Abstract
The impact of reperfusion therapies on cognition has been poorly explored and little knowledge exists. We explored the influence of endovascular treatment (EVT) on cognitive outcome in patients with anterior circulation ischemic stroke. Patients presenting with ischemic stroke due to anterior large vessel occlusion who underwent intravenous thrombolysis (IVT) alone or EVT plus IVT were recruited. Cognitive abilities were evaluated at 6 months from stroke through a neuropsychological test battery. A total of 88 patients with a mean age of 66.3 ± 12.9 years were included, of which 38 treated with IVT alone and 50 with IVT plus EVT. Compared to patients treated with IVT alone, patients who received EVT plus IVT performed significantly better at the neuropsychological tests exploring executive functions, attention, abstract reasoning, visuospatial ability, visual and verbal and memory. At multivariable regression analysis, the EVT was independently associated with the 6-month cognitive performance after the adjustment for age, sex, admission National Institutes of Health Stroke Scale score, systolic blood pressure, glucose level, Alberta Stroke Program Early CT score, side of stroke, site of occlusion, and Back Depression Inventory score [Stroop Test Word Reading: adjβ = 13.99, 95% confidence interval (CI) 8.47–19.50, p < 0.001; Stroop Test Colour Naming: adjβ = 6.63, 95% CI 2.46–10.81, p = 0.002; Trail Making Test-A: adjβ = − 92.98, 95% CI − 153.76 to − 32.20, p = 0.003; Trail Making Test-B: adjβ = − 181.12, 95% CI − 266.09 to − 96.15; p < 0.001; Digit Span Test Forward: adjβ = 1.44, 95% CI 0.77–2.10, p < 0.001; Digit Span Test Backward: adjβ = 1.10, 95% CI 0.42–1.77, p = 0.002; Coloured Progressive Matrices: adjβ = 5.82, 95% CI 2.71–8.93, p < 0.001; Rey Complex Figure Test-Copy: adjβ = 6.02, 95% CI 2.74–9.30, p < 0.001; Rey Complex Figure Test-Immediate recall: adjβ = 6.00, 95% CI 2.34–9.66, p = 0.002; Rey Complex Figure Test-Delayed recall: adjβ = 5.73, 95% CI 1.95–9.51, p = 0.003; Rey Auditory Verbal Learning Test-Immediate recall: adjβ = 12.60, 95% CI 6.69–18.52, p < 0.001; Rey Auditory Verbal Learning Test-Delayed recall: adjβ = 1.85, 95% CI 0.24–3.45, p = 0.025]. Patients treated with EVT plus IVT had better cognitive performance than patients treated with IVT alone at 6 months from anterior circulation ischemic stroke.
Similar content being viewed by others
Introduction
Cognitive impairment is a common consequence after stroke1,2. It is closely related to disability, dependency and institutionalization, and it is a major determinant of poor quality of life in stroke survivors3,4,5. So far, the impact of reperfusion therapies on cognition has been poorly explored and little knowledge exists. Indeed, physical recovery represents the main endpoint in stroke trials, whereas cognitive outcome is generally overlooked6,7.
The aim of this study was to investigate the effect of the endovascular treatment (EVT) on cognitive functioning in patients with ischemic stroke due to proximal arterial occlusion of the anterior circulation by comparing the 6-month neuropsychological performance in patients treated with intravenous thrombolysis (IVT) alone and IVT plus EVT.
Results
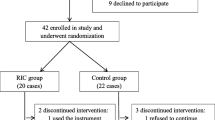
A total of 186 out of 1095 patients admitted to our Stroke Unit for ischemic stroke underwent IVT alone or IVT plus EVT for a proximal arterial occlusion of the anterior circulation (Fig. 1). Fifty-four patients were excluded due to history of prior stroke/dementia (n = 7), death (n = 26), and unavailability of neuropsychological assessment as lost to follow-up (n = 21). The comparison of baseline characteristics between the patients with 6-month neuropsychological assessment and those who were excluded due to lack of follow-up did not show significant differences (Supplementary Table S1). Among the patients (n = 132) who underwent neuropsychological evaluation at 6 months from stroke, 44 patients were further excluded from the full cognitive performance testing since they presented with aphasia (n = 24) and neglect (n = 20). The characteristics of the patients excluded due to the impairment in language and visuo-spatial inattention domains are shown in Supplementary Table S2.
Accordingly, 88 patients were included in the analysis, of which 38 treated with IVT alone and 50 with IVT plus EVT. Patients did not receive EVT due to stroke occurrence before full implementation of EVT delivery at the site (n = 21), mild neurologic deficit at onset (n = 8), successful opening of occlusion/marked improvement of neurological deficit by IVT (n = 8), and very elderly (n = 1).
The mean age of the patients was 66.3 ± 12.9 years and 31 (35.2%) were females; 45 (51.1%) patients had right and 43 (48.9%) left hemisphere stroke. Baseline demographic and clinical characteristics of the study cohort according to the treatment group are shown in Table 1. No statistically significant differences in the prevalence of vascular risk factors and stroke severity emerged among the two groups, with the exception of serum glucose levels and NIHSS score at admission, which were higher among the patients treated with IVT plus EVT.
The scores obtained by the patients in the neuropsychological tests performed at 6 months from stroke are summarized in Table 2. Patients treated with IVT alone obtained lower (worse) scores at the SCWT, DST, CPM, RCFT-C, RCFT-I, RCFT-D, RAVLT-I and RAVLT-D and higher (worse) scores at the TMT-A and TMT-B. Patients in the IVT group had also higher (worse) scores on the BDI in comparison to patients treated with IVT plus EVT [8.0 (2.0–11.0) versus 3.5 (0.0–9.0); p = 0.096] and higher (worse) scores on the mRS [3.0 (1.0–4.0) versus 1.0 (0.0–2.0); p < 0.001] in comparison to patients treated with IVT plus EVT.
The results of the regression analysis are shown in Table 3. The acute stroke treatment resulted a significant predictor of 6-month cognitive outcome being the EVT plus IVT associated with better cognitive performances, before and after the adjustment for potential confounding factors (Table 3). None of the multivariate models suffered from collinearity (variance inflation factors ranged from 1.10 to 2.05).
Discussion
The main finding of this study was the better 6-month cognitive outcome observed in patients with stroke due to proximal large vessel occlusion who underwent IVT combined with EVT than IVT alone. At the follow-up visit, patients treated with IVT plus EVT performed better in the tests exploring executive functions and attention, abstract reasoning, constructive ability, and visuospatial and verbal memory.
The early recanalization of the occluded vessels is the main mechanism underlying the beneficial effects of the reperfusion therapies: it can restore flow to the ischemic penumbra and prevent its transformation into necrotic tissue8. Significant differences, however, exist between pharmacological intravenous fibrinolysis and mechanical endovascular clot removal as the responsiveness of large thrombi to enzymatic digestion is quite poor, whereas EVT can rapidly remove proximal clots9,10,11,12. The early recanalization through EVT has demonstrated to be more efficacious in lowering the risk of mortality, reduces the severity of disability and increases the rate of functional independence in comparison to standard medical care in patients with strokes due to large vessels occlusions13. The current study extends the findings of the recent randomized controlled trials and provides evidence that the EVT has the potentiality to favorably influence the post-stroke cognitive recovery. Indeed, the mRS—the most commonly used instrument to assess clinical outcome in stroke trials—relies mostly on physical functions and under-represents cognitive abilities. Detailed neuropsychological assessments can be beneficial both in stroke trials and clinical practice14,15,16. First, a broad spectrum of cognitive changes occurs after stroke and multiple domains and complex neuropsychological abilities are typically compromised. Second, cognitive deficits are prevalent also in patients with the most favorable clinical recovery and no apparent functional disability. Third, even milder cognitive deficits can have impact on independent functioning, occupational abilities and quality of life17,18. Additionally, items that are often affected by stroke, as processing speed, calculation, and praxis, are not included in current screening measures, and require a comprehensive investigation to be fully explored19.
In the prespecified secondary analysis of the REVASCAT (Endovascular Revascularization With Solitaire Device Versus Best Medical Therapy in Anterior Circulation Stroke Within 8 h) trial, patients randomized to thrombectomy plus best medical treatment rather than best medical treatment alone performed better in the TMT-A and TMT-B at 3 months and 1 year after stroke due to anterior circulation proximal arterial occlusion20. It is however worth to notice that cognitive outcome was evaluated with one single test, which focused on executive functioning, and the lack of a comprehensive neuropsychological battery did not allow drawing conclusions on other cognitive domains. In addition, as motor dexterity is required to perform the TMT, the results and their interpretation could be biased by co-occurring impairment in motor function of the upper arm; the high proportion of participants who did not complete the task in the requested time and, hence, received the maximum time score, may have masked performance variability among the most severely impaired patients and allowed to identify significant differences between treatment groups only in functionally independent patients. Finally, symptoms of depression were collected indirectly and not included in multivariable analysis.
Recently, Xu et al. found that patients with mild to moderate anterior circulation infarct who received mechanical thrombectomy at broadened therapeutic window had higher scores in Mini-Mental State Examination and Montreal Cognitive Assessment tests at the 90 days follow-up than those receiving standard therapy treatment21. Although both tests can assess multiple cognitive abilities, they represent global screening tools for detecting cognitive impairment rather than instruments to thoroughly evaluate the neuropsychological domains. Moreover, the very small differences in total scores observed between the treatment arms and the lack of data about the individual items of both tests make difficult the clinical interpretation of the findings.
The main strengths of the current study included the comparison of patients who underwent treatment with rt-PA alone versus rt-PA combined with mechanical thrombectomy, which allowed to minimize the heterogeneity in baseline patients’ characteristics and time onset-to-treatment and, hence, estimate the actual effect deriving from the EVT. The exclusion of patients presenting with aphasia or neglect from the comprehensive neuropsychological assessment allowed to obtain a more reliably evaluation of the neurocognitive performance as results in cognitive tests are significantly affected and confounded by the presence of deficits in the domains of language and visuo-spatial inattention22,23. Finally, the 6-month interval from stroke to follow-up can be considered a sufficiently long time for the acute stroke effects to subside24,25, and the real-world setting of the research increased the generalizability of the findings to routine clinical practice. Nonetheless, some study shortcomings need to be considered. The retrospective analysis of data collected at a single academic center could have led to selection bias and findings need to be validated in independent cohorts. The relatively small sample size prevented sub-group analyses and no data on health-related quality of life have been considered at the follow-up. Additionally, no specific information regarding treatment success, including reperfusion rates, follow-up infarct volumes or hemorrhage rates have been considered, and further studies designed to comprehensively assess these parameters as well as the relationship between infarct location and test scores are warranted.
Conclusion
The growing number of stroke survivors has increased the interest in long-term sequelae and prediction of cognitive outcome. In this regard, treatment with EVT plus IVT can result in better cognitive performance than IVT alone in patients with anterior circulation ischemic stroke.
Methods
Study participants
We retrospectively identified consecutive patients with anterior circulation ischemic stroke, admitted to the Stroke Unit of the Marche Polytechnic University (Ancona, Italy) from January 2012 to June 2019, who were treated with IVT alone and IVT plus EVT, and underwent neuropsychological assessment at 6 months from the index event as part of routine care. The site serves in the region as referral comprehensive stroke center (hub) for mechanical thrombectomy for large vessel occlusion according to a drip-and-ship organizational model of stroke care. Patients were included if they had intracranial proximal arterial occlusion in the anterior circulation [intracranial carotid artery (ICA) or middle cerebral artery (M1/M2) or anterior cerebral artery (A1/A2)] demonstrated by vascular imaging (computed tomographic angiography or magnetic resonance angiography or digital subtraction angiography), received IVT within 4.5 h and started EVT within 6.0 h after the onset of stroke. IVT consisted of the administration of recombinant tissue plasminogen activator (rt-PA) at the dose of 0.9 mg/kg (maximum 90 mg; 10% bolus followed by a 60-min infusion). EVT consisted of mechanical thrombectomy with aspiration catheters alone, stent-retrievers alone, or both, depending on occlusion type and interventionist’s choice.
Data about demographic, vascular risk factors, medical history, baseline stroke severity according to the National Institutes of Health Stroke Scale (NIHSS) score26, admission systolic blood pressure (BP) and serum glucose were collected, as previously detailed27,28,29. The ischemic lesion extension was estimated according to the Alberta Stroke Program Early CT Score (ASPECTS) on head computed tomography (CT) performed in emergency prior to IVT administration30. Patients with a neurological or psychiatric history, pre-stroke modified Rankin Scale (mRS)31 score > 2, patients who did not perform the neuropsychological evaluation at 6 months from stroke and those who presented aphasia or neglect at the 6-month evaluation according to the Aphasia Neuropsychological Exam (ANE) (language)32 and Apples Cancellation Test (ACT) (visuo-spatial inattention)33 were not included.
Neuropsychological assessment
The neuropsychological assessment was administered by a trained examiner at a single session 6 months after stroke using standardized cognitive tests at the Clinic of Neurorehabilitation of the Marche Polytechnic University as part of clinical care. Scores obtained in the following neuropsychological tests were considered in the current analysis as representative of different cognitive domains: Stroop Colour and Word Test (SCWT)34, Trail Making Test parts A (TMT-A) and B (TMT-B)35, Digit Span Test (DST) (executive functions and attention)36, Coloured Progressive Matrices (CPM) (abstract reasoning)37, Rey Complex Figure Test Copy (RCFT-C) (visuospatial ability), Rey Complex Figure Test immediate (RCFT-I) and delayed recall (RCFT-D) (visual memory)38, Rey Auditory Verbal Learning Test immediate (RAVLT-I) and delayed recall (RAVLT-D) (verbal memory)39. All test scores were corrected according to normative values; the score ranges of the cognitive tests are summarized in Supplementary Appendix-SI. Post-stroke depressive symptoms and functional abilities were assessed with the Beck Depression Inventory (BDI)40 and mRS31.
Statistical analysis
Values were presented as mean ± standard deviation (SD) or median (interquartile range [IQR]) for continuous variables and as the number (%) of subjects for categorical variables. Univariate comparisons were made through the Student t test, Mann–Whitney test, or Chi-squared test, as appropriate. Linear regressions were performed to assess the influence of treatment (IVT alone versus IVT plus EVT) on scores obtained in each cognitive test, adjusting for pre-specified potential confounding factors (age, sex, admission NIHSS score, systolic BP, glucose level, ASPECT score, side of stroke, site of occlusion, BDI score). The collinearity between exposure variables was assessed with the variance inflation index. Results were considered significant for p values < 0.05 (two sided). Data analysis was performed using STATA/IC 13.1 statistical package (StataCorp LP, Texas, USA).
Standard protocol approvals, registrations, and patient consents
The study was approved by the Ethics Committee of the Marche Polytechnic University and conducted according to the Declaration of Helsinki. Informed consent was obtained from any patient or the legal representative.
Data availability
Anonymized data will be shared by request from any qualified investigator.
References
Leśniak, M., Bak, T., Czepiel, W., Seniów, J. & Członkowska, A. Frequency and prognostic value of cognitive disorders in stroke patients. Dement. Geriatr. Cogn. Disord. 26, 356–363 (2008).
Pendlebury, S. T. & Rothwell, P. M. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: A systematic review and meta-analysis. Lancet Neurol. 8, 1006–1018 (2009).
Nys, G. M. et al. The prognostic value of domain-specific cognitive abilities in acute first-ever stroke. Neurology. 64, 821–827 (2005).
Nys, G. M. et al. Early cognitive impairment predicts long-term depressive symptoms and quality of life after stroke. J. Neurol. Sci. 247, 149–156 (2006).
Patel, M. D., Coshall, C., Rudd, A. G. & Wolfe, C. D. Cognitive impairment after stroke: Clinical determinants and its associations with long-term stroke outcomes. J. Am. Geriatr. Soc. 50, 700–706 (2002).
McKevitt, C. et al. Self-reported long-term needs after stroke. Stroke 42, 1398–1403 (2011).
Pollock, A., St George, B., Fenton, M. & Firkins, L. Top ten research priorities relating to life after stroke. Lancet Neurol. 11, 209 (2012).
Kumar, G., Goyal, M. K., Sahota, P. K. & Jain, R. Penumbra, the basis of neuroimaging in acute stroke treatment: Current evidence. J. Neurol. Sci. 288, 13–24 (2010).
Saqqur, M. et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke 38, 948–954 (2007).
De Silva, D. A. et al. The benefits of intravenous thrombolysis relate to the site of baseline arterial occlusion in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET). Stroke 41, 295–299 (2010).
Paciaroni, M. et al. Systemic thrombolysis in patients with acute ischemic stroke and Internal Carotid ARtery Occlusion: The ICARO study. Stroke 43, 125–130 (2012).
Jansen, O., von Kummer, R., Forsting, M., Hacke, W. & Sartor, K. Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. Am. J. Neuroradiol. 16, 1977–1986 (1995).
Goyal, M. et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 387, 1723–1731 (2016).
Benjamin, E. J. et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation 135, e146-603 (2017).
Lattanzi, S. et al. Neurocognitive functioning and cerebrovascular reactivity after carotid endarterectomy. Neurology 90, e307-315 (2018).
Lattanzi, S. et al. Predictors of cognitive functioning after carotid revascularization. J. Neurol. Sci. 405, 116435 (2019).
Feigin, V. L., Lawes, C. M., Bennett, D. A. & Anderson, C. S. Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2, 43–53 (2003).
Jokinen, H. et al. Post-stroke cognitive impairment is common even after successful clinical recovery. Eur. J. Neurol. 22, 1288–1294 (2015).
Stolwyk, R. J., O’Neill, M. H., McKay, A. J. & Wong, D. K. Are cognitive screening tools sensitive and specific enough for use after stroke? A systematic literature review. Stroke 45, 3129–3134 (2014).
López-Cancio, E. et al. Endovascular treatment improves cognition after stroke: A secondary analysis of REVASCAT trial. Neurology 88, 245–251 (2017).
Xu, G. et al. Cognitive function and prognosis of multimodal neuroimage-guided thrombectomy on mild to moderate anterior circulation infarction patients with broadened therapeutic window: A prospective study. Eur. Neurol. 78, 257–263 (2017).
Wall, K. J., Cumming, T. B. & Copland, D. A. Determining the association between language and cognitive tests in poststroke aphasia. Front. Neurol. 8, 149 (2017).
Demeyere, N. et al. Domain-specific versus generalized cognitive screening in acute stroke. J. Neurol. 263, 306–315 (2016).
Tatemichi, T. K. et al. Dementia after stroke is a predictor of long-term survival. Stroke 25, 1915–1919 (1994).
Woo, J., Kay, R., Yuen, Y. K. & Nicholls, M. G. Factors influencing long-term survival and disability among three-month stroke survivors. Neuroepidemiology 11, 143–150 (1992).
Wityk, R. J., Pessin, M. S., Kaplan, R. F. & Caplan, L. R. Serial assessment of acute stroke using the NIH Stroke Scale. Stroke 25, 362–365 (1994).
Lattanzi, S. et al. The P-wave terminal force in embolic strokes of undetermined source. J. Neurol. Sci. 375, 175–178 (2017).
Lattanzi, S. et al. Prediction of outcome in embolic strokes of undetermined source. J. Stroke Cerebrovasc. Dis. 29, 104486 (2020).
Lattanzi, S. et al. Clinical phenotypes of embolic strokes of undetermined source. Neurol. Sci. https://doi.org/10.1007/s10072-020-04700-2 (2020).
Barber, P. A., Demchuk, A. M., Zhang, J. & Buchan, A. M. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 355, 1670–1674 (2000).
Banks, J. L. & Marotta, C. A. Outcomes validity and reliability of the modified Rankin scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 38, 1091–1096 (2007).
Capasso, R. & Miceli, G. Esame Neuropsicologico per l’Afasia (ENPA) (Springer, Berlin, 2001).
Mancuso, M. et al. Italian standardization of the Apples Cancellation Test. Neurol. Sci. 36, 1233–1240 (2015).
Barbarotto, R. et al. A normative study on visual reaction times and two Stroop colour-word tests. Ital. J. Neurol. Sci. 19, 161–170 (1998).
Giovagnoli, A. R. et al. Trail Making Test: Normative values from 287 normal adult controls. Ital. J. Neurol. Sci. 17, 305–309 (1996).
Monaco, M., Costa, A., Caltagirone, C. & Carlesimo, G. A. Forward and Backward span for verbal and visuo-spatial data: Standardization and normative data from an Italian adult population. Neurol. Sci. 34, 749–754 (2013).
Basso, A., Capitani, E. & Laiacona, M. Raven’s coloured progressive matrices: Normative values on 305 adult normal controls. Funct. Neurol. 2, 189–194 (1987).
Le Osterrieth, P. A. test de copie d’une figure complexe: Contribution a l’´etude de la perception et de la memoire. Arch. Psychol. 30, 286–350 (1944).
Carlesimo, G. A., Caltagirone, C. & Gainotti, G. The Mental Deterioration Battery: Normative data, diagnostic reliability and qualitative analyses of cognitive impairment. The Group for the Standardization of the Mental Deterioration Battery. Eur. Neurol. 36, 378–384 (1996).
Ghisi, M., Flebus, G. B., Montano, A., Sanavio, E. & Sica, C. Beck Depression Inventory—II (BDI-II) Manuale (Organizzazioni Speciali, Florence, 2006).
Author information
Authors and Affiliations
Contributions
S.L.: study concept and design, analysis and interpretation of data, writing and critical revision of the manuscript for important intellectual content. M.C., A.P., C.C., F.L.G., L.V., S.C., M.D., G.P., M.G.C.: acquisition of data, analysis and interpretation. M.S.: study concept and design, critical revision of the manuscript for important intellectual content, study supervision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lattanzi, S., Coccia, M., Pulcini, A. et al. Endovascular treatment and cognitive outcome after anterior circulation ischemic stroke. Sci Rep 10, 18524 (2020). https://doi.org/10.1038/s41598-020-75609-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-75609-1
- Springer Nature Limited