Abstract
A simple and accurate prognostic tool for Heart Failure (HF) patients is critical to improve follow-up. Different risk scores are accurate but with limited clinical applicability. The current study aims to derive and validate a simple predictive tool for HF prognosis. French outpatients with stable HF of two university hospitals were included in the derivation (N = 134) or in the validation (N = 274) sample and followed up for a median of 23 months. Potential predictors were variables with known association with mortality and easily available. The proSCANNED risk score was derived using a parametric survival model on complete case data; it includes 8 binary variables and its values are 0–8. In the validation sample, the ability of the score to discriminate the 1-year vital status was moderate (AUC = 0.71, IC95% = [0.64–0.71]). However, the stratification of the score in three groups showed a good calibration for patients in the low- and medium-risk risk group. The proSCANNED score is an easy-to-use tool in clinical practice with a good discrimination, stability, and calibration sufficient to improve the medical care of patients. Other follow up studies are necessary to assess score applicability in larger populations, and its impact.
Similar content being viewed by others
Introduction
Heart failure (HF) is a major public health concern and cause of death and hospitalization1,2. The increasing HF incidence in the population explains the growing need for new tools to enable accurate prognostic assessment. This will allow for propper treatment and monitoring, thereby improving patients’ quality of life and reducing the cost burden on the health system.
Different risk models for patients with HF have already been developed3. Most of the models are based on single cohorts of patients and some are restricted to patients with reduced left ventricular ejection fraction4,5,6 while other models are more complex, which limits their applicabillity to daily practice. The Meta-Analysis Global Group in Chronic Heart Failure (MAGGIC)7 was based on the largest available database of HF patients- 39,372 patients from 30 studies, with a median follow-up of 2.5 years and aimed to provide a user-friendly score to quantify patient mortality risk. This score was built from 13 routinely available patient characteristics and can be calculated using an online calculator. Importantly, this prediction model had an external validation by the Swedish Heart Failure Registry population8.
Although the MAGGIC score is supposed to be user-friendly, it is actually difficult to apply in practice for patients during outpatient consultation or at bedside visits because there are more than 10 characteristics to implement and the use of electronic devices is mandatory. By contrast, the CHADS score and later versions9 became a corner stone for the management of the patients due to their simplicity to use. A score available for the management of patients with HF could be valuable to guide treatment of follow-up.
Our aim was to define and validate a user-friendly, easily calculated score without using any device or website, based on the methodology and the characteristics defined by the MAGGIC score.
Material and methods
Population
Three clinical databases were used for this study. One database was used to derive the score (derivation sample); the two other databases were pooled and used for the validation (validation sample). The derivation sample included patients with stable HF who attended outpatient clinic visits in the University Hospital of Montpellier (CHU Montpellier, France) between May 2010 and February 2011. The validation sample included patients diagnosed with acute or chronic HF at least 6 months prior to study initiation, as recommended by the European Society of Cardiology10, and attending outpatient clinic visits in 2012 in the CHU Montpellier and in the University Hospital of Toulouse (France). Inclusion criteria were being older than 18 years of age and having confirmed HF diagnosis. Exclusion criteria were suffering from acute coronary syndrome within 1 month prior to induction into the study, cardiac surgery, and chemotherapy. HF etiology and treatment type had no influence on patient inclusion or exclusion.
The protocol was performed according to the principles of the Declaration of Helsinki, approved by the International Review Board of Montpellier University Hospital (198711). Following the European and French reglementation, informed consent was obtained from all patients (only adults were included). No patient stated his/her opposition to authors.
Potential predictors assessment
Comorbidities such as hypertension, diabetes, dyslipidemia, body mass index (BMI, kg/m2), atrial fibrillation (AF) (regardless of its characteristic – paroxystic or permanent), chronic obstructive pulmonary disease (COPD), smoking habits, were recorded. Other clinical variables such as age, gender, New York Heart association (NYHA) class, ischemic cardiomyopathy etiology, left ventricular ejection fraction (LVEF), presence of implantable cardioverter-defibrillator (ICD), HF medications were recorded. All these variables were prospectively collected by research teams, before the assessment of the outcome.
At each visit in cardiology wards, results of recent biological exams are checked (< 7 days); if no recent exam exists, they are completed during the visit. Nt-proBNP and Creatinine were collected in these exams. Nt-pro-Brain Natriuretic Peptide (Nt-pro-BNP, pg/mL) was determined using an immuno-electrochemiluminescence assay on the Cobas8000/e6021 immunochemistry system (Roche Diagnostics, Meylan, France). Renal function was assessed with creatinemia (μmol/L) performed on Cobas 8000/c7011 and ISE (Roche, Meylan, France). Glomular filtration rate (GFR) was estimated by Chronic Kidney Disease Epidemiology Collaboration (GFR CKD-EPI) equation.
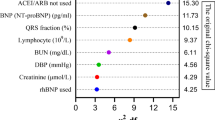
Choice of the variables to be tested in the predictive model
The original mortality model of the MAGGIC project had a high statistical power, and was validated in an external sample8. Therefore, we used the variables with the most significant prediction power from the MAGGIC model and discarded those with low prediction. Variables that were time consuming to collect or that were subject to inaccuracies (i.e. lowest systolic blood pressure (SBP), HF duration) were excluded. Interactions between variables (“interaction of ejection fraction and age” and “interaction of ejection freaction and SBP”) were also excluded. These exclusions were as such in order to establish a more “user friendly” score. Natriuretic peptides were included as potential predictors due to their increasing availability and significance as a gold-standard predictive marker of HF10,11.
The linearity of the link between quantitative predictors and time to death was assessed in univariate Cox models following validation of the proportional hazards hypothesis. When no linear link was found variables were dichotomized using thresholds that were clinically suggestive and statistically effective. The logarithm of the Nt-proBNP was used for model fitting, but results are presented using real values.
Outcome measure
The primary outcome was one-year mortality. The secondary outcome was mortality during the whole follow-up. Data collection was performed by analyzing the medical files and by phone with the cardiologist or general practitioner, the patient or the family. No blinding of outcome assessment was performed.
Statistical methods
Sample size
All patients included in the prospective database and meeting the inclusion criteria were included.
Model derivation
Poisson regression models were used to simultaneously relate baseline variables to the time to death from any cause. Since mortality risk is higher early on, the underlying Poisson rate was set in three time periods: up to 1 year, 1 to 3 years, and over 3 years. These time periods were chosen because the probability of dying within 1 year is an important prognostic feature, which helps to assess the risk–benefit balance of invasive therapeutic procedures. The model was built using backward stepwise regression targeting the minimal AIC. Missing values were not imputed.
Mortality risk score
The Poisson model predictor was converted to an integer score, which is then directly related to an individual’s probability of dying within 4.4 years (the longest follow-up). Each integer is a rounding of the exact coefficient in the Poisson model, making log rate ratio 1 equivalent to 1 point. A zero score represents a patient at lowest possible risk. Having only binary variables, the score increases by an integer amount for each risk factor. This method allows computing a predicted mortality risk at 1 year and a predicted mortality risk at the longest follow-up. We plotted the ROC curve of the score, and presented the area under the receiver operating characteristic (ROC) curve (AUC) as an overall measure of model discrimination. The 95% confidence interval of this AUC was calculated by a bootstrap method.
Validation of the score
An external validation on the validation sample was performed. The scores and predicted probabilities of death were computed. The ROC curve of the score was plotted and the AUC represents, an overall measure of model discrimination. The 95% confidence interval of this AUC was calculated by a bootstrap method. In order to assess the calibration of the score at one year, patients lost to follow-up before one year were excluded. As an overall summary measure of calibration, the observed 1-year mortality compared with the mean 1-year predicted mortality ratio was calculated.
Results
Population
173 patients were included in the derivation sample (Table 1). Of these patients only 134 had complete data and were included in the final analysis. The mean patient age was 75 year, 31% of whom were female. Most of the patients (79, 46%) presented with dyspnea graded as NYHA class III. LVEF ≤ 35% was observed in 57% of patients. Other comorbidities included hypertension in 63% of patients, 36% were diabetics, 47% had dyslipidemia, and 12% had a history of atrial fibrillation. The most common cardiomyopathy was coronary artery disease (49%). Not all patients were treated with long-term treatments (Table 1), and patients taking these medications had not all the maximal dose: mean dose of beta-blockers, ACE-I/ARB, and MRA, represented respectively 38%, 36%, and 51% of maximal dose. Overall, 65 (38%) patients died during a median follow-up of 42 months (3.5 years). Median follow-up was of 42 months (min 0 days, max 4.4 years). Table 1 further describes the derivation sample.
274 patients were included in the validation sample, with 41 death (15%). Comparatively to the derivation sample, patients of the validation sample were younger, with less comorbidities and a better NYHA status (Table 1). Median follow-up was of 23 months (min 9 days, max 4.2 years).
Model derivation
There were 11 baseline variables available for inclusion in our prognostic model. Table 1 provides their descriptive statistics and univariate analysis. As missing data could not be imputed, we derived the multivariate model on 134 patients. Using Poisson regression models for patient survival with backward stepwise variable selection, adjusting for follow-up time (higher mortality rate in early follow-up), 8 independent predictor variables were identified (Table 2).
Mortality risk score
From the risk coefficients given in Table 3, an integer score has been created. One point was attributed to each risk factor. The bell-shaped distribution of this integer risk score for all 134 patients is shown in Fig. 1. The points relate a patient’s score to his probability of dying within 1 and 4.4 years. For instance, scores of 2, 3, and 4 have 1-year probabilities of 0.05, 0.13, and 0.32, respectively. The values for scores of 6 and 7 are not represented, because they exceed the graphic zone.
Integer risk score and probability of dying within 1 and 4.4 years in the derivation sample. The histogram shows the number of patients for each score. The points and error bars show the mean predicted probabilities and their Wald’s 95% Confidence Interval. In bold, the predicted probabilities of dying within 1 year; in light, the predicted probabilities of dying within 4.4 years.
Figure 2 shows predicted mortality over 4.4 years for theoretical patients in the scores 0 to 5. One curve is drawn for each possible combination of risk factors in each score. For example, there are eight possibilities to have a score at 1, so there are eight curves. The ROC curves of the integer score for the prediction of 1 and 4.4-years mortality are displayed in Fig. 3.
ROC curves of the integer score for the prediction of 1 and 4.4-years mortality in the derivation sample. (A) 1 year mortality. (B) 4.4 years mortality. The grey shape displays the 95% confidence interval of sensitivity. ROC receiver operating characteristics. AUC area under the curve. CI confidence interval. CI were computed using a boot-strap method.
Validation of the mortality risk score
The mortality risk score was computed on 226 patients (82%) of the validation sample, due to missing values. The discrimination was good: the AUC was of 0.71 (IC 95% 0.64–0.79) (Fig. 4). The calibration is represented in Fig. 5.
ROC curves of the integer score for the prediction of 1 and 4.4-years mortality in the validation sample. The grey shape displays the 95% confidence interval of sensitivity. ROC receiver operating characteristics. AUC area under the curve. CI confidence interval. CI were computed using a boot-strap method.
Discussion
Main results
Similarly to the CHADS2 score for atrial fibrillation, we propose here a simple score easy to evaluate, in order to help clinicians to tackle heart failure. Indeed, in patients with higher score, the management has to be reinforced (drugs, rehabilitation, etc.) and patients’ education has to be implemented in these patients being in life-threatening condition. In the present study, 8 independent predictors of mortality in HF were identified. All these factors have been already described and proven to play a main role in the determination of the HF prognosis, and are routinely available in the medical history.
We based our scoring system on the original mortality model of MAGGIC7 which had a high statistical power. Comparing to the MAGGIC project our score seems to be by far easier for clinicians to use in their daily practice for several reasons: 1/we propose fewer predictors (our 8 comparing to MAGGIC’s) 2/they are easily obtained, evidenced by our low rate of missing data 3/each predictor is considered equivalent and provides 1 point which in turn can easily be calculated without the need for electronic device and thus save a valuable time for the physician. 4/Utilization of acronym “proSCANNED” (“pro” for “Nt-proBNP > 5000 pg/mL”, “S” for “smoking”, “C” for COPD, “A” for “age ≥ 75 years-old”, double N: one for “No betablockers”, the second one for “ NYHA III or IV class dyspnea”, “E” for “ejection fraction ≤ 35%”, “D” for “diabetes”) can be used to aid in the application of this score, with each item providing one point. 5/ The integer risk of proSCANNED provides an evaluation of the one-year mortality, more relevant than 3-year mortality rate studied by MAGGIC. One-year mortality appears for clinicians in practice as a critical time span not only to help them to adapt the frequency of medical consultations and to promote medical therapies increase but also to assess the risk–benefit balance for invasive therapies such as implantable cardioverter defibrillators, left ventricular assist devices or heart transplantation. In addition, especially in an elderly population, risk stratification should be repeated after one year because comorbidities may change but at the same time other predictors might also change12. Importantly, the only biological marker assessed in the score is a natriuretic peptide usually available at least once a year.
Of our selected predictors, four of them (age, NYHA class, ejection fraction and diabetes) had been previously identified by the MAGGIC model and described in other scores as well13,14. The other disease indicator of a poorer prognosis was prevalence of COPD, identified as an underdiagnosed HF comorbidity10. The most important factor in our study seems to be “no beta-blockers” with the highest rate ratio (3.55, 95% CI 1.70–7.42) already highly discussed in literature15. In regard to LVEF, it is well established that HF patients with reduced ejection fraction, in particular if below 40%, have a worse prognosis than with preserved ejection fraction7,13. In HF-ACTION, ambulatory patients with HF with systolic dysfunction (LVEF ≤ 35%) have a high rate of morbidity and mortality despite widespread use of evidence-based therapies5. Nevertheless, absolute mortality remains high in HF patients with preserved HF, thus highlighting the need to identify others prognostic factors.
The adjunction of natriuretic peptides appears crucial because they are currently recognized as gold-standard predictive markers in HF, and were already incorporate in prognostic scores of HF4,14. During HF, there is a myocardial stress resulting in neurohormonal activation by natriuretic peptides. One advantage of our score could be to underline the interest of beta-blockers each time the clinician calculates the score. Natriuretic peptides are recommended by 2013 ACC/AHA guidelines11 and 2016 ESC guidelines10 for diagnosis and prognosis in chronic HF (class I) and should be used with evidence-based treatments (2013 ACC/AHA guidelines, class IIa). Biomarkers couldn’t be included in the MAGGIC project’s model, certainly because population was recruited from studies dating from 1980 to 2006, when natriuretic peptides were not available and treatments differ greatly, considerably limiting its applicability to contemporary patients. In contrast, our proSCANNED score appears more suitable to recent guidelines and current treatments. Furthermore, the multimarker approach could represent a promising tool combining markers involved in pathophysiology of HF and might in the future lead to other markers subjoin the mortality risk score14. For example ST2, member of the interleukin 1 receptor family, marker integrating inflammation, fibrosis and cardiac stress16 in combination with C-reactive protein were demonstrated as a valuable tool for identifying patients at risk of death17 and ST2 has been proposed as a new tool for management of patients with HF18. On the other side, biomarkers will never banish clinical predictors because clinical parameters remain robust but also because the benefit of HF therapy guided by brain natriuretic peptide is depending of patients’ comorbidities19. Likewise, future studies could reveal that newest treatments of heart failure have also a high predictive power. This would need and ad-hoc study including patients eligible to newest treatments.
There are other scores in the literature predicting survival in HF. The Seattle Heart Failure Model (SHFM)6 providing an estimation of 1-, 2- and 3-year survival while integrating large amunts of clinical (excluding diabetes), pharmalogical, device and laboratory characteristics, although this makes it complicated and poorly applicable to clinical practice. In addition, the Seattle Heart Failure Model and other previous studies focused on single cohort of patients with predominantly reduced EF4,5. Other studied variables can sound very interesting but not easily available such as: exercise tests, quality of life questionnaires assessed in HF-ACTION or less attractive like percentage of lymphocyte count in SEATTLE HF model6 or ApoA-114. In opposition, the Cardiac and Comorbid Conditions HF (3C-HF)20 study aimed to predict all-cause 1-year mortality in HF patients with cardiac and comorbid variables and succeeded in balancing patients with preserved and reduced LVEF. Nevertheless 3C-HF model contains still a large number of variables and necessitated the use of electronic devices.
Forces of the study
The proSCANNED score is tailored to clinical practice and applicable for all patients with HF. Therefore, only variables that are easily available are included in this score. We provide an external validation, which is the most challenging validation method, and which is rarely done. This score is able to predict 1-year survival with good discrimination and with an area under the curve in an external validation sample of 0.71 (95%CI : 0.63–0.79), demonstrating a good calibration and stability, compared to other scores6,9,12,13,20,21.
Perspectives
Following guidelines improve outcomes22, but physicians need in clinical practice tools to better adjudicate times and means. Based on the proSCANNED score, various populations could be distinguished, guiding the management.
1/the low-risk patients with a score ≤ 2 have an expected < 5% predicted mortality at one year.
This could justify a level 1 follow-up (every 6 months by the cardiologist) with annual assessment of the natriuretic peptide and biology.
2/the medium risk patients—with a score of 3–4, have an 5–10% predicted mortality at one year.
3/the high risk patients with a score ≥ 5, which have a predicted mortality risk > 10% at one year. This could advocate for a strict follow-up with short-term reevaluation including frequent (monthly) consultation with the cardiologists, but also frequent biological or echography reevaluations.
Limitations
The first limitation is due to the small sample size, limiting the generalization at this stage. Indeed, the MAGGIC study included 39,372 patients7 and the study which demonstrated the external validation included 51,043 patients from the Swedish Heart Failure Registry8. Nevertheless, this study uses predictors already well established in very large studies, and shows a discrimination and a calibration which may be sufficient to improve the management of patients. Second, the cohort is 10 years old, and we cannot take into account the new development in HF treatments. Third, patients with a high score were scarce, preventing from the generalization to patients with multiple risk factors. This could explain the low calibration in high scores. Finally, selection bias may arise from the complete-case analysis, and from the specialized setting where patients were recruited. All these limitations may decrease the applicability to current patients. This should be assessed using an ad-hoc prospective validation study with sufficient power. Nevertheless, these results show that a user-friendly and stable score can be derived.
Finally, some aspects could be mis-evaluated, especially the compliance of the patient, his preferences or environmental factors23,24.
Conclusion
Estimating prognosis is a key element of HF management. The proSCANNED score appears as a new tool, easy to integrate in daily practice. However, it presents with limitations that may decrease its usefulness. Further studies will aim to validate and update the score on larger and more recent populations, and to assess the impact of this approach to improve the management of patients with HF.
Data availability
Data are available on demand to the corresponding author.
Abbreviations
- ACE-I:
-
Angiotensin converting enzyme inhibitor
- AF:
-
Atrial fibrillation
- ARBs:
-
Angiotensin II receptor antagonist
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- COPD:
-
Chronic obstructive pulmonary disease
- GFR:
-
Glomerular filtration rate
- HF:
-
Heart failure
- ICD:
-
Implantable cardioverter-defibrillator
- LVEF:
-
Left-ventricular ejection fraction
- MAGGIC:
-
The Meta-Analysis Global Group in Chronic Heart Failure
- MRA:
-
Mineralocorticoid receptor antagonist
- Nt-proBNP:
-
Nt-pro-Brain Natriuretic Peptide
- NYHA:
-
New York Heart Association
- P:
-
P-value
- SBP:
-
Systolic blood pressure
References
Benjamin, E. J. et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation 135, e146–e603 (2017).
Maggioni, A. P. Epidemiology of heart failure in Europe. Heart Fail. Clin. 11, 625–635 (2015).
Rahimi, K. et al. Risk prediction in patients with heart failure: A systematic review and analysis. JACC Heart Fail. 2, 440–446 (2014).
O’Connor, C. M. et al. Triage after hospitalization with advanced heart failure: The ESCAPE (Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness) risk model and discharge score. J. Am. Coll. Cardiol. 55, 872–878 (2010).
O’Connor, C. M. et al. Factors related to morbidity and mortality in patients with chronic heart failure with systolic dysfunction: The HF-ACTION predictive risk score model. Circ. Heart Fail. 5, 63–71 (2012).
Levy, W. C. et al. The Seattle Heart Failure Model: Prediction of survival in heart failure. Circulation 113, 1424–1433 (2006).
Meta-analysis Global Group in Chronic Heart F. The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;33:1750–7.
Sartipy, U., Dahlstrom, U., Edner, M. & Lund, L. H. Predicting survival in heart failure: Validation of the MAGGIC heart failure risk score in 51,043 patients from the Swedish heart failure registry. Eur. J. Heart Fail. 16, 173–179 (2014).
Camm, A. J. et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 33, 2719–2747 (2012).
Ponikowski, P. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37, 2129–2200 (2016).
Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128, 1810–1852 (2013).
Manzano, L. et al. Predictors of clinical outcomes in elderly patients with heart failure. Eur. J. Heart Fail. 13, 528–536 (2011).
Pocock, S. J. et al. Predictors of mortality and morbidity in patients with chronic heart failure. Eur. Heart J. 27, 65–75 (2006).
Wedel, H. et al. Predictors of fatal and non-fatal outcomes in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA): Incremental value of apolipoprotein A-1, high-sensitivity C-reactive peptide and N-terminal pro B-type natriuretic peptide. Eur. J. Heart Fail. 11, 281–291 (2009).
O’Connor, C. M. et al. Predictors of mortality after discharge in patients hospitalized with heart failure: An analysis from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). Am. Heart J. 156, 662–673 (2008).
Dieplinger, B. & Mueller, T. Soluble ST2 in heart failure. Clin. Chim. Acta. 443, 57–70 (2015).
Dupuy, A. M. et al. Multi-marker strategy in heart failure: Combination of ST2 and CRP predicts poor outcome. PLoS ONE 11, e0157159 (2016).
Curinier, C. et al. Evaluation of the sST2-guided optimization of medical treatments of patients admitted for heart failure, to prevent readmission: Study protocol for a randomized controlled trial. Contemp. Clin. Trials 66, 45–50 (2018).
Brunner-La Rocca, H. P. et al. Which heart failure patients profit from natriuretic peptide guided therapy? A meta-analysis from individual patient data of randomized trials. Eur. J. Heart Fail. 17, 1252–1261 (2015).
Senni, M. et al. Predicting heart failure outcome from cardiac and comorbid conditions: The 3C-HF score. Int. J. Cardiol. 163, 206–211 (2013).
Vazquez, R. et al. The MUSIC Risk score: A simple method for predicting mortality in ambulatory patients with chronic heart failure. Eur. Heart J. 30, 1088–1096 (2009).
Cowie, M. R. & Komajda, M. Quality of physician adherence to guideline recommendations for life-saving treatment in heart failure: An International Survey. Card. Fail. Rev. 3, 130–133 (2017).
Goldberg, L. R. & Jessup, M. A time to be born and a time to die. Circulation 116, 360–362 (2007).
Aaronson, K. D. & Cowger, J. Heart failure prognostic models: Why bother?. Circ. Heart Fail. 5, 6–9 (2012).
Author information
Authors and Affiliations
Contributions
CD, KS, and FR contributed to the conception of the work. RI, JR, ALG, BM, EK, FH, AA, DD, JCM contributed to the acquisition of data. CD and KS contributed to the analysis of data. CD, KS, and FR contributed to the interpretation of data and drafted the manuscript. MG, FL, and GM substantially revised the manuscript. All Authors approved the submitted version and agree to be personnaly accountable for the entire work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duflos, C., Solecki, K., Galinier, M. et al. Conception and bicentric validation of the proSCANNED score, a simplified bedside prognostic score for Heart Failure patients. Sci Rep 11, 6179 (2021). https://doi.org/10.1038/s41598-021-85767-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-85767-5
- Springer Nature Limited