Abstract
The incidence of invasive fungal infection (IFI) in patients with acute myeloid leukemia (AML) has decreased with the introduction of antimold prophylaxis. Although acute lymphoblastic leukemia (ALL) has a lower risk of IFI than does AML, the incidences of IFI in both AML and ALL in the era of antimold prophylaxis should be re-evaluated. We analyzed adults with AML or ALL who had undergone induction, re-induction, or consolidation chemotherapy from January 2017 to December 2019 at Seoul National University Hospital. Their clinical characteristics during each chemotherapy episode were reviewed, and cases with proven or probable diagnoses were regarded as positive for IFI. Of 552 episodes (393 in AML and 159 in ALL), 40 (7.2%) were IFI events. Of the IFI episodes, 8.1% (12/148) and 5.9% (13/220) (P = 0.856) occurred in cases of ALL without antimold prophylaxis and AML with antimold prophylaxis, respectively. After adjusting for clinical factors, a lack of antimold prophylaxis (adjusted odds ratio [aOR], 3.52; 95% confidence interval [CI], 1.35–9.22; P = 0.010) and a longer duration of neutropenia (per one day, aOR, 1.02; 95% CI, 1.01–1.04; P = 0.001) were independently associated with IFI. In conclusion, the incidence of IFI in ALL without antimold prophylaxis was not lower than that in AML. A lack of antimold prophylaxis and prolonged neutropenia were independent risk factors for IFI. Clinicians should be on guard for detecting IFI in patients with ALL, especially those with risk factors.
Similar content being viewed by others
Introduction
Invasive fungal infections (IFIs) are opportunistic infections that cause substantial morbidity and mortality in patients with acute leukemia. Classically, the risk of IFI has been considered higher in acute myelogenous leukemia (AML) than in acute lymphoblastic leukemia (ALL), possibly due to leukocyte dysfunctions in the myeloid lineage and a longer duration of neutropenia following cytotoxic chemotherapy1,2,3,4,5.
There are no specific recommendations for antifungal prophylaxis in cytotoxic chemotherapy for ALL, partly due to the lower incidence of IFI6. By contrast, posaconazole prophylaxis is now routinely recommended in induction or re-induction chemotherapy for patients with AML6, because it significantly reduces the incidence of IFI in those patients1.
The incidences of IFI in patients with AML and ALL with or without antimold prohpylaxis needs to be re-evaluated to guide clinicians what level of suspicion for IFI is warranted in these respective scenarios. Specifically, the incidences of IFI in ALL without prophylaxis and AML with prophylaxis are of interest to assess whether ALL still has a lower risk of IFI compared to AML in the era of antimold prophylaxis.
Therefore, we elucidated the incidence of, and risk factors for IFI in patients with AML or ALL receiving cytotoxic chemotherapy after the introdction of posaconazole prophylaxis for AML.
Results
Clinical characteristics of patients with AML or ALL
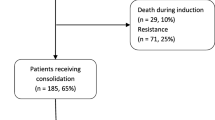
A total of 552 episodes were identified for 149 AML (393 episodes) and 51 ALL (159 episodes) patients (Table 1). The patients with AML episodes were significantly older (median {interquartile range [IQR]}) (56 [49–63] years for AML patients vs. 45 [31–62] years for ALL patients, P < 0.001) and had higher CCI scores (3 [3–5] for AML patients vs. 3 [2–4] for ALL patients, P < 0.001) and a longer duration of neutropenia (18 [11–28] days for AML patients vs. 8 [3–15] days for ALL patients, P < 0.001). Induction or re-induction episodes were significantly more frequent in the AML patients than in the ALL patients (237/393 [60.3%] for AML patients vs. 73/159 [45.9%] for ALL patients, P = 0.002), and the rate of antimold prophylaxis was significantly higher for AML episodes (220/393 [56.0%] for AML episodes vs. 11/159 [6.9%] for ALL episodes, P < 0.001). Posaconazole was the most commonly used prophylactic agent, which was used for durations of (days, median [IQR]) of 25 (18–34) in AML and 8 (6–8) in ALL.
Comparing the clinical characteristics between episodes with and without antimold prophylaxis, there were significant differences in CCI score, rate of induction or re-induction chemotherapy, type of leukemia, and duration of neutropenia (Supplementary Table S1).
Incidence of IFI
The incidence of IFI was not significantly different between AML and ALL episodes (28/393 [7.1%] for AML episodes vs. 12/159 [7.5%] for ALL episodes, P = 0.862). Of all episodes with IFI, invasive aspergillosis was the most frequent type (21/28 [75.0%] for AML episodes and 7/12 [58.3%] for ALL episodes), followed by invasive candidiasis. 27 of 28 invasive aspergillosis cases in the present study met the criteria for a probable diagnosis.
We examined the incidence of IFI in AML or ALL episodes with or without antimold prophylaxis (Table 2). The incidence of IFI in AML episodes with antimold prophylaxis was 5.9% (13/220) versus 8.7% (15/173) without. In ALL episodes, the incidence of IFI was 0% (0/11) with antimold prophylaxis and 8.1% (12/148) without. The difference in IFI incidence between ALL episodes without antimold prophylaxis and AML episodes with antimold prophylaxis was not significant (OR, 1.41; 95% CI, 0.62–3.17; P = 0.856). When the latest 2020 European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium (EORTC/MSGERC) definition was used (Supplementary Table S2), the incidences of IFI were 5.0% (11/220) in AML with prophylaxis and 7.5% (13/173) in ALL without prophylaxis.
We also evaluated the incidence of invasive mold infection in various scenarios (Supplementary Table S3). All of these were cases of invasive pulmonary aspergillosis. The incidence in AML episodes with antimold prophylaxis was 4.1% (9/220) versus 6.9% (12/173) without. The incidence of invasive mold infection in ALL episodes with antimold prophylaxis was 0% (0/11) versus 4.7% (7/148) without.
Independent risk factors for IFI
Uni- and multivariable analyses were performed to compare episodes with and without IFI to elucidate independent risk factors for IFI (Table 3). In the univariable analysis, there were significant differences in the rate of induction or re-induction chemotherapy (29/40 [72.5%] for IFI episodes vs. 281/512 [54.9%] for non-IFI episodes, P = 0.031) and the number of days of neutropenia (median [IQR], 21 [12–32] for IFI episodes vs. 14.5 [8–25] for non-IFI episodes, P = 0.006). Multivariable analysis revealed that a lack of antimold prophylaxis (adjusted OR [95% CI], 3.52 [1.35–9.22]; P = 0.01) and a longer duration of neutropenia (adjusted OR [95% CI], per day, 1.02 [1.01–1.04]; P = 0.004) were independent risk factors for IFI. The results were similar when the 2020 EORTC/MSGERC definition was applied (Supplementary Table S4).
Sensitivity analyses
Seventy-two episodes involving the therapeutic administration of antimold agents during the episodes were excluded for the first sensitivity analysis. The incidence of IFI in AML episodes with antimold prophylaxis was 7.4% (13/176) versus 9.0% (12/134) in ALL episodes without antimold prophylaxis (Supplementary Table S5; OR [95% CI], 1.23 [0.54–2.80]; P = 0.616). Independent risk factors for IFI were a lack of antimold prophylaxis (adjusted OR [95% CI], 3.77 [1.32–10.79]; P = 0.013) and prolonged neutropenia (adjusted OR [95% CI], per one day, 1.03 [1.01–1.04]; P = 0.001) (Supplementary Table S6).
The 200 episodes (all were induction or re-induction) included in the second sensitivity analysis, included 11 IFI episodes (Supplementary Table S7). In patients with AML, the incidence of IFI was 4.9% (7/144) with prophylaxis versus 20.0% (1/5) without. In patients with ALL, the incidence was 0% (0/6) and 6.7% (3/45), respectively. Only a longer duration of neutropenia was an independent risk factor for IFI in this subgroup (adjusted OR [95% CI], 1.03 [1.01–1.06]; P = 0.015) (Supplementary Table S8).
Discussion
Although AML has been traditionally believed to be associated with a greater risk of IFI than ALL2,3,4,5, the recent introduction of antimold prophylaxis in induction and re-induction chemotherapy has considerably reduced the incidence of IFI in AML1,6,7. Since then, it was unknown whether ALL is still associated with a lower risk of IFI than AML in the era of antimold prophylaxis. The study was performed to address this, and we found that the incidence of IFI in ALL was not lower than that in AML.
In addition to previous observations that AML is associated with a higher incidence of IFI than is ALL8,9, there are some theoretical reasons for a higher risk of IFI in AML than in ALL. First, myeloid cell dysfunction poses a greater risk of IFI than does lymphoid cell dysfunction. Second, the duration of neutropenia after cytotoxic chemotherapy is generally longer in AML than in ALL2,5,9. In an effort to reduce IFI in AML, a multicenter randomized controlled trial of patients with AML or myelodysplastic syndrome was performed, which showed that posaconazole prophylaxis significantly reduced the incidence of IFI compared with fluconazole or itraconazole prophylaxis1. This led to the current recommendation for posaconazole prophylaxis in patients with AML undergoing induction or re-induction chemotherapy6,10.
No routine antimold prophylaxis is recommended for patients with ALL receiving cytotoxic chemotherapy, owing to the lower IFI incidence and possible neurotoxic interactions between azoles and vinca alkaloids6,11. Therefore, studies of the incidences of, and risk factors for IFI in AML or ALL that reflect the current situation are warranted to guide clinicians. Because the diagnosis of IFI is often complicated, estimating the pre-test probability of IFI in patients with acute leukemia is very important for interpreting the results of clinical and mycological tests12,13,14. We showed that the incidence of IFI in ALL without antimold prophylaxis was not lower than that in AML with antimold prophylaxis, indicating that the notion of a lower risk of IFI in ALL than in AML needs to be modified. Clinicians should remain highly suspicious of IFI in ALL patients who are not receiving antimold prophylaxis, especially those with prolonged neutropenia. In addition, antimold prophylaxis could be considered in patients with ALL who are expected to have a longer duration of neutropenia than usual occasion.
Studies suggest that an advanced age, prolonged neutropenia, and the relapse of hematological malignancies are risk factors for IFI in acute leukemia2,5. However, most studies were performed on AML cases, and few have examined the risk factors for IFI in patients with ALL. In a single-center, retrospective study, Nicolato et al. showed that a longer duration of neutropenia, the relapse of underlying diseases, a longer duration of hospitalization before the first fever, and allogeneic HSCT were risk factors for IFI in ALL9, which is in accordance with our results. Notably, the type of acute leukemia itself (i.e., AML and ALL) was not independently associated with the occurrence of IFI in this study.
To increase the reliability of our results, sensitivity analyses were performed under two conditions. In the first, we excluded those who received a therapeutic antimold agent during an episode. In the second, we included only the first episodes of every patient in the study period, although we used a GEE to explore independent risk factors for IFI to lessen the effects of repeated inclusion of patients15. The main results, namely, that the incidence of IFI in ALL without prophylaxis was comparable to that in AML with prophylaxis, and a lack of antimold prophylaxis and a longer duration of neutropenia were independent risk factors for IFI, remained unchanged in these analyses (Supplementary Table S5–S8). In addition, the incidence of invasive mold infection did not differ significantly between these two groups (Supplementary Table S3).
There are some limitations to our study. First, it included a study population with a small sample size enrolled from a single university-affiliated hospital. Particularly, the analyses of the difference in IFI incidence according to the clinical scenario might have been under-powered. Second, because the diagnosis of IFI is often challenging and the majority of IFI cases in this study were only probable diagnoses, the retrospective nature of our study also needs to be considered. Lastly, we could not suggest a specific antimold prophylaxis regimen or schedule in ALL in this study. Further studies are warranted to validate our results and to examine clinical impact of antimold prophylaxis in selected patients with ALL. Therefore, a larger prospective study is warranted to validate our results.
In conclusion, the incidence of IFI in ALL episodes without antimold prophylaxis was not lower than that in AML episodes with antimold prophylaxis, and a lack of antimold prophylaxis and a longer duration of neutropenia were independent risk factors for IFI. Therefore, in the current era of antimold prophylaxis, clinicians should also be on guard for the occurrence of IFI in patients with ALL, especially those with characteristics that put them at higher risk.
Materials and methods
Study design and data collection
We retrospectively reviewed all adults (≥ 18 years) with AML or ALL who received induction, re-induction, or consolidation cytotoxic chemotherapy from January 2017 to December 2019 at Seoul National University Hospital. Cases of hematopoietic stem-cell transplantation (HSCT) were excluded, because antimold prophylaxis is routinely given regardless of the type of acute leukemia6. Episodes of palliative chemotherapy, such as that using decitabine or azacitidine, and research-based chemotherapy were also excluded.
Clinical data were reviewed using electronic medical records including those on age, gender, the type of acute leukemia, purpose of cytotoxic chemotherapy, specific agents administered, severity of underlying diseases measured by based on the Charlson’s comorbidity-weighted index (CCI) score16, administration of antimold agent, duration of neutropenia, and occurrence and type of IFI.
The incidence of IFI was examined in AML or ALL episodes with or without antimold prophylaxis. The clinical characteristics of the IFI episodes were compared to reveal independent risk factors for IFI.
This study was approved by the Institutional Review Board at Seoul National University Hospital (IRB no. 2008–167-1151), and they waived obtaining the informed consent because of the retrospective nature of the study. All study procedures were performed in accordance with the Declaration of Helsinki.
Definition
Only cases with proven and probable diagnoses following the 2008 Revised EORTC/MSG guideline were regarded as positive for IFI in this study17. Although we used the 2008 version in main analysis to account for the study period preceding the guideline revision, and to retain a higher sensitivity for the clinical diagnosis of IFI12, we performed the same analyses and presented the results using 2020 version.
An episode was defined as the period between the date of starting chemotherapy and the date of discharge. If two or more rounds of chemotherapy were performed during one hospitalization, the period was divided according to the day the subsequent chemotherapy began19. Antimold prophylaxis included routine posaconazole prophylaxis for induction or re-induction chemotherapy in AML or antimold agents for secondary prophylaxis due to a history of invasive mold infection.
The duration of neutropenia was defined as the time between the first date of an absolute neutrophil count (ANC) lower than 500/mm3 and the third day with an ANC higher than 500/mm3, as previously described9,20,21.
Sensitivity analysis
Two sensitivity analyses were performed to account for potential confounders. First, the incidences of, and risk factors for IFI were re-examined after excluding all episodes with therapeutic administration of an antimold agent (e.g., liposomal amphotericin B, caspofungin, etc.) for prolonged neutropenic fever, because this could obscure the effect of a prophylactic antimold agent. Second, we analyzed the subgroup that included only the first episodes for every patient to exclude the effects from repeated inclusion of the patients.
Statistical analysis
The chi-square or Fisher’s exact test was used to compare categorical variables. Based the normality of continuous variables assessed using the Shapiro–Wilk test, the Mann–Whitney U test or Students’ t- test was used. To calculate odds ratio (OR) and associated 95% confidence interval (CI) for IFI in different clinical scenarios (AML or ALL with or without antimold prophylaxis) logistic regression was used. For the multivariable analysis, variables were analyzed using backward stepwise logistic regression. Variables were removed using a P value of 0.05 as the cut-off value. Where applicable, generalized estimating equations (GEEs) were used to account for the inclusion of multiple episodes from a patient15. A P value < 0.05 was considered to indicate statistical significance in all analyses. All statistical analysis were performed using IBM SPSS Statistics, ver. 27.0 (IBM, Armonk, NY, USA).
References
Cornely, O. A. et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N. Engl. J. Med. 356, 348–59 (2007).
Nucci, M. & Anaissie, E. How we treat invasive fungal diseases in patients with acute leukemia: the importance of an individualized approach. Blood 124, 3858–3869 (2014).
Cattaneo, C. et al. Invasive pulmonary aspergillosis in acute leukemia: a still frequent condition with a negative impact on the overall treatment outcome. Leuk Lymphoma 60, 3044–3050 (2019).
Pagano, L. et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica 91, 1068–1075 (2006).
Pagano, L. et al. Risk assessment and prognostic factors for mould-related diseases in immunocompromised patients. J. Antimicrob. Chemother. 66(Suppl 1), i5-14 (2011).
Maertens, J. A. et al. European guidelines for primary antifungal prophylaxis in adult haematology patients: summary of the updated recommendations from the European Conference on Infections in Leukaemia. J. Antimicrob. Chemother. 73, 3221–3230 (2018).
Vehreschild, J. J. et al. Clinical effectiveness of posaconazole prophylaxis in patients with acute myelogenous leukaemia (AML): a 6 year experience of the Cologne AML cohort. J. Antimicrob. Chemother. 65, 1466–1471 (2010).
Mariette, C. et al. Epidemiology of invasive fungal infections during induction therapy in adults with acute lymphoblastic leukemia: a GRAALL-2005 study. Leuk Lymphoma 58, 586–593 (2017).
Nicolato, A. et al. Invasive fungal diseases in patients with acute lymphoid leukemia. Leuk Lymphoma 57, 2084–2089 (2016).
Tacke, D. et al. Primary prophylaxis of invasive fungal infections in patients with haematologic malignancies. 2014 update of the recommendations of the Infectious Diseases Working Party of the German Society for Haematology and Oncology. Ann. Hematol. 93, 1449–56 (2014).
Moriyama, B. et al. Adverse interactions between antifungal azoles and vincristine: review and analysis of cases. Mycoses 55, 290–297 (2012).
Siopi, M. et al. A Prospective Multicenter Cohort Surveillance Study of Invasive Aspergillosis in Patients with Hematologic Malignancies in Greece: Impact of the Revised EORTC/MSGERC 2020 Criteria. J Fungi (Basel) 7 (2021).
Ullmann, A. J. et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 24(Suppl 1), e1–e38 (2018).
Lass-Florl, C. How to make a fast diagnosis in invasive aspergillosis. Med. Mycol. 57, S155–S160 (2019).
Seibold, H. et al. A computational reproducibility study of PLOS ONE articles featuring longitudinal data analyses. PLoS One 16, e0251194 (2021).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383 (1987).
De Pauw, B. et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin. Infect. Dis. 46, 1813–1821 (2008).
Donnelly, J. P. et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin. Infect. Dis. 71, 1367–1376 (2020).
Chang, E. et al. Limited positive predictive value of beta-d-glucan in hematologic patients receiving antimold prophylaxis. Open Forum Infect. Dis. 7, ofaa048 (2020).
Freifeld, A. G. et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin. Infect. Dis. 52, e56-93 (2011).
Lee, D. G. et al. Evidence-based guidelines for empirical therapy of neutropenic fever in Korea. Korean J. Intern. Med. 26, 220–252 (2011).
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. We appreciate the Medical Research Collaborating Center at Seoul National University Hospital for statistical analysis and consultation. This study was presented as an abstract at European Congress of Clinical Microbiology and Infectious Diseases 2021, Vienna, Austria, 9 to 12 July 2021 (Abstract number 00801).
Author information
Authors and Affiliations
Contributions
C.K.K. and I.K. contributed to study design, definition. S.M.O. and J.M.B. searched and enrolled patient lists, data collection, and sensitivity and statistical analysis. D.Y.S., Y.K., J.H., S.S.Y. supervised data analysis about underlying hematologic malignancy and patient characteristics, and E.C., P.G.C., W.B.P., N.J.K., M.D.O. supervised about invasive mold infection and antimold prophylaxis. T.S.K. contributed to analysis of the results of laboratory data. S.M.O. and J.M.B. wrote the paper and C.K.K. and I.K. revised the manuscript. All other authors critically read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oh, SM., Byun, J.M., Chang, E. et al. Incidence of invasive fungal infection in acute lymphoblastic and acute myelogenous leukemia in the era of antimold prophylaxis. Sci Rep 11, 22160 (2021). https://doi.org/10.1038/s41598-021-01716-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01716-2
- Springer Nature Limited
This article is cited by
-
The evaluation of atorvastatin as an adjunct to fluconazole for the anti-fungal prophylaxis in acute myeloid leukemia: a multicenter, triple-blinded, randomized clinical trial
Naunyn-Schmiedeberg's Archives of Pharmacology (2024)
-
Infectious complications after intensive chemotherapy with CLAG-M versus 7+3 for AML and other high-grade myeloid neoplasms
Leukemia (2023)