Abstract
The reduced (GSH)-to-oxidized (GSSG) glutathione ratio represents a dynamic balance between oxidants and antioxidants. However, redox status in adolescents with obesity and anemia has not been investigated. This study investigated the association of erythrocyte GSH redox status (GSH, GSH:GSSG ratio, and glutathione peroxidase [GPx] activity) with anemia and adiposity in adolescents. This case–control study nested in a cross-sectional study enrolled 524 adolescents (268 boys; 256 girls). The prevalence of anemia in overweight and obesity (OWOB) was 5.2% in boys and 11.7% in girls. The GSH:GSSG ratio and GPx activity were significantly higher in girls than in boys (p < 0.001), in anemic than in non-anemic subjects (p < 0.001), and in OWOB than in normal-weight subjects (p < 0.001). Similarly, significantly higher GSH: GSSG level (p < 0.001) and GPx activity (p < 0.001) were found in subjects with 90th percentile waist circumference than in those with < 90th percentile. GPx and GSH:GSSG were positively associated with anemia after adjusting for age, sex, and body mass index (adjusted odds ratio, adjOR [95% confidence interval, CI] 2.18 [1.44–3.29]) or tertiles (adjOR [95% CI], T3 = 2.49 [1.03–6.01]). A similar association was noted for GSH and GPx. A compensatory increased redox defense mechanism exists in anemia and obesity among adolescents without metabolic disturbances.
Similar content being viewed by others
Introduction
Obesity and iron deficiency anemia are two common global childhood disorders that have a significant impact on lifelong health. Accumulating evidence indicates that children and adolescents with obesity are at a greater risk of iron deficiency (ID) and iron deficiency anemia (IDA) than their normal-weight (NW) peers1,2. Although the relationship between obesity and anemia has not been fully delineated, obese subjects appear to be at a greater risk of IDA due to several risk factors such as chronically low iron intake and increased blood volume due to a higher adipose tissue mass3. Obesity is a state of chronic low-grade inflammation associated with increased circulatory levels of proinflammatory cytokines that have been proposed to link anemia and obesity3,4. High levels of interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF)-α in obesity have been indicated to induce the dysregulation of the iron regulatory hormones hepcidin and lipocalin-2. This dysregulation leads to low circulatory iron and intracellular iron overload in adipose tissues5,6,7,8. The generation of reactive oxygen species (ROS) in obesity appears to be triggered by the increased levels of proinflammatory cytokines and by the intracellular iron overload, which then dysregulates adipocytes’ mitochondrial function7. This phenomenon creates a vicious cycle in which increased levels of adipokines generate ROS, and high levels of ROS dysregulate body weight by modulating satiety and appetite signals at the hypothalamic level9,10,11. Thus, the dysregulated iron homeostasis is not only the consequence of obesity but could also be involved in the pathogenesis of obesity-related morbidities such as insulin resistance and diabetes7.
An imbalance in the antioxidant network through the enhanced generation of ROS or depletion of antioxidants leads to oxidative stress. Sulfhydryl-rich molecules play a critical role in the antioxidant network. Glutathione (GSH), a tripeptide, is a key component in its reduced form in the cellular antioxidant defense system12,13. Through a reaction catalyzed by a selenium-dependent enzyme, glutathione peroxidase (GPx), GSH donates its hydrogen to the highly reactive ROS and converts them into more stable compounds. In such reactions, two GSH molecules dimerize through a disulfide bond to form oxidized glutathione (GSSG)14. The ratio of GSH to GSSG (GSH:GSSG ratio) is a commonly used sensitive early biomarker of the whole-body redox status15,16. Cellular alterations in the GSH:GSSG ratio are fundamental in the fine-tuning of signal transduction, including oxidative stress signaling needed for physiological events such as cell cycle regulation, and other cellular processes16. GPx is an important modulator of the balance between GSH and GSSG; therefore, its measurement provides a comprehensive view of the redox status along with the GSH:GSSG ratio.
Although oxidative stress in obese pediatric populations has been well demonstrated, there has been discordance in terms of redox biomarkers. Higher erythrocyte GPx activity and GSH levels were noted in children with obesity than in their NW counterparts, in contrast to increased oxidative stress indicators in obese children, such as oxidized low-density lipoprotein, malondialdehyde, and advanced oxidation products17,18,19,20,21. Thus far, the relationship between ID states and antioxidant enzymes, including GPx, has been inconsistent and controversial22,23. The studies report variation ranging from an increase in the antioxidant enzyme activity in IDA24 to a decrease23 or no effect25,26,27,28. The redox status of adolescents with obesity and anemia has not been investigated. Such studies would provide important evidence regarding the role of oxidative stress in the progression of metabolic dysregulation and the subsequent development of obesity and anemia-related comorbidities with their transition into young adulthood.
Kuwait has one of the highest rates of obesity in the adult and pediatric populations29. Childhood and adolescent obesity in Kuwait is particularly alarming, as up to 45% of children in the age group 5–19 years have either overweight or obesity30,31,32. Although anemia is not a major public health problem in Kuwait, it is still a public health issue in children and adolescents. The Kuwait Nutritional Surveillance System has consistently reported a 15–20% prevalence of anemia among school-age children32. A more recent study conducted on a nationally representative sample of adolescents reported the prevalence of anemia as 8.1% (11% in girls and 5% in boys)33. These reports provide preliminary support for the coexistence of both obesity and anemia in adolescents in Kuwait.
In this study, the prevalence of anemia in adolescents with overweight and obesity (OWOB) in Kuwait was assessed, and the relationship of erythrocyte GSH redox status (GSH, GSH:GSSG ratio, and GPx activity) with anemia and obesity was examined based on (a) measures of obesity in terms of body mass index (BMI) and waist circumference (WC) and (b) IDA status.
Results
Prevalence of obesity and anemia
The sociodemographic characteristics of the subjects (N = 524; 268 boys and 256 girls) are summarized in Table 1. The median (IQR) BMI percentile was 80.90 (48.93–95.88); 15.3% (10.8% boys, 19.9% girls; p = 0.006) of subjects were overweight, and 27.9% (26.9% boys, 28.9% girls) were classified as obese. When OWOB groups were combined, the total prevalence of excess adiposity was 43.1% in the overall sample (37.7% in boys and 48.8% in girls, p < 0.05). Based on the WC percentile obesogenic cutoff, 15.5% (17.9% boys and 12.9% girls; p = 0.073) were above the cutoff point.
The prevalence of anemia was 13% (8.2% in boys and 18% in girls; p = 0.001) (Table 2). The prevalence of anemia was 19.5% in subjects with OWOB and 8.1% in subjects with NW (p < 0.05). In boys, the prevalence of anemia in the OWOB group was 13.9% compared with 4.8% in the NW group (p < 0.05). In girls, the prevalence of anemia in the OWOB group was 24.0% compared with that of 12.2% in the NW group (p < 0.05). In the non-anemic overall sample, the prevalence of overweight was 39.9%, whereas it was 64.7% in anemic children (p < 0.05). A similar pattern was observed for boys and for girls separately. In boys, 59.3% were non-anemic and NW, 32.5% were non-anemic and OWOB, 3.0% were anemic and NW, and 5.2% were anemic and OWOB (Table 3). Among girls, 44.9% were non-anemic and NW, 37.1% were non-anemic and OWOB, 6.3% were anemic and NW, and 11.7% were anemic and OWOB. Significant interactions between boys and girls in terms of both weight and anemia statuses were observed. In the overall sample, the prevalence of anemia was 2.4 times higher in the OWOB group than in the NW group (p < 0.05). When stratified by sex, the prevalence of anemia in the OWOB group was 2.9 times higher in boys and 2.0-fold higher in girls than that in the NW group (p < 0.05 for both sexes). With regard to the weight status of anemic and non-anemic subjects, the prevalence of OWOB was 1.6-fold higher in anemic subjects than in non-anemic subjects (p < 0.05). When stratified by sex, the prevalence of OWOB in anemic subjects was higher by 1.8-fold in boys and by 1.4-fold in girls than that in non-anemic subjects (p < 0.05 for both sexes). The proportion of girls in the OWOB and anemic group was more than twice that of boys (Table 3).
Redox status in relation with sex, anemia, and adiposity
The erythrocyte concentrations of GSH, GSH:GSSG ratio, and GPx activity varied by sex, anemia status, and weight status, based on both BMI and WC categories (Table 4). GSH levels, in µmol/g Hb, (mean [standard deviation, SD]) were higher in girls than in boys (2.47 [0.67] vs. 1.69 [0.68], p < 0.001); in anemic subjects than in non-anemic subjects (2.60 [0.80] vs. 1.99 [0.74], p < 0.001); and higher in subjects with OWOB than in those with NW (2.31 [0.68] vs. 1.93 [0.80], p < 0.001). Similarly, the GSH:GSSG ratio was higher in girls than in boys (1.06 [0.48] vs. 1.00 [0.47], p < 0.001); in anemic subjects than in non-anemic subjects (1.10 [0.55] vs. 1.02 [0.46], p < 0.001); and in subjects with overweight/obesity than in those with NW (1.05 [0.44] vs. 1.01 [0.24], p < 0.001). The GPx activity, in U/g Hb, (median [IQR]) was higher in girls than in boys (95.16 [45.04–130.32] vs. 52.35 [39.53–104.20], p < 0.001); in anemic subjects than in non-anemic subjects (121.81 [92.86–154.60] vs. 57.83 [40.30–115.11], p < 0.001); and in subjects with OWOB than in those with NW (114.07 [62.46–137.69] vs. 48.11 [37.72–88.91], p < 0.001). Similarly, with WC percentile categories, those with ≥ 90th percentile had significantly higher levels of GSH:GSSG and GPx activity than those with < 90th percentile (GSH:GSSG, 1.08 [0.49] vs. 1.01 [0.48], p < 0.001; GPx, 98.32 [51.48–140.72] vs. 63.14 [41.32–118.44], p < 0.001), but the levels of GSH between the two waist categories were not different from each other.
Sex-wise comparisons between the combined anemia and weight categories
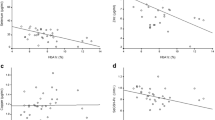
For the combined category of weight and anemia statuses in each sex (Fig. 1), anemic overweight boys, anemic NW boys, and non-anemic overweight boys had a significantly higher GSH:GSSG ratio than non-anemic NW boys (1.31 [1.06–1.70], 1.27 [0.89–2.23], and 1.19 [0.99–1.38] vs. 0.92 [0.84–1.10], respectively; p < 0.05). These observations were also similar in terms of GSH concentrations in µmol/g Hb, (Fig. 2; 2.36 [1.35–2.87], 2.45 [1.32–2.89], and 1.92 [1.56–2.24], vs. 1.40 [1.08–1.97], respectively; p < 0.05) and GPx activity, in U/g Hb, (Fig. 3; 108.58 [98.13–155.51], 104.24 [88.60–157.93], and 97.05 [46.72–121.11], vs. 46.25 [37.20–60.43], respectively; p < 0.05). Among girls, the differences in the median GSH:GSSG ratio were not significant among the four groups (Fig. 1; 1.35 [1.23–2.16], 1.04 [0.90–1.31], 1.11 [0.97–1.42], and 1.18 [0.94–1.37]). Anemic girls who were overweight had the highest level of GSH when compared with non-anemic overweight girls (2.79 [2.26–3.35] vs. 2.35 [1.99–2.75], p = 0.02) and non-anemic NW girls (2.79 [2.26–3.35] vs. 2.36 [2.03–2.77], p = 0.018; Fig. 2). Similarly, anemic overweight girls had the highest level of GPx activity when compared to non-anemic overweight girls (130.21 [113.13–164.19] vs. 111.49 [68.38–135.03], p = 0.036), anemic NW girls (130.21 [113.13–164.19] vs. 96.45 [40.18–133.79], p = 0.03), and non-anemic NW girls (130.21 [113.13–164.19] vs. 55.39 [39.10–144.26], p < 0.001) (Fig. 3).
Association of redox status with anemia and obesity in adolescents
The Spearman’s correlation analysis (Table 5) showed that GSH:GSSG ratio, GSH, and GPx activity were positively associated with anemic status (ρ = 0.181, p < 0.001; ρ = 0.251, p < 0.001; and ρ = 0.215, p < 0.001, respectively). Similarly, GSH:GSSG ratio, GSH, and GPx activity were negatively associated with Hb concentration (ρ = − 0.224, p < 0.001; ρ = − 0.301, p < 0.001; and ρ = − 0.149, p < 0.001, respectively). In terms of measures of adiposity, the GSH:GSSG ratio was positively correlated with BMI (ρ = 0.255, p < 0.001), WC (ρ = 0.317, p < 0.001), and WC:Ht (ρ = 0.333, p < 0.001). GSH and GPx activity also showed similar associations (Table 5). Sex was also positively correlated with GSH:GSSG ratio, GSH, and GPx activity, whereas age was significantly negatively correlated only with GSH: GSSG (ρ = − 0.111, p < 0.05). In multinomial logistic regression (Table 6), the GSH:GSSG ratio was positively associated with anemia status after adjusting for age, sex, and BMI categories, regardless of whether it was used as a continuous variable (adjusted odds ratio, adjOR [95% CI], 2.18 [1.44–3.29]; p < 0.001, R2 = 0.138) or as tertiles (adjOR [95% CI], T3 = 2.49 [1.03–6.01], T2 = 1.54 [0.67–3.56]; p < 0.001, R2 = 0.104). A similar association was observed for GSH (R2 = 0.154 as continuous and R2 = 0.126 as tertiles) and GPx (R2 = 0.179 as continuous and R2 = 0.139 as tertiles). When increased adiposity, as BMI categories, was examined in the multinomial logistic regression model adjusted for age, sex, and anemia status; GSH:GSSG ratio, GSH, and GPx activity remained significantly positively associated with similar magnitudes (Table 7).
Discussion
In the present study, erythrocyte GPx activity, GSH concentrations, and GSH:GSSG ratio were higher in adolescents with an OWOB status than in NW adolescents. Another novel finding was that the three redox erythrocyte parameters were also positively associated with anemia, even after adjusting for known covariates including sex, age, and obesity. In this regard, a significantly negative association was observed between Hb and redox status, including GSH and GPx activity. Of the three redox parameters studied, GPx activity showed the highest percent change in association with weight status and anemia. In the context of both obesity and anemia, it is possible that the observed increase in GPx antioxidant activity and the redox status was due to an appropriate adaptive response to the chronic oxidative stress that, as suggested previously, occurs in diabetic patients and smokers34. Although GPx provides protection against oxidative stress and modulates redox-mediated cellular signaling, excessive GPx activity exerts deleterious effects due to the reduction in essential cellular oxidants and the subsequent reductive stress35. Lack of essential cellular oxidants diminishes cell growth and dysregulates mitochondrial function and cellular metabolism. Excess GPx and reducing equivalents (GSH) have been linked to cardiomyopathy, cardiac dysfunction, and development of insulin resistance, a common feature of type 2 diabetes and metabolic syndrome35.
Although previous studies have not examined redox status in the adolescent obese population, Rowicka et al.36 and Kilic et al.37 reported a significantly higher total antioxidant capacity in children with obesity than in NW controls. Higher total oxidant capacity or oxidative stress index levels together with an elevated total antioxidant capacity were reported in children. Abuali18 reported increased activities of antioxidant enzymes (superoxide dismutase, GR, and GPx) in overweight children (mean age 9.7 ± 1.5 years); however, contrary to the findings of the present study, the above enzymatic parameters were decreased in the obese group in the previous study. A decrease in the GPx activity in obese children has been attributed to a depletion in the level of erythrocyte GSH, which is a cofactor for GPx38,39. The apparent contradictory results for obese adolescents described in the present work could indicate that the GSH status, particularly GPx, depends on the degree of adiposity and/or age of the subjects. Duration of adiposity, metabolic health status, degree of disease development and/or severity, and sex may also contribute to variations in the antioxidant status in response to obesity19,40. Further support for this notion comes from studies in which obese children with insulin resistance showed an impaired systemic oxidative status in contrast to obese children without insulin resistance or healthy controls. In these studies, obese children without insulin resistance, despite a transient decrease in GSH levels during the glucose tolerance test, were able to recover and maintain normal levels of lipid peroxides, similar to control subjects41. The ability of the antioxidant system to respond to an acute stressor in obese children without insulin resistance may be mediated through a more beneficial oxidative stress profile, with higher levels of principal antioxidants (GSH) together with lower levels of lipid peroxidation, possibly through shared anti-inflammatory pathways8,42.
The findings of the present study are consistent with those of some studies with regard to the redox status in anemia24,43, which indicates an increased activity of antioxidant defense enzymes in red blood cells during anemia. This can be an adaptive mechanism during the oxidative stress context of anemia, whereby sustained increased levels of erythrocyte H2O2 induce GPx and other antioxidant enzymes24,43, resulting in an increased redox status. However, considerable variations exist in human studies with regard to ID and redox status44, which can be attributed to the study differences in sample size, age of subjects, distribution of males and females in the sample, and severity of ID. For example, Altun et al.24 found no increase in GPx activity in groups of infants with IDA when compared with aged-matched controls. It was suggested that this discrepancy was due to the immaturity of the antioxidant capacity of infants, where it could not generate an adequate response to stress with GPx activity increase24.
In terms of sex-specific changes, while the values of the redox status (erythrocyte GSH concentrations, GPx activity, and the GSH:GSSG ratio) were higher in girls, the percent change associated with overweight and anemia was higher in boys. This discord was particularly evident when comparing the NW and overweight groups in the non-anemic category. This observation can be explained by the disproportionately higher percentage of girls in the anemic overweight groups than that of boys. GSH metabolism and GSH-dependent responses in humans appear to be regulated by both sex hormones, progesterone and testosterone45. In premenopausal women, the activity of erythrocyte GPx was found to be higher than that in healthy postmenopausal women. Furthermore, GPx activity in premenopausal women was significantly higher than that in age-matched men, but it was not significantly different between postmenopausal women and age-matched men46. Such findings suggest that there is a sex-dependent intensification of the antioxidant response, with girls being more resistant to the negative effects of an increased adiposity status than boys47.
OWOB in adolescents in Kuwait is a public health issue, and our result of > 40% of adolescents with OWOB is consistent with that of previous reports48,49. Kuwait and countries in the Arabian Gulf region have experienced a rapid transition from a traditional semi-urbanized life to a modern and urbanized society after the economic boom post the discoveries of oil since the 1960s. There has been a concomitant rise in the prevalence of obesity and other cardio-metabolic problems50. Adolescence is a critical period for the development and expression of obesity-related comorbidities in both sexes51. The prevalence of anemia in adolescents in the present study is in line with that mentioned in previous reports showing that anemia in adolescents is of mild public health significance, particularly in girls, as per the WHO classification (5.0–19.9%)33,52. There was, however, a disproportionately high prevalence of anemia in those with OWOB, which shows a clear coexistence of anemia and OWOB in this adolescent cohort. Similar to these findings, the coexistence of anemia and OWOB had been reported in many countries undergoing nutrition transition53,54,55. The combination of both anemia and obesity may affect adolescent growth and development, leading to psychological disorders, cognitive dysfunction, impaired motor abilities, altered timing of puberty, and multiple risk of comorbidities such as the metabolic syndrome and type 2 diabetes55,56.
The coexistence of both anemia and obesity was particularly high in girls, as the proportion of girls who were both overweight and anemic was more than twice that of boys. Increased iron loss in the menstrual blood and inadequate dietary iron intake have been suggested to contribute to a higher prevalence of anemia in girls33,48. The higher prevalence of both anemia and OWOB in adolescent girls, compared with that in boys, could be explainable by the higher consumption of energy-dense foods (sweets, cakes and donuts, burgers, French fries, and hot dogs), lower consumption of fruits and vegetables48,49,57,58, lower consumption of iron rich foods such as animal protein59, and lack of physical activity48. Therefore, adolescents with obesity may be at a higher risk of ID because of unbalanced meals, which are high in calories but low in iron, whether absolute or relative to body mass, together with increased iron needs.
To the best of our knowledge, this is the first study on the relationship between anemia and the redox status and GPx activity in a large sample of healthy adolescents. This study is among the few that put forward the concept of metabolic flexibility in overweight and obese adolescents and in relation to anemia through an increased antioxidant status as measured by the redox status and GPx activity. Most previous studies have been performed in infants, children, or adults and used biomarkers of lipid peroxidation or other biomarkers that are largely modulated by unknown factors. The present study had a powered sample size for the analyses and included both sexes equally. Another strength of this study is that it was based on a narrow age range, thus minimizing age-dependent variations. There are, however, a few limitations in this study. For example, not including inflammatory markers such as IL-1, IL-6, or C-reactive protein (CRP), markers of metabolic risk such as C-peptides or insulin resistance index, and oxidative stress markers such as plasma isoprostanes limited the interpretation of our findings to support the antioxidant compensation hypothesis, in particular in subjects with OWOB. In addition, the narrow age range of the study subjects that was included as a strength to minimize age-related variation limits the extrapolation of the results to other age groups such as children and adults. Furthermore, it has been reported that approximately 5–15% of the GSH could be oxidized to GSSG during sample deproteination with acids60. This could potentially result in the overestimation of GSSG and thus lower GSH:GSSG values. Derivatization of the GSH with N-ethylmaleimide has been suggested to overcome this analytical anomaly. However, this GSH-N-ethylmaleimide derivatization logistically was not possible for us as it is required during the sample collection, and we used sedimented erythrocytes provided to us from another study. The statistically significant increase in the GSH:GSSG ratio in cases vs controls, despite this apparent artifact if it has happened, suggests that the changes in the glutathione redox status are robust and could be detected despite this experimental anomaly. Finally, the cross-sectional nature of the study limits the interpretation of the findings to only correlations.
Conclusions
In conclusion, adolescents with anemia and obesity with no other metabolic disturbances were shown to have increased erythrocyte GSH concentrations, GSH:GSSG ratio, and GPx activity. The increased glutathione redox status could be a compensatory mechanism in response to the increased oxidative burden due to anemia and obesity. Further studies are warranted to investigate the basis for the relationship between these redox parameters and other biomarkers of oxidative stress, and to investigate the mechanisms underlying the association of anemia and excessive adiposity with alterations in the redox status in adolescence. The effects, if any, of dietary modifications on the three redox measures need further investigation. The assessment of the redox status in relation to the progression of obesity-related comorbidities such as metabolic syndrome, diabetes, and cardiovascular disease (CVD) in cohort studies on adolescents could have important public health relevance.
Methods
Study design and participants
This present study was nested within a cross-sectional study conducted in public middle schools in Kuwait, as previously described61,62. In the original study, data were collected from 1426 children (701 boys) in the age range of 11–16 years, randomly selected from all the six Governorates of Kuwait, utilizing multi-stage random cluster sampling methods with a probability proportional to the size of each governorate. All students of public schools, both boys and girls, in grades 6, 7, and 8 (age range 11–14 years) were eligible for inclusion in the study. Children who had any systemic diseases (diabetes, cardiovascular, liver, or kidney diseases) or those who were on any medication for behavioral or psychological problems were excluded from the study. Data were collected from parents through a self-administered questionnaire and from study subjects through a face-to-face interview by trained data collectors. For this study, a nested case–control design was employed in which patients were selected based on their overweight/obesity status and control subjects were age- and sex-matched subjects, both recruited at a ratio of 1:1.6. The sample size was calculated based on the obesity prevalence of 20% in Kuwaiti adolescents for a case–control study, to detect a similar odds ratio with 90% statistical power and a 5% margin of error. The calculated sample size was 181 subjects per group. The final sample of 524 subjects included 291 with NW and 226 with overweight/obesity. Ethical approval was granted by the Ethics Committee of the Health Sciences Centre, Kuwait University (No. DR/EC/2338), and the Ethics Committee of the Ministry of Health, Kuwait (No. 2015/248 and No. 2017/1025 for additional tests). Written informed consent was obtained from the subjects’ parents, and verbal assent was obtained from all the study subjects before drawing blood. The study was conducted according to the ethical standards set by the Helsinki Declaration.
Anthropometric measurements
Standing height (Ht) and body weight of the study subjects were measured in a standardized manner, using a digital weight and Ht scale (Detecto, Webb City, MO, USA) with the subjects standing erect without shoes and wearing light clothes. BMI-for-age z-scores (zBMI) were calculated using the World Health Organization (WHO) growth charts. A zBMI of ≥ + 3 SD was classified as obesity, while zBMIs of > + 2 SD and < + 3 SD were defined as overweight. Subjects with a zBMI of < + 2 SD were classified as NW. We originally categorized zBMI into four levels: underweight, NW, overweight, and obese. We then found that < 1% of the subjects were underweight. Due to the small number of adolescents in this latter category, the underweight and NW categories were combined. WC was measured in the horizontal plane at the superior border of the right iliac crest to the nearest 0.1 cm with a non-stretchable tape by a trained data collector. Measurements were taken at the end of normal expiration; three readings were taken, and the average of the three was recorded. Care was taken to ensure that the tape was horizontal to the floor and touched the skin without compressing it. Population-based age- and sex-specific percentile cutoffs63 were used to categorize adolescent obesogenic waist (in cm) for boys aged 12, 13, and 14 years old and for girls 12, 13, and 14 years old. The WC cutoffs for boys were ≥ 91.5, ≥ 95.3, and ≥ 98.5, while the WC cutoffs for girls were ≥ 91.3, ≥ 95.2, and ≥ 98.5, respectively.
Blood collection and biochemical analyses
Five milliliters of blood sample were collected by venipuncture by a trained nurse. One tube (EDTA-containing) was centrifuged at 16,000 × g for 10 min; plasma and buffy coats were separated, and the sedimented erythrocytes (1 mL) were collected in Eppendorf tubes and stored at − 80 °C for the redox status analysis. Classification of anemia was made according to hemoglobin (Hb) levels as described earlier33. Anemia was defined as Hb < 115 g/L in boys and girls aged younger than 12 years; Hb < 120 g/L in the 12–14 years age group; Hb < 130 g/L in boys aged 15 years or older; and Hb < 120 g/L in girls aged 15 years or older64.
Determination of erythrocyte glutathione redox status
The erythrocyte GSH redox status was measured using the commercial GSH assay kit (Cat. #: 703002; Cayman Chemical, Ann Arbor, MI, USA) according to the manufacturer’s instructions. This kit utilizes GSH reductase for the quantification of GSH. Briefly, the erythrocyte samples stored at − 80 °C were thawed and lysed in four volumes of ice-cold high-performance liquid chromatography (HPLC)-grade water; samples were then deproteinized by adding an equal volume of metaphosphoric acid (5%) on ice for 10 min. The suspension was centrifuged at 16,000 × g for 10 min at 4 °C. The supernatant was collected and stored on ice, when used immediately, or frozen at − 80 °C for future use. The contents of total GSH (TGSH) and GSSG in the erythrocytes were determined; additionally, the level of reduced GSH (the difference between TGSH and GSSG) and the GSH:GSSG ratio were calculated.
Assessment of erythrocyte GPx activity
GPx activity was determined using a kit assay (Cat. #: K762-100; BioVision, Milpitas, CA) as per the manufacturer’s instructions. In this assay, GPx reduced cumene hydroperoxide while oxidizing GSH to GSSG. The generated GSSG was then reduced to GSH with the consumption of NADPH by GR. The decrease in NADPH, which was measured colorimetrically at 340 nm, was proportional to GPx activity. The assay had a detection sensitivity of ~ 0.5 mU/mL of GPx in the samples.
Statistical analysis
Data were coded, entered into, and analyzed using the Statistical Package for the Social Sciences (SPSS) for Windows version 24 (IBM Corp., Armonk, N.Y., USA). GSH was normally distributed, whereas GPx and the GSH:GSSG ratio were not normally distributed. GPx activity had a more bimodal distribution and could not be normalized with the usual transformation. The GSH:GSSG ratio was normalized by taking the square root of the variable. For normally distributed variables, data are presented as mean (SD), whereas for non-normally distributed variables, descriptive data are reported as the median and interquartile range (IQR). Significant group differences in the GPx activity were assessed using the chi-square test and the independent-samples median test, whereas for GSH and the GSH:GSSG ratio, the t-test for independent samples and analysis of variance (ANOVA) were used. The Spearman’s correlation coefficients (ρ) were calculated to determine the correlation between GSH, GSH:GSSG ratio, and GPx activity, with each of these variables treated separately as the dependent variable and WC, BMI, and Hb as the independent variables. Hb was used as a continuous variable, whereas the other variables were used as categorical ones. The association of GSH, GSH:GSSG ratio, and GPx activity with obesity or anemia was evaluated using multinomial logistic regression. The odds ratios were adjusted for age, sex, and anemia status (or obesity status). Anemia, BMI, and WC were used as binary categorical variables. The WC/Ht ratio was used as both a continuous variable and as tertiles. The analyses were conducted by fitting GSH, GSH:GSSG ratio, and GPX as continuous variables as well as categorizing them into tertiles. The level of significance was set at p < 0.05.
Data availability
Data are available from the corresponding author upon reasonable request.
References
Pinhas-Hamiel, O. et al. Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int. J. Obes. 27, 416–418 (2003).
Manios, Y. et al. The double burden of obesity and iron deficiency on children and adolescents in Greece: The healthy growth study. J. Hum. Nutr. Diet 26, 470–478 (2013).
Yanoff, L. B. et al. Inflammation and iron deficiency in the hypoferremia of obesity. Int. J. Obes. 31, 1412–1419 (2007).
Haidari, F., Abiri, B., Haghighizadeh, M. H., Kayedani, G. A. & Birgani, N. K. Association of hematological parameters with obesity-induced inflammation among young females in Ahvaz, South-West of Iran. Int. J. Prev. Med. 11, 55. https://doi.org/10.4103/ijpvm.IJPVM_35_18 (2020).
Kern, L. et al. Obesity-induced TNFα and IL-6 signaling: The missing link between obesity and inflammation—Driven liver and colorectal cancers. Cancers 11, 4. https://doi.org/10.3390/cancers11010024 (2018).
Xiao, X., Yeoh, B. S. & Vijay-Kumar, M. Lipocalin 2: An emerging player in iron homeostasis and inflammation. Annu. Rev. Nutr. 37, 103–130 (2017).
Hubler, M. J., Peterson, K. R. & Hasty, A. H. Iron homeostasis: A new job for macrophages in adipose tissue?. Trends Endocrinol. Metab. 26, 101–109 (2015).
Wessling-Resnick, M. Iron homeostasis and the inflammatory response. Annu. Rev. Nutr. 30, 105–122 (2010).
Furukawa, S. et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Invest. 114, 1752–1761 (2004).
Kamigaki, M. et al. Oxidative stress provokes atherogenic changes in adipokine gene expression in 3T3-L1 adipocytes. Biochem. Biophys. Res. Commun. 339, 624–632 (2006).
Horvath, T. L., Andrews, Z. B. & Diano, S. Fuel utilization by hypothalamic neurons: Roles for ROS. Trends Endocrinol. Metab. 20, 78–87 (2009).
Circu, M. L. & Aw, T. Y. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic. Biol. Med. 48, 749–762 (2010).
Vacchi-Suzzi, C. et al. Low levels of lead and glutathione markers of redox status in human blood. Environ. Geochem. Health 40, 1175–1185 (2018).
Flora, G., Gupta, D. & Tiwari, A. Toxicity of lead: A review with recent updates. Interdiscip. Toxicol. 5, 47–58 (2012).
Gilbert, H. F. Catalysis of thiol/disulfide exchange: Single-turnover reduction of protein disulfide-isomerase by glutathione and catalysis of peptide disulfide reduction. Biochemistry 28, 7298–7305 (1989).
Aquilano, K., Baldelli, S. & Ciriolo, M. R. Glutathione: New roles in redox signaling for an old antioxidant. Front. Pharmacol. https://doi.org/10.3389/fphar.2014.00196 (2014).
Al-Dalaeen, A. M. & Al-Domi, H. A. Evaluation of oxidant-antioxidant status in obese children and adolescents. Pakistan J. Nutr. 15, 942–947 (2016).
Albuali, W. H. Evaluation of oxidant-antioxidant status in overweight and morbidly obese Saudi children. World J. Clin. Pediatr. 3, 6. https://doi.org/10.5409/wjcp.v3.i1.6 (2014).
Atabek, M. E., Vatansev, H. & Erkul, I. Oxidative stress in childhood obesity. J. Pediatr. Endocrinol. Metab. https://doi.org/10.1515/JPEM.2004.17.8.1063 (2004).
Lima, S. C., Arrais, R. F., Almeida, M. G., Souza, Z. M. & Pedrosa, L. F. Plasma lipid profile and lipid peroxidation in overweight or obese children and adolescents. J. Pediatr. 80, 23–28 (2004).
Mohn, A. et al. Increased oxidative stress in prepubertal severely obese children: Effect of a dietary restriction-weight loss program. J. Clin. Endocrinol. Metab. 90, 2653–2658 (2005).
Guo, W., Zhou, Q., Jia, Y. & Xu, J. Increased levels of glycated hemoglobin a1c and iron deficiency anemia: A review. Med. Sci. Monit. 25, 8371–8378 (2019).
Zaka-ur-Rab, Z. Effect of oral iron on markers of oxidative stress and antioxidant status in children with iron deficiency anaemia. J. Clin. Diagn. Res. 10, SC13. https://doi.org/10.7860/JCDR/2016/23601.8761 (2016).
Altun, D. et al. Malondialdehyde, antioxidant enzymes, and renal tubular functions in children with iron deficiency or iron-deficiency anemia. Biol. Trace Elem. Res. 161, 48–56 (2014).
Tekin, D., Yavuzer, S., Tekin, M., Akar, N. & Cin, S. Possible effects of antioxidant status on increased platelet aggregation in childhood iron-deficiency anemia. Pediatr. Int. 43, 74–77 (2001).
El-Shimi, M. S. et al. Renal functional and structural integrity in infants with iron deficiency anemia: Relation to oxidative stress and response to iron therapy. Pediatr. Nephrol. 30, 1835–1842 (2015).
Akarsu, S., Demır, H., Selek, S. & Oguzoncul, F. Iron deficiency anemia and levels of oxidative stress induced by treatment modality: Iron deficiency anemia and oxidative stress. Pediatr. Int. 55, 289–295 (2013).
Aycicek, A. et al. Ferrous sulfate (fe2+) had a faster effect than did ferric polymaltose (fe3+) on increased oxidant status in children with iron-deficiency anemia. J. Pediatr. Hematol. Oncol. 36, 57–61 (2014).
Al-Refaee, F. A. et al. The rising tide of overweight among Kuwaiti children: Study from Al-Adan hospital, Kuwait. Med. Princ. Pract. 22, 600–602 (2013).
Al Hammadi, H. & Reilly, J. Prevalence of obesity among school-age children and adolescents in the Gulf Cooperation Council (GCC) states: A systematic review. BMC Obes. 6, 3. https://doi.org/10.1186/s40608-018-0221-5 (2019).
Alrashidi, M., Shahwan-Akl, L., James, J. & Jones, L. Contributing factors to childhood overweight and obesity in Kuwait. Int. J. Health Sci. 3, 133–155 (2015).
Food and Nutrition Department. The Kuwait nutrition surveillance system—Annual report 2018 (accessed 15 August 2019). Ministry of Health. https://www.moh.gov.kw/en/FoodNutrition/Pages/FND.aspx (2019).
Shaban, L., Al-Taiar, A., Rahman, A., Al-Sabah, R. & Mojiminiyi, O. Anemia and its associated factors among adolescents in Kuwait. Sci. Rep. 10, 5857. https://doi.org/10.1038/s41598-020-60816-7 (2020).
Savini, I., Catani, M., Evangelista, D., Gasperi, V. & Avigliano, L. Obesity-associated oxidative stress: Strategies finalized to improve redox state. Int. J. Mol. Sci. 14, 10497–10538 (2013).
Lubos, E., Loscalzo, J. & Handy, D. E. Glutathione peroxidase-1 in health and disease: From molecular mechanisms to therapeutic opportunities. Antioxid. Redox Signal 15, 1957–1997 (2011).
Grażyna, R. et al. Total oxidant and antioxidant status in prepubertal children with obesity. Oxid. Med. Cell Longev. 2017, 5621989. https://doi.org/10.1155/2017/5621989 (2017).
Kilic, E. et al. Oxidative stress status in childhood obesity: A potential risk predictor. Med. Sci. Monit. 22, 3673–3679 (2016).
Ozata, M. et al. Increased oxidative stress and hypozincemia in male obesity. Clin. Biochem. 35, 627–631 (2002).
Dinçer, Y., Alademir, Z., İlkova, H. & Akçay, T. Susceptibility of glutatione and glutathione-related antioxidant activity to hydrogen peroxide in patients with type 2 diabetes: Effect of glycemic control. Clin. Biochem. 35, 297–301 (2002).
Brown, L. A. et al. Oxidant stress in healthy normal-weight, overweight, and obese individuals. Obesity 17, 460–466 (2009).
Lechuga-Sancho, A. M. et al. Obesity induced alterations in redox homeostasis and oxidative stress are present from an early age. Edited by Manuel Portero-Otin. PLoS ONE 13, e0191547. https://doi.org/10.1371/journal.pone.0191547 (2018).
Gustafsson, S. et al. Oxidative stress and inflammatory markers in relation to circulating levels of adiponectin: Adiponectin, oxidative stress, and inflammation. Obesity 21, 1467–1473 (2013).
İnal, M. E., Güngör, K. & Emine, S. Antioxidant enzyme activities and malondialdehyde levels related to aging. Clin. Chim. Acta 305, 75–80 (2001).
Usman, S. S. et al. Status of malondialdehyde, catalase and superoxide dismutase levels/activities in schoolchildren with iron deficiency and iron-deficiency anemia of kashere and its environs in Gombe State, Nigeria. Heliyon 5, e02214. https://doi.org/10.1016/j.heliyon.2019.e02214 (2019).
Wang, L., Ahn, Y. J. & Asmis, R. Sexual dimorphism in glutathione metabolism and glutathione-dependent responses. Redox Biol. 31, 101410. https://doi.org/10.1016/j.redox.2019.101410 (2020).
Massafra, C. et al. Gender-related differences in erythrocyte glutathione peroxidase activity in healthy subjects: Glutathione peroxidase in men and women. Clin. Endocrinol. 57, 663–667 (2002).
Sobieska, M., Gajewska, E., Kalmus, G. & Samborski, W. Obesity, physical fitness, and inflammatory markers in Polish children. Med. Sci. Monit. 19, 493–500 (2013).
Allafi, A. et al. Physical activity, sedentary behaviours and dietary habits among Kuwaiti adolescents: Gender differences. Public Health Nutr. 17, 2045–2052 (2014).
Badr, H. E., Lakha, S. F. & Pennefather, P. Differences in physical activity, eating habits and risk of obesity among Kuwaiti adolescent boys and girls: A population-based study. Int. J. Adolesc. Med. Health https://doi.org/10.1515/ijamh-2016-0138 (2019).
Ng, S. W., Zaghloul, S., Ali, H. I., Harrison, H. G. & Popkin, B. M. The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf states. Obes. Rev. 12, 1–13 (2011).
Daniels, S. R. et al. Overweight in children and adolescents: Pathophysiology, consequences, prevention, and treatment. Circulation 111, 1999–2012 (2005).
Al Zenki, S. et al. Prevalence and determinants of anemia and iron deficiency in Kuwait. Int. J. Environ. Res. Public Health 12, 9036–9045 (2015).
Eckhardt, C. L., Torheim, L. E., Monterrubio, E., Barquera, S. & Ruel, M. T. The overlap of overweight and anaemia among women in three countries undergoing the nutrition transition. Eur. J. Clin. Nutr. 62, 238–246 (2008).
Ornelas, P. T., Salazar, J. J. E. & Martínez-Salgado, H. Coexistence of obesity and anemia in children between 2 and 18 years of age in Mexico. Bol. Med. Hosp. Infant Mex. 68, 431–437 (2011).
Zhou, S. et al. Double burden of malnutrition: Examining the growth profile and coexistence of undernutrition, overweight, and obesity among school-aged children and adolescents in urban and rural counties in Henan province, China. J. Obes. 2020, 1–11 (2020).
Gregory, J. W. Prevention of obesity and metabolic syndrome in children. Front. Endocrinol. 10, 669. https://doi.org/10.3389/fendo.2019.00669 (2019).
Shaban, L. & Alkazemi, D. Trends in fast-food consumption among Kuwaiti youth. Int. J. Prev. Med. 10, 44. https://doi.org/10.4103/ijpvm.IJPVM_480_18 (2019).
Fraser, L. K. & Edwards, K. L. The association between the geography of fast food outlets and childhood obesity rates in Leeds, UK. Health Place 16, 1124–1128 (2010).
Alkazemi, D. Gender differences in weight status, dietary habits, and health attitudes among college students in Kuwait: A cross-sectional study. J. Nutr. Health 25, 75–84 (2019).
Giustarini, D., Dalle-Donne, I., Milzani, A., Fanti, P. & Rossi, R. Analysis of GSH and GSSG after derivatization with N-ethylmaleimide. Nat. Protoc. 8, 1660–1669 (2013).
Al-Taiar, A., Rahman, A., Al-Sabah, R., Shaban, L. & Al-Harbi, A. Vitamin D status among adolescents in Kuwait: A cross-sectional study. BMJ Open 8, e021401. https://doi.org/10.1136/bmjopen-2017-021401 (2018).
Rahman, A. et al. Plasma 25-hydroxy vitamin d is not associated with either cognitive function or academic performance in adolescents. Nutrients 10, 1197. https://doi.org/10.3390/nu10091197 (2018).
Jackson, R. T., Al Hamad, N., Prakash, P. & Al Somaie, M. Waist circumference percentiles for Kuwaiti children and adolescents. Public Health Nutr. 14, 70–76 (2011).
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System (accessed 20 August 2019). https://www.who.int/vmnis/indicators/haemoglobin/en/ (2011).
Acknowledgements
We acknowledge the contribution of Drs Abdullah Al-Tairar, Reem Al-Sabah, and Lemia Shaban in data collection in the original project (WF02/13). We would like to thank Dr. Stan Kubow for reviewing this manuscript and for providing endless support. We also thank Dasman Diabetes Institute for providing training, supervising the laboratory work, and generating data of the biomarkers of redox status. This work was supported and funded by Kuwait University Research Project No. YF01/18. The sponsors had no role in the design, execution, interpretation, or writing of the study.
Author information
Authors and Affiliations
Contributions
D.A. and A.R. conceived and designed the study; B.H. performed laboratory work for biomarkers of the redox status; A.R. is the principal investigator (PI) of the original study and provided data of weight status, WC, anemia status, and sociodemographic aspects; D.A. and B.H. coordinated data collection and entry; D.A. performed the statistical analysis; D.A. and A.R. wrote the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alkazemi, D., Rahman, A. & Habra, B. Alterations in glutathione redox homeostasis among adolescents with obesity and anemia. Sci Rep 11, 3034 (2021). https://doi.org/10.1038/s41598-021-82579-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-82579-5
- Springer Nature Limited
This article is cited by
-
Sex-specific interactions between stress axis and redox balance are associated with internalizing symptoms and brain white matter microstructure in adolescents
Translational Psychiatry (2024)
-
Air pollution, cardiorespiratory fitness and biomarkers of oxidative status and inflammation in the 4HAIE study
Scientific Reports (2024)
-
Dietary Supplemented Pomegranate Peel Ethanolic Extract Improves Growth, IGF-1 Expression and Immune Responses in Labeo Rohita Fingerlings Reared in Varying Stocking Densities
Waste and Biomass Valorization (2024)
-
Evolution of oxidative stress markers in livers of ducks during force-feeding
Scientific Reports (2023)
-
Principles and functions of metabolic compartmentalization
Nature Metabolism (2022)