Abstract
Few reports have discussed appropriate strategies for patient referrals to advanced heart failure (HF) centers with available left ventricular assist devices (LVADs). We examined the association between the characteristics and prognoses of referred patients with advanced HF and the bed volume of the referring hospitals. This retrospective analysis evaluated 186 patients with advanced HF referred to our center for consultation about the indication of LVAD between January 1, 2015, and August 31, 2018. We divided the patients into two groups according to the bed volume of their referring hospital (high bed volume hospitals (HBHs): ≥ 500 beds in the hospital; low bed volume hospitals (LBHs): < 500 beds). We compared the primary outcome measure, a composite of LVAD implantation and all-cause death, between the patients referred from HBHs and patients referred from LBHs. The 186 patients with advanced HF referred to our hospital, who were referred from 130 hospitals (87 from LBHs and 99 from HBHs), had a mean age of 43.0 ± 12.6 years and a median left ventricular ejection fraction of 22% [15–33%]. The median follow-up duration of the patients was 583 days (119–965 days), and the primary outcome occurred during follow-up in 42 patients (43%) in the HBH group and 20 patients (23%) in the LBH group. Patients referred from HBHs tended to require catecholamine infusion on transfer more often than those referred from LBLs (36.5% (HBH), 20.2% (LBL), P = 0.021). Kaplan–Meier analysis indicates that the occurrence of the primary outcome was significantly higher in the HBH patients than in the LBH patients (log-rank P = 0.0022). Multivariate Cox proportional hazards analysis revealed that catecholamine support on transfer and long disease duration were statistically significant predictors of the primary outcome. Patients from HBHs had a greater risk of the primary outcome. However, the multivariate analysis did not indicate an association between referral from an HBH and the primary outcome. In contrast, catecholamine support on transfer, long duration of disease, and low blood pressure were independent predictors of the primary outcome. Therefore, these should be considered when determining the timing of a referral to an advanced HF center, irrespective of the bed volume of the referring hospital.
Similar content being viewed by others
Introduction
In industrialized countries1, heart failure (HF) affects 0.4–2.2% of the population and is related to poor quality of life and high mortality rates. HF is also associated with various dysfunctions, leading to enormous financial burdens on the healthcare system2,3. In industrialized countries, the incidence of HF is increasing as the average life expectancy increases, and the HF pandemic era is imminent4. Furthermore, there are some juvenile cases of medically intractable HF, which is another important issue in medical care for HF5. There is an unmet need for the proper allocation of advanced HF therapy in conditions of limited medical resources.
Treatment strategies for advanced HF include a wide range of medical and surgical therapies6. These include heart transplantation (HTx) and left ventricular assist device (LVAD) implantation, which have been reported to significantly improve quality of life and survival rates in advanced HF7. However, these therapies have limited availability; for example, LVAD implantation is performed only as a bridge to transplantation in Japan, and HTx can be performed only after a long waiting period using LVAD support8. In addition, these therapies have not been generalized and can be only performed in limited, specialized facilities. Delays in referrals to specialized facilities for these interventions affect the prognosis and quality of life of patients, as well as the economies of the countries in which they live9.
In regard to the indication of LVAD or HTx for advanced HF, the patient should be transferred or referred to specialized facilities that provide these interventions. However, these patient-transfer pathways are wide-ranged and complex. Few reports have investigated the characteristics of patient transfer for considerations of LVAD or HTx.
Therefore, this study aimed to examine the characteristics of patient referrals to LVAD and HTx centers from clinics, community hospitals, and university hospitals to assess the determining factors for the post-transfer clinical course of advanced HF. It is possible that the criteria of transfer might be different in various hospital sizes. In stratifying the referral hospitals in this study, we focused on the bed volume of the hospital. Indeed, there are several reports suggesting that hospital bed volume has some degree of impact on the post-transfer clinical course of patients with advanced HF10,11. We investigated the different characteristics of referred patients with advanced HF according to the bed volume of the referring hospital.
Methods
Study protocol
The University of Tokyo Hospital is an approved HTx facility and has performed approximately 15–20 HTx procedures annually. This facility also performs LVAD surgery, making it the most active center for these interventions within the Kanto area, which is located in the north central region of the main island of Japan and is approximately 30,000 km2. In this study, we recruited consecutive patients who were referred to our hospital for advanced HF with consideration of the indication for an advanced intervention, including LVAD and HTx, between January 1, 2015, and August 31, 2018.
The exclusion criteria are as follows: age greater than 65 years (because there is no indication for transplantation in these patients), age less than 18 years, hospital transfer for an already-planned LVAD operation, and diagnosis of diseases other than HF that could cause volume overload, such as end-stage renal disease requiring hemodialysis and severe liver disease. We excluded patients with ischemic heart disease and patients with severe valve disease, if they could be improved by the treatment for each complication, such as coronary or valve interventions. We also excluded patients who were consulted from only documents due to a lack of information. The diagnosis of HF was confirmed if HF was diagnosed as the primary admitting diagnosis by the documented physical examination and laboratory and radiologic findings. The study protocol conformed to the tenets of the Declaration of Helsinki and was reviewed and approved by the institutional review board at the University of Tokyo (approval number: 2650). Informed consent was obtained from all patients, in accordance with the protocol approved by ethics committee.
Follow-up
In this study, follow-up examinations were completed on December 31, 2019. The patients’ survival was followed up from the date of patient transfer until death or HTx. We also evaluated the date of implantable LVAD operation, survival with LVAD implantation, and survival without LVAD implantation. The median follow-up duration was 583 (119–965) days. The primary outcome was a composite of implantable LVAD implantation and all-cause death. We also examined all-cause death inclusive of deaths after LVAD implantation as a secondary outcome. None of the patients included in this study underwent HTx without implantable LVAD implantation. The implantation of extracorporeal LVAD was not counted as an event, but we evaluated it as a bridging intervention toward implantable LVAD. In addition, the indication of LVAD was determined by an advanced HF therapeutics team including cardiologists, a surgeon, nurses, and a transplant coordinator. Timing of the LVAD implantation was determined by whether the patient developed a progressive decline in end-organ function despite receiving the maximal treatment.
Data collection
Patient characteristics, including medications, were collected at the time of transfer. The beta-blocker dose at baseline was standardized into bisoprolol equivalents12, and the loop diuretic dose was standardized into furosemide equivalents13, both of which were analyzed as continuous variables. The duration of the disease was defined as the time from the date of the first onset of HF symptoms according to the medical charts to the time of transfer. For the laboratory data, fasting blood samples were collected at the time of patient transfer, and the laboratory data were assessed using standard laboratory methods at the University of Tokyo Hospital. We examined the most recent transthoracic echocardiography data available around the time of transfer. “Direct transfer” means that hospitalized patients in other hospitals were transferred and admitted into our hospital directly. We also examined the status of the patient during direct transfer, and this assessment included statuses of “with catecholamine infusion,” “with intra-aortic balloon pumping (IABP),” and “with extracorporeal membrane oxygenation (ECMO).” The data generated and analyzed in the current study are not publicly available but are available from the corresponding author on reasonable request.
Statistical analysis
Data are presented as the mean ± standard deviation or as the median (interquartile range). The statistical analysis was performed using JMP version Pro 14. Student’s t-test or the Mann–Whitney U test was used to compare continuous variables, and Fisher’s exact test was used to compare categorical variables. Log-rank tests using the Kaplan–Meier estimator were performed to determine the survival rate of the patients, in which time zero was set as the time of transfer. The level of significance was set to 5%, and all reported P values and confidence intervals (CIs) were calculated as two-sided. The cutoff value of each variable for the hazard analysis was calculated using a receiver operating characteristic curve. We chose values that maximized the sum of sensitivity and specificity as the cutoff values to calculate the area under the curve. According to the analysis of risk factors for the primary outcome, a multivariate Cox proportional hazards analysis including the factor of hospital bed volume was performed using a backward selection procedure. Of note, a forward selection procedure resulted in the same selection of independent parameters. According to the analysis of risk factors for the secondary outcome, multivariate Cox proportional hazards analysis was performed using a backward selection procedure. A forward selection procedure resulted in the same results.
Results
Baseline characteristics
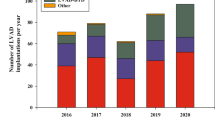
A total of 186 patients with advanced HF were assessed in this analysis after 33 patients were excluded according to the excluding criteria (Fig. 1). Figure 2 shows the number of hospital beds for the hospitals from which the advanced HF patients were transferred to our center. The median number of hospital beds was 504. The mean age of the included advanced HF patients was 43.0 ± 12.6 years; 72.0% of the patients were male; 67.2% of the patients had dilated cardiomyopathy; the median (25th percentile to 75th percentile) left ventricular ejection fraction (LVEF) of the patients was 22% (15–33%); and 24.6% of the patients were classified as New York Heart Association (NYHA) functional class II, whereas 75.4% were NYHA functional class III or IV. Beta-blockers were taken by 73.4% of the patients, angiotensin-modulating agents by 62.0%, and mineralocorticoid receptor antagonists by 61.4%. Furthermore, 22.2% had an implantable cardioverter defibrillator/cardiac resynchronization therapy defibrillator (ICD/CRTD). A total of 38% of the patients were directly transferred to our hospital, 73.2% of whom received a continuous infusion of catecholamine; additionally, 28.1% received IABP, and 18.3% received ECMO. Regarding the implantation of an extracorporeal LVAD, 11 patients had extracorporeal LVAD as a bridging therapy toward the explanation of it (N = 3) or implantable LVAD implantation (N = 4).
Differences in patient characteristics between the HBH and LBH groups
Next, we divided the patients into two groups based on the bed volume of the hospital from which they were referred: the high bed volume hospital (HBH, ≥ 500 beds) group and low bed volume hospital (LBH, < 500 beds) group. We compared the baseline characteristics between the patients referred from LBHs and the patients referred from HBHs (Table 1).
This study included patients referred from 70 LBHs (62% of these hospitals have their own coronary care unit) and 60 HBHs (100% of these hospitals have their own coronary care unit). The percentage of university hospitals was significantly different between the two groups (6% (LBHs) vs. 58% (HBHs)). The median age of the patients was 45.0 [36.0–53.0] years (LBHs) versus 44.0 [35.0–52.0] years (HBHs) (P = 0.60), and 73.6% (LBHs) vs 70.7% (HBHs) of the patients were male (P = 0.74). There were no significant differences in the etiologies of HF and previous medical histories of the patients between the two groups. In contrast, there were significant differences in the albumin levels (4.1 [3.6–4.4] g/dL (LBHs) vs. 3.9 [3.4–4.2] g/dL (HBHs); P = 0.037) and hemoglobin levels (14.2 ± 2.1 g/dL (LBHs) vs. 13.2 ± 2.2 g/dL (HBHs); P = 0.0015), which are surrogate markers of nutritional state, of the patients between the two groups. The duration of diagnosed HF was longer in the patients from HBHs than in patients from LBHs (350 [61–2635] days (LBHs) vs. 1658 [89–4223] days (HBHs); P = 0.041). Furthermore, there was a higher proportion of patients who had an ICD/CRTD from HBHs than those from LBHs (11.5% (LBHs) vs. 31.6% (HBHs); P = 0.0013). According to the transfer, catecholamine infusion (20.2% (LBHs) vs. 36.5% (HBHs); P = 0.0012), IABP (3.6% (LBHs) vs. 17.7% (HBHs); P = 0.0020), and ECMO (2.4% (LBHs) vs. 11.3% (HBHs); P = 0.018) were observed more frequently in the patients from HBHs. There were no significant differences in the rate of medication with other than statins for patients between the two groups (28.6% (LBHs) vs. 14.4% (HBHs); P = 0.028). Interestingly, no differences in echocardiographic parameters were observed between the LBHs and HBHs.
Clinical course after patient transfer
During the duration of follow-up in this study, there were 12 deaths among the patients (three after extracorporeal LVAD implantation and nine who did not undergo LVAD implantation) and 50 patients who underwent LVAD implantation. We also detected death in one patient after implantable LVAD implantation.
We investigated the impact of hospital bed volume on event occurrence of the primary outcome. The results show that the patients from HBHs had a higher occurrence of the primary outcome during follow-up than did the patients from LBHs (Kaplan–Meier log-rank P = 0.0022) (Fig. 3a). However, there was no significant difference in survival rate between these two groups (Fig. 3b).
(a) Differences in event-free survival curves of the primary outcome measures, including LVAD implantation and death, between patients referred from HBHs and patients referred from LBHs. (b) Differences in event-free survival curves of the secondary outcome measures between patients referred from HBHs and patients referred from LBHs. LVAD, left ventricular assist device; LBHs, low bed volume hospitals; HBHs, high bed volume hospitals.
Critical factors that affected the primary and secondary outcomes
Next, we performed monovariate and multivariate Cox proportional hazards analyses to determine the factors affecting the primary outcome, focusing on the impact of bed volume of the referring hospital (Table 2).
Monovariate analysis indicated that the patients referred from HBHs had a higher risk of the primary event compared to the patients from LBHs. During transfer, catecholamine infusion had the greatest impact on the primary outcome of all other factors, and this was also exemplified in the survival curve analysis (Fig. 4a). However, neither the IABP nor ECMO resulted in a higher risk for the primary outcome. Additionally, systolic blood pressure, LVEF on echocardiography, lymphocyte count, and the levels of albumin, alanine aminotransferase, total cholesterol, brain natriuretic peptide (BNP), sodium, and hemoglobin corresponded to varying risks for the primary event. The multivariate analysis indicated that catecholamine infusion, HF duration, low systolic blood pressure, ICD/CRTD, and alanine aminotransferase elevation corresponded to a significantly higher risk for outcomes occurring in the future. However, the difference in hospital bed volume between the two groups lost statistical significance in predicting the primary outcome after the multivariate analysis was performed. We also analyzed the predictive factors of all-cause death (secondary outcome), which demonstrated that catecholamine infusion during transfer was a statistically significant predictor of secondary outcomes (Table 3). The Kaplan–Meier analysis demonstrated that there was a higher risk of all-cause death in the group with catecholamine infusion during transfer than those without catecholamine infusion during transfer (Fig. 4b).
(a) Differences in event-free survival curves of the primary outcome measures, including LVAD implantation and death, between patients with and patients without catecholamine infusion during transfer. (b) Differences in event-free survival curves of the secondary outcome measures between patients with and patients without catecholamine infusion during transfer. LVAD, left ventricular assist device.
Discussion
The patients in this study cohort, more than one-quarter of whom were dependent on catecholamine infusion at the time of transfer, were younger and had higher severities of HF compared to the patients of other research studies on HF14,15,16. Georgiopoulou et al. analyzed a cohort of patients with HF referred for transplant evaluation who were slightly older and who had less severe HF compared to the patients in our study17. In our study, the patients from HBHs tended to have a poorer nutritional status and higher rate of catecholamine infusion during transfer than the patients from LBHs. In addition, an ICD or CRTD implantation was frequently performed before transfer for the patients from HBHs in our study. As a result, the patients from HBHs had a higher risk of experiencing the primary outcome, which was a composite of LVAD implantation and all-cause death. However, HBHs and the occurrence of the primary outcome did not show a statistically significant correlation in the multivariate analysis.
There are no established criteria for referral to specialized affiliations capable of performing LVAD or HTx. Therefore, the timing of referral to these specialized affiliations has been varied and wide-ranging. Indeed, a delay in referral can lead to a poorer prognosis in HF patients9. Therefore, investigating the appropriate timing for referral is imperative for improving the prognosis of advanced HF patients.
Approximately 10 centers in the Kanto area, which is 30,000 km2 and is located around Tokyo, perform LVAD interventions. The medical centers in this area are concentrated mainly around Tokyo compared with other sections, which suggests that the Kanto area is unevenly distributed compared with other areas in Japan. The patients transferred to our hospital usually came from hospitals in the Kanto area. This study included 186 patients with advanced HF from 116 hospitals, 50 of which have 500 beds or more and 66 of which have fewer than 500 beds.
We focused on the bed volume of hospitals in this study. However, hospitals also can be classified according to the hospital site (urban or rural), type of hospital facility, and funding background. The use of bed volume as a surrogate for hospital facility might be the simplest and easiest classification method, and we addressed the bed volume of hospitals classification in the analysis of the current study. There are several reports that demonstrated an association between hospital bed volume and clinical course of patients10,11, which might somewhat suggest the validity of this method. The cutoff value of 500 was calculated using the median of the referral hospital (504) in this study, and it corresponds to the criteria for large hospitals (500 beds) according to guidelines set by the American Hospital Association18. In contrast, another important measure that might reflect the scale of hospital is the “annual count of patients with a specific disease.” Indeed, several reports have demonstrated an association between HBH status and low mortality rate, and this trend is enhanced in patients who underwent major surgeries and cardiovascular procedures19,20,21. In addition, Kumbhani et al. demonstrated a weak association between HBH status and lower risk of short-term mortality in patients with HF22. However, our study analyzes referred patients, which do not have the same meaning as hospitalized patients in the referrer hospital, and there are few reports that have analyzed the association between referred patients and the referring hospital. We also compared the occurrence rates of the primary outcome and secondary outcome after classifying the hospitals into university hospitals and others or urban and rural hospitals (Supplementary Fig. 1, 2). However, these stratifications did not effectively classify patients with low and high risks.
According to the medication management for the patients, there were no significant differences in the medications taken for HF between the patients from the HBHs and patients from the LBHs, which is a result that is consistent with the results of previous studies23. In contrast, the finding that there was a large difference in the use of device therapies, such as CRTD and ICD, between the HBHs and LBHs suggests that hospitals with greater experience provide more advanced procedures.
The patient eligibility assessment for selecting patients with LVAD or HTx generally includes cardiopulmonary exercise testing, a comprehensive risk score, an evaluation of end-stage organ failure, and data on right heart catheterization24. Cardiopulmonary exercise testing can be performed only when patients are in a stable condition, so this evaluation was not useful for our cohort. In addition, there are several simple strategies for selecting suitable candidates for HTx or LVAD therapy without utilizing these data and measures. Thorvaldsen et al. demonstrated that risk factors such as low systolic blood pressure, renal dysfunction, anemia, and medication status can efficiently predict HTx/LVAD candidacy potential25. The study by Kagogeropoulos, which included patients with HF severities most similar to those in the current study, demonstrated that progression of HF to stage D is associated with a lower LVEF, lower blood pressure, and renal and hepatic dysfunction26. The BNP levels of patients in the present study likely reflect the effects of invasive and noninvasive treatments. This measure may be substantially affected by the timing of these treatments, which lessens the utility of this parameter27.
Some reports have noted that being referred to a HF center too late corresponds with a poor prognosis9. However, there was no significant difference in the survival rate between patients transferred from HBHs and those transferred from LBHs in this study. Indeed, the patients from HBHs had a longer disease history than did those from LBHs. Therefore, it is likely that the patients from HBHs endured a longer time without LVAD implantation than did those with from LBHs. Furthermore, differences in clinical characteristics between the patients from HBHs and LBHs were demonstrated for markers of nutrition and inflammation. A long duration of heart disease corresponded with a poorer nutritional state and higher degree of inflammation. We previously reported that a poor nutritional state with presence of inflammation corresponds to a poor clinical course following LVAD implantation28,29. Further recruitment of study patients and a more concise follow-up of LVAD complications would demonstrate an inferior survival and higher occurrence of LVAD-associated complications after LVAD implantation in patients from HBHs compared to patients from LBHs. However, this does not suggest that the timing of referral from HBHs was late. The factor of referral timing and HBH status should also be analyzed to elucidate appropriate patient allocation among various medical facilities. In addition, more patients should be evaluated to confirm the association found between survival after LVAD implantation and referral timing.
Many studies have analyzed prognostic factors in patients with HF30,31. However, there have been several differences among different subgroups of patients with HF, such as differences in their background characteristics or baseline cardiac function and etiology of HF. Therefore, the results of each study should be considered as subject to selection bias. In addition, the primary outcome of medical intractability, which includes LVAD implantation and death, was a determining factor. The present study has some similarities with the Kalogeropoulos study, which produced data on the progression of HF to stage D26, and with the Lanfear study, which examined LVAD-free survival32. Moreover, the treatment strategies of LVAD or HTx are limited to patients who meet the prescribed requirements of HTx candidacy, including age limitations, renal or liver function, and an absence of malignancy or active infection, which greatly affects the characteristics of the clinical course of disease.
This study has several limitations. The study population was comparatively small, and the study was performed at a single tertiary referral center in Japan, which might lessen the validity and importance of this study. In this cohort, the percentage of patients who were receiving beta-blockers or renin–angiotensin system antagonists was significantly lower than that of those in other studies24. However, this does not reflect the underutilization of appropriate medication for HF but rather indicates the difficulties of the administration of these medications due to patients having severe hypotension. Indeed, 32% of patients in the present study, which is significantly higher than that in previous studies, had a systolic blood pressure < 90 mmHg. In addition, the study design is limited in the evaluation of the effect of the medications. In this study, we analyzed only patients who were referred to our hospital. However, whether the referral was appropriate can be only sufficiently investigated after all patients, including both those referred and not referred, are analyzed. In addition, information is lacking in terms of the clinical course before patient transfer, such as transfer from LBHs to HBHs, which might also limit the validity of this study. The cultural context of LVAD and HTx in Japan also might affect the results of this study. For example, the implantation of LVAD is limited to functioning as a bridge to transplantation, and HTx is available only after a long duration of LVAD support. This substantially reduces the generalizability of the results of the present study. In addition, the high risk of complications, such as bleeding or thrombosis, from LVAD implantation makes its implementation and use more difficult. Therefore, there would be some possibility that factors other than those associated with advanced HF are considered in whether the patient receives LVAD implantation or HTx.
In conclusion, the patients referred to our center from HBHs had a higher risk of experiencing the primary outcome than did those referred to our center from LBHs. However, the association between HBH status and the outcomes was not significant in the multivariate analysis. In contrast, catecholamine support on transfer, long disease duration and low systolic pressure were independent predictors of the outcomes, and these should be considered as markers of advanced HF and justification for referral to an advanced HF center, irrespective of the bed volume of the referring hospital.
References
Benjamin, E. J. et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation 135, e146–e603 (2017).
Van Nuys, K. E. et al. Innovation in heart failure treatment: life expectancy, disability, and health disparities. JACC Heart Fail. 6, 401–409 (2018).
Joynt, K. E., Orav, E. J. & Jha, A. K. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann. Intern. Med. 154, 94–102 (2011).
Komuro, I. et al. Nationwide actions against heart failure pandemic in Japan-what should we do from academia?. Circ. J. 83, 1819–1821 (2019).
Friedrich, E. B. & Böhm, M. Management of end stage heart failure. Heart 93, 626–631 (2007).
Crespo-Leiro, M. G. et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 20, 1505–1535 (2018).
Rose, E. A. et al. Randomized evaluation of mechanical assistance for the treatment of congestive heart failure (REMATCH) study group. Long-term use of a left ventricular assist device for end-stage heart failure. N. Engl. J. Med. 345, 1435–1443 (2001).
Kyo, S. et al. HeartMate II Japanese Clinical InvestigatorsResults of the prospective multicenter Japanese bridge to transplant study with a continuous-flow left ventricular assist device. J. Artif. Organs 17, 142–148 (2014).
Guglin, M. et al. ACC heart failure and transplant member section and leadership council. Evaluation for heart transplantation and LVAD implantation: JACC council perspectives. J. Am. Coll. Cardiol. 75, 1471–1487 (2020).
Johnstone, J. et al. Patient- and hospital-level predictors of vancomycin-resistant Enterococcus (VRE) bacteremia in Ontario, Canada. Am. J. Infect. Control 46, 1266–1271 (2018).
Alqahtani, F. et al. Incidence, predictors, and outcomes of in-hospital percutaneous coronary intervention following coronary artery bypass grafting. J. Am. Coll. Cardiol. 73, 415–423 (2019).
Witte, K. K. et al. Mortality reduction associated with β-adrenoceptor inhibition in chronic heart failure is greater in patients with diabetes. Diabetes Care 41, 136–142 (2018).
Buckley, L. F. et al. Intravenous diuretic therapy for the management of heart failure and volume overload in a multidisciplinary outpatient unit. JACC Heart Fail. 4, 1–8 (2016).
Sawano, M. et al. Performance of the MAGGIC heart failure risk score and its modification with the addition of discharge natriuretic peptides. ESC Heart Fail. 5, 610–619 (2018).
Miura, M. et al. Usefulness of combined risk stratification with heart rate and systolic blood pressure in the management of chronic heart failure. A report from the CHART-2 study. Circ. J. 77, 2954–2962 (2013).
Voors, A. A. et al. A systems biology study to tailored treatment in chronic heart failure: rationale, design, and baseline characteristics of BioStat-CHF. Eur. J. Heart Fail. 18, 716–726 (2016).
Georgiopoulou, V. V. et al. Digoxin therapy does not improve outcomes in patients with advanced heart failure on contemporary medical therapy. Circ. Heart Fail. 2, 90–97 (2009).
Halpern, N. A. & Pastores, S. M. Critical care medicine beds, use, occupancy, and costs in the United States: a methodological review. Crit. Care Med. 43, 2452–2459 (2015).
Birkmeyer, J. D., Finlayson, E. V. & Birkmeyer, C. M. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery 130, 415–422 (2001).
Hannan, E. L. et al. Do hospitals and surgeons with higher coronary artery bypass graft surgery volumes still have lower risk-adjusted mortality rates?. Circulation 108, 795–801 (2003).
McGrath, P. D. et al. Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. JAMA 284, 3139–3144 (2000).
Kumbhani, D. J. et al. Association between hospital volume, processes of care, and outcomes in patients admitted with heart failure: insights from get with the guidelines-heart failure. Circulation 137, 1661–1670 (2018).
Maggioni, A. P. et al. Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur. J. Heart Fail. 15, 1173–1184 (2013).
Goda, A., Williams, P., Mancini, D. & Lund, L. H. Selecting patients for heart transplantation: comparison of the Heart Failure Survival Score (HFSS) and the Seattle heart failure model (SHFM). J. Heart Lung Transpl. 30, 1236–1243 (2011).
Thorvaldsen, T. et al. Triage of patients with moderate to severe heart failure: who should be referred to a heart failure center?. J. Am. Coll. Cardiol. 63, 661–671 (2014).
Kalogeropoulos, A. P. et al. Progression to stage d heart failure among outpatients with stage c heart failure and reduced ejection fraction. JACC Heart Fail. 5, 528–537 (2017).
Dhaliwal, A. S. et al. Reduction in BNP levels with treatment of decompensated heart failure and future clinical events. J. Card. Fail. 15, 293–299 (2009).
Saito, A. et al. Controlling nutritional status score as a predictive marker for patients with implantable left ventricular assist device. ASAIO J. 66, 166–172 (2020).
Tsuji, M. et al. Abdominal skeletal muscle mass as a predictor of mortality in Japanese patients undergoing left ventricular assist device implantation. ESC Heart Fail. 6, 526–535 (2019).
Voors, A. A. et al. Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur. J. Heart Fail. 19, 627–634 (2017).
Shiraishi, Y. et al. Validation and recalibration of Seattle heart failure model in Japanese acute heart failure patients. J. Card. Fail. 25, 561–567 (2019).
Lanfear, D. E. et al. Accuracy of seattle heart failure model and HeartMate II Risk Score in non-inotrope-dependent advanced heart failure patients: insights from the ROADMAP Study (Risk Assessment and Comparative Effectiveness of Left ventricular Assist Device and Medical Management in Ambulatory Heart Failure Patients). Circ. Heart Fail. 10, e003745 (2017).
Acknowledgements
This work was supported by the Ministry of Education, Culture, Sports, Science and Technology of Japan through Grant-in-Aid 17K09488 (to Amiya E).
Author information
Authors and Affiliations
Contributions
K.N.: Data collection, Statistical analysis, Writing of the manuscript. E.A.: Conception of the idea, Data collection, Critical feedback on the manuscript, Writing of the manuscript. M.H., J.I., H.M., A.S., S.M., M.T., C.B., S.I., N.K., M.S., Y.H., M.E., Y.K., H.I.: Data collection, Critical feedback on the manuscript. Y.I., M.A., S.S., O.K., O.M., I.K.: Critical feedback on the manuscript.
Corresponding author
Ethics declarations
Competing interests
EA and MH belong to the Department of Therapeutic Strategy for Heart Failure, Graduate School of Medicine, University of Tokyo, which is endowed by Actelion Pharmaceuticals Japan Ltd., Otsuka Pharmaceutical, NIPRO CORPORATION, Terumo Corp., Senko Medical Instrument Mfg., Century Medical Inc., Kinetic Concepts Inc., and St. Jude Medical. The other authors have no conflicts of interest to disclose. There are no patents, products in development, or marketed products to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Narita, K., Amiya, E., Hatano, M. et al. Differences in the prognoses of patients referred to an advanced heart failure center from hospitals with different bed volumes. Sci Rep 10, 21071 (2020). https://doi.org/10.1038/s41598-020-78162-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78162-z
- Springer Nature Limited
This article is cited by
-
Social and environmental risks as contributors to the clinical course of heart failure
Heart Failure Reviews (2022)