axSpA and healthy controls by the same observer (JS)23.
Disease duration from diagnosis, morning stiffness, the Bath Ankylosing Spondylitis Functional Index (BASFI)27, the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI)27 and treatments were collected for patients with axSpA only23.
Experimental protocol
A 10-m walk test was performed at comfortable walking speed28 in single- and dual-task conditions (3 trials per condition). For the dual-task condition, participants had to walk at comfortable speed and to carry a full cup of water in their dominant hand with the instruction to “perform both tasks as well as possible”29,30. Performance of the secondary task was assessed by the examiner who noted whether there was any spillage of water30. We decided to use a manual task for the same reasons as those recently explained by Kwon et al. in 20195: “there are more situations that require manual dual task than cognitive dual task in daily living”5(p2). Among different manual tasks (carrying a cup, carrying a tray, carrying a tray and a cup), carrying a cup was considered as “more challenging” and related to risk of falling31. Thus, carrying a cup is an ecological dual-task, which is commonly performed in daily life5,31,32,33 and is quickly assessed (i.e. there is no requirement to listen/analyse to the records after the execution of the dual task34,35) which provides it high usability in clinical practice.
Participants had to wear walking shoes and 2 inertial measurements units (IMUs) with tri-axial accelerometers and gyroscopes (Physilog5, 200 Hz, BioAGM, Gait Up, CH) were placed above both feet (behind the base of the fifth metatarsal)36 (Fig. 1). The two first and last steps were removed from the analysis37,38 and at least 16 steps were included in the analysis. Gait assessments were performed by the same examiner (JS). For patients with axSpA, assessments were planned at least 2 h from the end of morning stiffness in relationship with possible consequences of morning stiffness on functional limitations39.
Gait outcomes
Spatiotemporal gait parameters were calculated from IMUs (Physilog 5) signals using the Gait Analysis Software (Gait Up, CH, V5.3.0). Means of right and left feet values were computed after checking for non-significant differences between left and right feet. The means of the second and the third trials was calculated for each of the following spatiotemporal gait parameters40:
-
Speed (m s−1): Mean walking stride velocity of forward walking
-
Cadence (step/minute): Number of steps in a minute
-
Stride length (m): Distance between two consecutive footprints on the ground, from the heel of a foot to the heel of the same foot, one cycle after
-
Swing time (%): Portion of the cycle during which the foot is in the air and does not touch the ground
-
Stance time (%): Portion of the cycle during which part of the foot touches the ground
-
Double support time (%): Portion of the cycle where both feet touch the ground
Data analysis
Statistical analysis was performed using SPSS 20 (IBM) and Microsoft Excel.
To compare clinical characteristics between patients with axSpA and healthy controls, independent sample t-tests were performed for height, weight and pain intensity. Independent sample t-tests were used to compare performances of the secondary manual task.
To examine the effects of condition and group on spatiotemporal gait parameters, repeated measures analyses of variance (RM-ANOVA) were conducted with within factor being condition (single- or dual-task condition) and between factor being the group (healthy controls or patients with axSpA). From each comparison, 95% confidence intervals (CI) were calculated and effect sizes were computed using partial Eta-squared (η2) which was calculated as the ratio of the effect variance to the total variance. A partial η2 value of 0.45 means that the independent variable has 45% effect on the dependent variable outcome. The significance of the p value was set at 0.05.
Results
Study population
The population included in the present study is the same that has been presented in a previous publication and is presented in Table 220.
Mean disease axSpA duration was of 11.77 ± 10.11 years and mean morning stiffness duration of patients with axSpA was 28.17 ± 33.71 min. Patients with axSpA presented low disease activity (mean BASDAI: 3.04 ± 1.90) and low impact of axSpA on physical function (mean BASFI: 2.86 ± 2.04). Most of patients with axSpA had anti-TNF treatment (n = 21, 70.0%), while others had Interleukin-17A (n = 2, 6.7%), nonsteroidal anti-inflammatory drugs (n = 7, 23.3%), disease modifying anti-rheumatic drugs (n = 3, 10.0%) and/or pain reliefs (n = 7, 23.3%).
Gait performance
Spatiotemporal gait parameters in single- and dual-task conditions are illustrated in Fig. 2 for each group.
Results showed main effects of group for each evaluated spatiotemporal gait parameters, namely gait speed (F(1,58) = 31.528, p < 0.001, partial η2 = 0.352, Fig. 2A), cadence (F(1,58) = 9.383, p = 0.003, partial η2 = 0.139, Fig. 2B), stride length (F(1,58) = 23.067, p < 0.001, partial η2 = 0.285, Fig. 2C), double support time (F(1,57) = 24.329, p < 0.001, partial η2 = 0.299, Fig. 2D), swing time (F(1,58) = 20.922, p < 0.001, partial η2 = 0.265, Fig. 2E), and stance time (F(1,58) = 20.922, p < 0.001, partial η2 = 0.265, Fig. 2F).
Results also showed main effects of condition for five out of six evaluated spatiotemporal gait parameters, namely, gait speed (F(1,58) = 23.674, p < 0.001, partial η2 = 0.290, Fig. 2A), stride length (F(1,58) = 42.833, p < 0.001, partial η2 = 0.425, Fig. 2C), double support time (F(1,57) = 11.105, p = 0.002, partial η2 = 0.163, Fig. 2D), swing time (F(1,58) = 7.591, p = 0.008, partial η2 = 0.116, Fig. 2E), and stance time (F(1,58) = 7.691, p = 0.008, partial η2 = 0.116, Fig. 2F). No significant main effect of condition was observed for cadence (F(1,58) = 1.865, p = 0.177, partial η2 = 0.031, Fig. 2B).
Results further showed no significant interaction of group and condition for all evaluated spatiotemporal parameters, namely gait speed (F(1,58) = 0.108, p = 0.743, partial η2 = 0.002), cadence (F(1,58) = 0.540, p = 0.465, partial η2 = 0.009), stride length (F(1,58) = 0.215, p = 0.644, partial η2 = 0.004), double support time (F(1,57) = 1.562, p = 0.216, partial η2 = 0.027), swing time (F(1,58) = 1.171, p = 0.284, partial η2 = 0.020), and stance time (F(1,58) = 1.171, p = 0.284, partial η2 = 0.020).
Secondary task performance
Analysis of the performance of the secondary task first showed that most of the participants did not spilled water out of the glass (axSpA: n = 29, 96.6%; controls: n = 28, 93.3%). Furthermore, no significant difference was found on the number of time the participants spilled water out of the glass between the two groups (axSpA: 0.13 ± 0.73, controls: 0.07 ± 0.25, p = 0.638).
Discussion
Dual-task paradigm has become a well-established research paradigm to examine the interactions between cognition and the control of walking (e.g. see 2,3,4,5,6,7,8,9,10,11,12,13,14, for recent reviews). Although this paradigm has been widely used in older adults7,8,9,10 and patient populations11,12,13,14, to the best of our knowledge, this is the first study assessing dual tasking while walking in patients with axSpA41.
Results first showed that gait performance was adversely affected by the concurrent execution of the manual task in healthy adults. Specifically, significant changes in spatiotemporal gait parameters were characterized by walking speed decreased by 4.8%, stride length decreased by 3.9%, swing time decreased by 0.6%, stance time increased by 0.4% and double support time increased by 2.7% during the dual-task as compared to the single-task walking condition. These results were expected in line with hypothesis 1. They are indeed in accordance with previous studies that have used a similar secondary manual task while walking at self-selected comfortable speed5,42,43 and have reported significant alterations of gait patterns in healthy individuals5,42,43. These results 5,42,43 and ours hence suggest that interference of manual task with gait performance, that is classically explained by competing demands for attentional resources involved in both concurrent tasks3,8,10, can occur even in healthy adults5,42,43. Otherwise, indeed, the simultaneous execution of the manual task would not have significantly affected gait performance or secondary manual task performance.
More originally, in line with our hypothesis 1, results further showed that walking performance of patients with axSpA also was significantly impaired while performing walking and manual task simultaneously. The concurrent execution of the secondary manual task negatively affected walking performance in terms of significantly decreased mean speed by 6.5%, stride length by 5.2%, and swing time 1.4%, and significantly increased double support by 4.8% and stance time by 0.9% in the dual-task condition as compared to the single-task condition. To the best of our knowledge this result obtained in patients with axSpA is new.
Finally, perhaps the most interesting (and unexpected) result of this study was that dual task effects on walking performance were similar between patients with axSpA and age and sex matched healthy controls. Indeed, no significant interaction of group and condition for any of the calculated spatiotemporal gait parameter were found. In other words, contrary to our hypothesis 2 and to previous observations in other patient populations (e.g. patients with neurologic disorders (e.g., see for reviews11,12,13,14)), patients with axSpA were not more affected by the dual task than age and sex matched healthy controls. Interestingly, together with the absence of significant difference on the performance of the secondary manual task between the two groups, this result suggests that gait, although significantly altered in patients with axSpA in both single- and dual-task conditions as compared to age and sex healthy controls, did not require greater attention in patients with axSpA.
That being said, it is important to bear in mind that the explanations of dual-task interference are based on the assumption that attentional resources are limited3. Accordingly, dual-task interference is likely to occur if the available central capacity of the individual is exceeded, which causes an inability to appropriately adapt the allocation of attention between the two concurrently performed gait and secondary tasks. Accordingly, dual-task interference can theoretically be either (1) cognitive-locomotor related (i.e. with effects on both cognitive and locomotor tasks), (2) cognitive-related (i.e. with effects on cognitive task only), (3) motor-related (i.e. with effects on locomotor task only) or (4) absent12. In the present study, dual-task interference observed in both patients with axSpA and healthy controls can be placed in the class of ‘motor-related’ as the gait performance was significantly altered during dual-task walking and the performance of secondary manual task while walking remained maximal. However, note that both patients with axSpA and healthy controls experienced little ‘motor-related’ dual-task interference, as the decrement in gait performance on the a 10-m walk test relative to single-task performance was minimal (see percentage changes in spatiotemporal gait parameters from single- to dual-task condition below, from 0.4 to 4.78% in healthy controls and from 0.87 to 6.5% in patients with axSpA).
At this point, within the context of a dual-task, the attentional demand associated with gait depends on various factors8,10,12,15 that could account for the observed results. These factors could be regarded as possible explanations and as study limitation that we acknowledge.
Firstly, we are aware that the type, the level of complexity and novelty of either the primary walking task33,44,45,46 and/or concurrent secondary task8,10,12,15 can significantly influence the dual-task interference during walking (e.g., see 8,10,12,15 for recent reviews). However, in the present study, only one walking task (walking at a self-selected comfortable speed)28,45 and one secondary task (‘carrying a full cup of water’)5,42 were investigated. These two tasks were chosen on the basis on the recommendations from a recent systematic review that dual-task assessments should be performed “in similar contexts of individuals' daily lives to ensure ecological validity” (12, page 1). Note however that these two tasks may not be representative of all dual-task conditions during walking. These two tasks hence represents relatively easy and familiar tasks in terms of level of complexity (i.e. the task’s constraints and environmental context) and novelty (i.e. the individual’s previous experience with performance of the tasks). What is more, these two tasks are also routinely used in clinical settings to assess gait in a wide range of patient populations. Increasing tasks complexity could thus have modify tasks performance with possible differences between patients with axSpA and healthy controls during dual-tasking.
Secondly, we are aware that dual-task interference during walking also depends on the study population47,48. Naturally, this factor must be considered in close connection with the above-mentioned task-related factors. Indeed, depending on the characteristics of the study population, the tasks may not be challenging enough to reach/exceed the central capacity limit. It is thus probable that the attentional resources required to simultaneously perform the walking task and the manual task did not overload the available central resources and, consequently, only induced little dual-task interference with minor gait alterations. To the best of our knowledge, the present study is the first to investigate the effects of dual tasking on gait in patients with chronic rheumatic disease. One study assessed previously the effects of an arithmetic task on postural control in patients with rheumatoid arthritis49 and found that the effect of the arithmetic task on balance parameters was small and similar in patients and controls. These authors hypothesized that the slow evolution of joint destruction may let time to patients to adapt their postural coordination pattern without requiring attentional control49. A similar interpretation could be argue in the present population. However, the authors visually found that patients with rheumatoid arthritis with most severe joint destruction showed relatively strong dual-task effect and may have not have enough sample size to see this effect statistically49. Patients of the present study may not represent the whole population of axSpA50, as theywere 18–65, with stable treatment for at least 3 months, able to walk 180 m without technical help. Besides, they had low disease activity (BASDAI: 3.04 ± 1.90) with low impact of physical function (BASFI: 2.86 ± 2.04).
In other words, the present findings are neither transferable to other walking and secondary tasks nor other cohorts of patients with axSpA. Accordingly, further studies that will employ other walking tasks33,44,45,46 and/or secondary tasks8,10,12,15 and/or recruit other cohorts (e.g., patients with lower walking range, or higher disease activity with more impact on physical function) are needed to confirm and to generalize our results. It is possible that increasing the complexity of the walking and/or secondary task would increase the sensitivity of the dual-task design to patients with chronic rheumatic diseases. Limitations notwithstanding, the findings of the present study showed for the first time that gait of patients with axSpA is significantly impaired while performing walking and manual tasks simultaneously similar to what was observed in healthy controls.
Ethics approval and consent to participate
The study was approved by local ethic committee (CPP IDF1. RCB: 2017-A03468-45. Date of agreement: July 17th. Last version: V6.0. 2020. June 17th). The study is registered on ClinicalTrials.gov. With the following ID: NCT03761212 and followed the SPIRIT checklist. Written informed consent were obtained from all participants by the physiotherapist or a doctor.
Patient involvement
Patients were recruited from rheumatologist. Results will be disseminated via email to all study participants and via conference presentations to rheumatologists, general doctors, physical therapists and researchers. A poster of the results will be displayed in the Rheumatology Department of Grenoble University Hospital (France) to inform all patients with axSpA and visitors on the results of the study.
Data availability
The data of the present manuscript can be available on demand to the corresponding author.
References
McIsaac, T. L., Lamberg, E. M. & Muratori, L. M. Building a framework for a dual task taxonomy. BioMed Research International https://www.hindawi.com/journals/bmri/2015/591475/ (2015).
Kelly, V. E., Janke, A. A. & Shumway-Cook, A. Effects of instructed focus and task difficulty on concurrent walking and cognitive task performance in healthy young adults. Exp. Brain Res. Exp. Hirnforsch. Exp. Cerebrale 207, 65–73 (2010).
Beurskens, R., Steinberg, F., Antoniewicz, F., Wolff, W. & Granacher, U. Neural correlates of dual-task walking: effects of cognitive versus motor interference in young adults. Neural Plast. 2016, 8032180 (2016).
Stöckel, T. & Mau-Moeller, A. Cognitive control processes associated with successful gait performance in dual-task walking in healthy young adults. Psychol. Res. 84, 1766–1776 (2020).
Kwon, Y., Kwon, J. W. & Cho, I. H. The difference of gait characteristic according to the variety of dual tasks in young healthy adults. Work Read. Mass 63, 33–38 (2019).
Johnson, R. S., Scott, K. H. & Lynall, R. C. A proposal for complex gait evaluation using dual-task gait termination time. J. Sport Rehabil. https://doi.org/10.1123/jsr.2020-0080 (2020).
Beurskens, R. & Bock, O. Age-related deficits of dual-task walking: a review. Neural Plast. 2012, 1–9 (2012).
Al-Yahya, E. et al. Cognitive motor interference while walking: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 35, 715–728 (2011).
Smith, E., Cusack, T., Cunningham, C. & Blake, C. The influence of a cognitive dual task on the gait parameters of healthy older adults: a systematic review and meta-analysis. J. Aging Phys. Act. 25, 671–686 (2017).
Wollesen, B., Wanstrath, M., van Schooten, K. S. & Delbaere, K. A taxonomy of cognitive tasks to evaluate cognitive-motor interference on spatiotemoporal gait parameters in older people: A systematic review and meta-analysis. Eur. Rev. Aging Phys. Act. Off. J. Eur. Group Res. Elder. Phys. Act. 16, 12 (2019).
Lee, H., Sullivan, S. J. & Schneiders, A. G. The use of the dual-task paradigm in detecting gait performance deficits following a sports-related concussion: a systematic review and meta-analysis. J. Sci. Med. Sport 16, 2–7 (2013).
Deblock-Bellamy, A., Lamontagne, A. & Blanchette, A. K. Cognitive-locomotor dual-task interference in stroke survivors and the influence of the tasks: a systematic review. Front. Neurol. 11, 25689 (2020).
Yogev, G. et al. Dual tasking, gait rhythmicity, and Parkinson’s disease: which aspects of gait are attention demanding?. Eur. J. Neurosci. 22, 1248–1256 (2005).
Postigo-Alonso, B. et al. Cognitive-motor interference during gait in patients with Multiple Sclerosis: a mixed methods Systematic Review. Neurosci. Biobehav. Rev. 94, 126–148 (2018).
Bayot, M. et al. The interaction between cognition and motor control: A theoretical framework for dual-task interference effects on posture, gait initiation, gait and turning. Neurophysiol. Clin. Clin. Neurophysiol. 48, 361–375 (2018).
Aboutorabi, A., Arazpour, M., Bahramizadeh, M., Hutchins, S. W. & Fadayevatan, R. The effect of aging on gait parameters in able-bodied older subjects: a literature review. Aging Clin. Exp. Res. 28, 393–405 (2016).
Chatterjee, S. A. et al. Mobility function and recovery after stroke: preliminary insights from sympathetic nervous system activity. J. Neurol. Phys. Ther. JNPT 42, 224–232 (2018).
Pirker, W. & Katzenschlager, R. Gait disorders in adults and the elderly. Wien. Klin. Wochenschr. 129, 81–95 (2017).
Lam, R. Office management of gait disorders in the elderly. Can. Fam. Physician 57, 765–770 (2011).
Soulard, J., Vaillant, J., Baillet, A., Gaudin, P. & Vuillerme, N. Gait and axial spondyloarthritis: A comparative gait analysis study using foot-worn inertial sensors. JMIR MHealth UHealth (2021).
Belur, P., Hsiao, D., Myers, P. S., Earhart, G. M. & Rawson, K. S. Dual-task costs of texting while walking forward and backward are greater for older adults than younger adults. Hum. Mov. Sci. 71, 102619 (2020).
Prupetkaew, P., Lugade, V., Kamnardsiri, T. & Silsupadol, P. Cognitive and visual demands, but not gross motor demand, of concurrent smartphone use affect laboratory and free-living gait among young and older adults. Gait Posture 68, 30–36 (2019).
Soulard, J. et al. Gait as predictor of physical function in axial spondyloarthritis: The prospective longitudinal FOLOMI (Function, Locomotion, Measurement, Inflammation) study protocol. Rheumatol. Int. https://doi.org/10.1007/s00296-019-04396-4 (2019).
Zebouni, L., Helliwell, P. S., Howe, A. & Wright, V. Gait analysis in ankylosing spondylitis. Ann. Rheum. Dis. 51, 898–899 (1992).
Lwanga, S. K., Lemeshow, S. & Organization, W. H. Sample Size Determination in Health Studies: A Practical Manual (World Health Organization, 1991).
wnarifin.github.io—Sample size calculator. https://wnarifin.github.io/ssc/ss2mean.html.
Zochling, J. Measures of symptoms and disease status in ankylosing spondylitis: Ankylosing Spondylitis Disease Activity Score (ASDAS), Ankylosing Spondylitis Quality of Life Scale (ASQoL), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Functional Index (BASFI), Bath Ankylosing Spondylitis Global Score (BAS-G), Bath Ankylosing Spondylitis Metrology Index (BASMI), Dougados Functional Index (DFI), and Health Assessment Questionnaire for the Spondylarthropathies (HAQ-S). Arthritis Care Res. Hoboken 63(Suppl 11), S47-58 (2011).
Graham, J. E., Ostir, G. V., Fisher, S. R. & Ottenbacher, K. J. Assessing walking speed in clinical research: a systematic review. J. Eval. Clin. Pract. 14, 552–562 (2008).
Beauchet, O. et al. Guidelines for assessment of gait and reference values for spatiotemporal gait parameters in older adults: The biomathics and Canadian gait consortiums initiative. Front. Hum. Neurosci. 11, 353 (2017).
Yang, L., He, C. & Pang, M. Y. C. Reliability and validity of dual-task mobility assessments in people with chronic stroke. PLoS ONE 11, e0147833 (2016).
Nordin, E., Moe-Nilssen, R., Ramnemark, A. & Lundin-Olsson, L. Changes in step-width during dual-task walking predicts falls. Gait Posture 32, 92–97 (2010).
Deblock-Bellamy, A., Lamontagne, A. & Blanchette, A. K. Cognitive-locomotor dual-task interference in stroke survivors and the influence of the tasks: a systematic review. Front. Neurol. 11, 882 (2020).
Leone, C. et al. Comparing 16 different dual-tasking paradigms in individuals with multiple sclerosis and healthy controls: Working memory tasks indicate cognitive-motor interference. Front. Neurol. 11, 918 (2020).
Lima, L. C. A., Ansai, J. H., Andrade, L. P. & Takahashi, A. C. M. The relationship between dual-task and cognitive performance among elderly participants who exercise regularly. Braz. J. Phys. Ther. 19, 159–166 (2015).
Cedervall, Y. et al. Timed up-and-go dual-task testing in the assessment of cognitive function: A mixed methods observational study for development of the UDDGait protocol. Int. J. Environ. Res. Public. Health 17, 1715 (2020).
Lefeber, N., Degelaen, M., Truyers, C., Safin, I. & Beckwee, D. Validity and reproducibility of inertial physilog sensors for spatiotemporal gait analysis in patients with stroke. IEEE Trans. Neural Syst. Rehabil. Eng. Publ. IEEE Eng. Med. Biol. Soc. 27, 1865–1874 (2019).
Truong, P. H., Lee, J., Kwon, A.-R. & Jeong, G.-M. Stride counting in human walking and walking distance estimation using insole sensors. Sensors 16, 823 (2016).
Anwary, A. R., Yu, H. & Vassallo, M. An automatic gait feature extraction method for identifying gait asymmetry using wearable sensors. Sensors 18, 676 (2018).
Song, Y., Wang, C. & Chen, H. Functional limitation and associated factors in outpatients with ankylosing spondylitis in Southwest China. Clin. Rheumatol. 36, 871–877 (2017).
Soulard, J. et al. Foot-worn inertial sensors are reliable to assess spatiotemporal gait parameters in axial spondyloarthritis under single and dual task walking in axial spondyloarthritis. Sensors 20, 6453 (2020).
Soulard, J., Vaillant, J. & Vuillerme, N. Gait in patients with axial spondyloarthritis: a systematic review of the literature. Curr. Rheumatol. Rev. https://doi.org/10.2174/1573397117666210921114949 (2021).
Abbruzzese, L. D. et al. Effects of manual task complexity on gait parameters in school-aged children and adults. Gait Posture 40, 658–663 (2014).
Yang, Y.-R., Chen, Y.-C., Lee, C.-S., Cheng, S.-J. & Wang, R.-Y. Dual-task-related gait changes in individuals with stroke. Gait Posture 25, 185–190 (2007).
Fino, P. C. et al. Detecting gait abnormalities after concussion or mild traumatic brain injury: A systematic review of single-task, dual-task, and complex gait. Gait Posture 62, 157–166 (2018).
Nazary-Moghadam, S. et al. Gait speed is more challenging than cognitive load on the stride-to-stride variability in individuals with anterior cruciate ligament deficiency. Knee 26, 88–96 (2018).
Shkuratova, N., Morris, M. E. & Huxham, F. Effects of age on balance control during walking. Arch. Phys. Med. Rehabil. 85, 582–588 (2004).
Smith, E., Cusack, T. & Blake, C. The effect of a dual task on gait speed in community dwelling older adults: A systematic review and meta-analysis. Gait Posture 44, 250–258 (2016).
Yang, Q. et al. Gait change in dual task as a behavioral marker to detect mild cognitive impairment in elderly persons: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 101, 1813–1821 (2020).
Tjon, S. S., Geurts, A. C., van’t Pad Bosch, P., Laan, R. F. & Mulder, T. Postural control in rheumatoid arthritis patients scheduled for total knee arthroplasty. Arch. Phys. Med. Rehabil. 81, 1489–1493 (2000).
Madsen, O. R. Stability of fatigue, pain, patient global assessment and the Bath Ankylosing Spondylitis Functional Index (BASFI) in spondyloarthropathy patients with stable disease according to the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). Rheumatol. Int. 38, 425–432 (2018).
Sieper, J. et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: A guide to assess spondyloarthritis. Ann. Rheum. Dis. 68, 1–44 (2009).
van der Linden, S., Valkenburg, H. A. & Cats, A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 27, 361–368 (1984).
Acknowledgements
The authors acknowledge all the participants of the study and the Folomi team for conceiving and designing the Folomi study (J. Soulard, N. Vuillerme, P. Gaudin, L. Grange, A. Baillet, J.-L. Cracowski, R. Juvin, J. Vaillant). We also would like to thank Thomas Carlin for its help on data analysis.
Funding
This work is supported by the French Ministry of Health and Solidarity with the “Nursing and Paramedical Hospital Research Program” year 2016 (PHRIP-16-0528) and by the French National Research Agency in the framework of the "Investissements d’avenir” program (ANR-10-AIRT-05 and ANR-15-IDEX-02). The sponsors had no involvement in the design of the study, the collection, analysis and interpretation of data and in writing the manuscript. This study is part of the Ph.D. thesis of the first author JS (Univ. Grenoble Alpes. AGEIS. France & Grenoble Alps University Hospital. Grenoble. France). This work further forms part of a broader translational and interdisciplinary research program. GaitAlps (NV).
Author information
Authors and Affiliations
Contributions
Folomi team conceptualized and designed the study23. J.V. and N.V. supervised the project. J.S. was responsible for the acquisition and analysis of the data. J.S., J.V. and N.V. interpreted the results. J.S. drafted the first version of the manuscript. J.V. and N.V. revised the article critically for important intellectual content. All authors read and approved the final version and agreed to be accountable for all aspects related to the accuracy or integrity of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Soulard, J., Vaillant, J., Baillet, A. et al. The effects of a secondary task on gait in axial spondyloarthritis. Sci Rep 11, 19537 (2021). https://doi.org/10.1038/s41598-021-98732-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98732-z
- Springer Nature Limited