Abstract
Multiple sclerosis (MS) is a major demyelinating disease of the central nervous system; however, its exact mechanism is unknown. This study aimed to elucidate the profile of white blood cells (WBCs) in the acute phase of an MS attack. Sixty-four patients with MS at the time of diagnosis and 2492 age- and sex-adjusted healthy controls (HCs) were enrolled. Data regarding the blood cell counts were compared between the groups. The total WBC (p < 0.0001), monocyte (p < 0.0001), basophil (p = 0.0027), and neutrophil (p < 0.0001) counts were higher in the MS group than in the HC group, whereas the lymphocyte and eosinophil counts did not differ. Adjustments for the smoking status and body mass index yielded the same results. The total and differential WBC counts of the patients with MS did not correlate with the counts of T2 hyperintense brain lesions or the levels of neurological disturbance. In summary, patients with MS showed elevated counts of total WBCs, monocytes, basophils, and neutrophils at the time of diagnosis. However, the clinical relevance of these biomarkers in the context of the development and progression of MS remains unclear.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is an inflammatory neurological disease characterized by demyelinating lesions of the central nervous system (CNS) and typically presenting with recurrent neurological episodes, with or without the indolent progression of neurological disturbances between relapses1,2,3. Although the disease is believed to be an autoimmune-related neurological disorder, the exact mechanisms, which are thought to be multifactorial, have not yet been fully elucidated. Furthermore, the white blood cell (WBC) profiles in MS, as opposed to those in healthy controls (HCs), have not yet been largely examined. The WBC differential count is a popular biomarker for evaluating the presence of systemic inflammations4. Several previous studies have reported that patients with MS may show slightly elevated levels of neutrophil-to-lymphocyte ratios (NLR) in the peripheral blood compared to HCs, which may reflect the disease activity and prognosis4,5,6,7. This fact suggested that the innate immune system, rather than the adaptive immune system, might be activated in patients with MS8,9. The WBC differential count is an inexpensive and easily accessible biomarker, and hence can help in the diagnosis and treatment of the patients with MS. This study aimed to confirm the activation of the innate immune system in MS by enrolling a large number of HCs, and further attempted to determine the influence of differential WBC counts on the clinical manifestation of the disease.
Methods
Study design
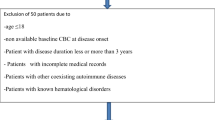
This study was a single-center retrospective case–control study. All consecutive patients who were diagnosed with MS as per the previous or latest diagnostic criteria3,10, and had hemogram data at the time of diagnosis before starting acute or chronic treatment (i.e., disease-modifying drugs) were enrolled. All enrolled patients were reconfirmed to meet the latest version of the McDonald diagnostic criteria as revised in 20173. All enrolled patients with MS were treated at Tohoku University Hospital. Patients whose conditions remained as clinically isolated syndromes or radiologically isolated syndromes and did not progress to MS by March 2021 were not recruited. A sufficiently large number of HCs in their 20s, 30s, and 40s, with no significant medical history, were also enrolled to compare the hemogram data. The profile of HCs has previously been reported11,12. Patients with MS whose hemogram data at the diagnosis were achieved before April 2013, when the automated hematology analyzer was changed to XN-Series at the hospital, were not enrolled for this study to avoid biases based on the measurement with different analyzers.
Evaluated Variables
The background and hemogram data of the evaluated participants were collected, and all the blood samples were collected and evaluated at a single university in Japan. Blood samples from patients with MS were collected at the time of diagnosis before they underwent acute treatment with intravenous methylprednisolone pulse therapy, or relapse prevention treatment. Age and sex data were evaluated to attain background information. Data regarding the current smoking status, previous smoking status, and body mass index (BMI) were also collected, as the current smoking status and obesity are known to affect the total and differential WBC counts.
Hemograms of all the participant samples were generated automatically using XN-Series systems (Sysmex, Kobe, Japan). The total WBC, red blood cell (RBC), and platelet counts in the peripheral blood were collected for both the groups (HC and MS). Furthermore, the differential counts of monocytes, lymphocytes, eosinophils, basophils, and neutrophils were determined, and the NLR, platelet-to-lymphocyte ratio (PLR), and monocyte-to-lymphocyte ratio (MLR) were derived from each component.
In addition to the blood cell count data, other blood test data, cerebrospinal fluid (CSF) analysis data, and clinical variables regarding disease activity and clinical severity were collected from the MS group. Additional blood test data included the serum C-reactive protein (CRP) level, anti-nuclear antibody (ANA; ≥ 1:160) positivity, presence of hepatitis B surface antigen (HBsAg), presence of antibodies against hepatitis C virus (HCV), and the results of Treponema pallidum hemagglutination (TPHA) testing for syphilis screening. The CSF analysis data included the total cell count (CSF-CC), presence of CSF-restricted oligoclonal bands (OCB), immunoglobulin-G index (IgG-index), CSF/serum ratios of albumin (QAlb), and CSF/serum ratios of IgG (QIgG). The outcome variables included the count of T2 hyperintense demyelinating lesions on brain MRI, regardless of the contrast enhancement at the time of hemogram, and the scores of the Kurtzke’s Expanded Disability Status Scale (EDSS) during the remission phase 1 year after the hemogram.
Statistical Analysis
Distributions of quantitative variables were described as the median and interquartile range (IQR, 25–75 percentiles). The Mann–Whitney U test was used to compare the quantitative variables between the two independent groups. As the total and differential WBC counts are known to be largely affected by the current smoking status and BMI, the analysis of covariance (ANCOVA) for each of the WBC differentials were performed by using the BMI and average number of cigarettes smoked per day as covariates. Correlation coefficients between the two variables were evaluated by calculating the Pearson’s correlation coefficient (R) or Spearman’s correlation coefficient (rho) according to the distribution patterns of the evaluated variables, which was followed by a test of no correlation. Hierarchical clustering was performed to categorize the five WBC subtypes and generate dendrograms. Statistical significance was set at p < 0.005 for simultaneous multiple comparisons with the Bonferroni adjustment. Statistical analyses were performed using the R Statistical Software (version 4.0.5; R Foundation, Vienna, Austria). The Cocor package was used to compare the R values of the two independent groups13.
Ethics
This study was approved by the Institutional Review Board of the Tohoku University School of Medicine (IRB approval number: 2020-4-072). All processes in this study were performed in accordance with the current version of the Declaration of Helsinki, as revised in 2013. Written informed consent was obtained from all enrolled individuals.
Results
Participants
A total of 64 patients with MS (13 men and 51 women) and 2492 HCs without any neurological disease (638 men and 1854 women) were enrolled. Among the 64 patients with MS, 62 had relapsing–remitting MS and two had primary progressive MS. Thirty-two of the patients were with acute myelitis with objective clinical evidence, while the other 32 patients were in the absence of acute myelitis at the time of diagnosis. The demographic features and blood test data of the MS and HC groups are summarized in Table 1.
Among the 64 patients with MS, 54 were tested for the presence of HBsAg, antibodies against HCV, and TPHA testing, and none of them tested positive for any of these antibodies. IgM antibodies against other infections, such as measles, rubella, mumps, varicella-zoster virus (VZV), herpes simplex virus (HSV), cytomegalovirus, and human immunodeficiency virus (HIV), were absent in all of the evaluated patients with MS. Fifty-eight of the 64 patients with MS were evaluated for ANA positivity; of them, 57 (98.3%) tested negative (1:40), and one patient presented a value of 1:160. Serum CRP level was evaluated in all 64 patients, of whom 62 (96.9%) revealed normal levels (< 0.30 mg/dL) and two patients revealed a slightly elevated level (0.38 mg/dL and 0.30 mg/dL). Fifty-seven of the 64 patients underwent CSF analysis at the time of hemogram, and CSF-restricted OCBs were positive in 47 (82.5%) patients. The median (IQR) for CSF-CC was 2 (1–5) [/μL], for IgG-index was 0.68 (0.60 – 0.89), for QAlb was 0.0048 (0.0034–0.0059), and for QIgG was 0.0035 (0.0025–0.0048).
Blood cell counts in the HC and MS groups
The total and differential WBC counts were subsequently compared between the MS and HC groups. The results are listed in the lower half of Table 1, and the boxplots for each of the measured blood cell counts and their ratios are depicted in Fig. 1. The WBC count was significantly higher in the MS group than in the HC group (Mann–Whitney U test, p < 0.0001). The RBC count (p = 0.0260) and platelet count (p = 0.0155) were not significantly different between the two groups. The differential counts of the five WBC subtypes were evaluated and compared between the groups to further investigate the elevated WBC count in the MS group. The differential counts of monocytes (p < 0.0001), basophils (p = 0.0027), and neutrophils (p < 0.0001) were significantly higher in the MS group than in the HC group, whereas the differential counts of lymphocytes (p = 0.5025) and eosinophils (p = 0.3523) did not differ significantly between the two groups. Further derivatives of NLR, PLR, and MLR were achieved using each of these components for the WBC count. The NLR (p = 0.0029) and MLR (p = 0.0003) were significantly higher in the MS group than in the HC group, whereas the PLR was the same in both groups. For reference, the blood neutrophil counts of the two patients with primary progressive MS were 3550 and 3050 cells/μL, and the blood monocyte counts were 290 and 340 cells/μL, respectively.
Boxplots of blood cell subtypes in the HC and MS Groups. Boxplots for three blood cell types, five differential white blood cell subtypes, and the three derived ratios (NLR, PLR, MLR) calculated from the differential white blood cell counts are shown. The p-values are the results of the Mann–Whitney U test, and the effect size \(r\) below each p-value was calculated as \(\left(Z/\sqrt{n}\right)\). HC, healthy controls; MLR, monocyte-to-lymphocyte ratio; MS, multiple sclerosis; NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio.
The ANCOVA, using the number of daily cigarette consumption and BMI, was further performed for each WBC differential to adjust for the possible confounding effects of the current smoking status and obesity on the measured WBC differentials. As a result, the monocyte (p < 0.0001), basophil (p = 0.0009), and neutrophil (p < 0.0001) counts remained significantly higher in the MS group than in the HC group, even after adjusting for these potential confounding factors. Meanwhile, the eosinophil (p = 0.0297) and lymphocyte (p = 0.4130) counts still showed no difference between the groups, even after adjusting for these factors.
Correlations between differential counts of WBC subtypes
Next, the correlation coefficients between each pair of differential counts of the five WBC subtypes were evaluated (Table 2). The correlation between neutrophils and lymphocytes was confirmed in the HC group (R = + 0.329). Meanwhile, there was no correlation in the MS group (R = − 0.096). The difference in the correlation coefficient between the HC and MS groups was statistically significant (p = 0.0007). The correlation between monocytes and lymphocytes was present in the HC group (R = + 0.395), but was absent in the MS group (R = + 0.099). Conversely, the correlation between basophils and lymphocytes was absent or very weak in the HC group (R = + 0.195), whereas it was statistically significant in the MS group (R = + 0.467). Correlation coefficients for other pairs of WBC subtypes were not significantly different between the HC and MS groups. Dendrograms for the five differential counts in the HC and MS groups were constructed using hierarchical clustering to visually confirm the different features of the correlation network between the WBC subtypes in the MS group (Fig. 2). The generated dendrograms showed different structures and abnormal lymphocyte behavior in the MS group. The structures of the dendrogram for the other four white blood cell subtypes in the MS group were similar to those in the HC group.
Dendrograms generated from Hierarchical Clustering of White Blood Cell Subtypes in the HC and MS Groups. The dendrogram generated for the HC group was with the distance of the lymphocyte count closer to monocyte and neutrophil counts than to eosinophil or basophil counts. Meanwhile, the dendrogram showed a different structure in the MS group, with the distance of the lymphocyte count closer to eosinophil and basophil counts. HC, healthy controls; MS, multiple sclerosis.
Scatterplots of lymphocyte and neutrophil counts in the HC and MS groups
The correlation between the differential counts of the neutrophil and lymphocyte pairs (R = + 0.329 vs. − 0.096, p = 0.0007) was significantly different between the HC and MS groups. Thus, scatterplots depicting the differential counts of neutrophils and lymphocytes were further constructed for the HC and MS groups (Fig. 3). On the log-transformed scatterplot, the distribution in MS patients was largely dispersed compared to that in HC, mainly in the upper-left area of the graph (i.e., suggesting neutrophilic dominance). Fifteen of the 64 patients with MS (23.4%) showed NLR values higher than the values for 95% of the individuals in the HC group. The correlation between neutrophil and lymphocyte counts was apparent in the HC group, whereas it was not apparent in the MS group.
Scatterplot of Lymphocyte and Neutrophil Counts in the Blood of the HC and MS Groups. Patients with MS showed a significantly higher distribution of neutrophil-to-lymphocyte ratio, together with no correlation between neutrophil and lymphocyte counts, compared to those in HC. Note that both the vertical and horizontal axes are log-transformed. HC, healthy controls; MS, multiple sclerosis.
Clinical significance of differential WBC counts in MS
Correlations between the evaluated laboratory data and the variables with respect to the disease activity or severity were further evaluated based on the significantly elevated WBC, monocyte, basophil, and neutrophil counts in MS at the time of diagnosis before starting the treatment (Table 3). None of the evaluated laboratory markers, including the differential WBC counts, significantly correlated with the disease activity (number of T2 hyperintense brain lesions) or severity (EDSS score after 1 year), except for a negative correlation between the eosinophil count and the number of T2 hyperintense brain lesions. Even when the impact of each differential WBC on disease activity or severity was evaluated based on its percentage [%] (i.e., not the absolute count [/μL]), none of the five cell types showed a significant impact on the disease activity or severity. For reference, the monocyte count showed a weak positive correlation with the value of QAlb (Pearson’s R = + 0.397, p = 0.0039), whereas the other WBC differentials did not.
Discussion
The profiles of blood cell counts in the peripheral blood of patients with MS before starting acute or chronic treatment were comprehensively evaluated and compared with the profiles of HCs in this study. The results revealed that the total WBC count and differential monocyte, basophil, and neutrophil counts, all of which are related to the innate immune system, were significantly elevated in the MS group compared to the HC group. Meanwhile, the lymphocyte count was not elevated in the MS group. The correlation between neutrophil and lymphocyte counts was apparent in the HCs, but was not apparent in the MS group. Based on the results that none of the patients tested positive for the serum antibodies against major viral infections (e.g., HBV, HCV, HIV, HSV, VZV), all the clinical attacks at the time of the hemogram in the 64 patients with MS could be considered to have occurred in the absence of infection. Moreover, the resultant findings were irrespective of the current amount of cigarette consumption or the BMI. These results suggest that the balance between the innate and adaptive (i.e., acquired) immune system may have changed systemically in MS from the early stages, which could have resulted in the observed elevations in NLR and MLR. An elevated NLR in patients with MS compared to healthy individuals has been similarly reported in several previous studies6,7. These previous studies even demonstrated that the level of NLR may affect the subsequent disability progression. These facts indicate that an upregulated innate immunity may play a possible role in some steps of the disease development and progression in MS.
Meanwhile, it has been known that an upregulated innate immune system can be observed non-specifically in several conditions. In general, neutrophils are the key cell type of the innate immune system, as well as the first cellular defense against external pathogens, including infections. Neutrophil trafficking to the site is an important step of inflammation, constituting a hallmark of inflammation, and presents as an increase in neutrophil and a decrease in lymphocyte counts. The inflammatory response is considered to result in the production of neutrophils and accelerated apoptosis of lymphocytes14. Consequently, the finding of the elevated total WBC count with elevated NLR would not certainly be distinct to MS, and the achieved results could have resulted from a non-specific activation of the innate immune system with the mild suppression of adaptive immunity. In neurological conditions other than MS, an elevated NLR and/or its potential for outcome prediction has been suggested in stroke, and some neurodegenerative disorders, such as Alzheimer’s and Parkinson’s diseases15,16,17. A shift from adaptive to upregulated innate immune systems may play some role in the progression or acceleration of the neurodegenerative processes in the damaged site in these diseases. Furthermore, this study failed to show significant positive correlations between the elevated differential WBC counts and the markers of disease activity or severity in MS. The exact role of elevated blood neutrophil and monocyte counts in the development and progression of MS remains largely unknown. A conceivable theory may be that psychological stress due to the neurological disturbances among patients with MS could have changed the balance of innate and adaptive immunities, thus resulting in the elevation of NLR and MLR. Psychological stress is known to increase the total WBC, neutrophil, and monocyte counts in the general population18,19,20. Although this is only a speculation as the stress level was not evaluated in the enrolled patients, such psychological distress with possible post-stress inflammation in the blood among the patients with MS could have produced the apparent difference in the total WBC, neutrophil, and monocyte counts between the patients with MS and HCs in this study.
Although the finding of the elevated blood neutrophils and monocytes is not specific to MS and may not play a pivotal role in the development of MS lesions, the role of neutrophils in the development of MS has been long discussed in previous studies. The possible association between neutrophils and the development of demyelinating lesions in MS has been previously reported. Previous studies using an animal model of MS, known as experimental autoimmune encephalomyelitis (EAE), demonstrated that neutrophils play a role in the development of demyelinating lesions by promoting parenchymal infiltration of leukocytes in the CNS21. Another study that evaluated the peripheral blood of patients with MS showed that the neutrophils in patients with MS are in a primed state, rather than a resting state, possibly resulting from the chronic proinflammatory environment and resulting in enhanced innate immunity responses during infections22. In addition to neutrophils, monocytes have been reported to play a role in the pathogenesis of MS. A previous study on EAE showed that circulatory monocytes prefer proinflammatory M1 activation rather than the immunomodulatory M2 activation and this plays a key role in the development of demyelinating CNS lesions23. Several other previous reports on peripheral blood samples from patients with MS demonstrated that elevated monocytes in MS are possibly associated with disease severity or subsequent neurological prognosis7,24. Meanwhile, neutrophils are not the major cell type of parenchymal infiltrations in MS lesions. Together with the results of the present study, these facts suggest that an activated innate immune system based on a chronic proinflammatory environment underlies the pathogenesis of MS and promotes cellular parenchymal infiltrations through the blood–brain barrier, which result in disease relapses. Furthermore, the results of this study and previous studies imply the possible role of the activated or primed innate immune system in MS may play roles in MS disease progression and the indolent progression of neurological disturbances between relapses. The current relapse-prevention treatments for MS mainly focus on suppressing the functions of the adaptive immune system, but suppressing the innate immune system in MS may be a possible therapeutic option.
This study has some limitations. First, the sample size in the MS group was relatively small. However, if we increase the number of facilities to achieve a larger sample size, the risks of bias based on errors between facilities may also increase. As such errors between facilities would surely cause significant bias in the measured WBC differential counts and the calculated correlation coefficients between the five WBC subtypes (especially for white blood cells with low counts such as eosinophils and basophils), the present study was performed using data from a single facility. Another limitation was that the mechanism and physiological significance of the observed correlation between lymphocyte and basophil counts in the MS group is unknown. Currently, the exact role of basophils in the pathogenesis of autoimmune-related diseases is not fully elucidated, although it is believed to be associated with innate immunity and plays a role in chronic allergic inflammations25. To establish the significance of monocytes, basophils, and neutrophils in the pathogenesis of MS, further research is needed to clarify the mechanisms underlying the altered profiles of these blood cells in patients with MS.
In conclusion, patients with MS are likely to show elevated counts of neutrophils, monocytes, and basophils in the peripheral blood at the early disease stages before the initiation of acute or chronic treatment. A positive correlation between the neutrophil and lymphocyte counts, which was evident in the healthy population, was weakened in patients with MS. A systemic shift from adaptive to upregulated innate immune processes may play possible role in the development or progression of MS and necessitates the need for further research with respect to the role of neutrophils and monocytes in the pathophysiology of MS.
Data availability
Data regarding the blood test data for MS patients are available from the authors on reasonable requests from qualified clinicians or researchers.
Abbreviations
- HC:
-
Healthy controls
- MLR:
-
Monocyte-to-lymphocyte ratio
- MS:
-
Multiple sclerosis
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- WBC:
-
White blood cell
References
Lassmann, H. Multiple sclerosis pathology. Cold Spring Harb. Perspect. Med. 8(3), a028936 (2018).
Kamm, C. P., Uitdehaag, B. M. & Polman, C. H. Multiple sclerosis: Current knowledge and future outlook. Eur. Neurol. 72(3–4), 132–141 (2014).
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17(2), 162–173 (2018).
Hasselbalch, I. C. et al. The neutrophil-to-lymphocyte ratio is associated with multiple sclerosis. Mult. Scler. J. Exp. Transl. Clin. 4(4), 2055217318813183 (2018).
Bisgaard, A. K., Pihl-Jensen, G. & Frederiksen, J. L. The neutrophil-to-lymphocyte ratio as disease activity marker in multiple sclerosis and optic neuritis. Mult. Scler. Relat. Disord. 18, 213–217 (2017).
Demirci, S., Demirci, S., Kutluhan, S., Koyuncuoglu, H. R. & Yurekli, V. A. The clinical significance of the neutrophil-to-lymphocyte ratio in multiple sclerosis. Int. J. Neurosci. 126(8), 700–706 (2016).
Hemond, C. C., Glanz, B. I., Bakshi, R., Chitnis, T. & Healy, B. C. The neutrophil-to-lymphocyte and monocyte-to-lymphocyte ratios are independently associated with neurological disability and brain atrophy in multiple sclerosis. BMC Neurol. 19(1), 23 (2019).
Prame Kumar, K., Nicholls, A. J. & Wong, C. H. Y. Partners in crime: neutrophils and monocytes/macrophages in inflammation and disease. Cell Tissue Res. 371(3), 551–565 (2018).
Chirumbolo, S., Bjørklund, G., Sboarina, A. & Vella, A. The role of basophils as innate immune regulatory cells in allergy and immunotherapy. Hum. Vaccin. Immunother. 14(4), 815–831 (2018).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 69(2), 292–302 (2011).
Hozawa, A. et al. Study profile of the Tohoku Medical Megabank Community-Based Cohort Study. J. Epidemiol. 31(1), 65–76 (2021).
Kuriyama, S. et al. The Tohoku Medical Megabank Project: Design and mission. J. Epidemiol. 26(9), 493–511 (2016).
Diedenhofen, B. & Musch, J. cocor: a comprehensive solution for the statistical comparison of correlations. PLoS ONE 10(3), e0121945 (2015).
Liu, Y. et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J. Infect. 81(1), e6–e12 (2020).
Tokgoz, S. et al. Neutrophil lymphocyte ratio as a predictor of stroke. J. Stroke Cerebrovasc. Dis. 22(7), 1169–1174 (2013).
Kuyumcu, M. E. et al. The evaluation of neutrophil-lymphocyte ratio in Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 34(2), 69–74 (2012).
Akıl, E. et al. The increase of carcinoembryonic antigen (CEA), high-sensitivity C-reactive protein, and neutrophil/lymphocyte ratio in Parkinson’s disease. Neurol. Sci. 36(3), 423–428 (2015).
Maes, M. et al. The effects of psychological stress on leukocyte subset distribution in humans: evidence of immune activation. Neuropsychobiology 39(1), 1–9 (1999).
Nishitani, N. & Sakakibara, H. Association of psychological stress response of fatigue with white blood cell count in male daytime workers. Ind. Health 52(6), 531–534 (2014).
Aydin Sunbul, E. et al. Increased neutrophil/lymphocyte ratio in patients with depression is correlated with the severity of depression and cardiovascular risk factors. Psychiatry Investig. 13(1), 121–126 (2016).
Pierson, E. R., Wagner, C. A. & Goverman, J. M. The contribution of neutrophils to CNS autoimmunity. Clin. Immunol. 189, 23–28 (2018).
Naegele, M. et al. Neutrophils in multiple sclerosis are characterized by a primed phenotype. J. Neuroimmunol. 242(1–2), 60–71 (2012).
Mikita, J. et al. Altered M1/M2 activation patterns of monocytes in severe relapsing experimental rat model of multiple sclerosis. Amelioration of clinical status by M2 activated monocyte administration. Mult. Scler. 17(1), 2–15 (2011).
Akaishi, T., Takahashi, T. & Nakashima, I. Peripheral blood monocyte count at onset may affect the prognosis in multiple sclerosis. J. Neuroimmunol. 319, 37–40 (2018).
Miyake, K. & Karasuyama, H. Emerging roles of basophils in allergic inflammation. Allergol. Int. 66(3), 382–391 (2017).
Funding
This work was supported by MHLW Program Grant Number 20FC1030 (I.N.) and JSPS KAKENHI Grant Number 20K07892 (I.N.).
Author information
Authors and Affiliations
Contributions
T.A.: designed and conceptualized the study, analyzed data, and wrote the first draft. T.M.: designed and conceptualized the study, collected data, analyzed data, critically revised the manuscript, and supervised the study process. K.F.: collected data, analyzed data, critically revised the manuscript, and supervised the study process. N.N., T.N., M.K., R.H., F.I., I.K., T.T., H.K., J.F., Y.T., S.N., and K.K.: collected data, analyzed data, and critically revised the manuscript. T.I. and M.A.: interpreted the data, critically revised the manuscript, and supervised the study process. I.N. and A.H.: designed and conceptualized the study, collected data, analyzed data, critically revised the manuscript, and supervised the study process.
Corresponding author
Ethics declarations
Competing interests
K. Fujihara received speaker honoraria and travel funding from Bayer, Biogen Japan, Eisai, Mitsubishi Tanabe, Novartis, Astellas, Takeda, Asahi Kasei Medical, Daiichi Sankyo, and Nihon Pharmaceutical and received research support from Bayer, Biogen, Asahi Kasei Medical, The Chemo-Sero-Therapeutic Research Institute, Teva, Mitsubishi Tanabe Pharma, Teijin, Chugai, Ono, Nihon Pharmaceutical, and Genzyme. I. Nakashima received speaker honoraria and travel funding from Mitsubishi Tanabe Pharma, Biogen Japan, and Novartis Pharmaceuticals and received research support from LSI Medience Corporation. The remaining authors don’t have any conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akaishi, T., Misu, T., Fujihara, K. et al. White blood cell count profiles in multiple sclerosis during attacks before the initiation of acute and chronic treatments. Sci Rep 11, 22357 (2021). https://doi.org/10.1038/s41598-021-01942-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01942-8
- Springer Nature Limited
This article is cited by
-
Autologous hematopoietic stem cell transplantation significantly alters circulating ceramides in peripheral blood of relapsing-remitting multiple sclerosis patients
Lipids in Health and Disease (2023)
-
White blood cell count profiles in anti-aquaporin-4 antibody seropositive neuromyelitis optica spectrum disorder and anti-myelin oligodendrocyte glycoprotein antibody-associated disease
Scientific Reports (2023)
-
Genetic susceptibility for autoimmune diseases and white blood cell count
Scientific Reports (2023)
-
Neutrophil-to-Lymphocyte Ratio: a Marker of Neuro-inflammation in Multiple Sclerosis Patients: a Meta-analysis and Systematic Review
SN Comprehensive Clinical Medicine (2023)