Abstract
Optochin susceptibility testing is a major assay used for presumptive identification of Streptococcus pneumoniae. Still, atypical optochin-resistant (Optr) pneumococci have been reported and this phenotype has been attributed to nucleotide substitutions in the genes coding for the F0F1ATPase. While substitutions in the atpC gene (c-subunit of ATPase) are more common and better characterized, data on mutations in the atpA (a-subunit) are still limited. We have characterized five Optr isolates presenting alterations in the atpA (Trp206Cys in four isolates and Trp206Ser in one isolate), constituting the first report of such mutations in Brazil. Most of the Optr isolates consisted of heterogeneous populations. Except for Opt MICs and the nucleotide changes in the atpA gene, Optr and Opts subpopulations originating from the same culture had identical characteristics. In addition, we compared phenotypic and genetic characteristics of these atpA mutants with those of atpC mutants previously identified in Brazil. No structural alterations were detected among predicted proteins, regardless of mutations in the coding gene, suggesting that, despite the occurrence of mutations, protein structures tend to be highly conserved, ensuring their functionalities. Phylogenetic analysis revealed that atypical Optr strains are true pneumococci and Opt resistance does not represent any apparent selective advantage for clinical isolates.
Similar content being viewed by others
Introduction
Streptococcus pneumoniae is a leading cause of invasive diseases among children and the elderly associated with considerable mortality and economic burden1. Although infant mortality rates have been declining since 2000 due to broader access to pneumococcal vaccines, pneumococcal pneumonia remains as a major cause of child mortality2. Thus, pneumococcal infections require fast and accurate diagnosis. Conventional laboratory identification of S. pneumoniae usually relies on one major characteristic of this species: the susceptibility to optochin (Opt). Opt susceptibility testing can distinguish the human pathogen S. pneumoniae from other alpha-hemolytic species, such as Streptococcus mitis and Streptococcus pseudopneumoniae3.
Nevertheless, isolation of Opt-resistant (Optr) pneumococcal has been reported in different geographical areas4,5,6,7,8,9,10,11, drawing attention to the potential for misidentification of this relevant pathogen. Point mutations in the atpC gene are usually attributed to this atypical phenotype; the atpC gene codes for the c-subunit of the bacterial F0F1ATPase, the molecular target of optochin4,5,6,8,9,11,12,13. Alterations in other subunits of this molecule are rare, and only two reports on Optr clinical strains of S. pneumoniae presenting mutations in the atpA gene (coding for the a-subunit of the bacterial F0F1ATPase) are available to date5,13.
Our group has reported the occurrence of previously recognized as well as novel mutations in the atpC gene among a set of 26 Optr pneumococcal isolates in Brazil6,9. In the present study, we describe five additional Optr isolates presenting alterations in the atpA gene, constituting the first report of such unusual mutations in pneumococcal isolates from our country. In addition, we extended the spectrum of methodologies used and compared phenotypic and genetic characteristics of all Optr pneumococcal strains described in Brazil up to now, including both atpC and atpA mutants.
Results
Strain identification and characterization of Opt resistance phenotypes
All five isolates described in the study had the following characteristics: they were gram-positive catalase-negative cocci; presented alpha-hemolysis on sheep blood agar plates; generated positive results in the bile solubility and in the latex agglutination tests; harbored the lytA, ply and psaA genes; and were resistant to Opt.
Opt susceptibility testing, under both CO2-enriched or conventional atmospheres, revealed the occurrence of two phenotypes among the five Optr isolates. The first was represented by one isolate displaying no inhibition zone, consisting of a homogeneous Optr population. The second phenotype was represented by the other four isolates, showing inhibition zones > 14 mm but with colonies within, consisting of heterogeneous populations comprised by Optr and Opt-susceptible (Opts) subpopulations. Opt MICs ranged from 16 to 32 μg ml among the five Optr strains evaluated (Fig. 1). The single Opt r homogeneous population had an Opt MIC of 32 μg/ml. Optr subpopulations derived from heterogeneous populations exhibited MICs between 16 and 32 μg/ml (Fig. 1); while Opts counterparts presented Opt MICs of 1 μg/ml. Opt MICs of Opts subpopulations were identical to those detected among optochin-susceptible reference strains of S. pneumoniae ATCC BAA-255 and ATCC 49619 (1 μg/ml). Opt MICs of reference strains of S. pseudopneumoniae ATCC BAA-960 and S. mitis ATCC 49456 were 8 μg/ml and 256 μg/ml, respectively.
UPGMA dendrogram generated by using BioNumerics v.7.6 based on PFGE profiles of 31 optochin-resistant Streptococcus pneumoniae strains isolated in Brazil. The five atpA gene mutants described in this work are marked in red. Ala alanine, CLI clindamycin, CHL chloramphenicol, CSF cerebrospinal fluid, Cys cysteine, ED eye discharge, ERY erythromycin, Gly glycine, HE heterogeneous, HO homogeneous, Ile isoleucine, Leu leucine, LRT low respiratory tract, Met methionine, MIC minimum inhibitory concentration, NP nasopharyngeal carriage, Opt optochin, PEN penicillin, Phe phenylalanine, Ser serine, ST sequence type, SXT sulfamethoxazole-trimethoprim, TET tetracycline, Thr threonine, Trp tryptophan, Val valine, U unknown.
In addition to the five Optr strains included in the present study, the 26 Optr isolates previously reported in Brazil6,9 were also subjected to identification by MALDI-TOF MS. All 31 strains were identified as S. pneumoniae, with scores between 2.089 and 2.452. Of note, Optr and Opts subpopulations derived from heterogeneous populations were also analyzed separately, and in all cases both subpopulations were identified as pneumococcus with scores higher than 2.0. However, reference strains S. mitis ATCC 49456 and S. pseudopneumoniae ATCC BAA-960 were also identified as S. pneumoniae by MALDI-TOF MS, with scores of 1.938 and 2.213, respectively.
Sequencing of atpA gene
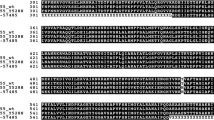
Sequencing of atpA genes revealed single-base substitutions leading to amino acid modifications in codon 206 in all five strains, comprising four isolates with a Trp206Cys substitution and one isolate with a Trp206Ser substitution (Figs. 1 and 2A,B). Interestingly, the single strain with a Trp206Ser substitution was also the single strain homogenously resistant to optochin. All the other four showing the Trp206Cys modification consisted on heterogeneous populations. Of note, while Optr subpopulations derived from heterogeneous populations presented this alteration in codon 206, Opts counterparts had atpA gene sequences identical to those of optochin-susceptible reference strains of S. pneumoniae (ATCC BAA-255 and ATCC 49619).
Alignment of representative atpA gene sequences observed among optochin-resistant (Optr) Streptococcus pneumoniae isolates. (A) Nucleotide sequences of the atpA gene representing the two different base-substitutions observed among the five Optr isolates included in the present study. (B) Deduced amino acid sequences of the a-subunit of ATPase representing, respectively, the two different base-substitutions mentioned above. Optochin-susceptible reference strain S. pneumoniae R6 was included for comparative purposes. Alterations are outlined with black boxes.
In silico prediction of c- and a-subunit 3D models
The 3D structure of the a-subunit of F0F1ATPase predicted in silico from the atpA nucleotide sequences of the five Optr S. pneumoniae strains included in the study were identical to the models generated from Opts reference strains (S. pneumoniae ATCC BAA-255 and ATCC 49619), consisting of five transmembrane α-helices (Fig. 3A). Likewise, 3D models of the c-subunit, predicted from the atpC gene sequences of 26 Optr strains previously reported6,9 and retrieved from GenBank database, were indistinguishable from the ones of Opts reference strains (S. pneumoniae ATCC BAA-255 and ATCC 49619), consisting of two transmembrane α-helices (Fig. 3B). The structures were also identical between Optr and Opts subpopulations derived from heterogeneous populations.
In silico predicted 3D models for c- (A) and a-subunits (B) of F0F1ATPase of Streptococcus pneumoniae created with Bioserf v.2.0. Alpha helices are colored in pink. All 31 optochin-resistant S. pneumoniae strains analyzed and the reference strains ATCC BAA-255 and ATCC 49619 generated identical models for both subunits.
Phenotypic and molecular characterization of Optr strains
Optr and Opts subpopulations derived from heterogeneous populations showed identical results regarding capsular type, antimicrobial susceptibility profile, ST, PFGE, MLVA and PI-1 genes profiles.
The five Optr pneumococcal isolates included in this study belonged to serotypes 6A, 6C, 18C, 19A and 19F. All strains were susceptible to antimicrobial agents tested, except for sulfamethoxazole/trimethoprim (Fig. 1).
Within the five atpA mutants, different PFGE patterns (Fig. 1), STs (193,733, 763, 3930 and 5847) (Figs. 1 and 5) and MLVA profiles (Fig. 4) were detected. When compared to the 26 Optr pneumococcal isolates previously described in Brazil, only three STs and two MLVA profiles were shared by two or more strains (Figs. 1, 4 and 5). It is also noteworthy that ten (32.25%) of all 31 Optr pneumococcal isolates analyzed belonged to internationally disseminated clones recognized by the PMEN (Fig. 5). Of note, there was no correlation between the type of atpC or atpA mutation with serotype, PFGE pattern, ST or MLVA type (Figs. 1, 4 and 5).
Minimum Spanning Tree generated by using BioNumerics v.7.6 and showing the genetic relationship among 31 optochin-resistant Streptococcus pneumoniae strains isolated in Brazil, according to the MLVA profiles. Each node represents one MLVA profile, and nodes are divided proportionaly to the number of isolates included in each MLVA profile. Clonal complexes (strains sharing five or more identical alleles) are shaded in grey. Absence of lines between nodes indicate they show three or more different alleles and are, therefore, genetically unrelated. Strains were differentiated by color according to the location of mutation (atpC or atpA; see legend).
Minimum Spanning Tree generated by using BioNumericsv.7.6 and displaying the genetic relatedness inferred by MLST among 31 optochin-resistant Streptococcus pneumoniae strains isolated in Brazil. Each node represents one sequence type (ST), and nodes are divided proportionaly to the number of isolates included in the same ST. Internationally disseminated clones recognized by the PMEN and related to strains analyzed in the study are indicated. Clonal complexes (strains sharing five or more identical alleles) are shaded in grey. Absence of lines between nodes indicate they show three or more different alleles and are, therefore, genetically unrelated. Strains were differentiated by color according to the location of mutation (atpC or atpA; see legend). Strains harboring pilus type 1 genes are highlighted with a blue arrow.
PI-1 genes were found in five (16.1%) of all 31 Optr isolates analyzed; of those, one had a mutation in the atpA gene while four had mutations in the atpC gene (Fig. 1). In addition, most of the PI-1 positive strains were related to PMEN clones.
Phylogenetic analysis
Phylogenetic analysis revealed that all 31 Optr pneumococcal strains, including both atpA and atpC mutants, were clustered within a monophyletic group, with 100% of probability in an analysis using a bootstrap of 1000 (Fig. 6). This analysis also included typical S. pneumoniae, representative of Opts strains. On the other hand, S. mitis, S. pseudopneumoniae and S. oralis were clustered in different and more distantly related groups.
MLSA tree generated from the concatenated sequences of six housekeeping genes (aroE, gdh, gki, recP, spi and xpt) showing the phylogenetic relationship among optochin-resistant Streptococcus pneumoniae (31 isolates), typical S. pneumoniae (8 isolates), Streptococcus pseudopneumoniae (strain 9230), Streptococcus mitis strain (SS691) and Streptococcus oralis (strain SS527). Scale bar indicates the nucleotide subtitution per site. Highlighted with a red box is the cluster comprising all 39 S. pneumoniae sequences analyzed, including the typical and the optochin-resistant strains.
Discussion
During the last decades, the occurrence of atypical optochin-resistant pneumococcal strains has been sporadically reported4,5,6,7,8,9,10,12,13,14, reinforcing the need of constant evaluation of traditional identification schemes for this relevant pathogen.
Different studies have described the occurrence of two phenotypes within collections of Optr S. pneumoniae isolates: a homogeneous type in which the isolate is fully resistant to optochin, and a heterogeneous type comprised by Optr and Opts subpopulations5,6,7,9,12,13. The distribution of each phenotype, however, seems to vary according to the geographical region. In Brazil, as well as in the United States5, the heterogeneous phenotype has been more commonly reported. Among the 26 Optr isolates previously reported from Brazil6,9, 16 (61.5%) were composed by heterogeneous populations (Fig. 1). On the other hand, in Portugal, homogenous Optr populations have been more frequently observed7. Of note, the only difference found between subpopulations derived from heterogeneous Optr populations, in this and previous studies, is the mutation in atpA or atpC gene. These observations suggest that an originally Opts population might at some point undergo a point mutation resulting in two different types of cells that, then, compose a heterogeneous Optr population. However, it remains unknown why in some strains these subpopulations tend to coexist while in others a homogeneous Optr phenotype occurs.
MALDI-TOF MS has gained large interest in the clinical microbiology setting and it has already been introduced in the routine of several clinical laboratories worldwide15,16. This methodology has been widely used for identification of a number of bacterial species, but the lack of discrimination among streptococcal species belonging to the mitis group is well documented15,17. Although alternative MALDI-TOF MS-based protocols for accurate differentiation of mitis group streptococci have been proposed, the majority depend on the analysis of mass spectra by trained staff, being unfeasible for application in many clinical laboratories, which usually rely on results generated by automated processing of spectra by dedicated softwares16,18. Therefore, when using MALDI-TOF MS for identification of S. pneumoniae in the clinical microbiology laboratory, it is mandatory to perform a complementary test, such as bile solubility or optochin susceptibility testing19. In this regard, laboratory personnel should be aware of the possible occurrence of atypical optochin-resistant pneumococcus, and preferentially perform an additional test if the isolate shows resistance to optochin.
Opt MICs found in this study, ranging between 16 and 32 μg/ml, were in agreement with MICs (8–64 μg/ml) observed among the 26 Optr Brazilian isolates previously described6,9 (Fig. 1), and also with those obtained for isolates from other locations5,7. Comparison of Optr and Opts MICs in heterogeneous populations revealed similar results to earlier studies, in which MICs of Optr subpopulations were 4–64 fold higher than those of Opts counterparts5,9. Moreover, no correlation between Opt MIC levels and Optr phenotype was detected since similar MIC levels were observed in both homogenous and heterogeneous populations. Likewise, no correlation between Opt MIC levels and type of mutation was observed, as previously reported5,9,10.
To the best of our knowledge, this is the first study to describe atpA mutants among clinical pneumococcal isolates in Brazil and also represents the largest and more extensively characterized collection of Optr S. pneumoniae clinical isolates reported in the literature. Earlier, only two Optr S. pneumoniae clinical isolates presenting mutations in atpA gene had been described5,13. The first was recovered from an individual’s nasopharynx in the United States, presented a heterogeneous phenotype, a Trp206Ser substitution, an Opt MIC of 32 μg/ml, and belonged to serotype 6B5. The second was recovered from a patient’s blood in Argentina, showed a homogeneous phenotype, a Trp206Cys modification, an Opt MIC of 64 μg/ml, and belonged to serotype 513.
Our results reinforce the observation that mutations in the atpA gene are not correlated with specific clinical source or serotype, but also highlight that substitutions in this gene, regardless of any other characteristic, are always in the same position, the codon 206. This is quite different from what has been observed within atpC mutants, among which substitutions have been identified in 12 different codons of the c-subunit4,5,6,8,9,10,13,14. Still, despite the higher variability, around 50% of the 48 atpC mutants described to date show alterations in the same location, the codon 49, which has been suggested as a hot-spot for this type of mutation. Codon 206 in the a-subunit could act as a hot-spot as well, but this should be established as more atpA mutants are identified.
In silico predicted 3D models of a- and c-subunits indicate that, despite the occurrence of alterations at the primary level, 3D models of c- and a-subunits tend to be highly conserved, regardless of optochin susceptibility profile, which could probably confer the maintenance of enzyme functional activity and, consequently, the survival of bacteria. Although no structural alterations on predicted proteins were detected in the present study, it has been previously observed that mutations in the c-subunit led to inability of these bacteria to survive in acidic conditions, including survival inside of macrophages20. Mutations in the a-subunit of F0F1 ATPase, on the other hand, presented no implications regarding acid tolerance20. Nevertheless, additional studies are needed to clarify the impact of atpA and atpC mutations on pneumococcal fitness.
The variability of PFGE profiles, STs and MLVA types detected in the study indicate that optochin resistance is not a clonal-specific characteristic, in agreement with previous findings7,9. However, PMEN clones previously associated with the presence of PI-121 and known to be circulating in Brazil in recent years9,22,23,24 were found among Optr strains, suggesting that highly successful clones can exhibit the atypical Optr phenotype, increasing the concern on possible consequences of the misidentification of these variants.
Phylogenetic analysis clearly shows that atypical Optr S. pneumoniae and typical pneumococci have evolved from the same ancestral (Fig. 6), while evolution that resulted in different streptococcal species occurred by an independent route. These data, in conjunction with the other results of this study, strongly suggest that Optr isolates are authentic S. pneumoniae that have diverged from typical strains by point mutations in the the atpC or atpA genes.
In conclusion, our results suggest that optochin resistance in S. pneumoniae is not related to a specific phenotypic or genetic characteristic, but is rather due to the random occurrence of mutations in the atpA or atpC genes. Even though mutations in a- or c-subunits of F0F1 ATPase can result in amino acid changes, their predicted 3D structures remain unaltered, ensuring survival of these strains. Phylogenetic analysis revealed that atypical Optr strains are true pneumococci and Opt resistance does not represent any apparent selective advantage for clinical strains.
Methods
Bacterial strains and identification tests
Five Optr S. pneumoniae isolates (Sp 921, Sp 2240, Sp 2263, NHG78 and NHG129) recovered from individuals living in Brazil were included in the present study, based on the finding that they showed no alterations in the atpC gene during initial screening tests, carried out as previously described9. Four isolates were obtained during nasopharyngeal carriage surveillance studies performed as approved by the ethics committees of the institutions involved. One isolate (Sp 921) was recovered from a blood culture taken as part of the standard patient care procedures, so a specific ethical approval was not needed. The isolates were subjected to conventional phenotypic identification tests, including observation of colony morphology and type of hemolytic activity on sheep blood agar plates; cellular characteristics as observed after Gram stain; Opt susceptibility, bile-solubility, and latex agglutination tests3. Identification was also performed by MALDI-TOF MS, using a Microflex LT equipment (Bruker Daltonics, Bremen, Germany), according to the manufacturer recommendations. For comparative purposes, a collection of 26 Optr pneumococcal isolates presenting mutations in the atpC gene, previously identified by our group6,9, was also included for further characterization by MALDI-TOF, MLSA, MLST, detection of PI-1 genes and in silico prediction of c-subunit 3D model. Reference strains of S. pneumoniae (ATCC BAA-255 and ATCC 49619), S. pseudopneumoniae (ATCC BAA-960) and S. mitis (ATCC49456) were included in all identification tests.
Optochin susceptibility testing
Opt susceptibility was determined by disk diffusion testing according to standard procedures3. Optochin disks (BBL Taxo P Discs, BD, Sparks, MD, USA) were applied to the surface of 5% sheep blood agar plates (Plast Labor, Rio de Janeiro, RJ, Brazil) streaked with the isolates being tested. After overnight incubation at 36 °C, under both 5% CO2 and conventional atmospheres25, growth inhibition zones around the disks were measured. Isolates displaying inhibition zones ≥ 14 mm in diameter were identified as susceptible, while strains were considered resistant when showing zones < 14 mm or zones ≥ 14 mm but with colonies within. This last case was classified as heterogeneous population, composed by both Optr and Opt-susceptible (Opts) subpopulations; all subsequent experiments were carried out separately for both subpopulations after obtaining pure cultures of each one. Additionally, optochin (Sigma Chemical Co., St. Louis, MO, USA) minimal inhibitory concentrations (MICs) were also determined, by the agar dilution method as previously described9.
Sequencing of atpA gene
DNAs for all PCR reactions were obtained by using the Chelex 100 resin (Bio-Rad, Hercules, CA, USA) as described earlier9, followed by amplification of the atpA gene11. Products were purified with ExoSAP-IT (USB Affymetrix, Cleveland, OH, USA) and sequenced using ABI 3130 Genetic Analyzer (Applied Biosystems). Sequences were aligned and analyzed with Bioedit software v7.0.9.026, using atpA nucleotide sequences of Opts reference strains (S. pneumoniae ATCC BAA-255 and ATCC 49619) as standards.
In silico prediction of c- and a-subunit 3D models
Using the amino acid sequences translated from the nucleotide sequences obtained in this study, predicted 3D models of the a-subunit of F0F1 ATPase were designed by using the online tool Bioserf v2.0, available at PSIPRED Protein Sequence Analysis Workbench27,28. Predicted 3D models of the c-subunit were generated using the atpC gene sequences of 26 Optr strains previously reported6,9 retrieved from the GenBank database (accession numbers KC513927 to KC513948); atpC and atpA nucleotide sequences of Opts reference strains (S. pneumoniae ATCC BAA-255 and ATCC 49619) were included for comparative purposes.
Determination of capsular types
Capsular types were determined by either PCR29 or the standard Quellung reaction30.
Antimicrobial susceptibility testing
Susceptibility to antimicrobial agents was evaluated by the agar diffusion test according to CLSI recommendations and interpretative criteria31. The following agents were tested: chloramphenicol, clindamycin, erythromycin, levofloxacin, oxacillin, rifampicin, tetracycline, sulfamethoxazole-trimethoprim and vancomycin (all from Oxoid, Basingstoke, Hampshire, United Kingdom). S. pneumoniae ATCC 49619 was used for quality control.
Detection of virulence-associated genes
The presence of virulence genes ply (coding for pneumolysin), lytA (coding for autolysin), psaA (coding for pneumococcal surface antigen A)32,33,34, and those coding for pilus type 1 (PI-1)21 was investigated by PCR using previously described primers and an automated Veriti 96-well thermal cycler (Applied Biosystems Inc, Carlsbad, CA, USA).
Evaluation of genetic diversity
Genetic diversity was assessed by Pulsed-Field Gel Electrophoresis (PFGE)9, Multiple Locus VNTR Analysis (MLVA)35 and Multilocus Sequence Typing (MLST)36,37,38 with modified primers39, according to earlier recommendations.
Phylogenetic analysis
Phylogenetic analysis was performed by Multilocus Sequence Analysis (MLSA)40. Concatenates of six housekeeping genes (aroE, gdh, gki, recP, spi, xpt) were generated with an online tool41 and a phylogenetic tree was built using Mega X software42, using the following parameters: Neighbor Joining algorithm, with bootstrap of 1000, Kimura 2p model and uniform rates of substitutions. There were also included in the analysis nucleotide sequences of typical S. pneumoniae strains belonging to STs 1, 2, 3, 4, 5, 7 and 9 (obtained from PubMLST)37 and sequences of other Streptococcus species (retrieved from GenBank database) including S. mitis strain S691 (accession numbers EU075887.1, EU075743.1, EU075784.1, EU075814.1, EU075851.1 and EU075674.1 for genes aroE, gdh, gki, recP, spi and xpt respectively), S. pseudopneumoniae strain 9230 (accession numbers KC491132.1, KC491108.1, KC491058.1, KC491034.1, KC490998.1 and KC490972.1 for genes aroE, gdh, gki, recP, spi and xpt respectively) and Streptococcus oralis strain S527 (accession numbers EU076013.1, EU076236.1, EU075980.1, EU076137.1, EU076186.1 and EU075945.1 for genes aroE, gdh, gki, recP, spi and xpt respectively).
Nucleotide sequence accession numbers
The atpA gene sequences of the five mutated isolates reported in the present study were deposited in GenBank database under accession numbers KR012497 to KR012501.
References
Shiri, T. et al. Pneumococcal disease: A systematic review of health utilities, resource use, costs, and economic evaluations of interventions. Value Health. 22, 1329–1344 (2019).
UN IGME (United Nations Inter-agency Group for Child Mortality Estimation). Levels & trends in child mortality report 2020 at https://childmortality.org/wp-content/uploads/2020/09/UNICEF-2020-Child-Mortality-Report.pdf (2020).
Spellerberg B & Brandt C. Streptococcus in Manual of Clinical Microbiology (ed. Carroll KC et al.) 383–402 (ASM Press, 2015).
Cogné, N., Claverys, J. P., Denis, F. & Martin, C. A novel mutation in the α-helix 1 of the C subunit of the F1/F0 ATPase responsible for optochin resistance of a Streptococcus pneumoniae clinical isolate. Diagn. Microbiol. Infect. Dis. 38, 119–121 (2000).
Pikis, A., Campos, J. M., Rodriguez, W. J. & Keith, J. M. Optochin resistance in Streptococcus pneumoniae: Mechanism, significance and clinical implications. J. Infect. Dis. 184, 582–590 (2001).
Dias, C. A. et al. Diversity of mutations in the atpC gene coding for the c subunit of F0F1ATPase in clinical isolates of optochin-resistant Streptococcus pneumoniae from Brazil. J. Clin. Microbiol. 45, 3065–3067 (2007).
Nunes, S., Sá-Leão, R. & De Lencastre, H. Optochin resistance among Streptococcus pneumoniae colonizing healthy children in Portugal. J. Clin. Microbiol. 46, 321–324 (2008).
Nagata, M. et al. Emergence of optochin resistance among Streptococcus pneumoniae in Japan. Open J. Med. Microbio.l 2, 8–15 (2012).
Pinto, T. C. et al. Phenotypic and molecular characterization of optochin- resistant Streptococcus pneumoniae isolates from Brazil, with description of five novel mutations in the atpC gene. J. Clin. Microbiol. 51, 3242–3259 (2013).
Raddaoui, A., Tanfous, F. B., Achour, W., Baaboura, R. & Hassen, A. B. Description of a novel mutation in the atpC gene in optochin-resistant Streptococcus pneumoniae strains isolates from Tunisia. Int. J. Antimicrob. Agents 51, 803–805 (2018).
Fenoll, A., Muñoz, R., Garcia, E. & de la Campa, A. G. Molecular basis of the optochin-sensitive phenotype of pneumococcus: Characterization of the genes encoding the F0 complex of the Streptococcus pneumoniae and Streptococcus oralis H(+)- ATPases. Mol. Microbiol. 12, 587–598 (1994).
Martín-Galiano, A. J., Gorgojo, B., Kunin, C. M. & De La Campa, A. G. Mefloquine and new related compounds target the F0 complex of the F0F1 ATPase of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 46, 1680–1687 (2002).
Cortes, P. R., Orio, A. G., Regueira, M., Piñas, G. E. & Echenique, J. Characterization of in vitro-generated and clinical optochin-resistant strains of Streptococcus pneumoniae isolated from Argentina. J. Clin. Microbiol. 46, 1930–1934 (2008).
Ikryannikova, L. N. et al. The mystery of the fourth clone: comparative genomic analysis of four non-typeable Streptococcus pneumoniae strains with different susceptibilities to optochin. Eur. J. Clin. Microbiol. Infect. Dis. 35, 119–130 (2016).
Isaksson, J. et al. Comparison of species identification of endocarditis associated viridans streptococci using rnpB genotyping and 2 MALDI-TOF systems. Diagn. Microbiol. Infect. Dis. 81, 240–245 (2015).
Marín, M. et al. Accurate differentiation of Streptococcus pneumoniae from other species within the Streptococcus mitis group by peak analysis using MALDI-TOF MS. Front. Microbiol. 8, 698 (2017).
Ikryannikova, L. N. et al. Discrimination between Streptococcus pneumoniae and Streptococcus mitis based on sorting of their MALDI mass spectra. Clin. Microbiol. Infect. 19, 1066–1071 (2013).
Yahiaoui, R. Y., Goessens, W. H., Stobberingh, E. E. & Verbon, A. Differentiation between Streptococcus pneumoniae and other viridans group streptococci by matrix-assisted laser desorption/ionization time of flight mass spectrometry. Clin. Microbiol. Infect. 26, 1088 (2020).
Burckhardt, I., Panitz, J., Burckhardt, F. & Zimmermann, S. Identification of Streptococcus pneumoniae: development of a standardized protocol for optochin susceptibility testing using total lab automation. Biomed. Res. Int. 2017, 4174168 (2017).
Cortes, P. R., Piñas, G. E., Cian, M. B., Yandar, N. & Echenique, J. Stress-triggered signaling affecting survival or suicide of Streptococcus pneumonia. Int. J. Med. Microbiol. 305, 157–169 (2015).
Moschioni, M. et al. Streptococcus pneumoniae contains 3 rlrA pilus variants that are clonally related. J. Infect. Dis. 197, 888–896 (2008).
Barroso, D.E et al. Β-Lactam resistance, serotype distribution, and genotypes of meningitis causing Streptococcus pneumoniae, Rio de Janeiro, Brazil. Pediatr. Infect. Dis. J. 31, 30–36 (2012).
Pinto, T. C. et al. Streptococcus pneumoniae serotypes 9 and 14 circulating in Brazil over a 23-year period prior to introduction of the 10-valent pneumococcal conjugate vaccine: Role of international clones in the evolution of antimicrobial resistance and description of a novel genotype. Antimicrob. Agents Chemother. 60, 6664–6672 (2016).
Neves, F. P. G. et al. Population structure of Streptococcus pneumoniae colonizing children before and after universal use of pneumococcal conjugate vaccines in Brazil: emergence and expansion of the MDR serotype 6C-CC386 lineage. J. Antimicrob. Chemother. 73, 1206–1212 (2018).
Arbique, J. C. et al. Accuracy of phenotypic and genotypic testing for identification of Streptococcus pneumoniae and description of Streptococcus pseudopneumoniae sp. J. Clin. Microbiol. 42, 4686–4696 (2004).
Hall, L. M. C. Application of molecular typing to the epidemiology of Streptococcus pneumoniae. J. Clin. Pathol. 51, 270–274 (1998).
Buchan, D. W., Minneci, F., Nugent, T. C. O., Bryson, K. & Jones, D. T. Scalable web services for the PSIPRED protein analysis workbench. Nucleic Acids Res. 41, 349–357 (2013).
Jones, D.T., Buchan, D., Cozzetto, D. & Bryson, K. The PSIPRED protein sequence analysis workbench. http://bioinf.cs.ucl.ac.uk/psipred (2016).
Dias, C. A., Teixeira, L. M., Carvalho, M. G. & Beall, B. Sequential multiplex PCR for determining capsular serotypes of pneumococci recovered from Brazilian children. J. Med. Microbiol. 56, 1185–1188 (2007).
Sorensen, U. B. Typing of pneumococci by using 12 pooled antisera. J. Clin. Microbiol. 31, 2097–2100 (1993).
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 29thl supplement M100-S29 (2019).
Toikka, P., Nikkari, S., Ruuskanen, O., Leinonen, M. & Mertsola, J. Pneumolysin PCR-based diagnosis of invasive pneumococcal infection in children. J. Clin. Microbiol. 37, 633–637 (1999).
Andrade, A. L. et al. Non-typeable Streptococcus pneumoniae carriage isolates genetically similar to invasive and carriage isolates expressing capsular type 14 in Brazilian infants. J. Infect. 61, 314–322 (2010).
Morrison, K. E. et al. Confirmation of psaA in all 90 serotypes of Streptococcus pneumoniae by PCR and potential of this assay for identification and diagnosis. J. Clin. Microbiol. 38, 434–437 (2000).
Costa, N. S. et al. MLVA Typing of Streptococcus pneumoniae isolates with emphasis on serotypes 14, 9N and 9V: comparison of previously described panels and proposal of a novel 7 VNTR loci-based simplified scheme. PLoS ONE 11, e0158651 (2016).
Enright, M. C. & Spratt, B. G. A multilocus sequence typing scheme for Streptococcus pneumoniae: Identification of clones associated with serious invasive disease. Microbiology 144, 3049–3060 (1998).
Jolley, K. A., Bray, J. E. & Maiden, M. C. J. Open-access bacterial population genomics: BIGSdb software, the PubMLST.org website and their applications. Wellcome Open. Res. 3, 124. https://doi.org/10.12688/wellcomeopenres.14826.1 (2018).
Jolley, K.A., Bray J.E. & Maiden M.C.J. Public databases for molecular typing and microbial genome diversity https://pubmlst.org/organisms/streptococcus-pneumoniae (2018).
Centers for Disease Control and Prevention. Streptococcus Laboratory. https://www.cdc.gov/streplab/pneumococcus/resources.html (2020).
Hanage, W. P. et al. Invasiveness of serotypes and clones of Streptococcus pneumoniae among children in Finland. Infect. Immun. 73, 431–435 (2005).
Hanage, W. P. et al. Using multilocus sequence data to define the pneumococcus. J. Bacteriol. 187, 6223–6230 (2005).
Kumar, S., Stecher, G., Li, M., Knyaz, C. & Tamura, K. MEGA X: Molecular evolutionary genetics analysis across computing platforms. Mol. Biol. Evol. 35, 1547–1549 (2018).
Acknowledgements
This work was supported in part by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES)—Finance Code 001, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), and Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ). The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Contributions
All authors have contributed substantially to the work reported. Conceptualization, L.M.T., F.P.G.N., V.L.C.M., and T.C.A.P.; methodology, A.R.V.S, N.S.C., S.E.C.M.P. and T.C.A.P.; formal analysis, A.R.V.S., L.M.T. and T.C.A.P.; investigation, L.M.T., F.P.G.N. and T.C.A.P.; resources, V.L.C.M., J.M.P. and L.M.T.; data curation, A.R.V.S, T.C.A.P. and L.M.T.; writing-original draft preparation, A.R.V.S, F.P.G.N., T.C.A.P; writing-review and editing, L.M.T, F.P.G.N., V.L.C.M., J.M.P., T.C.A.P and L.M.T.; supervision, V.L.C.M., J.M.P. and L.M.T.; funding acquisition, V.L.C.M., J.M.P. and L.M.T. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Souza, A.R.V., de Pina, S.E.C.M., Costa, N.S. et al. Description of optochin-resistant Streptococcus pneumoniae due to an uncommon mutation in the atpA gene and comparison with previously identified atpC mutants from Brazil. Sci Rep 11, 7936 (2021). https://doi.org/10.1038/s41598-021-87071-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-87071-8
- Springer Nature Limited