Abstract
Clinical outcomes are unknown after ticagrelor treatment in patients with end-stage renal disease (ESRD) who are diagnosed with acute myocardial infarction (AMI). ESRD patients who were on hemodialysis and received dual antiplatelet therapy (DAPT) for AMI between July 2013 and December 2016 were identified in Taiwan's National Health Insurance Research Database. Using stabilized inverse probability of treatment weighting, patients receiving aspirin plus ticagrelor (n = 530) were compared with those receiving aspirin plus clopidogrel (n = 2462) for the primary efficacy endpoint, a composite of all-cause death, nonfatal myocardial infarction, or nonfatal stroke, and bleeding, defined according to the Bleeding Academic Research Consortium. Study outcomes were compared between the two groups using Cox proportional hazards model or competing risk model for the hazard ratio or subdistribution hazard ratio (SHR). During 9 months of follow-up, ticagrelor was comparable to clopidogrel with respect to the risks of primary efficacy endpoint [11.69 vs. 9.28/100 patient-months; SHR, 1.16; 95% confidence interval (CI) 0.97–1.4] and bleeding (5.55 vs. 4.36/100 patient-months; SHR 1.14; 95% CI 0.88–1.47). In conclusion, among hemodialysis patients receiving DAPT for AMI, ticagrelor was comparable to clopidogrel with regard to the composite efficacy endpoint and bleeding.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) has long been considered a major risk factor for cardiovascular disease, and the risk increases linearly as renal function deteriorates1,2. CKD and end-stage renal disease (ESRD) not only accelerate the development of coronary artery disease (CAD) but also affect its clinical manifestation and symptoms, with acute myocardial infarction (AMI) more frequently being the initial presentation than stable angina3,4. AMI is a catastrophic clinical event for dialysis patients, and outcomes remain bleak even after coronary revascularization5,6. The complex hemostatic features of ESRD contribute to a simultaneous prothrombotic milieu and high bleeding risk in this population, which poses a great challenge for clinicians when prescribing dual antiplatelet therapy (DAPT) for ESRD patients who are diagnosed with AMI or who receive coronary stenting. Furthermore, ESRD is often excluded from randomized controlled trials of antithrombotic agents that establish risk–benefit profiles for the general population, precluding extrapolation of these results to this high-risk cohort.
Clopidogrel is the most widely used P2Y12 inhibitor and has several shortcomings, including delayed onset of action, modest and variable platelet inhibition, and a high on-treatment platelet reactivity (HPR) for a substantial portion of patients7,8,9. Abundant evidence has indicated an association between HPR under clopidogrel treatment and an increase in cardiovascular events after percutaneous coronary intervention (PCI), including stent thrombosis10,11,12. The prevalence of clopidogrel-related HPR is particularly high in patients with acute coronary syndrome or CKD, which has led to debate about its benefit to these patients13,14,15,16. Ticagrelor, a potent P2Y12 antagonist, provides more rapid onset and offset of action than clopidogrel and depends minimally on kidney function for metabolism and excretion17. In the PLATelet inhibition and patient Outcomes (PLATO) trial, ticagrelor, compared with clopidogrel, reduced the composite endpoint of cardiovascular death, nonfatal MI, or stroke but increased the rate of bleeding unrelated to procedure18. In a prespecified substudy of the PLATO trial, the advantage of ticagrelor was even greater in patients with CKD, with a 23% relative reduction in the primary ischemic endpoint19. However, ESRD was an exclusion criterion of the PLATO trial. Whether ticagrelor is superior to clopidogrel in the ESRD population is unknown. In this study, we used the National Health Insurance Research Database (NHIRD) of Taiwan to compare the efficacy and safety of ticagrelor versus clopidogrel in the treatment of AMI among patients with ESRD requiring maintenance hemodialysis.
Methods
Data source
Taiwan's National Health Insurance (NHI) Program is a government-run, mandatory health insurance program, covering approximately 99.9% of citizens in Taiwan20. Taiwan's NHIRD, one of the largest administrative healthcare databases in the world, provides patient-level data on basic demographic information, disease diagnosis, prescriptions, operations, investigations, and each outpatient visit or inpatient care details. Previous studies have validated the accuracy of the NHIRD with regard to diagnoses of MI and stroke as well as mortality associated with these events21,22,23. After passing rigid expert review on rationale and privacy protection, the datasets are made available at the National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. The current study was conducted in compliance with the standards of the 1964 Declaration of Helsinki. The Chang Gung Medical Foundation Institutional Review Board approved this study and waived the need of informed consent because patient information had been delinked in the NHIRD (No. 104-2932B).
Study population and exposure
ESRD patients who were on maintenance hemodialysis and admitted with a principal diagnosis of AMI from July 2013 to December 2016 were identified in the NHIRD. This period was chosen because Taiwan's NHI program began to reimburse expenses for ticagrelor starting in July 2013. The diagnoses of ESRD and maintenance hemodialysis, defined at continuous hemodialysis for at least 3 months, were made by the catastrophic illness certificate issued by Taiwan's NHI program. AMI was identified according to the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes 410.x (July 1, 2013 to December 31, 2014) and ICD-10-CM diagnosis codes I21.x and I22.x (January 1, 2015 to December 31, 2015). Figure 1 illustrates patient enrollment. We excluded patients who did not have ESRD or required maintenance hemodialysis (n = 35,497). We also excluded patients who were less than 18 years of age (n = 35); had a duration of index hospitalization longer than 30 days (n = 5474); died on the same date of AMI admission (n = 928); had no records of outpatient follow-up (n = 1028); underwent coronary-artery bypass grafting (CABG; n = 3050); received fibrinolytic therapy (n = 616) or oral anticoagulation agents (n = 6567); and those who received no (n = 2325) or single antiplatelet agent (n = 5397) or switched between ticagrelor and clopidogrel (n = 5897) during hospitalization for AMI. A total of 2992 ESRD patients who were hospitalized for AMI and treated with DAPT were analyzed in this study. The patients who received aspirin and ticagrelor were defined as the ticagrelor group; the remaining patients who received aspirin and clopidogrel were defined as the clopidogrel group. The admission date for AMI was defined as the index date. Some patients switched between P2Y12 inhibitors or downgraded DAPT to single antiplatelet therapy for unknown reasons; therefore, any discontinuation of the original DAPT that was not related to clinical events was defined as an endpoint apart from clinical outcomes. All patients were followed up for 9 months or until the original DAPT was discontinued or clinical endpoints were reached, whichever came first. A 9-month follow-up was chosen because Taiwan's NHI program covers ticagrelor or clopidogrel treatment for 9 months, and we could not identify patients who paid for these drugs at their own expense beyond this period.
Covariates
Reimbursement claims for emergency, outpatient, and inpatient services were used to obtain patient demographics and clinical characteristics. A comorbid condition was defined as a discharge diagnosis or a diagnosis that was confirmed by two or more outpatient visits, based on the ICD-9-CM (before December 31, 2014) and ICD-10-CM diagnosis codes (after January 1, 2015) (Supplemental Table 1). Baseline medication use was defined as medications prescribed during hospitalization for AMI or within half a year before the index date. The use of medical devices and performance of interventional procedures were identified based on the ICD-9-CM and ICD-10-CM procedure codes or the Taiwan NHI reimbursement codes.
Outcome measures
The primary efficacy endpoint was defined as a composite of all-cause death, nonfatal MI, or nonfatal stroke at 9-month follow-up. The secondary efficacy endpoints included the individual components of the primary efficacy endpoint, with stroke further classified into ischemic and hemorrhagic. The safety endpoint was defined as Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding24. The diagnostic codes of the outcomes are listed in Supplemental Table 1. We excluded BARC type 1 bleeding (bleeding that is not actionable and does not require evaluation or treatment from a healthcare professional) because it could not be captured in the NHIRD. BARC type 4 (CABG-related) bleeding was also excluded according to the study design. Therefore, any bleeding extracted from the database would be BARC type 2, 3, or 5 bleeding. Since the database does not contain hemoglobin data, we modified the definition of BARC type 3 bleeding as bleeding requiring blood transfusion, intravenous vasoactive agents, or exploratory laparotomy; cardiac tamponade; intracranial hemorrhage; intraocular bleeding. Blood transfusion, intravenous vasoactive agents, and exploratory laparotomy were identified with the use of drug codes and procedure codes of the NHIRD. BARC type 5 bleeding was defined as bleeding being the principal diagnosis of admission with mortality within 7 days. BARC type 2 bleeding was defined as bleeding that did not fit the criteria for type 3 or 5 bleeding in this study. For the primary efficacy endpoint (a composite of all-cause death, nonfatal MI, or nonfatal stroke) and the safety endpoint (BARC type 2, 3, or 5), the numerator of the rate was the first event of a study outcome. All clinical outcomes had to be a discharge diagnosis to avoid misclassification. The follow-up period was from the index date to the first occurrence of any study outcome, up to 9 months, or discontinuation of DAPT, whichever came first.
Statistical analysis
Stabilized inverse probability of treatment weighting (IPTW) was used to balance baseline differences between the ticagrelor and clopidogrel groups25. The advantage of stabilized IPTW is that it provides an appropriate estimation of the variance of main effect and maintains an appropriate type I error by preserving the sample size of the original data. The propensity score, defined as the probability of a patient to receive ticagrelor for AMI treatment, was calculated using a generalized boosted model (GBM)26 that included all the covariates listed in Table 1. The GBM method gives the best performance in various scenarios (the model is additivity and linearity, mild non-additivity and nonlinearity, and moderate non-additivity and nonlinearity), and various weight trimming percentiles (from 50 to 100)27. A standardized mean difference of less than the absolute value of 0.1 was considered to be a negligible difference between the two groups after stabilized IPTW28. The incidence rates of clinical endpoints were expressed as the total number of events during the follow-up period divided by the person-months at risk. The risks of all-cause death were compared using the Cox proportional hazards model, with the clopidogrel group as the reference group. To account for the competing risk of death, the incidence rates of nonfatal, time-to-event outcomes (i.e., nonfatal MI, nonfatal stroke, and bleeding) were compared using the Fine and Gray subdistribution hazard model29. A p value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Ethics declarations
The Institutional Review Board of Chang Gung Medical Foundation approved this study (No. 104-2932B).
Results
From July 2013 to December 2016, a total of 2992 patients with ESRD on maintenance hemodialysis who were diagnosed with AMI were eligible for this study. Among these patients, 530 (17.7%) received ticagrelor and 2462 (82.3%) received clopidogrel (Table 1). Before stabilized IPTW, ticagrelor group patients were younger; more frequently presented with ST-elevation myocardial infarction (STEMI); received PCI or coronary stenting; and were treated with glycoprotein IIb/IIIa inhibitors, angiotensin-converting enzyme inhibitors, beta-blockers, and statins during hospitalization, whereas clopidogrel group patients were older and had higher rates of non-STEMI (NSTEMI), peripheral artery disease, and previous MI and bleeding events. There was no significant difference between the two treatment groups for the following factors: gender; underlying diseases, including diabetes, hypertension, dyslipidemia, heart failure, atrial fibrillation, or previous stroke; or the use of medications, including unfractionated or low-molecular-weight heparin, angiotensin II receptor blockers, or proton pump inhibitors. After stabilized IPTW, the two groups were well balanced for baseline characteristics.
Table 2 shows clinical outcomes after stabilized IPTW. During 9 months of follow-up, there was no significant difference in the incidence rates of primary efficacy endpoint between the two groups (ticagrelor vs. clopidogrel, 11.69 vs. 9.28 per 100 patient-months; subdistribution hazard ratio (SHR), 1.16; 95% confidence interval (CI), 0.97–1.4; p = 0.11). Between the two groups, incidence rates were comparable of all-cause death (9.31 vs. 7.22 per 100 patient-months; hazard ratio (HR), 1.17; 95% CI, 0.97–1.42; p = 0.11) and MI (1.58 vs. 1.50 per 100 patient-months; SHR, 0.96; 96% CI, 0.61–1.52; p = 0.86). Ticagrelor reduced the rate of stroke (0.19 vs. 0.67 per 100 patient-months; SHR, 0.25; 95% CI, 0.07–0.85; p = 0.03) after accounting for the competing risk of death, although the numbers of stroke events were small in both groups (4 and 55 in the ticagrelor and the clopidogrel groups, respectively).
With regard to safety outcomes, no significant difference was noted between the two groups regarding the risk of overall bleeding (5.55 vs. 4.36 per 100 patient-months; SHR, 1.14; 95% CI, 0.88–1.47; p = 0.33). Ticagrelor increased the rate of BARC type 2 bleeding compared with clopidogrel (4.55 vs. 3.34 per 100 patient-months; HR, 1.35; 95% CI, 1.01–1.81; p = 0.04), but the difference was no longer significant after taking the competing risk of death into account (SHR, 1.24; 95% CI, 0.93–1.65; p = 0.15). BARC type 3 or 5 bleeding risks were comparable between the two groups (1.0 vs. 1.02 per 100 patient-months; SHR, 0.86; 95% CI, 0.47–1.58; p = 0.63).
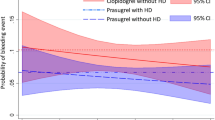
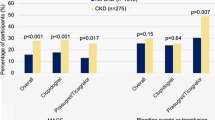
Figures 2 and 3 illustrate comparisons of the cumulative incidence rates of the efficacy and bleeding endpoints between the two study groups after stabilized IPTW, respectively. Most deaths and BARC type 3 or 5 bleeding occurred during the first month after AMI, whereas BARC type 2 bleeding, the most common type of bleeding, constantly increased over the follow-up period. Supplemental Table 2 lists the efficacy and bleeding endpoints before weighting.
Comparison of the cumulative incidence rates of (A) all-cause death, (B) nonfatal myocardial infarction, and (C) nonfatal stroke among end-stage renal disease patients with acute myocardial infarction treated between the ticagrelor and clopidogrel groups after stabilized inverse probability of treatment weighting.
Comparison of the cumulative incidence rates of (A) any bleeding, (B) BARC type 2, and (C) BARC type 3 or 5 bleeding among end-stage renal disease patients with acute myocardial infarction treated between the ticagrelor and clopidogrel groups after stabilized inverse probability of treatment weighting. BARC Bleeding Academic Research Consortium.
Discussion
This retrospective nationwide cohort study compared clinical outcomes after ticagrelor versus clopidogrel in combination with aspirin for the treatment of ESRD patients who were diagnosed with AMI. The principal findings of this study are as follows: (1) ticagrelor was comparable to clopidogrel regarding the primary composite outcome of all-cause death, non-fatal MI, or non-fatal stroke; and (2) ticagrelor did not significantly increase the risk of bleeding after accounting for the competing risk of death.
Post hoc analyses of studies evaluating the addition of clopidogrel to aspirin have shown divergent results in the CKD population, with reduced or lack of effect observed with clopidogrel versus placebo15,30,31. Clopidogrel resistance, or HPR under clopidogrel therapy, has been recognized to be one of the plausible explanations for increased cardiovascular events in these patients. The prevalence of HPR in the ESRD population is even higher, reaching up to 60% to 80%32,33. Therefore, some physicians may consider more effective platelet-inhibiting strategies for selected ESRD patients at high risk for ischemic and thrombotic events. As shown in patients with normal17 and impaired kidney function34, ticagrelor exhibits potent antiplatelet effects and fast onset of action in those on dialysis compared with clopidogrel, with a prevalence of HPR ranging from 10 to 47%35,36. Even though evidence is lacking and bleeding remains a concern, the impetus to prescribe ticagrelor to ESRD patients may be due in part to the remarkable outcomes of the CKD subgroup in the PLATO trial. In a sub-analysis of the PLATO study, ticagrelor was associated with a 4.0% absolute and 28% relative risk reduction of all-cause mortality in CKD patients, and the mortality benefit was even greater in patients with advanced CKD19. Consistent with the overall PLATO population, the incidence of non–CABG-related major bleeding was higher in the ticagrelor group than in the clopidogrel group, but this difference did not increase in the CKD cohort. A Swedish database study supported the advantage of ticagrelor in CKD for the real-world treatment of AMI37. Across all strata of estimated glomerular filtration rates (eGFRs) in this study, ticagrelor reduced ischemic events but increased bleeding compared with clopidogrel. Notably, ticagrelor was associated with mortality reduction in patients with normal or mildly reduced eGFR, but this benefit was attenuated among those with eGFR < 30 ml/min/m2 (HR, 1.08; 95% CI, 0.70–1.49), with a significant interaction between eGFR and ticagrelor (p for interaction = 0.04). The lack of mortality benefit with ticagrelor across the eGFR spectrum may be due to an increased risk of bleeding (HR, 1.79; 95% CI, 1.00–3.21) in patients with eGFR < 30 ml/min/m2 compared with those with higher eGFR levels (HR 1.1 and 1.13 for eGFR > 60 ml/min/m2 and 30–60 ml/min/m2, respectively). Severe CKD (eGFR < 30 ml/min/m2) is a major criterion for high bleeding risk in the consensus of Academic Research Consortium for High Bleeding Risk38. One possible explanation for incremental bleeding associated with worsening CKD is reduced clearance of antithrombotic drugs. Given the adverse impact of bleeding on mortality39,40, increased bleeding with ticagrelor therapy may eventually offset its anti-ischemic efficacy as kidney function deteriorates to severe CKD.
In the present study, ticagrelor was comparable to clopidogrel regarding the composite endpoint of all-cause death, MI, or stroke in patients with ESRD. This finding is consistent with the results of our recent study in a general AMI population in Taiwan41. Growing evidence shows that the risk–benefit ratio for antithrombotic therapy may be different between Caucasians and East Asians. Two prospective randomized controlled trials conducted in East Asian patients, the PHILO42 and the TICAKOREA studies43, did not reproduce the superiority of ticagrelor over clopidogrel in the PLATO study. Ticagrelor was even associated with a higher incidence of clinically significant bleeding in the TICAKOREA study. Despite the high prevalence of clopidogrel hypo-responsiveness among East Asian patients44, a higher bleeding risk and a lower ischemic risk have been observed in East Asians who are on DAPT after PCI than in Caucasians, a phenomenon commonly referred to as the “East Asian paradox”45. As mentioned above, the results of ticagrelor in treating patients with normal or less advanced CKD may not be extrapolated to dialysis patients. As kidney function deteriorates to ESRD, comorbid burden, traditional and nontraditional uremic risk factors, and dialysis-related factors may not only contribute to mortality in these patient but also have a complex interaction with antiplatelet therapy4,46. Potential benefits of ischemic reduction with potent platelet inhibition may have been counterbalanced by increased bleeding risk, leading to an overall neutral impact on mortality in our study.
The superiority of ticagrelor over clopidogrel for MI reduction in the PLATO trial was not seen in our ESRD cohort. In the aforementioned Swedish study, the point estimates for MI indicated a lower risk for ticagrelor compared with clopidogrel in all eGFR strata, except in patients with eGFR < 30 ml/min/m2, where the CI was wide and crossed the line of unity. These results suggest that the benefit of preventing subsequent MI with ticagrelor may be attenuated as kidney function progressively declines. Evidence has suggested that ticagrelor could be potentially beneficial for stroke prevention in patients with cardiac or cerebrovascular diseases47,48. However, we could not draw a conclusion on whether this benefit exists in patients with ESRD, since the stroke events were far less than deaths or bleeding in this study. Further studies are needed to evaluate the role of ticagrelor in stroke prevention in these patients.
The risk of major bleeding in patients with ESRD is estimated to be 20-fold higher than in patients with normal kidney function49. Although bleeding definitions and follow-up duration differ between studies, we noted a remarkably high risk of severe (BARC type 3 or 5) bleeding in our ESRD patients (12% per person-years) compared to the risk of BARC type ≥ 3 bleeding in a general, stable CAD population treated with antiplatelet therapy for secondary prevention (0.6% per person-years) or the risk of major bleeding in patients receiving DAPT after PCI (0.4% to 0.8% per person-years)50,51. In fact, the majority of our patients may have had a PRECISE-DAPT sore of ≥ 25 (old age, impaired renal function, heighted inflammatory state during AMI, and a high prevalence of anemia or prior bleeding), indicating a high risk for bleeding52,53. To avoid bleeding, a short duration of DAPT is generally recommended for these patients. However, a significant portion of our patients received off-label use of ticagrelor (17.7%), suggesting the concerns over high thrombotic risk following AMI. A US registry study reported contraindicated use of antithrombotic agents in 22% of dialysis patients undergoing PCI, leading to an increased risk of major bleeding among these patients54. In our study, the risk of overall bleeding or BARC type 2 bleeding associated with ticagrelor was attenuated after taking the competing risk of death into account. Since we excluded the patients who were prescribed no or single antiplatelet therapy (presumably judged as having high bleeding tendency by physicians), we might have selected a population with a relatively low risk of bleeding. This may have skewed the bleeding outcomes in favor of ticagrelor in our study.
In a retrospective study using the United States Renal Data System, Mavrakanas et al. analyzed the outcomes of P2Y12 inhibitors in dialysis patients who received DES and were alive at 90 days after stenting55. They found that both prasugrel and ticagrelor were comparable to clopidogrel with respect to ischemic outcomes but were associated with a numerically higher incidence of clinically relevant bleeding. Li et al. also used the NHIRD of Taiwan to compared ticagrelor versus clopidogrel in treating dialysis patients with acute coronary syndrome in the same time frame as our study56. They found that ticagrelor was associated with higher risks of MACE and major bleeding compared with clopidogrel. Different enrollment criteria and definitions of clinical endpoints may account for the different results between the two studies. Li et al. excluded the patients who died within 30 days of acute coronary syndrome or received P2Y12 inhibitors before the index event, leading to a smaller sample size and a relatively low atherosclerotic burden (13% of patients with underlying coronary artery disease and 3% with peripheral artery disease) and bleeding tendency (3% with prior bleeding) in their study population compared with ours. The concomitant use of parenteral antithrombotic agents (unfractionated or low-molecular-weight heparin and glycoprotein IIb/IIIa inhibitors) may have confounded the comparative outcomes between ticagrelor versus clopidogrel but was not taken into account in the study of Li et al. Furthermore, major studies on antiplatelet therapy in patients with acute coronary syndrome have shown a rapid surge in the clinical events during the early period of follow-up18,57. Excluding death in the first 30 days in the study of Li et al. makes it difficult to interpret the results. Therefore, our study may be more representative of the real-world treatment of dialysis patients with AMI.
Limitations
This retrospective database analysis has several inherent limitations. Our study results may have been subject to selection bias. Physicians may have conceivably prescribed ticagrelor to patients with high risk for ischemic events and a low risk for bleeding. However, their exact reasons for choosing between ticagrelor and clopidogrel are not listed in the database. Another source of selection bias in this study is that only the patients who received, or potentially could tolerate, DAPT were enrolled. To mitigate potential differences in baseline bleeding risk, we incorporated past history of bleeding among other covariates as a proxy of bleeding tendency in stabilized IPTW. Certain factors that may have contributed to outcome differences, including the duration and adequacy of dialysis, parameters of CKD-related mineral and bone disorder such as parathyroid hormone, calcium, and phosphate58, left ventricular ejection fraction, levels of troponin and hemoglobin, and coronary angiographic findings, were not included in this database analysis. Although we included all the demographic and clinical variables and concomitant medications for stabilized IPTW, we could not mitigate unknown or unmeasured confounding between the study groups. The lack of laboratory data hindered us from calculating the bleeding scores to weigh the trade-off between ischemic and bleeding risks with ticagrelor treatment in this high-risk population. We also could not differentiate between silent bleeding and anemia due to ESRD in this study. Clinical outcomes were identified based on the ICD-9-CM and ICD-10-CM diagnosis codes without adjudication. Although outcomes like mortality, MI, or stroke have been validated in the NHIRD of Taiwan, how the risk of ascertainment bias may have affected the study results was unknown. The lack of causes of deaths in the database impeded a detailed comparison of cardiac and noncardiac deaths between the study groups. We did not analyze BARC types 3 and 5 bleeding separately or classify stroke into ischemic and hemorrhagic subtypes because of the small numbers of these individual events. Adverse effects like dyspnea or bradyarrhythmias related to inhibition of adenosine uptake by ticagrelor could not be addressed with certainty in this database study. In substudies of PLATO, ticagrelor did not affect pulmonary function, and bradycardia or ventricular pauses related to ticagrelor were predominantly asymptomatic and of no apparent clinical consequence59,60. However, we cannot fully recognize the clinical impact of these adverse events in patients with ESRD. Lastly, our results could only be applied to East Asian populations and should be validated with prospective randomized trials.
In conclusion, among patients with ESRD who underwent hemodialysis and received DAPT for AMI, ticagrelor was comparable to clopidogrel with regard to the composite endpoint of all-cause death, MI, or stroke. Ticagrelor did not significantly increase the risk of bleeding compared with clopidogrel in hemodialysis patients. Our findings suggest an altered risk–benefit ratio for ticagrelor when kidney function deteriorates from less advanced CKD to ESRD.
Data availability
Data are available from the National Health Insurance Research Database (NHIRD) published by Taiwan National Health Insurance (NHI) Bureau. Due to legal restrictions imposed by the government of Taiwan in relation to the “Personal Information Protection Act”, data cannot be made publicly available.
References
Schiffrin, E. L., Lipman, M. L. & Mann, J. F. Chronic kidney disease: Effects on the cardiovascular system. Circulation 116(1), 85–97 (2007).
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C.-Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 351(13), 1296–1305 (2004).
Go, A. S. et al. Chronic kidney disease and risk for presenting with acute myocardial infarction versus stable exertional angina in adults with coronary heart disease. J. Am. Coll. Cardiol. 58(15), 1600–1607 (2011).
Stenvinkel, P., Pecoits-Filho, R. & Lindholm, B. Coronary artery disease in end-stage renal disease: No longer a simple plumbing problem. J. Am. Soc. Nephrol. 14(7), 1927–1939 (2003).
Fox, C. S. et al. Use of evidence-based therapies in short-term outcomes of ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction in patients with chronic kidney disease: A report from the national cardiovascular data acute coronary treatment and intervention outcomes network registry. Circulation 121(3), 357–365 (2010).
Herzog, C. A., Ma, J. Z. & Collins, A. J. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N. Engl. Med. 339(12), 799–805 (1998).
Müller, I. et al. Prevalence of clopidogrel non-responders among patients with stable angina pectoris scheduled for elective coronary stent placement. Thromb. Haemost. 89(05), 783–787 (2003).
Angiolillo, D. J. et al. Variability in individual responsiveness to clopidogrel: Clinical implications, management, and future perspectives. J. Am. Coll. Cardiol. 49(14), 1505–1516 (2007).
Tantry, U. S. et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J. Am. Coll. Cardiol. 62(24), 2261–2273 (2013).
Gurbel, P. A. et al. Clopidogrel effect on platelet reactivity in patients with stent thrombosis: Results of the CREST Study. J. Am. Coll. Cardiol. 46(10), 1827–1832 (2005).
Buonamici, P. et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J. Am. Coll. Cardiol. 49(24), 2312–2317 (2007).
Stone, G. W. et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): A prospective multicentre registry study. Lancet 382(9892), 614–623 (2013).
Cuisset, T. et al. High post-treatment platelet reactivity identified low-responders to dual antiplatelet therapy at increased risk of recurrent cardiovascular events after stenting for acute coronary syndrome. J. Thromb. Haemost. 4(3), 542–549 (2006).
Gremmel, T. et al. Chronic kidney disease is associated with increased platelet activation and poor response to antiplatelet therapy. Nephrol. Dial. Transpl. 28(8), 2116–2122 (2013).
Best, P. J. et al. The efficacy and safety of short-and long-term dual antiplatelet therapy in patients with mild or moderate chronic kidney disease: Results from the clopidogrel for the reduction of events during observation (CREDO) trial. Am. Heart J. 155(4), 687–693 (2008).
Htun, P. et al. Low responsiveness to clopidogrel increases risk among CKD patients undergoing coronary intervention. J. Am. Soc. Nephrol. 22(4), 627–633 (2011).
Gurbel, P. et al. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: The ONSET/OFFSET study. Circulation 120(25), 2577 (2009).
Wallentin, L. et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 361(11), 1045–1057 (2009).
James, S. et al. Ticagrelor versus clopidogrel in acute coronary syndromes in relation to renal function: Results from the platelet inhibition and patient outcomes (PLATO) trial. Circulation 122(11), 1056–1067 (2010).
Hsieh, C.-Y. et al. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 11, 349 (2019).
Cheng, C.-L. et al. Validation of acute myocardial infarction cases in the national health insurance research database in Taiwan. J. Epidemiol. 24(6), 500–507 (2014).
Cheng, C. L., Kao, Y. H. Y., Lin, S. J., Lee, C. H. & Lai, M. L. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 20(3), 236–242 (2011).
Cheng, C.-L., Chien, H.-C., Lee, C.-H., Lin, S.-J. & Yang, Y.-H.K. Validity of in-hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance research database in Taiwan. Int. J. Cardiol. 201, 96–101 (2015).
Mehran, R. et al. Standardized bleeding definitions for cardiovascular clinical trials. Circulation 123(23), 2736–2747 (2011).
Xu, S. et al. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health 13(2), 273–277 (2010).
McCaffrey, D. F. et al. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat. Med. 32(19), 3388–3414 (2013).
Lee, B. K., Lessler, J. & Stuart, E. A. Weight trimming and propensity score weighting. PLoS ONE 6(3), e18174 (2011).
Austin, P. C. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun. Stat.-Simul. C 38(6), 1228–1234 (2009).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94(446), 496–509 (1999).
Keltai, M. et al. Renal function and outcomes in acute coronary syndrome: Impact of clopidogrel. Eur. J. Cardiovasc. Prev. Rehabil. 14(2), 312–318 (2007).
Dasgupta, A. et al. Clinical outcomes of patients with diabetic nephropathy randomized to clopidogrel plus aspirin versus aspirin alone (a post hoc analysis of the clopidogrel for high atherothrombotic risk and ischemic stabilization, management, and avoidance [CHARISMA] trial). Am. J. Cardiol. 103(10), 1359–1363 (2009).
Alexopoulos, D. et al. Prevalence of inadequate platelet inhibition by clopidogrel in patients receiving hemodialysis. Am. J. Kidney Dis. 59(3), 469–471 (2012).
Ohno, Y. et al. High residual platelet reactivity after switching from clopidogrel to low-dose prasugrel in Japanese patients with end-stage renal disease on hemodialysis. J. Cardiol. 73(1), 51–57 (2019).
Butler, K. & Teng, R. Pharmacokinetics, pharmacodynamics, and safety of ticagrelor in volunteers with severe renal impairment. J. Clin. Pharmacol. 52(9), 1388–1398 (2012).
Alexopoulos, D. et al. Ticagrelor in clopidogrel-resistant patients undergoing maintenance hemodialysis. Am. J. Kidney Dis. 60(2), 332–333 (2012).
Jeong, K. H. et al. Platelet reactivity after receiving clopidogrel compared with ticagrelor in patients with kidney failure treated with hemodialysis: A randomized crossover study. Am. J. Kidney Dis. 65(6), 916–924 (2015).
Edfors, R. et al. Outcomes in patients treated with ticagrelor versus clopidogrel after acute myocardial infarction stratified by renal function. Heart 104(19), 1575–1582 (2018).
Urban, P. et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: A consensus document from the Academic Research Consortium for high bleeding risk. Eur. Heart J. 40(31), 2632–2653 (2019).
Doyle, B. J., Rihal, C. S., Gastineau, D. A. & Holmes, D. R. Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: Implications for contemporary practice. J. Am. Coll. Cardiol. 53(22), 2019–2027 (2009).
Mehran, R. et al. Impact of bleeding on mortality after percutaneous coronary intervention: Results from a patient-level pooled analysis of the REPLACE-2 (randomized evaluation of PCI linking angiomax to reduced clinical events), ACUITY (acute catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc. Interv. 4(6), 654–664 (2011).
Chang, C. J. et al. Efficacy and safety of ticagrelor vs. clopidogrel in East Asian patients with acute myocardial infarction: A nationwide cohort study. Clin. Pharmacol. Ther. 109(2), 443–451 (2021).
Goto, S., Huang, C.-H., Park, S.-J., Emanuelsson, H. & Kimura, T. Ticagrelor vs. clopidogrel in Japanese, Korean and Taiwanese patients with acute coronary syndrome–randomized, double-blind, phase III PHILO study. Circ. J. 79(11), 2452–2460 (2015).
Park, D.-W. et al. Clinically significant bleeding with ticagrelor versus clopidogrel in Korean patients with acute coronary syndromes intended for invasive management: A randomized clinical trial. Circulation 140(23), 1865–1877 (2019).
Pan, Y. et al. Genetic polymorphisms and clopidogrel efficacy for acute ischemic stroke or transient ischemic attack: A systematic review and meta-analysis. Circulation 135(1), 21–33 (2017).
Jeong, Y.-H. “East asian paradox”: Challenge for the current antiplatelet strategy of “one-guideline-fits-all races” in acute coronary syndrome. Curr. Cardiol. Rep. 16(5), 485 (2014).
Ganesh, S. K., Hulbert-Shearon, T., Port, F. K., Eagle, K. & Stack, A. G. Mortality differences by dialysis modality among incident ESRD patients with and without coronary artery disease. J. Am. Soc. Nephrol. 14(2), 415–424 (2003).
Bonaca, M. P. et al. Prevention of stroke with ticagrelor in patients with prior myocardial infarction: Insights from PEGASUS-TIMI 54 (prevention of cardiovascular events in patients with prior heart attack using ticagrelor compared to placebo on a background of aspirin-thrombolysis in myocardial infarction 54). Circulation 134(12), 861–871 (2016).
Malhotra, K. et al. Ticagrelor for stroke prevention in patients with vascular risk factors: A systematic review and meta-analysis. J. Neurol. Sci. 390, 212–218 (2018).
Molnar, A. O. et al. The risk of major hemorrhage with CKD. J. Am. Soc. Nephrol. 27(9), 2825–2832 (2016).
Hamon, M. et al. Incidence, source, determinants, and prognostic impact of major bleeding in outpatients with stable coronary artery disease. J. Am. Coll. Cardiol. 64(14), 1430–1436 (2014).
Giustino, G. et al. Efficacy and safety of dual antiplatelet therapy after complex PCI. J. Am. Coll. Cardiol. 68(17), 1851–1864 (2016).
Costa, F. et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: A pooled analysis of individual-patient datasets from clinical trials. Lancet 389(10073), 1025–1034 (2017).
Covic, A. et al. Practical issues in clinical scenarios involving CKD patients requiring antithrombotic therapy in light of the 2017 ESC guideline recommendations. BMC Med. 16(1), 1–11 (2018).
Tsai, T. T. et al. Contraindicated medication use in dialysis patients undergoing percutaneous coronary intervention. JAMA 302(22), 2458–2464 (2009).
Mavrakanas, T. A., Kamal, O. & Charytan, D. M. Prasugrel and ticagrelor in patients with drug-eluting stents and kidney failure. Clin. J. Am. Soc. Nephrol. 16(5), 757–764 (2021).
Li, Y. S., Wang, S. H., Hwang, S. J., Yang, Y. H. & Hsieh, K. P. Comparison of effectiveness and safety between ticagrelor and clopidogrel in patients with acute coronary syndrome and on dialysis in Taiwan. Br. J. Clin. Pharmacol. (2021).
Wiviott, S. D. et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Med. 357(20), 2001–2015 (2007).
Block, G. A., Kilpatrick, R. D., Lowe, K. A., Wang, W. & Danese, M. D. CKD–mineral and bone disorder and risk of death and cardiovascular hospitalization in patients on hemodialysis. Clin. J. Am. Soc. Nephrol. 8(12), 2132–2140 (2013).
Storey, R. F. et al. Pulmonary function in patients with acute coronary syndrome treated with ticagrelor or clopidogrel (from the platelet inhibition and patient outcomes [PLATO] pulmonary function substudy). Am. J. Cardiol. 108(11), 1542–1546 (2011).
Scirica, B. M. et al. The incidence of bradyarrhythmias and clinical bradyarrhythmic events in patients with acute coronary syndromes treated with ticagrelor or clopidogrel in the PLATO (platelet inhibition and patient outcomes) trial: Results of the continuous electrocardiographic assessment substudy. J. Am. Coll. Cardiol. 57(19), 1908–1916 (2011).
Funding
This study was partially supported by Chang Gung Memorial Hospital, Taiwan (Grant CMRPG3J0621, CMRPG3K0051, CLRPG3D0046).
Author information
Authors and Affiliations
Contributions
Research idea and study design: Y.C.T., C.J.C.; data acquisition: J.R.L., S.H.C.; statistical analysis: J.R.L., S.H.C., L.C.S.; data interpretation: Y.C.T., C.J.C., J.R.L., S.H.C., Y.H.C., C.T.K., L.C.S.; supervision/mentorship: C.J.C., Y.H.C., C.T.K., L.C.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tung, YC., Chang, CJ., Liu, JR. et al. Outcomes after ticagrelor versus clopidogrel treatment in end-stage renal disease patients with acute myocardial infarction: a nationwide cohort study. Sci Rep 11, 20826 (2021). https://doi.org/10.1038/s41598-021-00360-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-00360-0
- Springer Nature Limited
This article is cited by
-
Ticagrelor or Clopidogrel as Antiplatelet Agents in Patients with Chronic Kidney Disease and Cardiovascular Disease: A Meta-analysis
American Journal of Cardiovascular Drugs (2023)