Abstract
There is growing evidence for a role of maternal diabetes in the pathogenesis of neurodevelopmental disorders. However, the specific association between gestational diabetes (GDM), as opposed to pre-gestational diabetes, has been poorly isolated. Thus the aim was to systematically review and meta-analyse literature pertaining to prevalence and risk for two neurodevelopmental disorders: autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD), when exposed to GDM. PubMed, Cochrane Library, EMBASE, PsycINFO and CINAHL were systematically searched for eligible literature, with forward and backward citation tracking. Screening for eligibility, risk of bias assessment and data extraction were performed by two independent reviewers. 18 studies measuring ASD and 15 measuring ADHD met inclusion criteria. On meta-analysis there was an increased risk of ASD (OR 1.42; 95% CI 1.22, 1.65) but not ADHD (OR 1.01; 95% CI 0.79, 1.28). We discuss potential mechanisms for these differing risks. Greater understanding of risk factors, including GDM, for these neurodevelopmental disorders and potential mechanisms may help inform strategies aimed at prevention of exposure to these adversities during pregnancy.
Similar content being viewed by others
Introduction
Gestational diabetes (GDM) is glucose intolerance that begins during pregnancy and has an estimated prevalence of between 1.8% and 22.3% in Europe, with higher rates in Africa, North and South America and the Middle East1. It is associated with adverse outcomes for mother and baby, including obstetric complications such as emergency Caesarean delivery and longer-term risks of Type 2 Diabetes in the mother and metabolic syndrome in offspring2.
There is also some emerging evidence for a relationship between GDM and adverse neurobehavioural outcomes in children. Several systematic reviews suggest an association between maternal diabetes and lower IQ scores, language impairment and symptoms of attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD). However, many of these reviews group together women experiencing pregestational (Type 1 and Type 2) and gestational diabetes so do not investigate the effect of GDM specifically3,4,5,6,7,8. While GDM and pregestational diabetes share similar pathology of insulin resistance, in GDM this insulin resistance arises only during pregnancy, which is itself a state of insulin resistance. Therefore, while there may be some women diagnosed with GDM who have undiagnosed pregestational diabetes, the pathology is slightly different between the two conditions. There are many potential mechanisms that may underpin such an association between GDM and adverse offspring neurobehavioural outcomes. There may be mediating factors of obstetric and neonatal adversities such as pre-eclampsia or infants born large for gestational age9,10,11. There may also be epigenetic changes12 or oxidative stress13,14 resulting from a hyperglycaemic in-utero environment.
Thus, the aim of this study was to conduct a systematic review and meta-analysis of the prevalence and risk for ADHD and ASD in children of women affected specifically by GDM. Both ADHD and ASD are commonly diagnosed neurodevelopmental disorders encompassing a spectrum of neurobehavioural symptoms that are often diagnosed from a young age. ADHD has a global prevalence of around 5%15, is characterised by symptoms of inattention and hyperactivity16 and often has broad and enduring adverse impacts on quality of life and functioning17. ASD describes a range of conditions characterised by some or all of: impaired communication, impaired social interaction and repetitive, restricted and stereotyped behaviour16 and may also result in profound struggles in both personal and professional life. A range of pathophysiological mechanisms have been implicated for these neurodevelopmental disorders, including hyperglycaemia during pregnancy18. Thus, a greater understanding of the aetiology of these disorders could help to identify early life risk factors for their development.
Methods
The review followed ‘Meta-analysis of Observational Studies in Epidemiology’ (MOOSE)19 and ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (PRISMA) guidelines20 and was registered with PROSPERO (CRD42019128376).
Search strategy
An electronic literature search was performed in the databases PubMed, Cochrane Library, EMBASE, PsycINFO and CINAHL from inception to 04/04/2019, with forward and backward citation tracking of eligible papers. Search terms were adapted from previous systematic reviews in the area (see supplementary material). Two separate searches were conducted for ASD and ADHD.
Study selection
Inclusion criteria were: published, peer-reviewed studies with children aged 18 and under, whose mothers had clinically diagnosed GDM during pregnancy and who were investigated for symptoms and/or diagnosis of ASD or ADHD. Report of symptoms of ASD and ADHD by questionnaires or other tests was accepted and clinical diagnosis was accepted through self-report, report from medical professionals or medical records. Either self-report of GDM, report from medical professionals, or medical records was accepted. Observational studies and baseline data from intervention studies were included, in any language.
Exclusion criteria were: case studies, editorials, reviews and conference abstracts. Non-human studies were also excluded. Studies which were known to include women with established pregestational diabetes were excluded, unless it was possible to extract data pertaining specifically to GDM. Studies in which there was some doubt surrounding this were included in the review but not included in the meta-analysis.
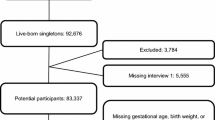
Two independent reviewers screened titles and abstracts then full texts for eligibility. Results of study selection are presented in Figs. 1 and 2.
Data extraction and risk of bias assessment
Two independent reviewers extracted data, including study characteristics, prevalence and odds ratios (ORs) and any information on mechanisms for the associations. Study authors were e-mailed to request raw data if potentially relevant data may be available.
Risk of bias in all included studies was also assessed by two independent reviewers using a pre-piloted modified Newcastle Ottawa Scale (see supplementary material). Scores for selection bias and measurement bias were of particular interest as most of the studies were of observational design. Each question in the tool had a score of zero to two (low to high risk of bias). A score of two on any item within the selection and measurement bias domains meant that the study was categorised as having a high risk of bias.
Data synthesis
Meta-analyses of ORs and prevalence were undertaken separately for ASD and ADHD if at least five studies were available21. In studies providing only prevalence data, ORs were calculated from this data (or raw data provided by authors). If there was any doubt as to whether or not pregestational diabetes had been excluded from the comparison group without GDM, these studies’ ORs were not included in meta-analysis.
Data were analysed using Stata 15. Metan and metaprop commands were used to produce pooled unadjusted ORs and prevalence and 95% confidence intervals (CIs) displayed as forest plots. Insufficient numbers of studies adjusted for similar characteristics to enable pooling of adjusted ORs. DerSimonian-Laird random effects meta-analysis22 was used as there was expected to be substantial heterogeneity between studies23,24. Heterogeneity was assessed using I2: proportion of total variation in study estimates that is due to heterogeneity25. It was decided a-priori that I2 > 75% would preclude meta-analysis as this represents considerable heterogeneity26. Both of the prevalence meta-analyses produced I2 > 75% so prevalence is presented as median with interquartile range (IQR) as a standard summary measure of non-parametric data. Sensitivity analyses on effect of risk of bias were conducted when sufficient studies were available. Publication bias was not assessed for the meta-analyses as there were insufficient numbers of studies (less than ten)27.
Results
Characteristics of ASD studies
18 studies measuring ASD were identified; three of these also measured ADHD. Table 1 provides a summary of their characteristics and findings. Nine of these studies were from North America. Four were from middle income countries; none were from low- income countries (according to World Bank classification at June 2019). All studies were observational. Most of the studies used medical records or parental report of ASD and GDM; diagnostic criteria for GDM were usually not reported. 11 of the studies were assessed as high risk of bias due to lack of information about how GDM or ASD was diagnosed, increasing the risk of measurement bias and/or lack of information about selection criteria preventing accurate assessment of risk of selection bias.
Pooled odds and prevalence of ASD in those exposed to GDM
Data on prevalence of ASD in those exposed to GDM were available for 15 studies; there were three studies which measured ASD and GDM but from which prevalence data could not be extracted28,29,30 (see Table 1). Heterogeneity on meta-analysis of these 15 studies was 98%, precluding meta-analysis. Median prevalence was 16.3% (IQR 0.9–48.8%).
Eight of these studies were included in a meta-analysis of ORs. Studies were excluded in the absence of a control group or if there was doubt that pregestational diabetes had been excluded from the control group (not specifically mentioned in the exclusion criteria and no response to an e-mail to clarify). Pooled unadjusted OR was 1.42 (95% CI 1.22, 1.65) with heterogeneity 29% (see Fig. 3).
Characteristics of ADHD studies
15 studies measuring ADHD were identified. Table 2 provides a summary of their characteristics and findings. Compared to those studies measuring ASD, more of these studies were from European countries. All studies were observational; ten were prospective cohorts but there were less population-based cohorts than in the ASD literature so sample sizes were generally smaller. Moreover, measurement of symptoms using questionnaires were more frequently used in the ADHD literature (as opposed to diagnoses) and this in part led to only two studies being assessed as low to moderate risk of bias.
Pooled odds and prevalence of ADHD in those exposed to GDM
Data on prevalence of ADHD in those exposed to GDM were available for eight studies. Heterogeneity on meta-analysis of prevalence from these eight studies was 93.7%, precluding meta-analysis. Median prevalence was 14.4% (IQR 6.7–41.3%).
Studies not included in meta-analysis were those presenting numerical scores on a symptom-based questionnaire, as opposed to numbers scoring above or below a defined threshold, precluding the calculation of prevalence or odds (see Table 2). Relatively small numbers of children are included in these studies, with only one study including over 100 children exposed to GDM31. All but one of these studies found no evidence of differences in scores between GDM exposed and unexposed children; one study found some evidence for greater concentration and inattention symptoms in children of mothers with versus those without GDM32, which was attenuated on adjustment for a range of obstetric, neonatal and sociodemographic confounders (see Table 2)..
Five of the eight studies providing information on prevalence were included in a meta-analysis of ORs; three studies were excluded for the same reasons as in the ASD meta-analysis i.e. unable to verify that pregestational diabetes had been excluded from the control population. Pooled unadjusted OR was 1.01 (95% CI 0.79, 1.28) with heterogeneity 26.2% (see Fig. 4).
Sensitivity analyses
In the meta-analysis of ORs for ASD, it appeared that effect sizes were slightly larger for those studies at low to moderate risk of bias. However, removal of the two studies at high risk of bias from the meta-analysis resulted in little change. Indeed, the pooled OR was slightly reduced at 1.39 (95% CI 1.19, 1.63). There were insufficient numbers of studies to facilitate the same sensitivity analysis for ADHD.
Discussion
Main findings
Pooled OR for risk of ASD following exposure to GDM was 1.42 (95% CI 1.22, 1.65) and for ADHD was 1.01 (0.79, 1.28). In general, studies measuring ADHD more often utilised screening tools of symptoms in smaller populations than the studies measuring ASD, which more often measured clinical diagnoses within larger population-based cohorts. Median prevalence of ASD of 16.3% and ADHD of 14.4% in those exposed to GDM is higher than that estimated in the general population15,33. However, there was substantial heterogeneity between studies included in these estimates, also reflected in wide IQRs for these medians and indicative of the broad range of study designs, populations and measures of both exposure and outcomes. That ORs in these studies when comparing risk in the GDM exposed versus unexposed were only modestly elevated also suggests that rates of ASD and/or ADHD were elevated in the study population as a whole, either due to selection of at-risk samples or due to systematic measurement of symptoms. Nonetheless, pooled unadjusted OR for risk of ASD in those exposed to GDM of 1.42 provides some evidence for a slightly increased risk, not seen to the same extent for ADHD (OR 1.01). Two previous meta-analyses investigating only risk for ASD found an increased risk; one with a pooled relative risk (RR) of 1.63 had substantially more heterogeneity (I2 75%)7 and the other with RR between 1.48 and 1.72 did not separate pregestational and gestational diabetes6. In contrast to our meta-analysis, in a meta-analysis of risk for ADHD following exposure to GDM across four studies, RR was 2.0 (95% CI 1.42, 2.81)5. However, as previously discussed, these meta-analyses did not specifically exclude pregestational diabetes from their control populations, which may explain the difference in results.
Strengths and limitations
This is the first study to our knowledge that has rigorously reviewed the literature and meta-analysed prevalence and risk from studies pertaining to both diagnoses and symptoms of ASD and ADHD. Using the same review strategy for more than one neurodevelopmental disorder allows a direct comparison of risk across a range of disorders. Another unique strength of this review is the exclusion from meta-analysis those studies in which pregestational diabetes was not removed from the control population. As previously discussed, pregestational and gestational diabetes differ somewhat in their pathology which could have implications for the degree of risk for adverse neurobehavioural outcomes and potential mechanistic pathways discussed below. However, just as the degree of glucose intolerance may differ between pregestational and gestational diabetes, it can also differ between populations with GDM due to widespread variation in diagnostic criteria. A significant limitation of the studies included within this review is that most of them do not provide information on GDM diagnostic criteria or any other indicators of GDM severity such as use of insulin or medication. Yet there is now evidence that maternal hyperglycaemia even below that of diagnostic threshold for GDM may be associated with adverse obstetric and neonatal outcomes34. It may be useful for future studies to investigate the impact of severity of maternal hyperglycaemia on risk for neurodevelopmental disorders; for example, whether or not there is a dose response relationship between maternal glucose levels and risk for disorder.
Lack of reporting on GDM diagnostic criteria within the included studies is one of the reasons why over half of the studies were assessed as at high risk of bias, although removal of studies at high risk of bias in the ASD meta-analysis of ORs resulted in minimal change to the effect estimate. However, there was also substantial diagnostic heterogeneity in the outcome of neurodevelopmental disorders, particularly in ADHD, where a broad range of questionnaires measuring levels of symptoms of ADHD were measured, which may not have met diagnostic threshold. Insufficient numbers of studies were available for ADHD to explore the impact that this may have had within a sensitivity analysis. A further limitation of the studies included within this review is that only some investigated the influence of other factors on the GDM and neurodevelopmental disorders association. This is discussed further below.
Potential mechanisms
The differences in risk between ASD and ADHD found in this review could be due to differing causal pathways, although clearly there are limitations to inferring any causality from observational studies. It could also be due to differences in the exposure, specifically degree of hyperglycaemia, although as previously discussed, this is often difficult to assess as so few studies consider it. Another possibility is that smaller sample sizes in the ADHD studies have failed to provide sufficient power to detect a difference in risk.
There were a few studies which looked at possible indicators of severity of GDM and degree of hyperglycaemia. For example, studies comparing GDM treated with medication versus without suggested an increased risk in medication-treated groups for both ASD35 and ADHD36. The pathway through which hyperglycaemia may impact neurodevelopment may be mediated by oxidative stress, which has been associated with adverse neurobehavioural outcomes such as motor deficits13. It may also influence epigenetic changes in the offspring, such as reduced DNA methylation seen in neurodevelopmental disorders such as ASD14. Moreover, hyperglycaemia can lead to systemic inflammation and pro-inflammatory cytokines are able to cross the placenta and the foetal blood–brain barrier, which may affect neurodevelopment37. However, there may be critical periods of exposure to hyperglycaemia during pregnancy for the different neurodevelopmental conditions. Xiang et al. have conducted analyses in a large population-based cohort on risk for both ASD38 and ADHD36 following exposure to maternal diabetes. They found that the later the GDM is diagnosed, the lesser the risk of ASD but saw no association with ADHD which may indicate differing critical periods.
Women with GDM are at a greater risk of several adverse obstetric outcomes, such as pre-eclampsia, foetal macrosomia, perinatal mortality, Caesarean delivery and preterm delivery9,39, which may also increase the risk of neurodevelopmental disorders40. While some studies presented data on gestational age at birth and birthweight, none explored their role as a potential mediator. A number of studies also investigated the role of obesity and socioeconomic status (SES) as effect modifiers of the association between GDM and neurodevelopmental disorders. Higher body mass index (BMI) increased the risk of both ASD29,41 and ADHD29,42,43 following exposure to GDM. Likewise, low SES has been shown to further increase the risk of ADHD44,45 following exposure to GDM, although this has been less explored in ASD.
Implications and conclusions
Therefore, future potential areas for research include an investigation of these mechanistic pathways underlying the association between maternal hyperglycaemia across the spectrum of subclinical, gestational and pregestational diabetes, and adverse neurobehavioural outcomes. Baseline risk for neurodevelopmental disorders in the general population is relatively low so absolute risk for a neurodevelopmental disorder in the offspring of mothers with GDM is still relatively low and there are many children exposed to GDM during pregnancy who do not develop a neurodevelopmental disorder. This supports an approach to measuring risk on a continuum and is one of the reasons that we chose to include symptoms of disorder in addition to clinical diagnoses.
A greater understanding of the early determinants of a child’s cognitive, social and emotional wellbeing would add support to interventions aimed at better management of these adversities, such as GDM, during pregnancy. Access to information about their condition has been identified as an enabler for women with GDM to manage their condition46. Such information could include sensitively informing women about potential risks to their baby. There is now evidence that effective management results in reductions in obstetric morbidities such as shoulder dystocia and pre-eclampsia47. However, there is also some evidence to support an inverse correlation between level of hyperglycaemia in pregnancy and longer-term neurobehavioral outcomes in offspring, such as verbal IQ48.
Furthering knowledge of these early predictors of adverse neurobehavioural outcomes would also underscore the importance of interventions aimed at prevention of such adverse pregnancy exposures by targeting their broader determinants in early pregnancy or even earlier in the preconception period. For example, there is some evidence that diet and physical activity interventions in early pregnancy reduce gestational weight gain and may be associated with a reduced risk of GDM49. That a number of studies included in the review found that socioeconomic status was an effect modifier of the association between GDM and neurodevelopmental disorders also highlights the importance of considering the broader determinants of health within healthcare. Thus there are a number of points at which healthcare professionals and policy makers involved in the care of women and children affected by GDM may usefully intervene.
In conclusion, there may be an association between GDM and the neurodevelopmental disorders of ASD and ADHD, with potentially differing levels of risk and mechanistic pathways for different neurodevelopmental disorders. Greater understanding of these risks and mechanisms may help to modify potential adverse developmental trajectories from becoming established in children.
References
Zhu, Y. & Zhang, C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: A global perspective. Curr. Diab. Rep. 16, 7 (2016).
Kampmann, U. et al. Gestational diabetes: A clinical update. World J. Diabetes. 6, 1065–1072 (2015).
Aguilar Cordero, M. J. et al. Diabetes mellitus materna y su influencia en el neurodesarrollo del niño; revisión sistemática. Nutr. Hosp. 32, 2484–2495 (2015).
Camprubí Robles, M. et al. Maternal diabetes and cognitive performance in the offspring: A systematic review and meta-analysis. PLoS One. 10, e0142583, https://doi.org/10.1371/journal.pone.0142583 (2015).
Zhao, L. et al. The association of maternal diabetes with attention deficit and hyperactivity disorder in offspring: A meta-analysis. Neuropsychiatr. Dis. Treat. 15, 675–684 (2019).
Xu, G., Jing, J., Bowers, K., Liu, B. & Bao, W. Maternal diabetes and the risk of autism spectrum disorders in the offspring: A systematic review and meta-analysis. J. Autism Dev. Disord. 44, 766–775 (2014).
Wan, H., Zhang, C., Li, H., Luan, S. & Liu, C. Association of maternal diabetes with autism spectrum disorders in offspring: A systematic review and meta-analysis. Medicine. 97, e9438, https://doi.org/10.1097/MD.0000000000009438 (2018).
Perna, R., Loughan, A. R., Le, J. & Tyson, K. Gestational diabetes: Long-term central nervous system developmental and cognitive sequelae. Appl. Neuropsychol. Child. 4, 217–220 (2015).
Wendland, E. M. et al. Gestational diabetes and pregnancy outcomes - A systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childb. 12, 23 (2012).
Moore, G. S., Kneitel, A. W., Walker, C. K., Gilbert, W. M. & Xing, G. Autism risk in small-and large-for-gestational-age infants. Am. J. Obstet. Gynecol. 206(314), e1-314.e9. https://doi.org/10.1016/j.ajog.2012.01.044 (2012).
Maher, G. M. et al. Association of hypertensive disorders of pregnancy with risk of neurodevelopmental disorders in offspring: A systematic review and meta-analysis. JAMA Psychiatry. 78, 809–819 (2018).
Latham, K. E., Sapienza, C. & Engel, N. The epigenetic lorax: Gene–environment interactions in human health. Epigenomics. 4, 383–402 (2011).
Wells, P. G. et al. Oxidative stress in developmental origins of disease: Teratogenesis, neurodevelopmental deficits, and cancer. Toxicol. Sci. 108, 4–18 (2009).
Deth, R., Muratore, C., Benzecry, J., Power-Charnitsky, V. A. & Waly, M. How environmental and genetic factors combine to cause autism: A redox/methylation hypothesis. Neurotoxicology. 29, 190–201 (2008).
Polanczyk, G., de Lima, M. S., Horta, B. L., Biederman, J. & Rohde, L. A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry. 164, 942–948 (2007).
World Health Organisation. International Statistical Classification of Disease and Related Health Problems (10th revision). https://icd.who.int/browse10/2016/en (2016).
Harpin, V. A. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch. Dis. Child. 90, 2–7 (2005).
Hami, J. et al. Some of the experimental and clinical aspects of the effects of the maternal diabetes on developing hippocampus. World J. Diabetes. 15, 412–422 (2015).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283, 2008–2012 (2000).
Moher, D. et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6, e1000097, https://doi.org/10.1371/journal.pmed.1000100 (2009).
Tufanaru, C., Munn, Z., Stephenson, M. & Aromataris, E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int. J. Evid. Based Healthc. 13, 196–207 (2015).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin. Trials. 7, 177–188 (1986).
Schmidt, F. L., Oh, I. S. & Hayes, T. L. Fixed- versus random-effects models in meta-analysis: Model properties and an empirical comparison of differences in results. Br. J. Math. Stat. Psychol. 62, 97–128 (2009).
Higgins, J. P. T., Thompson, S. G. & Spiegelhalter, D. J. A re-evaluation of random-effects meta-analysis. J. R. Stat. Soc. Ser. A Stat. Soc. 172, 137–159 (2009).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Higgins, J. P. T., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Sterne, J.A.C. et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 343, d4002, https://doi.org/10.1136/bmj.d4002 (2011).
Alshaban, F. et al. Prevalence and correlates of autism spectrum disorder in Qatar: A national study. J. Child Psychol. Psychiatry. 60, 1254–1268 (2019).
Kong, L., Norstedt, G., Schalling, M., Gissler, M. & Lavebratt, C. The risk of offspring psychiatric disorders in the setting of maternal obesity and diabetes. Pediatrics. 142, e20180776, https://doi.org/10.1542/peds.2018-0776 (2018).
Maramara, L. A., He, W. & Ming, X. Pre- and perinatal risk factors for autism spectrum disorder in a New Jersey cohort. J. Child Neurol. 29, 1645–1651 (2014).
Wolford E. et al. Maternal depressive symptoms during and after pregnancy are associated with attention-deficit/hyperactivity disorder symptoms in their 3- to 6-year-old children. PLoS One. 12, e0190248, https://doi.org/10.1371/journal.pone.0190248 (2017).
Veena, S. R. et al. Childhood cognitive ability: Relationship to gestational diabetes mellitus in India. Diabetologia 53, 2134–2138 (2010).
Baxter, A. J. et al. The epidemiology and global burden of autism spectrum disorders. Psychol. Med. 45, 601–613 (2015).
Metzger, B. E. et al. Hyperglycemia and adverse pregnancy outcomes. N. Engl. J. Med. 358, 1991–2002 (2008).
Sacks, K.N. et al. Prenatal exposure to gestational diabetes mellitus as an independent risk factor for long-term neuropsychiatric morbidity of the offspring. Am. J. Obstet. Gynecol. 215, 380.e.1–380.e7, https://doi.org/10.1016/j.ajog.2016.03.030 (2016).
Xiang, A. H. et al. Maternal gestational diabetes mellitus, type 1 diabetes, and type 2 diabetes during pregnancy and risk of ADHD in offspring. Diabetes Care 41, 2502–2508 (2018).
Buehler, M. R. A proposed mechanism for autism: an aberrant neuroimmune response manifested as a psychiatric disorder. Med Hypotheses. 76, 863–870 (2011).
Xiang, A. H. et al. Association of maternal diabetes with autism in offspring. JAMA 313, 1425–1434 (2015).
Billionnet, C. et al. Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012. Diabetologia 60, 636–644 (2017).
Schieve, L. A. et al. Population impact of preterm birth and low birth weight on developmental disabilities in US children. Ann Epidemiol. 26, 267–274 (2016).
Connolly, N. et al. Maternal metabolic risk factors for autism spectrum disorder—An analysis of electronic medical records and linked birth data. Autism Res. 9, 829–837 (2016).
Li, M. et al. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics. 137, e20152206, https://doi.org/10.1542/peds.2015-2206 (2016).
Mina, T. H. et al. Prenatal exposure to very severe maternal obesity is associated with adverse neuropsychiatric outcomes in children. Psychol Med. 47, 353–362 (2017).
Nomura, Y. et al. Exposure to gestational diabetes mellitus and low socioeconomic status: Effects on neurocognitive development and risk of attention-deficit/hyperactivity disorder in offspring. Arch. Pediatr. Adolesc. Med. 166, 337–343 (2012).
Schmitt, J. & Romanos, M. Prenatal and perinatal risk factors for attention-deficit/hyperactivity disorder. Arch. Paediatr. Adolesc. Med. 166, 1074–1075 (2012).
Martis, R., Brown, J., McAra-Couper, J. & Crowther, C.A. Enablers and barriers for women with gestational diabetes mellitus to achieve optimal glycaemic control—A qualitative study using the theoretical domains framework. BMC Pregnancy Childb. 18, 91, https://doi.org/10.1186/s12884-018-1710-8 (2018).
Hartling, L. et al. Benefits and harms of treating gestational diabetes mellitus: a systematic review and meta-analysis for the U.S. preventive services task force and the national institutes of health office of medical applications of research. Ann. Intern. Med. 159, 123–129 (2013).
Ornoy, A. Growth and neurodevelopmental outcome of children born to mothers with pregestational and gestational diabetes. Pediatr. Endocrinol. Rev. 3, 104–113 (2005).
Oteng-Ntim, E., Varma, R., Croker, H., Poston, L. & Doyle, P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: Systematic review and meta-analysis. BMC Med. 10, 47, https://doi.org/10.1186/1741-7015-10-47 (2012).
Burstyn, I., Sithole, F. & Zwaigenbaum, L. Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Dis. Can. 30, 125–134 (2010).
Chien, Y. L. et al. Prenatal and perinatal risk factors and the clinical implications on autism spectrum disorder. Autism. 23, 783–791 (2018).
Dodds, L. et al. The role of prenatal, obstetric and neonatal factors in the development of autism. J. Autism Dev. Disord. 41, 891–902 (2011).
George, B., Padmam, M. S., Nair, M. K., Leena, M. L. & Russell, P. S. CDC Kerala 13: Antenatal, natal and postnatal factors among children (2–6 y) with autism—A case control study. Indian J Pediatr. 81, 133–137 (2014).
Hadjkacem, I. et al. Prenatal, perinatal and postnatal factors associated with autism spectrum disorder. J. Pediatr. (Rio J). 92, 595–601 (2016).
Kania, M. et al. The association of maternal gestational diabetes mellitus with autism spectrum disorders in the offspring. Clin. Diabetol. 5, 147–151 (2016).
Khanom, F., Chowdhury, S., Ahmed, S., Moniruzzaman, M. & Ahmed, M. S. A. M. Association of autism spectrum disorder and gestational diabetes mellitus of mothers in Bangladesh. Indian J. Commun. Health. 27, 391–397 (2015).
Krakowiak P. et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics. 129, e1121, https://doi.org/10.1542/peds.2011-2583 (2012).
Li M. et al. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics. 137, e20152206, https://doi.org/10.1542/peds.2015-2206 (2016).
Raz, R. et al. Autism spectrum disorder and particulate matter air pollution before, during, and after pregnancy: A nested case-control analysis within the Nurses’ Health Study II cohort. Environ. Health Perspect. 123, 264–270 (2015).
Say, G. N., Karabekiroğlu, K., Babadağı, Z. & Yüce, M. Maternal stress and perinatal features in autism and attention deficit/hyperactivity disorder. Pediatr. Int. 58, 265–269 (2016).
Straughen, J. K. et al. The association between placental histopathology and autism spectrum disorder. Placenta 57, 183–188 (2017).
Akaltun İ., Yapça Ö.E., Ayaydin H. & Kara T. An evaluation of attention deficit hyperactivity disorder and specific learning disorder in children born to diabetic gravidas: A case control study. Anadolu Psikiyatr De. 20, https://doi.org/10.5455/apd.10445 (2019).
Chiu, Y. N., Gau, S. S. F., Tsai, W. C., Soong, W. T. & Shang, C. Y. Demographic and perinatal factors for behavioral problems among children aged 4–9 in Taiwan. Psychiatry Clin. Neurosci. 63, 569–576 (2009).
Daraki, V. et al. Effect of parental obesity and gestational diabetes on child neuropsychological and behavioral development at 4 years of age: The Rhea mother–child cohort, Crete, Greece. Eur. Child Adolesc. Psychiatry. 26, 703–714 (2017).
Galera, C. et al. Prenatal diet and children’s trajectories of hyperactivity-inattention and conduct problems from 3 to 8 years: The EDEN mother-child cohort. J. Child Psychol. Psychiatry. 59, 1003–1011 (2018).
Ornoy, A., Wolf, A., Ratzon, N., Greenbaum, C. & Dulitzky, M. Neurodevelopmental outcome at early school age of children born to mothers with gestational diabetes. Arch. Dis. Child Fetal Neonatal Ed. 81, F10-14 (1999).
Pohlabeln, H. et al. Further evidence for the role of pregnancy-induced hypertension and other early life influences in the development of ADHD: Results from the IDEFICS study. Eur. Child Adolesc. Psychiatry. 26, 957–967 (2017).
Acknowledgements
The authors wish to thank those who contributed raw data: Yoko Nomura (Queens College, City University of New York, USA), Hermann Pohlabeln (Leibniz Institute for Prevention Research and Epidemiology- BIPS, Germany), Rebecca Reynolds (University of Edinburgh, UK) and Marius Lahti-Pulkkinen (University of Helsinki, Finland). CAW carried out this work as part of a Medical Research Council (MRC) funded Clinical Research Training Fellowship (MR/P019293/1).
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study conception and design. Literature search was performed by J.R. Study selection, data collection and risk of bias assessment was performed by J.R. and C.A.W. Meta-analysis was conducted by C.A.W. The first draft of the manuscript was written by J.R. and C.A.W. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rowland, J., Wilson, C.A. The association between gestational diabetes and ASD and ADHD: a systematic review and meta-analysis. Sci Rep 11, 5136 (2021). https://doi.org/10.1038/s41598-021-84573-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84573-3
- Springer Nature Limited