Abstract
Vascular graft or endograft Infections (VGEI) are rare but severe complications of vascular reconstructive surgery, and associated with significant mortality and morbidity risk. Positron emission tomography/computed tomography with 18F-fluorodeoxyglucose (PET/CT) has been shown to have a high diagnostic accuracy in the detection of VGEI. In this single-center prospective cohort study, we assessed the rate and the impact on patient management of relevant unknown incidental findings in PET/CT of patients with proven or suspected VGEI, and clinical follow-up of all patients was performed. Our study results show a comparably high rate of relevant unknown incidental findings (181 in 502 examinations), with documented direct impact on patient management in 80 of 181 (44%) of all findings. PET/CT scan- and patient-based evaluation revealed impact on patient management in 76 of 502 (17%) of all PET/CT scans, and in 59 of 162 (36%) of all patients, respectively. Furthermore, PET/CT correctly identified the final diagnosis in 20 of 36 (56%) patients without VGEI. In conclusion, in proven and suspected VGEI, PET/CT detects a high rate of relevant unknown incidental findings with high impact on patient management.
Similar content being viewed by others
Introduction
Vascular graft or endograft Infections (VGEI) are a rare but severe complication of vascular reconstructive surgery, and are associated with a significant mortality and morbidity risk1,2,3. The therapy of VGEI is usually demanding and needs to be individualized with respect to clinical findings, graft material, site of infection, microorganism/s involved and patient co-morbidities. A combination of the overall appraisal of clinical presentation, laboratory, and imaging is considered the gold standard for the diagnosis of VGEI4. With respect to imaging, 18F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) has been demonstrated to be highly accurate for the initial diagnosis5,6,7,8,9, and its usefulness in therapy control of VGEI has also been documented by initial studies10,11. Likewise, PET/CT has been shown to be accurate and sensitive in the detection of other infections and numerous malignant diseases12,13,14,15,16,17,18,19,20. Furthermore, as PET/CT is usually performed as a whole-body examination, a higher incidence of incidental findings may be expected compared to traditional imaging modalities, such as contrast-enhanced CT, which are usually limited to the anatomical site of a suspected VGEI in the chest and/or abdomen. Hence, PET/CT may potentially increase the likelihood of detection of hitherto unknown co-morbidities.
Therefore, the aim of our study was to determine the rate and the impact on patient management of unknown incidental findings in PET/CT examinations of patients with proven or suspected VGEI.
Methods
Study design
All patients were prospectively enrolled as part of the Vascular Graft Cohort Study (VASGRA; clinical trials. gov identifier: NCT01821664), an open, prospective observational cohort study21, including patients aged ≥ 18 years with any type of vascular graft operation and clinical suspicion of VGEI. The diagnosis of VGEI was defined as suggested by the Management of Aortic Graft Infection Collaboration (MAGIC). Every clinical case was adjudicated by a multidisciplinary team of infectious disease specialists, cardiovascular surgeons, radiologists, nuclear medicine physicians and microbiologists. The gold standard for VGI diagnosis was a positive microbiological culture of the deep tissue around the vascular prosthesis, obtained by open biopsy or a positive microbiological culture of an explanted vascular graft. In cases with excluded VGEI, clinical, laboratory, histopathological and imaging results were also considered, and served as the standard of reference.
A case file review was performed in all patients, and information collected at the time of the initial diagnosis, at the time of imaging and at the last clinical visit (recorded until June 2020). Data included patient demographics, laboratory data, results of microbiology, clinical information, and information about treatment. Written informed consent was obtained from all participants. The institutional ethics committee approved the study, namely the Kantonale Ethikkomission Zürich (KEK-ZH-Nr. 2012-0583). All procedures were performed in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
PET/CT data acquisition
Patients fasted for at least four hours prior to PET/CT imaging. Blood glucose levels < 12 mmol/l were accepted22. The standardized uptake time was 60 min in supine position. A non-enhanced CT scan for attenuation correction and anatomic localization of 18F-FDG uptake was performed with arms overhead whenever possible, using automated dose modulation (range 10–100 mA, 120–140 kV) with a scan range from the vertex of the skull to the mid of the thighs or to the feet. Two types of PET/CT scanners were used within the study period between 2012 and 2020 (i.e. Discovery VCT, and Discovery MI, both GE Healthcare, Waukesha, WI), using either the 3-dimensional acquisition mode with a fixed scan duration of two minutes per bed position (Discovery VCT), or a time-of-flight acquisition mode with a fixed scan duration of 2.5 min per bed position (Discovery MI).
PET/CT image analysis and definitions
All PET/CT were analysed independently on a dedicated workstation (Advantage Workstation, version 4.7, GE Healthcare Biosciences, Pittsburgh, PA) by two dually board-certified radiologists and nuclear medicine physicians, both with more than 8 years experience in hybrid imaging. Primary and secondary (e.g. infectious foci not in the vicinity of the aorta or other relevant findings such as malignancies) diagnoses were documented if deemed potentially relevant for patient management. A consensus reading was performed if results differed. All findings were retrospectively analysed, whether the findings were previously known (e.g.: by previous other imaging modalities). If findings were not previously known and were considered to harbour potential impact on patient management, they were defined as “unknown incidental findings”.
All patients were clinically followed by reviewing electronic patient charts, to document the impact on patient management of all findings.
Statistical analyses
Variables were expressed as median and interquartile range (25th, 75th percentiles) or percentages. All statistical analyses were performed using commercially available software (Stata/SE, Version 16.1, StataCorp, College Station, Texas).
Results
Patient population
We analyzed 505 PET/CT scans of 162 patients who consented to participate in the VASGRA Cohort Study. After dropping three PET/CT from three patients scanned for the evaluation of mycotic aneurysms prior to graft placements, we finally included 502 PET/CT of 162 patients. Patient demographics of the final study population are displayed in Table 1.
Findings
PET/CT was successfully performed with diagnostic image quality after body-weight adjusted intravenous injection of FDG (i.e., 295 Megabecquerel (interquartile range (IQR) 248–360) in all patients with proven or suspected VGEI. One hundred twenty six (78%) patients had a VGEI, as defined by the Management of Aortic Graft Infection Collaboration (MAGIC)4. VGEI was ruled out in the remaining 36 patients (22%). In three of these patients (8%), PET/CT was performed after treatment of sepsis, to rule out a VGEI or other remaining infectious foci (all three PET/CT were correctly negative). In another three patients (8%), the suspicion for a graft infection was not confirmed, and the reason for the clinical symptoms, which had led to the study inclusion, remained unclear (i.e. no other site of inflammation of infection was detected). The final diagnosis of the remaining 30 patients with excluded VGEI were pneumonia (n = 9), endocarditis (n = 4), Dressler-syndrome (n = 2), soft tissue infection (n = 3), colitis (n = 2), sternal wound infection and spondylodiscitis (n = 1), thrombophlebitis and spondylodiscitis (n = 1), diverticulitis (n = 1), gastritis (n = 1), pyelonephritis (n = 1), aortic dissection (n = 1), gout (n = 1), retroperitoneal fibrosis with consecutive ureteral obstruction (n = 1), inflammatory aortic aneurysms (n = 1), and sinusitis (n = 1). PET/CT correctly identified 20 (67%) of these findings (pneumonia (n = 9), soft tissue infection (n = 2), colitis (n = 2), sternal wound infection and spondylodiscitis (n = 1), thrombophlebitis and spondylodiscitis (n = 1), diverticulitis (n = 1), gastritis (n = 1), retroperitoneal fibrosis with consecutive ureteral obstruction (n = 1), inflammatory aortic aneurysms (n = 1), and sinusitis (n = 1) (Table 2).
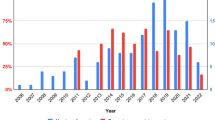
Overall, PET/CT identified 181 previously unknown and clinically relevant incidental findings (Figs. 1, 2, 3, 4, Table 2) in 502 scans: 340 PET/CT scans revealed no incidental finding, 147 scans one, 12 scans two, 2 scans three, and 1 scan four incidental findings. The initial PET/CT of each patient revealed 95 findings in 162 examinations (59%), while 86 findings were detected in 340 follow-up examinations. (25%). At least one unknown incidental finding was detected in 162 of 502 (32%) PET/CT scans and in 111 of 162 (69%) patients. Direct impact on patient management was documented in 80 of 181 (44%) of all incidental findings, in 76 of 502 (17%) of all PET/CT scans, and in 59 of 162 (36%) of all patients.
A 70-year old female patient was referred to PET/CT 14 months after the initial diagnosis of a vascular graft infection due to Streptococcus hominis. The reason for referral was whether antibiotic treatment could be stopped. PET/CT [maximum intensity reconstructions of PET (A) and fused PET/CT images (B–D)] showed diffuse FDG uptake along the ascendens graft (Index surgery: aortic arch replacement with 28 mm Intergard® prosthesis) (black arrow heads in A, white arrow heads in C) which was focally pronounced (A) indicating persistent infection. Antibiotic treatment was continued for another eight months and then successfully stopped (no signs for recurrence at the last control seven months later). The patient had known thyroiditis, which presented with diffuse FDG uptake (upper black arrow in A, white arrow in B); this finding was not evaluated for impact on patient management in our study, as it was already known prior to PET/CT. An unknown and relevant incidental finding was detected in the sigmoid colon with intense focal FDG uptake (lower black arrow in A, white arrow in D). This PET/CT finding was rated to have impact on patient management—subsequent coloscopy and resection revealed a colonic polyp with dysplasia.
A 75-year old male patient was referred to PET/CT five years and two months after the initial diagnosis of a vascular graft infection due to Streptococcus pneumoniae. The reason for referral was whether antibiotic treatment could be stopped. PET/CT [maximum intensity reconstructions of PET (A) and fused PET/CT images (B–D)] showed no focal FDG uptake along the ascendens graft (index surgery: biologic composite graft replacement by Gelweave graft; reconstruction of right pulmonary artery with xenopericardium), indicating complete response to antibiotic therapy. There was physiologic FDG uptake at the base of the left ventricle (black arrow heads in A, white arrow heads in D). As a relevant incidental finding with impact on patient management, PET/CT detected two foci with intense focal FDG uptake in the esophagus (lower black arrow in A, white arrow in B) and upper mediastinum (upper black arrow in A, white arrow in C). Endoscopy and biopsy confirmed metastasized esophageal cancer and the patient was subsequently treated with palliative radiation therapy.
A 61-year old male patient was referred to PET/CT one year and four months after the initial diagnosis of a vascular endograft infection due to Streptococcus dysgalactiae. The patient was under antimicrobial therapy, but had acute fever and the reason for referral was the search for new infectious foci. PET/CT [maximum intensity reconstructions of PET (A) and fused PET/CT images (B–D)] showed faint residual focal FDG uptake along the extraanatomical aorto bi-iliac reconstruction (Dacron silver Intergard graft) (black arrow in A, white arrow in B), suggestive for persistent infection. Unknown and relevant incidental findings with impact on patient management were detected by PET/CT with intense focal FDG uptake in the prostate gland (black arrow head in A, white arrow in C), and in the epididymis (white arrows in A and D). Subsequent further work-up confirmed prostatitis with Enterobacter cloacae and antibiotic treatment was escalated accordingly.
A 66-year old male patient was referred to PET/CT for follow-up of a vascular graft infection with P. aeruginosa. PET/CT [maximum intensity reconstructions of PET (A) and fused PET/CT images (B–D)] showed intense focal FDG uptake of the aortobifemoral graft (black arrow head in A, white arrow in B), suggestive for persistent infection. Subsequently, the aortobifemoral graft was reconstructed in situ with a SilverGuard Dacron graft. An unknown and potentially relevant incidental finding was detected in the upper thighs with intense focal FDG uptake, in line with septic emboli (black arrows in A, white arrow in C and D). The incidental PET/CT finding was rated not to have impact on patient management, since no direct action was initiated with regard to the potential septic emboli in the upper thighs.
Discussion
We assessed the rate and the impact on patient management of relevant unknown incidental findings in PET/CT of patients with proven or suspected VGEI.
Our study results show a comparably high rate of relevant unknown incidental findings (181 in 502 examinations), with documented direct impact on patient management in 80 of 181 (44%) of all findings. PET/CT scan- and patient-based evaluation revealed impact on patient management in 76 of 502 (17%) of all PET/CT scans, and in 59 of 162 (36%) of all patients, respectively. Furthermore, PET/CT correctly identified the final diagnosis in 20 of 36 (56%) patients without VGEI.
The present study represents the first study to analyze the impact of incidental findings on patient management in a large prospectively enrolled study population with suspected or proven VGEI. Several other studies have performed similar analysis in different study populations, however, the definitions of “impact on management” and “relevant unknown incidental findings” are very inhomogeneous throughout the literature. For example, Wan et al.23 performed PET/CT in patients with psoriasis. Similar to our study, their “relevant” findings were determined by the report of the reading radiologist/nuclear medicine physician. The authors found less relevant findings (i.e. in 12% of 259 patients), and documented that the risk of discovery of significant findings was associated with age. In comparison, the age of our study population was much higher (i.e. 45 years versus 69 years) and we did not exclude patients due to other comorbidities, while Wan et al.23 excluded patients with significant comorbidities such as diabetes or uncontrolled hypertension. Both differences may account for the higher incidence of incidental findings in our study.
On the other hand, Nihuis et al.24 found a much higher incidence of non-melanoma findings on baseline and annual surveillance CT and PET/CT of asymptomatic melanoma patients (i.e. 912 findings in 1022 scans versus 181 findings in 502 scans in our study). The authors included findings which were not considered “relevant” findings in our study (e.g., coronary artery calcifications or heart valve calcifications), and their rate of findings with impact on patient management was lower as compared to our study (114 of 912 findings versus 80 of 181 findings). The latter, may possibly be explained by the younger age (i.e., mean age 49) of the patient population in the study by Nihuis et al.24,25, and also by a higher comorbidity rate in cardiovascular patients, in general26.
An even higher rate on impact on management was reported by Hadad et al.27, reporting 642 of 1090 (59%) incidental foci to be clinically relevant in a literature review of selected patient cohorts with different types of cancer. We suppose that the comparably lower rate of findings with impact on patient management in our study, may in part be due to systematic differences between patient populations with cancer and patient populations with infectious diseases. For example, an incidentally detected pneumonia in a patient with cancer will result in a change in patient management, as antibiotic treatment will be initiated. However, in a patient with a newly detected VGEI and a synchronous pneumonia, both diseases might be treated with the same antibiotic agent, rendering the incidentally detected pneumonia to “without impact on management”. Hence, we believe that the rate of relevant incidental findings with impact on patient management may even be underestimated in patient populations with infectious diseases.
Finally, PET/CT has been shown to have a high diagnostic accuracy in the detection of VGEI, with an excellent negative predictive value6,7,28,29,30. Our study demonstrates that PET/CT may not only rule out VGEI correctly in patients with suspected VGEI, but may also provide the correct diagnosis in a large proportion of patients without VGEI but with clinical symptoms that were responsible for the referral to PET/CT with the question for VGEI. In fact, PET/CT identified the final diagnosis in 56% of patients with clinical symptoms but without VGEI in our study. Notably, some of the final diagnoses made in the patients without VGEI and with negative PET/CT were diagnoses, which cannot reliably be detected in normal state-of-the-art PET/CT without additional intravenous contrast medium (e.g., pyelonephritis, Dressler-syndrome, or endocarditis). Our data is in line with previous publications indicating that PET/CT is helpful in detecting sites of infections in general [in a median of 54% (range 26–92%)31] and is often superior to other imaging modalities, e.g. in fever of unknown origin13, chronic osteomyelitis32, or mycotic aortic aneurysms15.
Limitations of the study
The definitions of “impact on management” and “relevant unknown incidental findings” are very inhomogeneous throughout the literature and challenge the comparability of our study results to previous ones. To date, our study represents the largest prospectively enrolled study population with suspected or proven VGEI and our results clearly underline the impact of PET/CT on patient management. Notably, the study population is selective and also inhomogeneous (e.g. including aortic and peripheral grafts). Finally, it was beyond the scope of the present study to analyse the risks and drawbacks of the detection of incidental findings, as these findings may cause patient anxiety, trigger further investigations and increase health care costs33.
Conclusion
In proven and suspected VGEI, PET/CT detects a high rate of relevant unknown incidental findings with high impact on patient management.
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Chakfe, N. et al. Editor’s choice - European Society for Vascular Surgery (ESVS) 2020 clinical practice guidelines on the management of vascular graft and endograft infections. Eur. J. Vasc. Endovasc. Surg. 59, 339–384 (2020).
Wilson, W. R. et al. Vascular graft infections, mycotic aneurysms, and endovascular infections: A Scientific Statement From the American Heart Association. Circulation 134, e412–e460 (2016).
Hallett, J. W. Jr. et al. Graft-related complications after abdominal aortic aneurysm repair: Reassurance from a 36-year population-based experience. J. Vasc. Surg. 25, 277–284 (1997) (Discussion 285–276).
Lyons, O. T. et al. Diagnosis of aortic graft infection: A case definition by the management of aortic graft infection collaboration (MAGIC). Eur. J. Vasc. Endovasc. Surg. 52, 758–763 (2016).
Bruggink, J. L. et al. Accuracy of FDG-PET-CT in the diagnostic work-up of vascular prosthetic graft infection. Eur. J. Vasc. Endovasc. Surg. 40, 348–354 (2010).
Husmann, L. et al. Comparing diagnostic accuracy of (18)F-FDG-PET/CT, contrast enhanced CT and combined imaging in patients with suspected vascular graft infections. Eur. J. Nucl. Med. Mol. Imaging. 46, 1359–1368 (2019).
Fukuchi, K. et al. Detection of aortic graft infection by fluorodeoxyglucose positron emission tomography: Comparison with computed tomographic findings. J. Vasc. Surg. 42, 919–925 (2005).
Kim, S. J., Lee, S. W., Jeong, S. Y., Pak, K. & Kim, K. A systematic review and meta-analysis of (18)F-fluorodeoxyglucose positron emission tomography or positron emission tomography/computed tomography for detection of infected prosthetic vascular grafts. J. Vasc. Surg. 70, 307–313 (2019).
Reinders Folmer, E. I. et al. A systematic review and meta-analysis of (18)F-fluoro-d-deoxyglucose positron emission tomography interpretation methods in vascular graft and endograft infection. J. Vasc. Surg. 72, 2174–2185 (2020).
Husmann, L. et al. The role of FDG PET/CT in therapy control of aortic graft infection. Eur. J. Nucl. Med. Mol. Imaging. 45, 1987–1997 (2018).
Husmann, L. et al. (1)(8)F-FDG PET/CT for therapy control in vascular graft infections: A first feasibility study. J. Nucl. Med. 56, 1024–1029 (2015).
Pfannenberg, C. et al. Practice-based evidence for the clinical benefit of PET/CT-results of the first oncologic PET/CT registry in Germany. Eur. J. Nucl. Med. Mol. Imaging. 46, 54–64 (2019).
Pereira, A. M., Husmann, L., Sah, B. R., Battegay, E. & Franzen, D. Determinants of diagnostic performance of 18F-FDG PET/CT in patients with fever of unknown origin. Nucl. Med. Commun. 37, 57–65 (2016).
Mikail, N. et al. (18)F-FDG-PET/CT imaging to diagnose septic emboli and mycotic aneurysms in patients with endocarditis and cardiac device infections. Curr. Cardiol. Rep. 20, 14 (2018).
Husmann, L. et al. Diagnostic accuracy of PET/CT and contrast enhanced CT in patients with suspected infected aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 59, 972–981 (2020).
Frenkel Rutenberg, T. et al. The role of 18F-fluorodeoxyglucose positron-emission tomography/computed tomography in the diagnosis of postoperative hardware-related spinal infections. Isr. Med. Assoc. J. 21, 532–537 (2019).
Kim, J., Feller, E. D., Chen, W., Liang, Y. & Dilsizian, V. FDG PET/CT for early detection and localization of left ventricular assist device infection: Impact on patient management and outcome. JACC Cardiovasc. Imaging. 12, 722–729 (2019).
Priftakis, D., Riaz, S., Zumla, A. & Bomanji, J. Towards more accurate (18)F-fluorodeoxyglucose positron emission tomography ((18)F-FDG PET) imaging in active and latent tuberculosis. Int. J. Infect. Dis. 92S, S85–S90 (2020).
Husmann, L. et al. PET/CT in therapy control of infective native aortic aneurysms. Sci. Rep. 11, 5065 (2021).
Ben Shimol, J. et al. The utility of PET/CT in large vessel vasculitis. Sci. Rep. 10, 17709 (2020).
Hasse, B. et al. Vascular graft infections. Swiss Med. Wkly. 143, w13754 (2013).
Eskian, M. et al. Effect of blood glucose level on standardized uptake value (SUV) in (18)F- FDG PET-scan: a systematic review and meta-analysis of 20,807 individual SUV measurements. Eur. J. Nucl. Med. Mol. Imaging. 46, 224–237 (2019).
Wan, M. T. et al. Prevalence of clinically significant incidental findings by whole-body fludeoxyglucose F 18 positron emission tomography/computed tomography scanning in moderate-to-severe psoriasis patients participating in clinical trials. J. Am. Acad. Dermatol. 80, 1630–1639 (2019).
Nijhuis, A. A. G. et al. False-positive results and incidental findings with annual CT or PET/CT surveillance in asymptomatic patients with resected stage III melanoma. Ann. Surg. Oncol. 26, 1860–1868 (2019).
Adams, S. J., Rakheja, R., Bryce, R. & Babyn, P. S. Incidence and economic impact of incidental findings on (18)F-FDG PET/CT imaging. Can. Assoc. Radiol. J. 69, 63–70 (2018).
Hinton, W. et al. Incidence and prevalence of cardiovascular disease in English primary care: A cross-sectional and follow-up study of the Royal College of General Practitioners (RCGP) Research and Surveillance Centre (RSC). BMJ Open 8, e020282 (2018).
Hadad, Z. S. H., Afzelius, P., Sorensen, S. M. & Jurik, A. G. Clinical relevance of 18F-FDG-PET/CT incidental findings. Dan. Med. J. 67, 1–10 (2020).
Keidar, Z., Engel, A., Hoffman, A., Israel, O. & Nitecki, S. Prosthetic vascular graft infection: The role of 18F-FDG PET/CT. J. Nucl. Med. 48, 1230–1236 (2007).
Spacek, M., Belohlavek, O., Votrubova, J., Sebesta, P. & Stadler, P. Diagnostics of “non-acute” vascular prosthesis infection using 18F-FDG PET/CT: Our experience with 96 prostheses. Eur. J. Nucl. Med. Mol. Imaging. 36, 850–858 (2009).
Sah, B. R. et al. Diagnostic performance of F-FDG-PET/CT in vascular graft infections. Eur. J. Vasc. Endovasc. Surg. 49(4), 455–464 (2015).
Hess, S. FDG-PET/CT in fever of unknown origin, bacteremia, and febrile neutropenia. PET Clin. 15, 175–185 (2020).
Wenter, V. et al. The diagnostic value of [(18)F]FDG PET for the detection of chronic osteomyelitis and implant-associated infection. Eur. J. Nucl. Med. Mol. Imaging. 43, 749–761 (2016).
O’Sullivan, J. W., Muntinga, T., Grigg, S. & Ioannidis, J. P. A. Prevalence and outcomes of incidental imaging findings: Umbrella review. BMJ 361, k2387 (2018).
Acknowledgements
We are grateful to our patients for their participation in the study. We thank C. Mueller/S. Buergin, study nurses and Ch. Laich /C. Voegtli for administrative assistance. The members of the VASGRA Cohort Study are (in alphabetical order): B. Hasse (PI), N. Eberhard, M. Hoffmann, L. Husmann, R. Kopp, B. Ledergerber, Z. Rancic, C.A. Mestres, R. Zbinden, A. Zinkernagel, A. Zimmermann.
Funding
This study was financed within the framework of the Vascular Graft Cohort Study (VASGRA), supported by the Swiss National Science Foundation (SNF) Grant 320030_184918/1. This work was also supported by the Clinical Research Priority Program of the University of Zurich for the CRPP Precision medicine for bacterial infections. M.H. is a recipient of grants from GE Healthcare, grants for translational and clinical cardiac and oncological research from the Alfred and Annemarie von Sick Grant legacy, and grants from the Artificial Intelligence in oncological Imaging Network by the University of Zurich. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
B.H. and L.H. designed the study. L.H., B.L., and B.H. analysed the data. L.H. wrote the first draft, and L.H. and B.H. wrote the final version of the manuscript. The remaining investigators (N.E., M.W.H., A.M., H.G., M.M., C.A.M, Z.R., A.Z.) contributed to data collection and interpretation of the data, reviewed drafts of the manuscript, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Husmann, L., Eberhard, N., Huellner, M.W. et al. Impact of unknown incidental findings in PET/CT examinations of patients with proven or suspected vascular graft or endograft infections. Sci Rep 11, 13747 (2021). https://doi.org/10.1038/s41598-021-93331-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93331-4
- Springer Nature Limited