Abstract
The red blood cell distribution width (RDW) measures the variability in the size of circulating erythrocytes. Previous studies suggested a powerful correlation between RDW obtained from a standard complete blood count and cardiovascular diseases in both primary and secondary cardiovascular prevention. The current study aimed to evaluate the prognostic role of RDW in patients undergoing cardiac rehabilitation after myocardial revascularization and/or cardiac valve surgery. The study included 1.031 patients with available RDW levels, prospectively followed for a mean of 4.5 ± 3.5 years. The mean age was 68 ± 12 years, the mean RDW was 14.7 ± 1.8%; 492 patients (48%) underwent cardiac rehabilitation after myocardial revascularization, 371 (36%) after cardiac valve surgery, 102 (10%) after valve-plus-coronary artery by-pass graft surgery, 66 (6%) for other indications. Kaplan–Meier analysis and Cox hazard analysis were used to associate RDW with mortality. Kaplan–Meier analysis demonstrated worse survival curves free from overall (log-rank p < 0.0001) and cardiovascular (log-rank p < 0.0001) mortality in the highest RDW tertile. Cox analysis showed RDW levels correlated significantly with the probability of overall (HR 1.26; 95% CI 1.19–1.32; p < 0.001) and cardiovascular (HR 1.31; 95% CI 1.23–1.40; p < 0.001) mortality. After multiple adjustments for cardiovascular risk factors, hemoglobin, hematocrit, C-reactive protein, microalbuminuria, atrial fibrillation, glomerular filtration rate,left ventricular ejection fraction and number of exercise training sessions attended, the increased risk of overall (HR 1.10; 95% CI 1.01–1.27; p = 0.039) and cardiovascular (HR 1.13; 95% CI 1.01–1.34; p = 0.036)mortality with increasing RDW values remained significant. The RDW represents an independent predictor of overall and cardiovascular mortality in secondary cardiovascular prevention patients undergoing cardiac rehabilitation.
Similar content being viewed by others
Introduction
Red blood cell distribution width (RDW), obtained from a standard complete blood count, represents a measure of the variability in size of circulating erythrocytes and is indicated as the coefficient of variation of the erythrocyte size1. RDW is the ratio between standard deviation (SD) and mean of the mean corpuscular volume; the ratio is multiplied by 100 to yield a percentage value1. The normal reference range of RDW is 11–15%2 and values > 15% indicate the presence of anisocytosis. Recently, high RDW percentage values have been associated with the progression and the severity of CV diseases3. Several possible pathogenetic mechanisms have been proposed including microvascular disorder4, anemia5,6, inflammatory cytokines7, oxidative stress8, free cholesterol9, thrombosis10,11, nutritional deficiency12, renal dysfunction13, and hyper-adrenergic tone14. Moreover, correlations were also found between RDW and increased risk of hypertension15,16, atrial fibrillation12, myocardial infarction8, heart failure17, stroke18 and mortality19,20. On the other hand, no studies have so far evaluated whether RDW may play a role in the long-term outcome of patients undergoing cardiac rehabilitation programme after cardiac surgery; therefore, the present work aimed to elucidate this issue.
Methods
We considered all the consecutive patients admitted to our rehabilitation department between January 2007 and June 2015 to undergo cardiac rehabilitation (CR) after cardiac surgery. Clinical indication for CR were the following: myocardial revascularization by coronary artery bypass graft (CABG), valve surgery and valve and CABG surgery. For the present study we included the 1031 patients with available RDW levels, after excluding patients who underent CR after percutaneous coronary intervention, percutaneous valve replacement, heart failure hospitalization, patients who have not completed the CR programme due to complications that required intensive care unit as well as those without available RDW levels. All the enrolled patients provided written informed consent. The ethics committee on human research of the IRCCS Fondazione Don C. Gnocchi, Milan (Italy) approved the study that was carried out in accordance with the Declaration of Helsinki.
All the patients completed a standard in-hospital CR program, lasting approximately 2 weeks, consisting of supervised exercise sessions (120 min per day), lifestyle and risk factor management, counseling, and medical therapy optimization. Anamnestic data and demographics, clinical and laboratory variables including RDW levels, electrocardiographic and echocardiographic measurements, coronary angiography data, physical activity parameters and pharmacological therapy adherence were collected for each patient at the discharge from the CR program. Coronary artery disease was assessed by coronary angiography during hospitalization before cardiac surgery. At discharge to the CR program after surgery, in all the patients a standard 12-lead ECG (Mortara Instrument-Portrait) and a standard adult transthoracic echocardiography (EsaoteMyLab 60) was performed according to the American Society of Echocardiography (ASE) recommendations21.
Outcomes during follow-up were collected periodically (every 2 years) by a medical doctor through telephone-administered questionnaires. Whenever we received information about any event after the telephone call, we verified the nature of the event on the hospital clinical records and/or contacted the general practitioner. Endpoints were overall and cardiovascular (CV) mortality. CV death was identified only in the presence of clear data demonstrating sudden cardiac death or death resulting from acute myocardial infarction, or heart failure or stroke. In the absence of clear data on the modality of death, the event was not classified as cardiovascular death.
Statistical analysis
We represented continuous variables by the mean (M) and standard deviation (SD) over the group and tested the differences among groups by the analysis of variance (ANOVA), applying the least-significant difference test as post-hoc analysis. We expressed categorical variables in percentage (%) and tested the differences among groups by the Pearson chi-square test. We considered RDW, the predictor variable, both as a continuous and categorical quantity. In the latter case we expressed it as the tertile of its distribution and evaluated the hazard ratio (HR) separately for overall mortality and cardiovascular mortality by the Cox proportional hazard analysis.
We considered a model of covariates in the Cox proportional hazard analysis applied with RDW as a predictor of events to take into account the differences among the RDW tertiles in the patients’ characteristics and known prognostic markers in secondary cardiovascular prevention. The model included age, gender, weight, height, history of arterial hypertension, hyperlipidemia, diabetes, smoking, hemoglobin, hematocrit, C-reactive protein (CRP), microalbuminuria, atrial fibrillation, glomerular filtration rate (GRF) and left ventricular ejection fraction (LV-EF) as covariates. Event-free survival time between the admission and the event was measured and Kaplan–Meier analysis created event-free survival curves among RDW tertiles. Statistical significance was set at p < 0.05. All statistics were performed with SPSS version 24 (IBM Corporation, Armonk, NY, USA).
Results
Demographic and clinical characteristics
Among the included 1.031 patients, 724 patients (71%) reported arterial hypertension and 251 (25%) type 2 diabetes; 492 patients (48%) underwent myocardial revascularization by coronary artery bypass graft (CABG), 371 (36%) valve surgery, 102 (10%) valve and CABG surgery, and 66 patients (6%) underwent surgery for other clinical indications (e.g. tricuspid valve disease, aortic aneurysm, atrial masses). Among myocardial revascularization, 59% underwent cardiac surgery after acute coronary syndrome (ACS) and 41% after stable angina or silent ischemia. Among the patients who received valve surgery, 31% underwent surgery for mitral disease, 59% for aortic disease and 10% for both mitral and aortic disease. Number of exercise training sessions attended were 25 ± 5 (two separate sessions: one in the morning and one in the afternoon).
The RDW mean value ± standard deviation was 14.7 ± 1.8% in the whole group of patients. The ANOVA test revealed significant differences among subgroups (p < 0.001) being the RDW value in the CABG subgroup (14.5 ± 1.8%) significantly lower than in the valve surgery subgroup (14.8 ± 1.9%, p = 0.012), in the combined valve-and-CABG surgery subgroup (15.2 ± 1.8%, p = 0.002) as well as in the subgroup operated for other clinical indications (15.2 ± 1.9%, p = 0.002).
The RDW tertiles ranged between 11.2 and 13.8%, between 13.9 and 14.9%, and between 15.0 and 28.6%. The mean follow-up was 4.5 ± 3.5 years, during which there were 146 deaths (14.2%) and 66 cardiovascular deaths (6.9%). Atrial fibrillation at discharge was found in 142 patients (14%).
Patients characteristics by RDW tertiles are reported in Table 1. Patients with elevated RDW (highest tertile) showed a higher prevalence of female gender, arterial hypertension, and smoking habit, older age and lower height and weight. No differences between groups were found in the rate of cardiovascular drugs except for a lower rate of antiplatelet drugs as well as a higher rate of anticoagulants in the highest tertile.
Patients in the third RDW tertile also showed higher levels of microalbuminuria, total and HDL cholesterol, higher rate of atrial fibrillation at dicharge, as well as lower values of glomerular filtration rate, hemoglobin, and lower left ventricular ejection fraction.
RDW and mortality
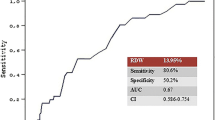
A significantly higher rate of overall (5% vs 9% vs 28%; p < 0.001) and cardiovascular mortality (1% vs 5% vs 16%; p < 0.001) were found in the highest tertile of RDW compared to the first and second tertiles. Kaplan–Meier analysis demonstrated worse survival curves free from overall (log-rank p < 0.0001) and cardiovascular (log-rank p < 0.0001) mortality in the highest RDW tertile in the overall population, as well as in patients who received CABG surgery alone (log-rank p < 0.0001) and valve surgery alone (log-rank p < 0.0001) (Fig. 1). Considered also as a continuous variable RDW correlated directly and significantly with the probability of overall mortality (HR 1.26; 95% CI 1.19–1.32; p < 0.001), corresponding to a 26% increase of the relative risk of death per unitary of RDW increase. Similarly, RDW correlated directly and significantly with the probability of cardiovascular mortality (HR 1.31; 95% CI 1.23–1.40; p < 0.001), corresponding to a 31% increase of the relative risk of CV death per unitary of RDW increase. Interestingly, after dividing the patients' population according to gender, arterial hypertension, diabetes, glomerular filtration rate (cut-off 60 ml/min), left ventricular ejection fraction (cut-off 40%), and type of intervention (myocardial revascularization in both acute or chronic coronary syndrome and valve surgery), overall and cardiovascular mortality risk rate were significantly higher with the progressive increase of RDW levels in all sub-groups (Fig. 2). Moreover, a significantly increased risk of overall mortality (HR 1.10; 95% CI 1.01–1.27; p = 0.039) and cardiovascular (HR = 1.13; 95% CI 1.01–1.34; p = 0.036) was found even after multiple adjustments for age, gender, weight, height, history of arterial hypertension, dyslipidemia, diabetes, smoking, heamoglobin, hematocrit, C-reactive protein, atrial fibrillation, microalbuminuria, GFR, LV-EF and number of exercise training sessions attended.
Discussion
Our study is among the few investigating the predictive value of RDW after a period of cardiac rehabilitation following cardiac surgery in both ischemic and valve disease patients. Our results demonstrate a role of RDW percentage values in predicting overall and cardiovascular mortality independent from gender, arterial hypertension, diabetes, GFR, LVEF and type of intervention.
Although RDW was historically used as a diagnostic marker of hematological disorders (such as chronic anemia due to vitamins deficiency and liver or kidney failure), the role of red blood cells biology in the pathogenesis of non-hematological disorders has been recently evaluated and a correlation between RDW and increased risk of hypertension15,16, atrial fibrillation12, myocardial infarction8, heart failure17, stroke18 and mortality19,20 have been reported.
Skjelbakken et al., investigating the association between RDW and the risk of the first-ever event of myocardial infarction in 25.612 participants, found that, independently of anemia and cardiovascular risk factors, RDW was associated with incident myocardial infarction in a general population8. A post-hoc analysis from the Cholesterol And Recurrent Events (CARE) on 4.111 participants in the Tromsø study with available RDW data (follow-up of 59.7 months) reported a graded, independent relationship between higher levels of RDW and the risk of death and cardiovascular events in people with prior myocardial infarction22.
Furthermore, Warwick et al.23 found that pre-operative RDW represents a significant determinant of in-hospital mortality and long-term survival in 8.615 patients undergoing isolated CABG (median follow up of 5.8 years) and our data are in line with the above-cited results, even when RDW was examined in the post-surgical period during the cardiac rehabilitation programme.
A retrospective, observational work investigating 214 consecutive patients with unstable angina pectoris who underwent successful percutaneous coronary interventions, also showed a strong association between baseline RDW and in-stent restenosis24 as well as a study aimed to identify potential laboratory markers in 2.679 symptomatic chronic heart failure patients from the North American CHARM (Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity) program, demonstrated that higher RDW is associated with morbidity and mortality17. In particular, a higher RDW did result among the most powerful predictors, age and cardiomegaly only showing a better independent association with outcome17.
The prognostic value of elevated RDW was also confirmed in patients undergoing valve replacement or repair surgery as demonstrated by a higher risk of transient ischaemic attack, early peri-operative stroke, and death25. Moreover, the evaluation of the short- and long-term prognostic value of RDW in a large cohort of transcatheter aortic valve implantation patients revealed that elevated RDW represents a strong independent marker and predictor of short- and long-term mortality26. Experimental and human studies have proposed microvascular dysfunction4, anemia5,6, inflammatory cytokines7, oxidative stress8, free cholesterol9, thrombosis10,11, nutritional deficiency12, renal failure13, and autonomic dysfunction14 as possible pathophysiological mechanisms linking RDW with CV diseases.
Interestingly, beta-blockers administration27, as well as 3-week exercise training28, both powerful modulators of autonomic activity and functional capacity during cardiac rehabilitation29, did result associated with a significant reduction of RDW levels, thereby supporting an autonomic pathogenetic hypothesis. More recently some scheming scenarios have been opened in the field of CV medicine where RDW seems to behave not only as a marker of pathological processes but also as a possible active actor. In fact, anisocytosis has been shown to be positively associated with decreased red blood cell deformability, thus contributing to impair microvascular function by decreasing blood viscosity30. Furthermore, the accumulation of free cholesterol driving from the red blood cell membrane has been reported as increased in subjects with high, anisocytosis levels9 promoting the expansion of the lipid core31. Moreover,
during the atherosclerosis process, the iron released as a consequence of erythrophagocytosis or mediated by erythrocyte injury, may also amplify the formation of foam cells, thus promoting the growth and the instability of the atherosclerotic plaque32,33. Finally, nitric oxide released by cell-free hemoglobin upon injury of erythrocytes within the necrotic core of the atherosclerotic plaque may also contribute to inhibiting endothelium-dependent vasodilation34. Even though our data do not allow to provide a pathophysiological explanation, we may speculate that some of the above-mentioned mechanisms, especially hyper-adrenergic tone, inflammation, and endothelial dysfunction, may persist throughout rehabilitation period following cardiac surgery. In particular, in operated cardiac patients (e.g., for CABG or valve repair/replacement), cardiac surgery could activate a series of potentially negative mechanisms (inflammation, hyper adrenergic tone, etc.) contributing to induce bone marrow to produce red blood cells with a wide width distribution (anysocitosis) and to increase long-term mortality (Fig. 3).
Some methodological limitations should be highlighted: (a) pre-existing hematological diseases and pre-operative RDW measures are lacking, (b) RDW was measured only at discharge from cardiac rehabilitation programme, (c) data were adjusted considering hematocrit and hemoglobin values while neutrophil/lymphocyte ratio and platelets counts were not collected, (d) long-term RDW measurement is lacking, (e) peri- and postoperative transfusion data are not available, (f) the exact etiologies of non-cardiovascular deaths are lacking, (f) lack of a control group of subjects that did not attend CR to assess its relative contribution on RDW and outcomes, (g) lack of functional improvement during CR (between admission and discharge) to assess the impact of exercise based programme on RDW and outcomes, (h) a loss to follow-up bias cannot be excluded since 24% of patients were lost at the last follow-up session, (i) finally, an intrinsic risk of over-adjustment cannot be excluded in the presence of a broad multivariate analysis. In conclusion, our data demonstrate that RDW represents an independent predictor of overall and cardiovascular mortality in patients undergoing cardiac rehabilitation after myocardial revascularization or cardiac valve surgery (in secondary cardiovascular prevention patients undergoing cardiac rehabilitation).
References
Clarke, K., Sagunarthy, R. & Kansal, S. RDW as an additional marker in inflammatory bowel disease/undifferentiated colitis. Dig. Dis. Sci. 53, 2521–2523 (2008).
Danese, E., Lippi, G. & Montagnana, M. Red blood cell distribution width and cardiovascular diseases. J. Thorac. Dis. 7, E402-411 (2015).
Li, N., Zhou, H. & Tang, Q. Red blood cell distribution width: A novel predictive indicator for cardiovascular and cerebrovascular diseases. Dis. Mark. 20, e7089493 (2017).
Reinhart, W. H., Piety, N. Z., Goede, J. S. & Shevkoplyas, S. S. Effect of osmolality on erythrocyte rheology and perfusion of an artificial microvascular network. Microvasc. Res. 98, 102–107 (2015).
Sharma, S., Gage, B. F., Deych, E. & Rich, M. W. Anemia: An independent predictor of death and hospitalizations among elderly patients with atrial fibrillation. Am. Heart J. 157, 1057–1063 (2009).
Xu, D. et al. Anemia and reduced kidney function as risk factors for new onset of atrial fibrillation (from the Ibaraki prefectural health study). Am. J. Cardiol. 115, 328–333 (2015).
Pierce, C. N. & Larson, D. F. Inflammatory cytokine inhibition of erythropoiesis in patients implanted with a mechanical circulatory assist device. Perfusion 20, 83–90 (2005).
Skjelbakken, et al. Red cell distribution width is associated with incident myocardial infarction in a general population: The Tromsø Study. J. Am. Heart Assoc. 3, e001109 (2014).
Tziakas, D. et al. Red blood cell distribution width: A strong prognostic marker in cardiovascular disease: Is associated with cholesterol content of erythrocyte membrane. Clin. Hemorheol. Microcirc. 51, 243–254 (2012).
Engström, G. et al. Red cell distribution width, haemoglobin A1c and incidence of diabetes mellitus. J. Intern. Med. 276, 174–183 (2014).
Zöller, B., Melander, O., Svensson, P. & Engström, G. Red cell distribution width and risk for venous thromboembolism: A population-based cohort study. Thromb. Res. 133, 334–339 (2014).
Adamsson Eryd, S. et al. Red blood cell distribution width is associated with incidence of atrial fibrillation. J. Intern. Med. 275, 84–92 (2014).
Yoon, H. E. et al. Progressive rise in red blood cell distribution width predicts mortality and cardiovascular events in end-stage renal disease patients. PLoS One 10, e0126272 (2015).
Okonko, D. O., Marley, S. B., Anker, S. D., Poole-Wilson, P. A. & Gordon, M. Y. Suppression of erythropoiesis in patients with chronic heart failure and anaemia of unknown origin: Evidence of an immune basis. Int. J. Cardiol. 166, 664–671 (2013).
Tanindi, A., Topal, F. E., Topal, F. & Celik, B. Red cell distribution width in patients with prehypertension and hypertension. Blood Press. 21, 177–181 (2012).
Buyukkaya, E. et al. Relation of red cell distribution width with dipper and non-dipper hypertension. Med. Glas. (Zenica). 13, 75–81 (2016).
Uyarel, H. et al. Red cell distribution width as a novel prognostic marker in heart failure: Data from the CHARM Program and the Duke Databank. J. Am. Coll. Cardiol. 50, 40–47 (2007).
Söderholm, M., Borné, Y., Hedblad, B., Persson, M. & Engström, G. Red cell distribution width in relation to incidence of stroke and carotid atherosclerosis: A population-based cohort study. PLoS One 10, e0124957 (2015).
Chen, P. C. et al. Red blood cell distribution width and risk of cardiovascular events and mortality in a community cohort in Taiwan. Am. J. Epidemiol. 171, 214–220 (2010).
Arbel, Y. et al. Red blood cell distribution width and the risk of cardiovascular morbidity and all-cause mortality. A population-based study. Thromb. Haemost. 111, 300–307 (2014).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28, 1-39.e14 (2015).
Tonelli, M. et al. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation 117, 163–168 (2008).
Warwick, R. et al. Red cell distribution width and coronary artery bypass surgery. Eur. J. Cardiothorac. Surg. 43, 1165–1169 (2013).
Geng, N. et al. High red blood cell distribution width is closely associated with in-stent restenosis in patients with unstable angina pectoris. BMC Cardiovasc. Disord. 19, 175 (2019).
Duchnowski, P., Hryniewiecki, T., Stokłosa, P., Kuśmierczyk, M. & Szymański, P. Red cell distribution width as a prognostic marker in patients undergoing valve surgery. J. Heart Valve Dis. 26, 714–720 (2017).
Szekely, Y. et al. Red blood cell distribution width as a prognostic factor in patients undergoing transcatheter aortic valve implantation. J. Cardiol. 74, 212–216 (2019).
Fici, F. et al. Comparative effects of nebivolol and metoprolol on red cell distribution width and neutrophil/lymphocyte ratio in patients with newly diagnosed essential hypertension. J. Cardiovasc. Pharmacol. 62, 388–393 (2013).
Nishiyama, Y. et al. Effect of exercise training on red blood cell distribution width as a marker of impaired exercise tolerance in patients with coronary artery disease. Int. Heart J. 57, 553–557 (2016).
Lazzeroni, D. et al. Improvement in aerobic capacity during cardiac rehabilitation in coronary artery disease patients: Is there a role for autonomic adaptations?. Eur. J. Prev. Cardiol. 24, 357–364 (2017).
Patel, K. V. et al. Association of the red cell distribution width with red blood cell deformability. Adv. Exp. Med. Biol. 765, 211–216 (2013).
Virmani, R. et al. Atherosclerotic plaque progression and vulnerability to rupture: Angiogenesis as a source of intraplaque hemorrhage. Arterioscler. Thromb. Vasc. Biol. 25, 2054–2061 (2005).
Kolodgie, F. D. et al. Intraplaque hemorrhage and progression of coronary atheroma. N. Engl. J. Med. 349, 2316–2325 (2003).
Kockx, M. M. et al. Phagocytosis and macrophage activation associated with hemorrhagic microvessels in human atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 23, 440–446 (2003).
Kim-Shapiro, D. B., Schechter, A. N. & Gladwin, M. T. Unraveling the reactions of nitric oxide, nitrite, and hemoglobin in physiology and therapeutics. Arterioscler. Thromb. Vasc. Biol. 26, 697–705 (2006).
Acknowledgements
We thank all the students of Parma University Medical School who took part in the creation of our registry; their time spent on data collection was essential for the realization of the present study.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
D.L., L.M., P.L.M., P.C., C.P., E.M., and P.C.: analysed the results and wrote the manuscript. U.C., M.B., S.G., L.B., V.B.: reviewed the manuscript. All authors collected the data and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lazzeroni, D., Moderato, L., Marazzi, P.L. et al. Red blood cell distribution width as a novel prognostic marker after myocardial revascularization or cardiac valve surgery. Sci Rep 11, 7889 (2021). https://doi.org/10.1038/s41598-021-87075-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87075-4
- Springer Nature Limited