Abstract
Tuberculous meningitis (TBM) remains a serious disease for children and its risk factors of poor outcome remain unclear. Therefore, a retrospective study was conducted aiming to investigate the risk factors associated with poor outcome of childhood TBM. Between January 2006 and December 2019, consecutive children patients (≤ 15 years old) who had a diagnosis of TBM were included for the analysis. The demographic, clinical, laboratory, and radiographic data were collected from the electronic medical records retrospectively. Poor outcome was defined as death or transfer to a higher-level hospital. Patients were then divided into good and poor outcome groups. Subsequently, risk factors for poor outcome were estimated using univariate and multivariate logistic regression analysis. A total of 149 children with TBM was enrolled, twenty-two patients suffered poor outcome, including 16 transfers to a higher-level hospital and 6 deaths, and the remaining 127 patients were classified as good outcome group. Further multivariate analysis revealed that coma (age- and sex-adjusted OR = 6.425, 95% CI: 1.743, 23.676; P < 0.01) and cerebrospinal fluid (CSF) protein (> 1188.3 mg/L; age- and sex-adjusted OR = 4.680, 95% CI: 1.469, 14.902; P < 0.01) were associated with the poor outcome of childhood TBM. Childhood TBM remains to have a high mortality rate in China. High CSF protein and coma were identified as risk factors for poor outcome of childhood TBM. Hence, more attention is required to be paid to suspected patients with such characteristics, thus facilitating access to optimum treatment.
Similar content being viewed by others
Introduction
Currently, the situation of tuberculosis (TB) control in children has undergone many changes. First, the leading infectious agents causing death in children have shifted from rabies virus and M.tuberculosis to human immunodeficiency virus1. Second, during the past years, the annual notified incidence of childhood pulmonary TB was low (compared with that of adults) and decreased significantly2. However, TB caused by M.tuberculosis infection remains the most common bacterial infection in children and a serious public health threaten in China.
Tuberculous meningitis (TBM) is the most severe form of TB, leading to a high rate of mortality. In children, mortality rates of 15–29% were reported for TBM3,4,5. Recently, our findings demonstrated that the proportion of TBM among childhood TB in Shandong, China, is estimated at 9.4%, a remarkably high value required for effective intervention6. In addition, during the last decade, the trend in the proportion of TBM among childhood TB suggested a steady-state6. Therefore, a better management of childhood TBM is required to improve the current situation of TB patients, especially the survival rate.
It is well-known that delays in initiating therapy for TBM would increase mortality7. Unfortunately, the diagnosis of TBM in children is difficult. For example, routine microbiological examinations (such as smear and culture) show limited capacity in the diagnosis of the disease among children; polymerase chain reaction (PCR) has a moderate sensitivity in the diagnosis8, and a similar result was reported, when cerebrospinal fluid (CSF) Xpert was applied9; metagenomic next-generation sequencing is also tested in the diagnosis of TBM and presented with a moderate diagnostic performance10. The diagnosis remains a clinical challenge and this would contribute a significant delay in the initiation of anti-TB therapy, which may lead to a poor outcome. Hence, to characterize the risk factors associated with the poor outcome may improve the present situation in the management of childhood TBM.
The current study aims to investigate the risk factors for a poor outcome of TBM in children. There are few studies that address the factors associated with the outcome of TBM in this population. Our findings may be helpful in understanding the clinical characteristics of children patients with poor outcomes, and may improve the management of the disease.
Materials and methods
The study was approved by the Ethics Committee of Shandong Provincial Chest Hospital, Jinan, China (NO. 2020XKYYEC-29) and performed in compliance with Helsinki declaration. Due to the retrospective nature of the study design and anonymous data collection, written informed consent was waived by the Ethics Committee of Shandong Provincial Chest Hospital.
Between January 2006 and December 2019, consecutive children patients (≤ 15 years old) who had a diagnosis of TBM were included for the analysis. TBM was defined if one of the following criteria (modified from the criteria established by Marais et al.11) was met: (1) definite: acid fast bacilli (AFB, +) on cerebrospinal fluid (CSF) microscopy, or CSF TB-PCR( +), or M.tuberculosis cultured from CSF. (2) conclusive: symptoms and signs of meningitis and CSF findings (such as total white cell count > 5 cells × 106/L, protein > 0.45 g/L, glucose < 2.2 mmol/L, and CSF/serum glucose ratio < 0.5), plus at least one of the following (i) TB suggested by abnormal radiographic features (chest, or cerebral imaging), (ii) positive TB assays (such as AFB, PCR, and culture) using non-CSF samples. All patients were censored at death or discharge from our center.
The demographic, clinical, laboratory, and radiographic data were collected from the electronic medical records retrospectively. Poor outcome was defined as death or transfer to a higher-level hospital. Then, patients were divided into good and poor outcome groups and analyzed. Subsequently, risk factors for poor outcome were estimated in the study.
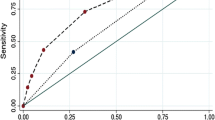
Statistical analysis were performed using SPSS version 16.0 (SPSS, Chicago, IL, USA). Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as count (percentages). Univariate and multivariate logistic regression analysis adjusted by age and sex were performed to determine risk factors for poor outcomes, and odds ratios (OR) and the corresponding 95% confidence interval (CI) were calculated12. Additionally, to make a better clinical understanding, continuous variables were transformed into categorical variables, based on cutoffs determined by the receiver operating characteristic curve (ROC) analysis. The goodness-of-fit was assessed using the Hosmer–Lemeshow test. A P value < 0.05 was considered significant.
Results
Patient characteristics
A total of 149 children was enrolled during the study period. Twenty-two patients suffered poor outcomes, including 16 transfers to a higher-level hospital and 6 deaths. Table 1 shows a comparison of clinical-pathological characteristics between patients with poor and good outcomes.
In general, 22 patients were grouped as poor outcome group, and the remaining 127 patients as good outcome group. The mean age and weight were 7.8 ± 5.3 years and 24.2 ± 16.0 kg, respectively. Of them, eighty-two patients (55.0%) were male and 120 (80.5%) were from rural areas. Additionally, other sites involved with TB were reported as pulmonary (45.0%), miliary (15.4%), lymph node (4.0%), and pleural (4.0%). Among them, 30 patients (good outcome group, n = 25; poor outcome group, n = 5) have been confirmed with TBM: CSF culture (+ , n = 24); CSF AFB (+ , n = 2); TB PCR (+ , n = 13); CSF Xpert (+ , n = 2).
The mean times of hospitalization were 2.1 ± 1.7, and the mean treatment delay was reported at 40 ± 61 days. Among the enrolled patients, 32 patients (21.5%) had a TB contact history and 128 patients (85.9%) were transferred from a teaching hospital. Almost all patients (96.0%) had inpatient therapy, over half (58.4%) had outpatient therapy, and a significant proportion (13.4%) were reported having self-treatment. In addition, a majority (76.5%) of patients had experienced antibiotics therapy and a few (20.8%) were administrated with anti-TB therapy.
The vital signs were as follows: temperature, 37.3 ± 0.9 °C; heart rate, 99.2 ± 21.5 beats/min; respiratory rate, 22.6 ± 3.0 breaths/min; systolic pressure, 106.9 ± 16.1 mmHg; diastolic pressure, 68.9 ± 11.5 mmHg. The symptoms were as follows: fever (88.6%), headache (51.7%), vomiting (48.3%), cough (20.1%), convulsion (16.8%), coma (14.8%), drowsiness (9.4%), and dizziness (3.4%). In addition, a total of 16 patients (10.7%) were reported with symptoms related to cranial nerve involvement: motor abnormalities (n = 7), speech difficulty (n = 4), swallowing difficulty (n = 1), and visual loss (n = 4).
T-SPOT.TB were tested in 38 patients and 26 (68.4%) of them had a positive result. Other lab examinations, such as blood cell count, flow cytometry, and CSF analysis, were shown in Table 1 and Supplementary Table 1.
Univariate and multivariate analysis
Table 1 shows the results of univariate analysis between poor and good outcome groups. It was found that poor outcome was associated with systolic pressure (OR = 1.025, 95% CI: 1.002, 1.048), frequency of hospitalization (OR = 0.437, 95% CI: 0.207, 0.924), self-treatment (OR = 3.027, 95% CI: 1.017, 9.005), CSF protein (OR = 1.001, 95% CI: 1.000, 1.001), CSF α-hydroxybutyrate dehydrogenase (α-HBDH, OR = 1.007, 95% CI:1.000, 1.014), and CSF IgA (OR = 1.043, 95% CI: 1.001, 1.085; all P < 0.05).
Further multivariate analysis (Hosmer–Lemeshow goodness-of-fit test: χ2 = 8.034, df = 8, P = 0.430) revealed that coma (age- and sex-adjusted OR = 6.425, 95% CI: 1.743, 23.676; P < 0.01) and CSF protein (> 1188.3 mg/L; age- and sex-adjusted OR = 4.680, 95% CI: 1.469, 14.902; P < 0.01) were associated with the poor outcome of childhood TBM (Table 2).
Discussion
To our knowledge, this study is the first assessing the risk factors associated with poor outcome in childhood TBM in China. Our findings were based on a moderate sample size and suggested that an increased level of CSF protein and coma were associated with the poor outcome in children with TBM. TBM treatment is more difficult and prone to failure than pulmonary TB. Our data may be useful to improve the current situation of childhood TBM.
Delays in treatment have limited influence on the outcome of the disease. As reported previously, delay in the treatment of TBM was associated with a poor outcome13. Besides, similar findings were also found by Verdon et al.14, and Sheu et al.15. However, these findings disagreed with our findings, our data demonstrated that no significant difference was observed in treatment delay between the poor and good outcome groups. Nevertheless, in the study, the treatment delay remains strongly suspected. Frequency of hospitalization was found to be associated with poor outcome in univariate analysis. On the one hand, the frequency of hospitalization may be associated with a prolonged period seeking an appropriate treatment. On the other hand, transfers between hospitals are more prone to support that these individuals have a more serious situation due to a delayed diagnosis or inappropriate treatment. Additionally, self-treatment also appeared to play a role in the treatment delay. However, this fact was not included in the final regression model.
Not surprisingly, coma is identified as a risk factor of poor outcome in our study. This may be explained that poor outcomes in TBM were largely confined to cases presenting in an advanced stage16. Similar observations were reported in several studies13,17,18. In our study, 22 (14.8%) of them had coma on arrival. In Romania, coma was noted in a similar proportion19. However, in low TB burden countries, this appears to be rare20. Although Glasgow coma scale has been introduced to evaluate the severity and predict the outcome of TBM21 and a low Glasgow coma scale (GCS) score on admission was associated with a poor prognosis, the accurate criteria (score cut-off) for this is not well characterized. For example, GCS (score: 3–8) is thought as an independent predictor of poor outcome in TBM patients22; the scale with ≤ 10 has a poor outcome23. In contrast, compared with Glasgow coma scale, coma as a symptom may be easy to use in the management of childhood TBM. Besides, if only death is defined as poor outcome, coma remains to be a risk factor for poor outcome of childhood TBM (data not shown).
Usually, a high level of CSF protein indicates disruption of the blood–brain barrier and the subarachnoid blockage of the CNS circulation in central nervous system involvement of tuberculosis, especially in tuberculous meningitis24,25,26. Besides, an elevated level of CSF protein is also known as an enhanced immunological reaction27. In the study, high level of CSF protein was identified as another risk factor for the poor outcome in children with TBM. As known, CSF examination of TBM patients showed low glucose, high protein, and pleocytosis17,28, and these CSF findings also served as criteria for the diagnosis of TBM. Previously, the association between CSF findings and outcome has been confirmed in adulthood TBM. For example, Hosoğlu et al. reported that high level of CSF protein was one of the five factors predicting the fatal outcome of TBM29. Similar finding was observed in our study. Our data suggested that high level of CSF protein is associated with poor outcome of childhood TBM. Besides this, several interesting findings about CSF protein were yielded recently. Such as faster normalization of CSF parameters (such as glucose, high protein, and pleocytosis) was associated with better outcome28; an increased level of CSF protein may cause more formation of basal exudates in patients with TBM, leading to cranial nerve involvement30.
The study has several limitations that should be taken into account. First, our study has a retrospective nature and a long inclusion period, during which diagnostic assays and treatment may have improved. Second, due to the observational and exploratory nature, the results may not be generalized to other settings. Third, due to the limited information collected from medical records and small sample size, our study did not address the relationship between GCS and outcome. Fourth, transfer to a higher-level hospital is defined as a poor outcome of childhood TBM. However, it does not mean that patient required transfer would experience death. Hence, our results should be interpreted with care. In a word, further analysis is needed to address the above mentioned questions and validate our findings in a large-scale prospective study.
Conclusions
During the last decade, childhood TBM remains to have a high mortality rate in China. The study identified several risk factors of poor outcome, such as high level of CSF protein and coma. Childhood TBM remains a severe problem to the public health and more attention are required to initiate anti-TB therapy timely.
References
Dong, Y. et al. Infectious diseases in children and adolescents in China: analysis of national surveillance data from 2008 to 2017. BMJ 369, m1043 (2020).
Yang, R. et al. The epidemiology of pulmonary tuberculosis in children in Mainland China, 2009–2015. Arch. Dis. Child. 105, 319–325 (2020).
Bang, N. D. et al. Clinical presentations, diagnosis, mortality and prognostic markers of tuberculous meningitis in Vietnamese children: a prospective descriptive study. BMC Infect. Dis. 16, 573 (2016).
Dhawan, S. R. et al. Predictors of neurological outcome of tuberculous meningitis in childhood: a prospective cohort study from a developing country. J. Child. Neurol. 31, 1622–1627 (2016).
Israni, A. V. et al. Tubercular meningitis in children: clinical, pathological, and radiological profile and factors associated with mortality. J. Neurosci. Rural Pract. 7, 400–404 (2016).
Wang, M. S., Wang, J. L. & Liu, X. J. Epidemiological trends in the form of childhood tuberculosis in a referral tuberculosis hospital in Shandong, China. Biomed. Res. Int. 2020, 6142567 (2020).
Boyles, T. H., Lynen, L. & Seddon, J. A. Tuberculous meningitis international research, C. Decision-making in the diagnosis of tuberculous meningitis. Wellcome Open Res. 5, 11 (2020).
Agarwal, S. et al. Comparative evaluation of IS6110 and protein antigen b PCR in cerebrospinal fluid for rapid diagnosis of tuberculous meningitis in children. J. Med. Microbiol. 69, 979–985 (2020).
Jyothy, A., Ratageri, V. H., Illalu, S., Fattepur, S. R. & Wari, P. K. The Utility of CSF Xpert MTB/RIF in diagnosis of tubercular meningitis in children. Indian J. Pediatr. 86, 1089–1093 (2019).
Wang, S. et al. The feasibility of metagenomic next-generation sequencing to identify pathogens causing tuberculous meningitis in cerebrospinal fluid. Front. Microbiol. 10, 1993 (2019).
Marais, S. et al. Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect. Dis. 10, 803–812 (2010).
Zhang, W., Han, C., Wang, M. S. & He, Y. Characteristics and factors associated with treatment delay in pleural tuberculosis. QJM 111, 779–783 (2018).
Hosoglu, S. et al. Predictors of outcome in patients with tuberculous meningitis. Int. J. Tuberc. Lung Dis. 6, 64–70 (2002).
Verdon, R., Chevret, S., Laissy, J. P. & Wolff, M. Tuberculous meningitis in adults: review of 48 cases. Clin. Infect. Dis. 22, 982–988 (1996).
Sheu, J. J., Yuan, R. Y. & Yang, C. C. Predictors for outcome and treatment delay in patients with tuberculous meningitis. Am. J. Med. Sci. 338, 134–139 (2009).
Kent, S. J., Crowe, S. M., Yung, A., Lucas, C. R. & Mijch, A. M. Tuberculous meningitis: a 30-year review. Clin. Infect. Dis. 17, 987–994 (1993).
Raberahona, M., Rakotoarivelo, R. A., Razafinambinintsoa, T., Andrianasolo, R. L. & Randria, M. J. Clinical features and outcome in adult cases of tuberculous meningitis in tertiary care hospital in Antananarivo, Madagascar. Biomed. Res. Int. 2017, 9316589 (2017).
Yasar, K. K., Pehlivanoglu, F. & Sengoz, G. Predictors of mortality in tuberculous meningitis: a multivariate analysis of 160 cases. Int. J. Tuberc. Lung Dis. 14, 1330–1335 (2010).
Miftode, E. G. et al. Tuberculous meningitis in children and adults: a 10-year retrospective comparative analysis. PLoS ONE 10, e0133477 (2015).
Christensen, A. S., Andersen, A. B., Thomsen, V. O., Andersen, P. H. & Johansen, I. S. Tuberculous meningitis in Denmark: a review of 50 cases. BMC Infect. Dis. 11, 47 (2011).
Gunes, A. et al. Clinical, radiological and laboratory findings in 185 children with tuberculous meningitis at a single centre and relationship with the stage of the disease. Ital. J. Pediatr. 41, 75 (2015).
Mo, X., Xu, X., Ren, Z., Guan, J. & Peng, J. Patients with tuberculous meningitis and hepatitis B co-infection have increased risk for antituberculosis drug-induced liver injury and poor outcomes. Infect. Dis. (Lond.) 52, 793–800 (2020).
Jaipuriar, R. S. et al. Early mortality among immunocompetent patients of tuberculous meningitis: a prospective study. Am. J. Trop. Med. Hyg. 101, 357–361 (2019).
Chaudhuri, A. & Behan, P. O. The clinical spectrum, diagnosis, pathogenesis and treatment of Hashimoto’s encephalopathy (recurrent acute disseminated encephalomyelitis). Curr. Med. Chem. 10, 1945–1953 (2003).
Haddad, N., McMinn, B. & Hartley, L. Headache meets neurology and psychiatry: a framework for diagnosis. Arch. Dis. Child. Educ. Pract. Ed. 101, 200–205 (2016).
van der Flier, M. et al. Vascular endothelial growth factor and blood-brain barrier disruption in tuberculous meningitis. Pediatr. Infect. Dis. J. 23, 608–613 (2004).
Griffiths, M. J., McGill, F. & Solomon, T. Management of acute meningitis. Clin. Med. (Lond.) 18, 164–169 (2018).
Faella, F. S. et al. Factors influencing the presentation and outcome of tuberculous meningitis in childhood. In Vivo 20, 187–191 (2006).
Hosoglu, S., Ayaz, C., Geyik, M. F., Kokoglu, O. F. & Ceviz, A. Tuberculous meningitis in adults: an eleven-year review. Int. J. Tuberc. Lung Dis. 2, 553–557 (1998).
Sharma, P., Garg, R. K., Verma, R., Singh, M. K. & Shukla, R. Incidence, predictors and prognostic value of cranial nerve involvement in patients with tuberculous meningitis: a retrospective evaluation. Eur. J. Intern. Med. 22, 289–295 (2011).
Author information
Authors and Affiliations
Contributions
M.S.W and X.J.L designed the study. M.S.W collected and analyzed the data. M.S.W wrote the paper. M.Z revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, MS., Zhao, M. & Liu, XJ. Risk factors for poor outcome in childhood tuberculous meningitis. Sci Rep 11, 8654 (2021). https://doi.org/10.1038/s41598-021-87082-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87082-5
- Springer Nature Limited
This article is cited by
-
Epidemiology, clinical presentation, and predictors of outcome in nontuberculous mycobacterial central nervous system infection: a systematic review
Tropical Medicine and Health (2023)
-
Ventriculoperitoneal shunt for tuberculous meningitis-associated hydrocephalus: long-term outcomes and complications
BMC Infectious Diseases (2023)