Abstract
The aim of this study was to investigate the association between maternal physical activity (PA) before and during pregnancy and sleep and developmental problems in 1-year-old infants. We used data from a nationwide cohort study in Japan that registered 103,062 pregnancies between 2011 and 2014. Participants were asked about their PA before and during pregnancy, and the sleep and development of their children at the age of 1 year. Maternal PA was estimated using the International Physical Activity Questionnaire and was expressed in METs per week. We defined scores below the cut-off points of the Ages and Stages Questionnaire (ASQ) as abnormal for infant development. Based on the levels of PA before or during pregnancy, the participants were divided into five groups. In mothers with higher PA levels, the risk ratio for bedtime after 22:00 or abnormal ASQ scores in their 1-years-old infants were lower. These associations were observed for PA before and during pregnancy. Higher levels of maternal PA, both before and during pregnancy, may reduce sleep and developmental problems in infants.
Similar content being viewed by others
Introduction
Many previous studies have reported that maternal physical activity (PA) and exercise during pregnancy are associated with decreases in various perinatal outcomes, such as gestational diabetes mellitus (GDM)1, hypertensive disorders of pregnancy (HDP)2, and risk for cesarean section3,4. In recent years, a positive association between PA during pregnancy and infant development has been reported. Two review articles in 2018 concluded that PA during pregnancy was associated with improved language development5 and total neurodevelopment6. To our knowledge, no published studies have reported the association between maternal PA or exercise before pregnancy and infant neurodevelopment.
Recently, the importance of preconception care has become more recognized7,8,9. For example, moderate exercise prior to conception is recommended by the American College of Obstetricians and Gynecologists8. However, the publication focused on the benefits of exercising for improving obesity and reducing perinatal complications, and the statement did not mention infant development. It has also been reported that exercise before pregnancy reduces GDM10 . GDM increases the risk of developmental disorders11; therefore, the level of PA or exercise during preconception may affect infant development. Children with developmental disorders, such as autism, tend to have sleeping problems, including frequent awakening, crying during the night, and short sleep time due to late bedtime12,13. These children also tend to experience developmental delays during early infancy14. To our knowledge, no published studies have reported the effects of maternal PA before or during pregnancy on infant sleep. We hypothesize that higher maternal PA before and during pregnancy may improve sleep and neurodevelopment in infants.
This study aimed to investigate the association between maternal PA before and during pregnancy, and infant sleep and developmental problems at 1-year-old using large-scale data.
Results
The baseline characteristics of the participants, along with the available data on maternal PA before pregnancy, are shown in Table 1. The characteristics of the participants with available data during pregnancy are shown in Table S1. The median (interquartile range) levels of PA before and during pregnancy were 854 (196–2975) METs-min/week and 497 (63–1386) METs-min/week, respectively.
Association of maternal PA before and during pregnancy with sleep problems in 1-year-old infants
Low levels of maternal PA before and during pregnancy were associated with an increased risk ratio for bedtime after 22:00 but were not associated with other sleep outcomes (Tables 2 and 3). The risk ratio of bedtime after 22:00 in the group with the highest levels of PA (Quartile 4) both before and during pregnancy was lower than the reference group (PA before pregnancy, RR = 0.91, 95% CI = 0.87–0.95; PA during pregnancy, RR = 0.88, 95% CI = 0.84–0.92).
Association of maternal PA before and during pregnancy with development in 1-year-old infants
Low levels of maternal PA both before and during pregnancy were associated with an increased risk of abnormal ASQ scores. Compared to the reference PA group before pregnancy, the group with the lowest levels of PA (PA = 0) had higher risk ratios of abnormal scores in the following domains of the ASQ: fine motor skills (RR = 1.15, 95% CI = 1.05–1.26), problem-solving (RR = 1.20, 95% CI = 1.09–1.33), and personal–social skills (RR = 1.29, 95% CI = 1.04–1.60) (Table 2).
Correspondingly, the risk ratios of abnormal scores for different domains of the ASQ were lower in the group with highest levels of PA (quartile 4) before pregnancy: fine motor skills (RR = 0.81, 95% CI = 0.73–0.90), problem-solving (RR = 0.86, 95% CI = 0.78–0.96), and overall skills (RR = 0.84, 95% CI = 0.79–0.90).
Similar associations were found in the analysis of PA during pregnancy (Table 3). Compared to the reference group for PA during pregnancy, the group with the lowest PA levels (PA = 0) showed higher risk ratios of abnormal scores in the following ASQ domains: fine motor skills (RR = 1.14, 95% CI = 1.04–1.25), problem-solving (RR = 1.14, 95% CI = 1.03–1.25), personal–social skills (RR = 1.27, 95% CI = 1.03–1.58), and overall skills (RR = 1.09, 95% CI = 1.03–1.16).
Conversely, in the group with the highest PA levels during pregnancy (quartile 4), the risk ratios of abnormal ASQ scores were lower in the following domains: fine motor skills (RR = 0.87, 95% CI = 0.78–0.97), problem-solving (RR = 0.86, 95% CI = 0.77–0.96), and overall skills (RR = 0.89, 95% CI = 0.84–0.95).
In other domains of the ASQ, including communication and gross motor skills, maternal PA both before and during pregnancy was not associated with significant risk ratios of abnormal scores.
The association between the risk ratios of abnormal ASQ scores and maternal PA levels, both before and during pregnancy, did not change in the subgroup analysis that excluded women with HDP and GDM (Table S2).
Discussion
In the present study, lower maternal PA levels before and during pregnancy increased the risk ratios of abnormal scores on the infants’ ASQ at 1 year of age. Higher maternal PA levels were associated with lower risk ratios of abnormal ASQ scores. Similarly, maternal PA levels before and during pregnancy were inversely associated with infant late bedtime at or after 22:00, as shown by the risk ratio. However, other sleep outcomes were not associated with maternal PA levels. This is the first study to show that maternal PA levels before pregnancy influence measures of development and concur with previous findings associated with PA during pregnancy. Higher PA levels during preconception may decrease the risk of developmental delay.
Regarding infant sleep problems, lower maternal PA levels before and during pregnancy were associated exclusively with late bedtime in 1-year-old infants. In this study, the proportion of infants who fell asleep after 22:00 was approximately 20%, which is a larger percentage than other sleep outcomes. Thus, a small but significant difference in late bedtime was detected. A high level of maternal activity during pregnancy has been reported to improve maternal sleep15,16. The sleep cycle develops from the fetal period17, and the association between maternal sleep during pregnancy and infants’ sleep has also been reported18,19. Therefore, maternal PA during pregnancy may affect infants’ sleep through maternal sleep. No other studies have addressed the direct association between maternal PA and infant sleep patterns. Further investigations are required to evaluate these associations.
This is the first study to show that maternal PA before pregnancy may influence infant developmental outcomes. Regarding PA during pregnancy, there have been many previous studies that reported an association between PA during pregnancy and language development20,21,22. The association between PA during pregnancy, motor function, and social skills remains inconclusive5,6. A recent RCT study reported a positive association between maternal exercise and infant neuromotor outcomes at 1- month-old23. Although there was a significant association between maternal PA and child development, it was also reported that the association became insignificant as the child matured21,24. Future studies should investigate the association between maternal PA before and during pregnancy and development in older children.
There are several hypotheses on how maternal PA before and during pregnancy affects infant neurodevelopment. The first hypothesis involves maternal inflammation, which affects fetal neurodevelopment in utero and may cause developmental disorders25. One study reported that exercise intervention in pregnant women reduced inflammatory cytokines26. Therefore, high maternal PA levels may protect fetal neurodevelopment from inflammation.
The second hypothesis is that maternal PA directly affects neurodevelopment in infants. In an experiment with mice and rats, exercise during pregnancy improved neurogenesis in the hippocampus, memory, and learning outcomes27,28,29,30,31. From this study, it can be inferred that for humans, PA during pregnancy may have a beneficial influence on fetal neurodevelopment.
The third hypothesis is that maternal activity may stimulate fetal sensory systems, such as vestibular function. A study of preterm infants reported that auditory, tactile, visual, and vestibular interventions increased nipple feeding and decreased the length of infant hospitalization32. As fetal vestibular function develops from early pregnancy33,34, maternal PA may stimulate the fetal vestibular system to positively affect neurodevelopment.
Perinatal complications, such as GDM, HDP, and perinatal depression, have negative effects on child neurodevelopment1,2,35,36. These complications are known risk factors of developmental disorders11. However, in our subgroup analysis, which excluded cases of HDP and GDM, an association between abnormalities in ASQ scores and maternal PA before and during pregnancy was found. This finding implies that HDP and GDM may not be the only complications associated with maternal PA before and during pregnancy.
This study has several limitations. First, this was an observational study, so there could be unmeasured confounding factors, such as parental life rhythm or sleep cycle. Second, maternal PA and infant outcomes (infant sleep problems and ASQ scores) were evaluated using a self-reported questionnaire, so there could be some bias. In particular, maternal PA before pregnancy was reported at recruitment in the first trimester of pregnancy. On the other hand, the strength of the present study was that it was based on national data. Additionally, this was the first study to focus on the association between maternal PA before pregnancy and infant development.
In conclusion, lower maternal PA before or during pregnancy was associated with negative effects on infant development and increased risk of late bedtimes in 1-year-old infants. In contrast, higher maternal PA before or during pregnancy may have positive effects on infant development and decrease the risk of late bedtimes in 1-year-old infants.
Methods
Research ethics
The study protocol was approved by the Ministry of the Environment’s Institutional Review Board on Epidemiological Studies (No. 100406001) and by the Ethics Committee of all participating institutions: the National Institute for Environmental Studies that leads the Japan Environment and Children’s Study (JECS), the National Center for Child Health and Development, Hokkaido University, Sapporo Medical University, Asahikawa Medical College, Japanese Red Cross Hokkaido College of Nursing, Tohoku University, Fukushima Medical University, Chiba University, Yokohama City University, University of Yamanashi, Shinshu University, University of Toyama, Nagoya City University, Kyoto University, Doshisha University, Osaka University, Osaka Medical Center and Research Institute for Maternal and Child Health, Hyogo College of Medicine, Tottori University, Kochi University, University of Occupational and Environmental Health, Kyushu University, Kumamoto University, University of Miyazaki, and University of Ryukyu. Written informed consent, which also included a follow-up study of children after birth, was obtained from all participants. All methods were performed in accordance with approved guidelines.
Study participants
The data used in this study were obtained from the JECS, an ongoing large-scale cohort study. The JECS was designed to follow children from the prenatal period to the age of 13 years. The detailed protocol of the study and the baseline profile of participants in the JECS have been previously reported previously37,38. The participants answered a questionnaire about lifestyle and behavior twice during pregnancy. The questionnaire completed at recruitment was referred to as M-T1, and the questionnaire completed later during mid- and late pregnancy was M-T2. The mean gestational weeks (SD) at the time of responding to M-T1 and M-T2 were 16.4 (8.0) and 27.9 (6.5) weeks, respectively. Participants also answered a questionnaire about their offspring one year after delivery (C-1y).
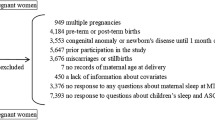
Between 2011 and 2014, 103,062 pregnant women were recruited from 15 regions throughout Japan (Fig. 1). Of these, we excluded 26,694 pregnancies due to the following reasons: previous participation in the study (n = 5647), multiple fetuses (n = 949), miscarriage or stillbirth (n = 3,676), congenital anomaly or disease at 1 month of age (n = 3553), missing information on maternal age at delivery (n = 7), delivery before 37 weeks or after 42 weeks of gestation (n = 4184), lack of information about maternal PA in the M-T1 and M-T2 (n = 1109), and no response to questions about children’s sleep and development at C-1y (n = 7569). The remaining 76,368 participants (74,971 with M-T1 data and 72,700 with M-T2 data) were included in the analysis.
Exposure: maternal PA
We used the Japanese short version of the International Physical Activity Questionnaire (IPAQ) to evaluate maternal PA, for which test–retest reliability and criterion validity were reported elsewhere39,40. Participants reported their mean PA per week before pregnancy on the M-T1 questionnaire based on recall and their mean PA per week during pregnancy on the M-T2 questionnaire. We calculated PA in terms of metabolic equivalent of a task (MET), measured as the number of minutes per week (METs-min/week)39. PA, as defined in the IPAQ, includes all activities of daily life, such as work, housework, and leisure activities.
We divided the participants into five groups based on their level of PA before pregnancy. We also divided the participants into five groups based on their levels of PA during pregnancy. In each of the five groups, the “PA = 0” group consisted of participants whose PA was 0. The other participants were divided into four groups using PA quartile points. The groups were labeled Quartiles 1–4 in ascending order of PA. Quartile 1 referred to the group with the lowest PA levels among the four groups. Quartile 4 referred to the group with the highest PA levels. To visualize the effects when the amount of activity was very low, we defined the Quartile 1 groups as the reference groups for the purpose of statistical analysis instead of the PA = 0 groups.
Outcome 1: infant sleeping problems
One year after delivery, information on infant sleep habits was collected via parent-reported questionnaires (C-1y). The participants answered questions regarding their infant’s sleep time in the previous 24 h, in 30-min increments. They were also asked whether their children cried at night, and if so, the crying frequency (“rarely,” “1–3 times in a month,” “1–2 times in a week,” “3–4 times in a week,” “5 times in a week or more”) was reported. In this analysis, we focused on five points. First, we determined the number of nocturnal awakenings from maternal responses to infants’ sleeping periods. We defined ≥ 3 awakenings as too many because a previous study reported that the upper limit of the number of awakenings during the night was 2.5 for 1-year-old infants41. Second, we determined whether the infants awoke more than once and whether they stayed awake for more than 1 h during the night. If so, these were defined as unusual. Third, we analyzed the duration of nighttime sleep (20:00–07:59). We regarded less than 8 h of sleep as too short because past research reported that the mean duration of sleep for this age group was 8.3 h41. Fourth, we determined the infants’ bedtime. In this study, about 65% of 1-year-old infants slept later than 21:00, and about 20% slept later than 22:00. Therefore, we defined bedtime after 22:00 as too late. Fifth, we obtained information about crying at night in the past month. If the mother answered that her infant cried during the night, and the frequency of crying at night was more than five times per week, we defined the case as “crying at night”.
Outcome 2: infant development
We used the Japanese version of the Ages and Stages Questionnaire (ASQ), third edition, to evaluate infant development. The C-1y questionnaire included ASQ. ASQ captures developmental delay in five domains: communication, gross motor skills, fine motor skills, problem-solving, and personal–social characteristics. The answer to each question is one of the following: “yes,” “sometimes,” or “not yet.” The scores were 10, 5, and 0 points, respectively. Each ASQ domain was composed of six questions, and the total score ranged from 0 to 60. The cut-off point for each domain in the Japanese version was 2SD below the mean, and all the cut-off points were determined by age groups in a previous study42. The cut-off points at 1-year-old are as follows: communication, 4.53; gross motor skill, 9.43; fine motor skill, 25.47; problem solving, 15.37; and personal-social characteristics, 4.95. The outcomes were defined as whether the score was less than the cut-off point for each ASQ domain and whether the score was less than the cut-off point of any one of the five ASQ domains.
Covariates
Information on maternal age at delivery, pre-pregnancy body mass index (BMI), parity, gestational age at birth, infertility treatment, type of delivery, current history of hypertensive disorders of pregnancy and diabetes or gestational diabetes, infant birth weight, and infant sex were collected from medical records. Information about smoking habits, alcohol consumption, educational background, household income, maternal psychological distress at 1 year after delivery, doctor diagnosis of asthma and atopic dermatitis in children up to 1 year of age, and feeding status were collected via self-administered questionnaires. Maternal depression has been reported to affect infant development43. In the present study, we did not know whether the participants had a mental illness after delivery. Thus, maternal psychological distress was assessed using the Kessler 644,45 questionnaire at C-1y. In concordance with previous studies, participants with a score of five or more were categorized as having distress46.
Statistical analyses
We used a log-binominal regression model to explore the association of maternal PA with each outcome and to estimate the risk ratio (RR) of each outcome and the 95% confidence intervals (CIs). We initially adjusted for maternal age at delivery and then further adjusted for smoking habits (never smokers, ex-smokers who quit before pregnancy, smokers during early pregnancy), alcohol consumption (never drinkers, ex-drinkers who quit before pregnancy, drinkers during early pregnancy), pre-pregnancy BMI (< 18.5, 18.5–24.9, ≥ 25.0 kg/m2), parity (0, ≥ 1), infertility treatment (no ovulation stimulation/artificial insemination by sperm from husband, assisted reproductive technology), type of delivery (vaginal or cesarean section), gestational age at birth (37–38, 39–41 weeks), infant sex (boys, girls), psychological distress at 1 year after delivery (yes, no), doctor diagnosis of asthma and atopic dermatitis at 1 year of age, and feeding (breast milk, formula, both). The covariates to be added to the multivariate model were determined by referring to the previous literature as potential risk factors for developmental disorders11,47. Due to the large sample size in this study, we used the risk factors contained in the dataset in the multivariate model as covariates whenever possible. However, since there were many missing data on household income and educational background, we excluded them from the covariates of the multivariate model after confirming that the results did not change significantly even if they were included in the model. We did not complete the missing data. Thus, the multivariate analysis was limited to those participants that had all the covariate data.
We also performed a subgroup analysis excluding women with HDP and GDM to investigate the influence of these factors on infant development.
In this study, we used a fixed dataset “jecs-an-20180131,” which was released in March 2018. Stata version 15 (StataCorp LP, College Station, TX, USA) was used for all statistical analyses.
The statistical analyses of this study were conducted in a manner that was similar to that of our previous study48.
References
Russo, L. M., Nobles, C., Ertel, K. A., Chasan-Taber, L. & Whitcomb, B. W. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet. Gynecol. 125, 576–582 (2015).
Barakat, R. et al. Exercise during pregnancy protects against hypertension and macrosomia: randomized clinical trial. Am. J. Obstet. Gynecol. 214(649), e1-649.e8 (2016).
Di Mascio, D., Magro-Malosso, E. R., Saccone, G., Marhefka, G. D. & Berghella, V. Exercise during pregnancy in normal-weight women and risk of preterm birth: a systematic review and meta-analysis of randomized controlled trials. Am. J. Obstet. Gynecol. 215, 561–571 (2016).
Owe, K. M., Nystad, W., Stigum, H., Vangen, S. & Bø, K. Exercise during pregnancy and risk of cesarean delivery in nulliparous women: a large population-based cohort study. Am. J. Obstet. Gynecol. 215(791), e1-791.e13 (2016).
Álvarez-Bueno, C. et al. Pregnancy leisure physical activity and children’s neurodevelopment: a narrative review. BJOG 125, 1235–1242 (2018).
Niño Cruz, G. I., Ramirez Varela, A., da Silva, I. C. M., Hallal, P. C. & Santos, I. S. Physical activity during pregnancy and offspring neurodevelopment: a systematic review. Paediatr. Perinat. Epidemiol. 32, 369–379 (2018).
Public Health Agency of Canada. Family-Centred Maternity and Newborn Care: National Guidelines. (2018).
ACOG Committee Opinion #762. Obstet. Gynecol. 133, e78–e89 (2019).
Shawe, J. et al. Preconception care policy, guidelines, recommendations and services across six European countries: Belgium (Flanders), Denmark, Italy, the Netherlands, Sweden and the United Kingdom. Eur. J. Contracept. Reprod. Heal. Care. 20, 77–87 (2015).
Mijatovic-Vukas, J. et al. Associations of diet and physical activity with risk for gestational diabetes mellitus: a Systematic review and meta-analysis. Nutrients 10, 698 (2018).
Wang, C., Geng, H., Liu, W. & Zhang, G. Prenatal, perinatal, and postnatal factors associated with autism: a meta-analysis. Medicine 96, 1–7 (2017).
Humphreys, J. S. et al. Sleep patterns in children with autistic spectrum disorders: a prospective cohort study. Arch. Dis. Child. 99, 114–118 (2014).
Reynolds, A. M. et al. Sleep problems in 2-to 5-year-olds with autism spectrum disorder and other developmental delays. Pediatrics 143, e20180492 (2019).
Lai, M. C., Lombardo, M. V. & Baron-Cohen, S. Autism. Lancet. 383, 896–910 (2014).
Borodulin, K. et al. Physical activity and sleep among pregnant women. Paediatr Perinat Epidemiol. 24, 45–52 (2010).
Tan, L., Zou, J., Zhang, Y., Yang, Q. & Shi, H. A longitudinal study of physical activity to improve sleep quality during pregnancy. Nat. Sci. Sleep 12,431–442 (2020).
Mirmiran, M., Maas, Y. G. H. & Ariagno, R. L. Development of fetal and neonatal sleep and circadian rhythms. Sleep Med. Rev. 7, 321–334 (2003).
Nakahara, K. et al. Association of maternal sleep before and during pregnancy with preterm birth and early infant sleep and temperament. Sci. Rep. 10, 1–14 (2020).
Huang, Y. J. et al. [Association of maternal nocturnal sleep throughout pregnancy with the early nocturnal sleep of infants]. Zhonghua er ke za zhi = Chinese J. Pediatr. 57, 608–613 (2019).
Esteban-Cornejo, I. et al. Maternal physical activity before and during the prenatal period and the offspring’s academic performance in youth. The up and down study. J. Matern. Neonatal Med. 29, 1414–1420 (2016).
Domingues, M. R. et al. Physical activity during pregnancy and offspring neurodevelopment and iq in the first 4 years of life. PLoS ONE 9, e110050 (2014).
Clapp, J. F., Simonian, S., Lopez, B., Appleby-Wineberg, S. & Harcar-Sevcik, R. The one-year morphometric and neurodevelopmental outcome of the offspring of women who continued to exercise regularly throughout pregnancy. Am. J. Obstet. Gynecol. 178, 594–599 (1998).
McMillan, A. G., May, L. E., Gaines, G. G., Isler, C. & Kuehn, D. Effects of aerobic exercise during pregnancy on 1-month infant neuromotor skills. Med. Sci. Sports Exerc. 51, 1671–1676 (2019).
Jukic, A. M. Z. et al. Physical activity during pregnancy and language development in the offspring. Paediatr. Perinat. Epidemiol. 27, 283–293 (2013).
Estes, M. L. & McAllister, A. K. Maternal immune activation: implications for neuropsychiatric disorders. Science 353, 772–777 (2016).
Acosta-Manzano, P. et al. Influence of a concurrent exercise training intervention during pregnancy on maternal and arterial and venous cord serum cytokines: the GESTAFIT project. J. Clin. Med. 8, 1862 (2019).
Kim, H., Lee, S. H., Kim, S. S., Yoo, J. H. & Kim, C. J. The influence of maternal treadmill running during pregnancy on short-term memory and hippocampal cell survival in rat pups. Int. J. Dev. Neurosci. 25, 243–249 (2007).
Akhavan, M. M. et al. Serotonergic and noradrenergic lesions suppress the enhancing effect of maternal exercise during pregnancy on learning and memory in rat pups. Neuroscience 151, 1173–1183 (2008).
Bick-Sander, A., Steiner, B., Wolf, S. A., Babu, H. & Kempermann, G. Running in pregnancy transiently increases postnatal hippocampal neurogenesis in the offspring. Proc. Natl. Acad. Sci. USA. 103, 3852–3857 (2006).
Lee, H. H. et al. Maternal swimming during pregnancy enhances short-term memory and neurogenesis in the hippocampus of rat pups. Brain Dev. 28, 147–154 (2006).
Parnpiansil, P. Exercise during pregnancy increases hippocampal brain-derived neurotrophic factor mRNA expression and spatial learning in neonatal rat pup. Neurosci. Lett. 352, 45–48 (2003).
Dnsc, R. C. W. & Silvestri, J. M. Effect of auditory, tactile, visual, and vestibular intervention on length of stay, alertness, and feeding progression in preterm infants. Dev. Med. Child Neurol. 44, 91–97 (2002).
Lim, R. & Brichta, A. M. Anatomical and physiological development of the human inner ear. Hear. Res. 338, 9–21 (2016).
Richard, C. et al. Inner ear ossification and mineralization kinetics in human embryonic development-microtomographic and histomorphological study. Sci. Rep. 7, 1–11 (2017).
Vargas-Terrones, M., Barakat, R., Santacruz, B., Fernandez-Buhigas, I. & Mottola, M. F. Physical exercise programme during pregnancy decreases perinatal depression risk: a randomised controlled trial. Br. J. Sports Med. 53, 348–353 (2019).
Hinman, S. K., Smith, K. B., Quillen, D. M. & Smith, M. S. Exercise in pregnancy: a clinical review. Sports Health 7, 527–531 (2015).
Kawamoto, T. et al. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health 14, 1–8 (2014).
Michikawa, T. et al. Baseline profile of participants in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 28, 99–104 (2018).
Craig, C. L. et al. International physical activity questionnaire: 12-Country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
Murase, N. et al. Validity and reliability of Japanese version of international physical activity questionnaire. J Health Welfare Stat. 49, 1–9 (2012) ([In Japanese]).
Galland, B. C., Taylor, B. J., Elder, D. E. & Herbison, P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med. Rev. 16, 213–222 (2012).
Mezawa, H. et al. Psychometric profiles of the ages and stages questionnaires ,Japanese translation. Pediatr. Int. 61, 1086–1095 (2019).
Abdollahi, F., Abhari, F. R. & Zarghami, M. Post-partum depression effect on child health and development. Acta Med. Iran. 55, 109–114 (2017).
Kessler, R. C. et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry. 60, 184–189 (2003).
Toshia, F., Norito, K., Mari, S. & Yutaka, O. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 17, 152–158 (2008).
Sakurai, K., Nishi, A., Kondo, K., Yanagida, K. & Kawakami, N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin. Neurosci. 65, 434–441 (2011).
Walker, S. P., Wachs, T. D. & Gardner, J. M. Child development: risk factors for adverse outcomes in developing countries. Lancet 369, 145–157 (2007).
Nakahara, K. et al. Non-reassuring foetal status and sleep problems in 1-year-old infants in the Japan Environment and Children’s Study: a cohort study. Sci. Rep. 10, 1–7 (2020).
Acknowledgements
We would like to express our gratitude to all the participants of this study and all individuals involved in data collection. This work was inspired by other works supported by the RIKEN Healthcare and Medical Data Platform Project and JSPS KAKENHI (Grant Nos.: JP16H01880, JP16K13072, JP18H00994, JP18H03388).
Funding
The Japan Environment and Children’s Study was funded by the Ministry of Environment, Japan. The findings and conclusions of this article are solely the responsibility of the authors and do not represent the official views of the Ministry of the Environment.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design: S.M. Statistical analyses: T.M. Drafting of the manuscript and approval of final content: K.N., S.M., and T.M. Critical revision of the manuscript for important intellectual content and manuscript review: K.N., T.M., S.M., M.O., K.K. (Kiyoko Kato), M.S. (Masafumi Sanefuji), E.S., M.T., M.S. (Masayuki Shimono), T.K., S.O., K.K. (Koichi Kusuhara), and JECS group members.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakahara, K., Michikawa, T., Morokuma, S. et al. Influence of physical activity before and during pregnancy on infant’s sleep and neurodevelopment at 1-year-old. Sci Rep 11, 8099 (2021). https://doi.org/10.1038/s41598-021-87612-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87612-1
- Springer Nature Limited
This article is cited by
-
Factors influencing physical inactivity status among chinese pregnant women: a cross-sectional study
BMC Public Health (2022)