Abstract
The objective of this study was to evaluate a novel microstream method by comparison with PaCO2 and the more standard mainstream capnometer in intubated pediatric patients. We hypothesized that the novel microstream method would superior compared to the traditional mainstream method in predicting PaCO2. This was a prospective single-center comparative study. The study was carried out on 174 subjects with a total of 1338 values for each method. Data were collected prospectively from mainstream and microstream capnometer simultaneously and compared with PaCO2 results. Although both mainstream PetCO2 (mainPetCO2) and microstream PetCO2 (microPetCO2) were moderately correlated (r = 0.63 and r = 0.68, respectively) with PaCO2 values, mainPetCO2 was in better agreement with PaCO2 in all subjects (bias ± precision values of 3.8 ± 8.9 and 7.3 ± 8.2 mmHg, respectively). In those with severe pulmonary disease, the mainPetCO2 and microPetCO2 methods were highly correlated with PaCO2 (r = 0.80 and r = 0.81, respectively); however, the biases of both methods increased (14.8 ± 9.1 mmHg and 16.2 ± 9.0 mmHg, respectively). In cases with increased physiologic dead space ventilation, the agreement levels of mainPetCO2 and microPetCO2 methods became distorted (bias ± precision values of 20.9 ± 11.2 and 25.0 ± 11.8 mm Hg, respectively) even though mainPetCO2 and microPetCO2 were highly correlated (r = 0.78 and r = 0.78, respectively). It was found that the novel microstream capnometer method for PetCO2 measurements provided no superiority to the traditional mainstream method. Both capnometer methods may be useful in predicting the trend of PaCO2 due to significant correlations with the gold standard measurement in cases with severe pulmonary disease or increased physiological dead space –despite reduced accuracy.
Similar content being viewed by others
Introduction
The monitoring of carbon dioxide (CO2) level is essential for diagnosis and therapeutic guidance in mechanically ventilated patients1. The current gold standard method for the measurement of partial pressure of carbon dioxide in the blood (PaCO2) is the arterial blood gas (ABG) method. But ABG is an invasive method and does not provide continuous monitoring2.
Capnometers, which continuously monitor PCO2 levels and display the waveform of PCO2 in exhaled air non-invasively, provide information on the adequacy of ventilation3. Detection of exhaled PCO2 (end-tidal PCO2) has proven to be a valuable mechanism to confirm tracheal intubation and to recognize accidental esophageal intubations, among other critical patient safety benefits4. The patient protection enhancements provided by end-tidal PCO2 (PetCO2) monitoring also include the detection of invasive airway disconnection, dislodgement or obstruction, prediction of underlying airway or lung pathologies and monitoring the effectiveness of cardiopulmonary resuscitation3,5,6.
It is possible to measure PetCO2 by mainstream or sidestream capnometer technologies. The technique is named based on the localization of the PetCO2 sensor7,8. Mainstream capnometers are devices in which the infrared source and PCO2 detector are placed between the proximal endotracheal tube (ETT) and the ventilator circuit7,9. On the other hand, sidestream capnometers aspirate samples from the airway through tubing attached to a sampling line and airway adapter between the ETT and the ventilation circuit. Sidestream methods utilize an infrared PCO2 sensor in a monitor that may be located far from the patients10. A new technology for sidestream systems (Microstream, Oridion Medical, Inc., Danville, CA) is now available that uses very low flow rates (50 mL/min) to preserve the accuracy and resolution of the waveform as well as eliminating secretion/moisture-related occlusion problems by the use of special filters7.
There are many studies evaluating the accuracy of mainstream, sidestream and microstream capnometer technologies in the literature11,12,13,14,15. Critics of capnometer usage cite multiple studies which demonstrate that PetCO2 and PaCO2 do not reliably correlate in some clinical situations12,16,17. The analyses utilized in these studies are highly variable and fail to consider physiologic dead space/severity of pulmonary disease and/or their effect on the relationship between PaCO2 and PetCO2. Additionally, there are few studies that have compared different PetCO2 monitoring techniques with each other18,19,20,21.
This study was undertaken to evaluate the correlations of gold standard PaCO2 measurements with the microstream and mainstream PetCO2 capnometers, and to compare the accuracy and results of the latter two methods among ventilated patients in the pediatric intensive care unit (PICU). We hypothesize that, (i) in intubated pediatric patients, the microstream technology will allow better prediction of PaCO2 compared to the traditional mainstream method, and that (ii) microstream measurements predict PaCO2 more reliably than mainstream measurements across increased levels of dead space ventilation and in the presence of severe pulmonary disease—after controlling for the expected PetCO2-PaCO2 gradient.
Methods
This prospective, single-center comparative study was conducted at the PICU of Medeniyet University, Goztepe Training and Research Hospital (Istanbul, Turkey) between January 2018 and July 2019. All procedures and processes were carried out according to principles mentioned in the Helsinki Declaration and the Good Clinical Practice guideline.
Population
The study evaluated all children aged between 1 month to 17 years that had been intubated with cuffed ETT due to a definite indication for mechanical ventilation. Among these, those who accepted invasive monitoring of arterial blood pressure and provided informed consent (parents or legal guardians) were included in the study. The presence of any one of the following characteristics was defined as grounds for exclusion from the study: patients with tracheostomy, sampling performed with venous blood, non-compliance to study protocol (premature discontinuation of measurement, signal abnormality [absence of waveform or presence of interrupted waveform]), use of uncuffed endotracheal tubes, patients with known congenital heart and lung defects, need for high-frequency oscillatory ventilation or extracorporeal life support, determination of any type of air leakage in the lung (pneumothorax, pneumomediastinum etc.).
Monitoring
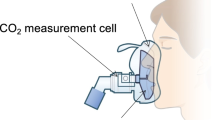
The intubations were performed with single-lumen cuffed ETT that was appropriately sized for age and weight. CO2 in the exhaled air of patients was monitored simultaneously with mainstream (Mainstream EtCO2; Philips Capnostat M25O1A, Germany) and microstream (Microstream EtCO2; Medtronic Capnostream35, USA) capnometers. The dimensions of the airway adapters to be used were based on the manufacturer's guidelines. The airway adaptors of both methods of measurements were kept in the same location and insertions were performed sequentially between the airway circuit and the proximal ETT. ABG were analyzed at the bedside using an ABL 90 FLEX blood gas analyzer (Radiometer, Medical ApS, Copenhagen, Denmark) within 3 min of collection and without any delay. No additional ABG was performed for the data collection of consecutive samples.
Study protocol and recording
ABG analysis, mainPetCO2 and microPetCO2 values and mechanical ventilator parameters were recorded simultaneously. Prior to obtaining each arterial blood gas sample, a researcher checked whether the capnometer adapters were blocked by secretions or moisture. Capnometer adapters were replaced with new ones in the event of any type of blockage. Both capnometer methods were analyzed using continuous steady waveforms of expired CO2 through the ventilator cycle, in order to ensure the accuracy of readings. A minimum of 4 and a maximum of 8 simultaneous PCO2 measurements (PaCO2, mainPetCO2, microPetCO2) were planned to be taken from each patient. Patients with a measurement number less than 4 for various reasons (death, extubation, interruption of monitoring etc.) were excluded from the study.
Patients’ demographic characteristics and their clinical and laboratory parameters were identified (gender, age [months] and primary diagnosis). The parameters of mechanical ventilation, including FiO2 (Fractional inspired oxygen), mean airway pressure (MAP) were recorded in addition to PetCO2 values (mainPetCO2 and microPetCO2), parameters of arterial blood gas analysis (pH, PaCO2, PaO2, HCO3ˉ) and oxygenation index (OI) (OI = [FiO2 × MAP × 100)/PaO2])22. Lung physiologic dead space volume is defined as wasted tidal volume during respiration (i.e., the volume remaining in the conducting airways [anatomical dead space] and in poorly perfused and non-perfused alveoli [alveolar dead space] that are not participating in gas exchange). A ratio of dead space volume to tidal volume (Vd/Vt) was calculated using the Enghoff modification of the Bohr equation: Vd/Vt = [PaCO2 − PetCO2]/PaCO223. Dead space ventilation was calculated separately using PetCO2 values obtained from microstream and mainstream methods.
For subgroup analyses, patients were grouped with regard to the severity of pulmonary disease and physiological dead space ventilation levels. Severe pulmonary disease was defined as an OI of ≥ 10 and mild-to-moderate pulmonary disease was defined as an OI of < 1018,24. Determination of Vd/Vt ratio ≥ 0.4 was defined as increased dead space ventilation23,25. The consistency of PetCO2 monitoring (mainPetCO2 and microPetCO2) within each patient and subgroup was assessed by examining the relationships between the changes in PaCO2 and the two PetCO2 methods in consecutive samples.
Statistical analysis
Analyses were performed by using the IBM Statistical Package for the Social Sciences version 21 (SPSS, Inc., Chicago, IL) or Med Calc version 19.1 (Med Calc Software, Ostend, Belgium). Patient characteristics are described using qualitative variables (using frequencies and percentages) and quantitative variables (using means and standard deviation [SD] or median with interquartile range [IQR], depending on type of distribution). Simple linear regression analysis was performed and Spearman correlation coefficients were calculated for the assessment of relationships between PaCO2, main-PetCO2 and micro-PetCO2. We assessed the agreement between these measurements (bias [mean difference] and precision [SD of the differences]) by the Bland–Altman technique. The results were considered statistically significant in tests resulting in a P value lower than 0.05.
Power analysis
Power analysis was conducted using the Power Analysis Sample Size (PASS) for Windows version 11.0 Package Program. Group sample sizes of 174 were determined to achieve 97% power to detect a difference of − 3.6 between the null hypothesis that both group means were 3.8, and the alternative hypothesis that the mean of group 2 was 7.4 (with estimated group standard deviations of 9.0 and 8.3), and with a significance level (alpha) of 0.05 using a two-sided two-sample t-test.
Ethics approval and consent to participate
The study was approved by the institutional review board of our center. The parents of all patients signed an informed consent form before inclusion into the study.
Conference presentation
This study presented at the 15th National Congress of Pediatric Emergency and Critical Care, 18–20 October 2018, Turkey.
Results
The study was performed in 174 patients that provided 1338 measurements for each method. The median age and interquartile range (IQR) of the included subjects was 42 months (IQR: 12–108 mo.). Table 1 shows the characteristics of the study group. Conventional invasive mechanical ventilator modes were used in all patients included in the study (Galileo Mechanical Ventilator, Hamilton Medical AG, Rhäzüns, Switzerland).
The median (range) levels of PaCO2, mainPetCO2, and microPetCO2 were 40.7 (IQR: 35.4–47.3) mm Hg, 38.0 (IQR: 32.0–44.0) mm Hg, and 35.0 (IQR: 29.0–40.0) mm Hg, respectively. The results of the Bland–Altman analysis comparing mainPetCO2/PaCO2 and microPetCO2/PaCO2 pairs are summarized in Table 2 and illustrated in Fig. 1 in all subject groups—and also according to severity of pulmonary disease. In all subjects (1338 pairs), the mean difference (bias) and SD of the differences (precision) for mainPetCO2 was 3.8 ± 8.9 mm Hg (95% limits of agreement -13.7 to 21.4 mm Hg) with moderate correlation (r = 0.63, p < 0.001) (Fig. 1A). The mean bias and precision for microPetCO2 was 7.3 ± 8.2 mm Hg (95% limits of agreement − 8.8 to 23.6 mm Hg) with moderate correlation (r = 0.68, p < 0.001) (Fig. 1B). Although both PetCO2 measurement methods were moderately correlated, mainPetCO2 was more accurate compared to the microPetCO2 method overall (in the whole subject group). Additionally, when we evaluated the correlation between mainPetCO2 and microPetCO2 throughout all patients, the methods demonstrated a strong level of correlation (r = 0.84, p < 0.001) (Fig. 2).
Bland–Altman plots for mean mainPetCO2 versus PaCO2 (A) and mean microPetCO2 versus PaCO2 (B) for all patients, mainPetCO2 and PaCO2 for the patients with mild to moderate pulmonary disease (C), microPetCO2 and PaCO2 for the patients with mild to moderate pulmonary disease (D), mainPetCO2 and PaCO2 for the patients with severe pulmonary disease (E), microPetCO2 and PaCO2 for the patients with severe pulmonary disease (F). The mean difference is represented as a continuous line, and 95% limits of agreement are represented as dotted lines.
Study subjects were also compared based on the presence of lung pathology (Table 2). In the mild-to-moderate pulmonary disease group, 1242 measurements from each end-tidal CO2 method were compared. In this group, the mean bias and precision for mainPetCO2 was 2.9 ± 8.4 mm Hg (95% limits of agreement − 13.4 to 19.4 mm Hg) with moderate correlation (r = 0.64, p < 0.001) (Fig. 1C). The mean bias and precision for microPetCO2 was 6.7 ± 7.8 mm Hg (95% limits of agreement − 8.5 to 22.1 mm Hg) with moderate correlation (r = 0.68, p < 0.001) (Fig. 1D). Although both PetCO2 measurement methods were moderately correlated, mainPetCO2 was more accurate than microPetCO2.
In the severe lung disease group, we compared 96 results from each method of measurement. For the mainPetCO2 and PaCO2 comparison, the mean bias and precision was 14.8 ± 9.1 (95% limits of agreement − 3.0 to 32.7 mm Hg) (Fig. 1E). Whereas the mean bias and precision between microPetCO2 and PaCO2 was 16.2 ± 9.0 mm Hg (95% limits of agreement − 1.4 to 33.9 mm Hg) (Fig. 1F). In the severe lung disease group, almost all PaCO2 values were higher than PetCO2 measurements (Fig. 1E,F). Additionally, in this group, both mainPetCO2 and microPetCO2 were highly correlated with PaCO2 (r = 0.80, p < 0.001 and r = 0.81, p < 0.001, respectively); however, the biases of both methods increased.
To determine whether the accuracy of the non-invasive PCO2 measurement methods were altered in the presence of high physiologic dead space, we compared the mainPetCO2 and microPetCO2 values with regard to groups formed according to Vd/Vt ratio (< 0.4 vs. ≥ 0.4). The Vd/Vt ratio was < to 0.4 in 1247 of 1338 (93%), and > 0.4 in 91 (7%) measurements.
In the Vd/Vt < 0.4 (the normal physiologic dead space) group, the comparison of mainPetCO2 and PaCO2 values showed a mean bias and precision of 3.0 ± 8.0 mm Hg, with moderate correlation (r = 0.63, p < 0.001). Whereas the mean bias and precision between microPetCO2 and PaCO2 was 6.5 ± 7.0 mm Hg, again with moderate correlation (r = 0.68, p < 0.001). In the Vd/Vt ≥ 0.4 (increased physiologic dead space) group, both mainPetCO2 and microPetCO2 were highly correlated (r = 0.78, p < 0.001 and r = 0.78, p < 0.001, respectively) with increased PetCO2—PaCO2 gradient (bias ± precision values of 20.9 ± 11.2 and 25.02 ± 11.8 mm Hg, respectively). Although both non-invasive PCO2 measurement methods were highly correlated with PaCO2, mainPetCO2 was more accurate than microPetCO2 in both the normal and increased dead space ventilation groups.
Discussion
To our knowledge, this is the largest cohort study including 174 pediatric patients who received mechanical ventilation in the PICU. The evaluation of 1338 measurements for each method and the comparison of two different PetCO2 monitoring methods with accuracy determined according to simultaneous PaCO2 measurements are among the other strengths of this study. Although different PetCO2 measurement methods have distinct advantages, the accuracy and correlation of these methods in comparison to ABG measurements is without doubt the most vital feature of any method. The microstream capnometer requires in-depth analysis to prove that it contributes to or surpasses available methods by analyzing whether the advantageous properties expressed in the literature are indeed superior in the real-life follow-up of intubated pediatric patients.
Although there are many studies evaluating the accuracy and correlation of various non-invasive PetCO2 measurement methods, the majority of these studies were performed in non-intubated patient groups26,27,28,29,30. In intubated patients, the studies on PetCO2 monitoring are mostly compared with the ABG analysis of a single method and often evaluate the relationship between the severity of lung disease and the accuracy of the method. In our study, two different PetCO2 monitoring methods were evaluated simultaneously, and both mainPetCO2 and microPetCO2 measurements were found to be moderately correlated with PaCO2.
Rozycki et al. reported that mainPetCO2 measurements were highly correlated with PaCO2 in intubated newborns, with a mean bias of -6.9 mm Hg13. Similar results have been found in other studies using the mainstream technology in intubated newborns31,32. Microstream is preferred especially in the neonatal age group due to the use of very low flow rates (50 mL/min), causing smaller dead space and allowing measurement from the distal part of the ETT. In the study by Kugelman et al.24 microPetCO2 was found in adequate agreement with PaCO2, which indicated closer agreement than seen in the current research. Although similar ‘close’ results have been obtained in other studies18,33, Singh and colleagues found similar results to ours in terms of agreement between microPetCO2 and PaCO215. In intubated patients, PetCO2 measurements can be performed from the proximal or distal part of the ETT. To compare the advantages of different PetCO2 measurement technologies in our study, it was thought that the measurements obtained from the same locations would be more guiding. Therefore, in order for one of the methods to gain no advantage due to localization, both PetCO2 measurements were obtained from the same location (proximal part of ETT). In various studies comparing PetCO2 measurements obtained from the distal and proximal parts of the ETT, it has been suggested that distal measurements provide more accurate results; however, several other studies have demonstrated comparable accuracy between proximal and distal measurements21,33,34,35.
The first study comparing two different PetCO2 measurement methods in intubated patients was performed by Kugelman and colleagues. This study, which was comprised of 27 infants, showed better correlation between PetCO2 and PaCO2 with distal sampling of expired air using microstream technology against the mainstream method through a proximal port using double lumen ETT18. The measurements made in this study were obtained from different locations of the ETT and this situation may have led to an advantage for the microstream method. In our study, although the correlation coefficients of both methods were similar, the agreement level of main PetCO2 measurements was better.
There are various studies investigating the relationships between pulmonary disease and PaCO2-PetCO2 values. These studies have defined pulmonary disease severity according to various parameters, such as OI, arterial-alveolar PO2 gradient and PaO2/FiO2 ratio. In this study we used the OI value to define severe pulmonary disease. Sivan et al. reported in their study that mainPetCO2 and PaCO2 compatibility decreased as lung disease severity increased in neonatal patients36. Hagerty et al. evaluated the compatibility of microPetCO2 and PaCO2 in intubated newborn patients and found that microPetCO2 and PaCO2 differences were higher in the pulmonary disease group compared to controls33. Different results were reported by other investigators. Tingay et al.37 found that the PetCO2 bias was independent of severity of lung disease and similarly Rozycki et al.13 reported that the degree of lung disease had little influence on the degree of discrepancy between measurement. Kugelman and colleagues reported that although the accuracy of microPetCO2 decreased with lung disease it still remained good correlation as a useful measure of PaCO2 in conditions of severe lung disease18. The study by McDonald et al. found an overall moderately correlation between PaCO2 and mainPetCO2 for all included patients, but the investigators concluded that significant lung disease (defined by PaO2/FiO2 < 200) had a negative effect on the correlation12. In our study, it was concluded that both PetCO2 measurement methods highly correlated in patients with severe lung disease, albeit with a significant decrease in measurement accuracy.
The most important parameter contributing to the PetCO2-PaCO2 gradient is the increase in physiological dead space due to ventilation-perfusion mismatch38,39. Physiologic dead space ventilation is the sum of anatomical dead space from the conducting airways and alveolar dead space from disease processes and/or therapies employed. The increased gradient between PetCO2 and PaCO2 with high PaCO2 levels are directly proportional to the degree of physiologic dead space. Although typical alveolar CO2 concentrations are slightly greater than of ABG, PetCO2 normally 2–5 mmHg lower than PaCO2 due to mixing of CO2 containing alveolar gas with exhaled gas devoid of CO2 from the anatomical dead space. In a patient with lung disease, the addition of alveolar dead space further dilutes PetCO2 relative to PaCO2. As a result, PetCO2 measurements depict greatly reduced results compared to PaCO2. The normal physiologic dead space to tidal volume ratio (Vd/Vt) is established to be 0.20–0.3523. In this study, we provide evidence that physiologic dead space ventilation is a major factor in determining the relationship between capnographic monitoring of PetCO2 and PaCO2. Despite multiple earlier publications comparing PetCO2 and PCO2 in presence of pulmonary disease and hypercarbia, few studies have examined the effect of change in physiologic dead space on the relationship between PetCO2 and PaCO2 across an increased range of Vd/Vt ratios in mechanically ventilated pediatric patients23. Our study is the first to investigate the correlations between two different capnometers in patients with increased physiological dead space ventilation.
In patients with a low calculated physiologic dead space to tidal volume ratio (Vd/Vt < 0.4), there is a moderate correlation between both PetCO2 (measured noninvasively by capnography) measurements and PaCO2 value. Despite the high correlation between PetCO2 and PaCO2 values in patients with high physiologic dead space to tidal volume ratio (Vd/Vt ≥ 0.4), the accuracy of measurements was greatly reduced. Therefore, in the presence of severe pulmonary diseases with increased physiological dead space, it is much more reliable to use PetCO2 results as a measure of trend rather than absolute value. It is also critical to note that further problems in accuracy may arise with smaller infants or newborns (which were not included in the study population) and reduced volumes or I:E values. In a study including 56 intubated pediatric patients by McSwain et al., it was found that, while the strength of the association diminished slightly as the dead space ratio increased, the correlation still remained strong between the methods. The PaCO2-PetCO2 gradient was increased predictably with increasing Vd/Vt23. Our findings show that increased physiological dead space as a result of severe pulmonary disease will increase the gradient between PaCO2 and PetCO2 in favor of PaCO2 values, making almost all PaCO2 results greater than those recorded by PetCO2. These findings were similar to the outcomes of previous studies performed in newborns and children with pulmonary disease33,36.
To our knowledge, there are no other studies investigating the relationships between PetCO2 measurements and increased physiological dead space ventilation. There are however, various studies investigating PetCO2 correlations with hypercarbia as a proxy for increased dead space ventilation. In the study conducted by Kugelman et al., microPetCO2 was reported as a useful measure of PaCO2, whereas mainPetCO2 was distorted on the high range of PaCO2 level18. Rosycki et al.13 did not find any effect of increased PaCO2 on mainPetCO2 measurements.
Our study has several limitations. Non-consecutive ABGs were used for data collection and inadvertent selection bias may have been introduced. In our study, we used proximal measurement method for both PetCO2 methods. In subsequent studies, the relationship between concurrent microPetCO2 measurements obtained from the proximal and distal part of the ETT may reveal differences in results which could be crucial for physicians and patients in intensive care units. Although our study reached the highest number of patients and samples in the literature, the number of samples in the subgroups of severe pulmonary disease and increased physiologic dead space ventilation, were relatively low; thus limiting the generalizability of those results. Due to the low number of patients with ARDS, we could not group patients as mild, moderate, severe ARDS with regard to the criteria put forth by the Pediatric Acute Lung Injury Consensus Conference (PALICC); thus, subgroup analyses concerning these groups could not be performed. Also, the number of cases with increased physiologic dead space (Vd/Vt ≥ 0.4) was low, leading to a lack of further subgroup analysis.
Conclusion
It was found that the novel microstream capnometer has no superiority to the traditional mainstream method. Although the mainstream and microstream capnometer measurements had similar correlation values with ABG results, the agreement level of the mainstream method was higher. Although the absolute gradient between both PetCO2 methods and PaCO2 results demonstrated a consistent increase in the presence of severe pulmonary disease and increased dead space ventilation, both methods showed significant correlations with PaCO2 values. Therefore, in the presence of severe pulmonary disease and/or increased dead space ventilation, it is possible that both PetCO2 monitoring methods may be helpful in predicting the trend of PaCO2 despite limitations in accuracy.
Abbreviations
- CO2 :
-
Carbon dioxide
- ABG:
-
Arterial blood gas
- PICU:
-
Pediatric intensive care unit
- MAP:
-
Mean airway pressure
- OI:
-
Oxygenation index
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- PASS:
-
Power analysis sample size
References
Huttmann, S. E., Windisch, W. & Storre, J. H. Techniques for the measurement and monitoring of carbon dioxide in the blood. Ann. Am. Thorac. Soc. 11, 645–652 (2014).
Tobias, J. D. Transcutaneous carbon dioxide monitoring in infants and children. Pediatric Anesthesia 19, 434–444 (2009).
Bhende, M. End-tidal carbon dioxide monitoring in pediatrics-clinical applications. J. Postgrad. Med. 47, 215 (2001).
Wyllie, J. & Carlo, W. A. The role of carbon dioxide detectors for confirmation of endotracheal tube position. Clin. Perinatol. 33, 111–119 (2006).
Siobal, M. S. Monitoring exhaled carbon dioxide. Respir. Care 61, 1397–1416 (2016).
Whitaker, D. Time for capnography–everywhere. Anaesthesia 66, 544–549 (2011).
Bhende, M. Capnography in the pediatric emergency department. Pediatr. Emerg. Care 15, 64–69 (1999).
Ward, K. R. & Yealy, D. M. End-tidal carbon dioxide monitoring in emergency medicine, part 1: basic principles. Acad. Emerg. Med. 5, 628–636 (1998).
Nobel, J. J. Carbon dioxide monitors: exhaled gas (capnographs, capnometers, end-tidal CO2 monitors). Pediatr. Emerg. Care 9, 244–246 (1993).
Bhende, M. S. & Lacovey, D. C. End-tidal carbon dioxide monitoring in the prehospital setting. Prehosp. Emerg. Care 5, 208–213 (2001).
Trevisanuto, D. et al. End-tidal carbon dioxide monitoring in very low birth weight infants: correlation and agreement with arterial carbon dioxide. Pediatr. Pulmonol. 47, 367–372 (2012).
Mcdonald, M. J. et al. Comparison of end-tidal CO2 and PaCO2 in children receiving mechanical ventilation. Pediatr. Crit. Care Med. 3, 244–249 (2002).
Rozycki, H. J. et al. Mainstream end-tidal carbon dioxide monitoring in the neonatal intensive care unit. Pediatrics 101, 648–653 (1998).
Wu, C. H. et al. Good estimation of arterial carbon dioxide by end-tidal carbon dioxide monitoring in the neonatal intensive care unit. Pediatr. Pulmonol. 35, 292–295 (2003).
Singh, B. S., Gilbert, U., Singh, S. & Govindaswami, B. Sidestream microstream end tidal carbon dioxide measurements and blood gas correlations in neonatal intensive care unit. Pediatr. Pulmonol. 48, 250–256 (2013).
Russell, G. B. & Graybeal, J. M. Reliability of the arterial to end-tidal carbon dioxide gradient in mechanically ventilated patients with multisystem trauma. J. Trauma 36, 317–322 (1994).
Short, J., Paris, S., Booker, P. & Fletcher, R. Arterial to end-tidal carbon dioxide tension difference in children with congenital heart disease. Br. J. Anaesth. 86, 349–353 (2001).
Kugelman, A. et al. A novel method of distal end-tidal CO2 capnography in intubated infants: comparison with arterial CO2 and with proximal mainstream end-tidal CO2. Pediatrics 122, e1219–e1224 (2008).
Pascucci, R. C., Schena, J. A. & Thompson, J. E. Comparison of a sidestream and mainstream capnometer in infants. Crit. Care Med. 17, 560–562 (1989).
Chan, K., Chan, M. & Gin, T. Mainstream vs. sidestream capnometry for prediction of arterial carbon dioxide tension during supine craniotomy. Anaesthesia 58, 149–155 (2003).
Mcevedy, B. A. et al. End-tidal carbon dioxide measurements in critically ill neonates: a comparison of side-stream and mainstream capnometers. Can. J. Anaesth. 37, 322 (1990).
Group PaLICC. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr. Crit. Care Med. J. Soc. Crit. Care Med. World Fed. Pediatr. Intens. Crit. Care Soc. 16, 428 (2015).
Mcswain, S. D. et al. End-tidal and arterial carbon dioxide measurements correlate across all levels of physiologic dead space. Respir. Care 55, 288–293 (2010).
Kugelman, A. et al. Impact of continuous capnography in ventilated neonates: a randomized, multicenter study. J. Pediatr. 168, 56–61 (2016).
Kallet, R. H., Alonso, J. A., Pittet, J.-F. & Matthay, M. A. Prognostic value of the pulmonary dead-space fraction during the first 6 days of acute respiratory distress syndrome. Respir. Care 49, 1008–1014 (2004).
Howe, T. A. et al. The use of end-tidal capnography to monitor non-intubated patients presenting with acute exacerbation of asthma in the emergency department. J. Emerg. Med. 41, 581–589 (2011).
Kartal, M. et al. The value of ETCO2 measurement for COPD patients in the emergency department. Eur. J. Emerg. Med. 18, 9–12 (2011).
Barten, C. W. & Wang, E. S. Correlation of end-tidal CO2 measurements to arterial PaCO2 in nonintubated patients. Ann. Emerg. Med. 23, 560–563 (1994).
Plewa, M. C. et al. Evaluation of capnography in nonintubated emergency department patients with respiratory distress. Acad. Emerg. Med. 2, 901–908 (1995).
Casati, A. et al. End tidal carbon dioxide monitoring in spontaneously breathing, nonintubated patients. A clinical comparison between conventional sidestream and microstream capnometers. Minerva Anestesiol. 67, 161–164 (2001).
Bhat, Y. R. & Abhishek, N. Mainstream end-tidal carbon dioxide monitoring in ventilated neonates. Singap. Med. J. 49, 199 (2008).
Singh, S. A. & Singhal, N. Does end-tidal carbon dioxide measurement correlate with arterial carbon dioxide in extremely low birth weight infants in the first week of life?. Indian Pediatr. 43, 20 (2006).
Hagerty, J. J. et al. Accuracy of a new low-flow sidestream capnography technology in newborns: a pilot study. J. Perinatol. 22, 219–225 (2002).
Badgwell, J., Mcleod, M., Lerman, J. & Creighton, R. End-tidal PCO2 measurements sampled at the distal and proximal ends of the endotracheal tube in infants and children. Anesth. Analg. 66, 959–964 (1987).
Mcevedy, B. A. et al. End-tidal, transcutaneous, and arterial pCO2 measurements in critically ill neonates: a comparative study. Anesthesiology 69, 112–116 (1988).
Sivan, Y., Eldadah, M. K., Cheah, T. E. & Newth, C. J. Estimation of arterial carbon dioxide by end-tidal and transcutaneous PCO2 measurements in ventilated children. Pediatr. Pulmonol. 12, 153–157 (1992).
Tingay, D. G., Stewart, M. J. & Morley, C. J. Monitoring of end tidal carbon dioxide and transcutaneous carbon dioxide during neonatal transport. Arch. Dis. Childh. Fetal Neonatal Ed. 90, F523–F526 (2005).
Burrows, F. A. Physiologic dead space, venous admixture, and the arterial to end-tidal carbon dioxide difference in infants and children undergoing cardiac surgery. Anesthesiol. J. Am. Soc. Anesthesiol. 70, 219–225 (1989).
Fletcher, R. The arterial-end-tidal CO2 difference during cardiothoracic surgery. J. Cardiothorac. Anesth. 4, 105–117 (1990).
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. D.M.: study design, statistical analysis, drafted the manuscript, and is responsible for the overall content. D.B.A.: Study design, data extraction and quality assessment. K.Z.: Contributed to the writing of the manuscript and revised the manuscript for important intellectual content. B.M.: Data extraction and quality assessment. G.A.: Data extraction and quality assessment. M.C.Y.: Data extraction and quality assessment. Y.M.N.: Data extraction. B.O.: Data extraction.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duyu, M., Bektas, A.D., Karakaya, Z. et al. Comparing the novel microstream and the traditional mainstream method of end-tidal CO2 monitoring with respect to PaCO2 as gold standard in intubated critically ill children. Sci Rep 10, 22042 (2020). https://doi.org/10.1038/s41598-020-79054-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-79054-y
- Springer Nature Limited
This article is cited by
-
Novel approaches to capturing and using continuous cardiorespiratory physiological data in hospitalized children
Pediatric Research (2023)
-
Non-invasive carbon dioxide monitoring in neonates: methods, benefits, and pitfalls
Journal of Perinatology (2021)