Abstract
Lysophosphatidic acid (LPA) species are bioactive lipids participating in neurodevelopmental processes. The aim was to investigate whether the relevant species of LPA were associated with clinical features of alcohol addiction. A total of 55 abstinent alcohol use disorder (AUD) patients were compared with 34 age/sex/body mass index-matched controls. Concentrations of total LPA and 16:0-LPA, 18:0-LPA, 18:1-LPA, 18:2-LPA and 20:4-LPA species were quantified and correlated with neuroplasticity-associated growth factors including brain derived neurotrophic factor (BDNF), insulin-like growth factor-1 (IGF-1) and IGF-2, and neurotrophin-3 (NT-3). AUD patients showed dysexecutive syndrome (22.4%) and memory impairment (32.6%). Total LPA, 16:0-LPA, 18:0-LPA and 18:1-LPA concentrations, were decreased in the AUD group compared to control group. Total LPA, 16:0-LPA, 18:2-LPA and 20:4-LPA concentrations were decreased in men compared to women. Frontal lobe functions correlated with plasma LPA species. Alcohol-cognitive impairments could be related with the deregulation of the LPA species, especially in 16:0-LPA, 18:1-LPA and 20:4-LPA. Concentrations of BDNF correlated with total LPA, 18:2-LPA and 20:4-LPA species. The relation between LPA species and BDNF is interesting in plasticity and neurogenesis functions, their involvement in AUD might serve as a biomarker of cognitive impairment.
Similar content being viewed by others
Introduction
Alcohol use disorders (AUD) are one of the main global health problems, with a worldwide impact on individuals and society. They cause a significant medical burden in prevention and treatment effort1,2. Among the medical consequences related to alcohol dependence we can highlight the prevalence of nutritional deficiencies, hepatic and liver damage3,4 and the appearance of comorbid psychopathological lifetime complications5. Moreover, cognitive impairment associated to AUD is considered one of the main factors for the development of any type of dementia6. The presence of comorbid medical conditions during AUD could contribute to the lack of control over drinking aggravating the medical treatment7.
While major depressive disorders and anxiety are the most prevalent psychopathological comorbid disorders in alcohol use population8,9,10, cocaine and cannabis abuse are the most common lifetime comorbid substance disorders associated to AUD11. Moreover, chronic alcohol consumption could modulate neurogenesis and produce distortions on the central nervous system causing neurocognitive impairment12,13. Thus, functional circuits involved on these medical consequences of alcohol include those related to cognition (such as prefrontal cortex-involving circuits) and emotional processing (such as limbic-amigdalar circuits). The most common cognitive alterations in alcohol dependence patient are those related with executive functions, episodic and visuoconstructive memory and emotion4,14. In AUD patients, the measurable neuropsychological damage belonging to executive functions have been found impaired in those tasks related to inhibition, flexibility, deduction of rules, organization and planning15,16. Recently, we have linked AUD associated with mild and severe cognitive impairment and to a dysfunctional signaling of both, the insulin growth factor (IGF) and the brain derived neurotrophic factor (BDNF), a member of the neurotrophin family of growth factors17,18,19. These findings suggest that at least partially, monitoring BDNF signaling might help to identify early stages of cognitive impairment in AUD patients. However, in these studies neither IGF-1 nor BDNF were found to be associated to any additional comorbidity, especially psychiatric entities such as depressive and psychotic disorders that it is known to contribute to cognitive impairment17.
In an attempt to further explore biomolecules that might mediate the effects of alcohol on psychiatric comorbidity and cognitive impairment, we focused our research on lysophosphatidic acid (LPA), an ubiquitous signaling lipid involved in neurodevelopment20,21 and emotional behavior, including anxiety21,22. LPA has the simplest structure of all glycerophospholipids in serum and is highly expressed in the brain23. The term LPA refers to a group of different chemical species where the glycerophospholipid moiety is associated to several different carbon acyl chains (i. e. 16-, 18- and 20-LPA), being the species mono-unsaturated oleic acid (18:1-LPA), and poly-unsaturated linoleic acid (18:2-LPA) and arachidonic acid (20:4-LPA) the more abundant in human serum24,25. LPA participates in brain cortex formation, cell proliferation, differentiation and survival functions through the activation of distinct G-protein-coupled receptors20,26,27, although there are evidences that LPA participates in apoptosis processes through oxidative stress28. In addition, LPA also is involved in adult neurogenesis29,30. These important roles in neurodevelopment and plasticity have suggested that abnormalities in LPA signaling might be related to neurodevelopmental disturbances and neuropsychiatric diseases as schizophrenia, Alzheimer’s diseases or autism31,32. Recent preclinical studies have also linked LPA to depression, since genetically modified animals lacking LPA1 receptors exhibits an anxious-depressive phenotype33 associated with high alcohol intake34. Because of the previously described involvement of LPA in both alcohol intake and depression, and the participation of these lipids in neural plasticity events, it is feasible to suspect a potential role for LPA species in comorbidities associated with AUD.
Since preclinical studies have suggested a potential role of LPA and its LPA1 receptor as vulnerability factors for excessive alcohol intake, depression and cognitive impairment, we further explore whether this association might also be present in AUD patients. Thus, the main aim of this descriptive clinical study was to characterize the plasma concentrations of LPA species in a chronic alcohol dependence context and to explore if they correlate with the associated psychiatric (i.e. affective disorders) and neuropsychological (cognitive impairment) comorbidities. Additionally, because previous studies have reported the existence of sexual dimorphism in the biological activity of LPA with a greater presence in healthy women compared with men30,35, the present study was performed in male and female patients to examine the plasma concentration of LPA species according to sex.
Materials and methods
Participants and recruitment
The present study included 89 Caucasian volunteers divided into two groups: 55 abstinent alcohol use disorders patients (AUD group) in outpatient treatments and 34 control subjects (Control group) matched by age, body mass index (BMI) and proportion of sex with the alcohol group. Patients were recruited at the Hospital Universitario 12 de Octubre (Madrid, Spain) and Centro provincial de Drogodependencias (Malaga, Spain). Control participants were included from databases of healthy subjects willing to participate in medical research projects from Hospital Universitario 12 de Octubre (Madrid, Spain) and Hospital Regional Universitario de Malaga (Málaga, Spain).
To be eligible for the present study, participants had to meet the following inclusion criteria: ≥ 18–65 years of age, and abstinence from alcohol for at least 4 weeks. The exclusion criteria included: personal history of long-term inflammatory diseases or cancer, cognitive or language limitations, pregnant or breast-feeding women, and infectious diseases. With regard the control group, participants with psychiatric disorders in Axis I were also excluded.
Clinical and neuropsychological assessments
Substance use disorders and other psychiatric disorders were diagnosed according to the DSM-IV-TR criteria36 using the Spanish version of the Psychiatric Research Interview for Substance and Mental Disorders (PRISM)36,37. PRISM is a semi-structured interview with good psychometric properties in the evaluation of substance use disorders and in the main psychiatric comorbid disorders related to substance use population37,38.
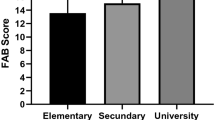
The cognitive assessment was performed with two scales, the Spanish Versions of the Frontal Assessment Battery (FAB)39 and the Memory Failures Everyday (MFE)40. The FAB test is useful for a screening of a frontal lobe dysfunction evaluation. The total score was obtained from 0 to 18 evaluating the respectively subdomains: prehension, go-no-go, conflicting, Luria motor and lexical fluency; a cut-off point less than 16 separate normal from mild dysexecutive deficits, and a cut-off point less than 13 separate mild and severe dysexecutive syndrome39. The MFE questionnaire is formed by 30 items and is useful to evaluate the lack of memory in daily life. The cognitive complaints scores over 36 are related with memory deficits40.
Collection of plasma samples
Plasma sample collection was based on previous studies about lipid mediators in addiction and comorbid disorders41. Blood samples were obtained in the morning after fasting for 8–12 h (prior to the psychiatric interviews) by experienced nurses. Venous blood was extracted into 10 mL K2 EDTA tubes (BD, Franklin Lakes, NJ, USA) and immediately centrifuged at 2200×g for 15 min (4 °C) to obtain plasma. The plasma samples were individually assayed to detect infectious diseases using commercial rapid tests for HIV, hepatitis B, and hepatitis C (Strasbourg, Cedex, France). Plasma samples were individually stored at – 80 °C until further analyses.
Analysis of LPA species
The LPA species of saturated fatty acids palmitic acid (16:0-LPA) and stearic acid (18:0-LPA), the LPA of the monounsaturated fatty acid oleic acid (18:1-LPA), and the LPA species of the polyunsaturated fatty acids linoleic acid (18:2-LPA) and arachidonic acid (20:4-LPA) were determined using an extraction protocol followed by LC–MS–MS separation and quantification. Briefly, 0.2 mL of plasma were spiked with 100 ng of a mathanolic solution of 17:0-LPA (IS). A liquid–liquid extraction was performed after the addition of 200 μL of butanol. The organic phase was evaporated and reconstituted in 100 μL of mobile phase (80A:20B, see below) prior to analysis.
Stock solutions (100 μg/mL) for each analyte were independently prepared by diluting adequate amounts of standards in methanol. The working solutions were prepared by mixture of the stock solutions and dilution in methanol. The linearity of calibration curves containing the following concentrations for all the target analytes: 0.2, 0.5, 1, 1.5, 2, 4, 6, 8, 10 μg/mL was verified being the coefficient of determination r2 > 0.99 in all cases.
Before the quantification of real samples and in order to verify matrix effect and recovery of the analytical method for each analyte, calibration curves were prepared in both plasma and water samples. In all cases, matrix effects lower than 6% and recoveries higher than 66% were achieved. At this point, calibration curves to perform quantification of real samples were prepared in water, and were added in duplicate in each analytical batch.
The procedure of lipid analysis in plasma was performed by a validated method previously described in clinical samples41. Quantification of LPA species in human plasma was performed using an ACQUITY UPLC system (Waters Associates, Milford, MA, USA) for the chromatographic separation coupled to a triple quadrupole (Xevo TQ-S micro) mass spectrometer provided with an orthogonal Z-spray-electrospray interface (ESI) (Waters Associates, Milford, MA, USA). The drying and nebulizing gas was nitrogen. The desolvation gas flow was set to 1200 L/h and the cone gas flow to 50 L/h. A capillary voltage of 3 kV was used in negative ionization mode. The nitrogen desolvation temperature was set to 600 °C and the source temperature to 150 °C. Collision gas was argon and the injection volume was 5 μL.
The chromatographic separation was achieved at 30 °C using an ACQUITY UPLC BEH C18 column (2.1 × 100 mm × 1.7 µm) (Waters Associates, Milford, MA, USA), at a flow rate of 300 µL/min. Mobile phase A was ammonium formate 1 mM with formic acid (0.01% v/v) dissolved in methanol. Mobile phase B was ammonium formate 1 mM with formic acid (0.01% v/v) in water. A gradient program was employed for the separation of the analytes; the percentage of mobile phase B linearly changed as follows: 0 min, 20%; 0.2 min, 20%; 6 min, 10%; 6.5 min, 10%; 7 min, 20%; 8 min, 20%. Total run time was 8 min. Analytes were determined by a Selected Reaction Monitoring (SRM) method by acquiring two transitions for each compound as specified (Supplementary Table S1). The most specific transition was selected for quantitative purposes. MassLynx software V4.1 and TargetLynx XS were used for data management. Finally, the LPA species plasma concentrations were recalculated to molar concentration (nmol/L).
Analysis of neurotrophic factors
Plasma concentrations of BDNF, IGF-2 and NT-3 were determined using different enzyme-linked immunosorbent assay (ELISA) according to the manufacturer’s instructions: human BDNF SimpleStep ELISA Kit (#ab212166, Abcam, Cambridge, UK) human IGF-2 Quantikine ELISA Kit (#DG200, R&D Systems, Minneapolis, MN, USA) and NT-3 ELISA Kit (#EHNTF3, ThermoFisher Scientific, Alcobendas, Madrid, Spain). To perform the ELISA protocols we used 50 μL of plasma as described previously17 and plasma concentrations of IGF-1 were estimated by double antibody radioimmunoassay. Plasma fractions were incubated with 125I-IGF-1 at 4 °C for 24 h with IGF-1 antiserum (UB2-495). In each assay a calibration curve and internal controls were included. The BDNF, IGF-1, IGF-2 and NT-3 plasma concentration were recalculated to molar concentration (nmol/L).
Statistical analysis
All data in the tables are expressed as number and percentage of subjects [N (%)] or mean and standard deviation (SD). The significance of differences in categorical and normal continuous variables was determined using Fisher’s exact test (chi-square test) and Student’s t test, respectively.
Multiple analysis of covariance (ANCOVA) was performed to indicate the relative effects of explanatory variable (i.e., lifetime alcohol use disorders, cognitive impairment) on the plasma concentrations of molecular LPA species, controlling for additional independent variables and covariates (e.g., sex, age and BMI). Because we used factors with two levels and there were not significant interactions between factors in the ANCOVA models, post hoc tests for multiple comparisons were not performed. Correlation analyses were performed using the Spearman’s coefficient (rho) (Plasma concentrations of LPA species and MFE or FAB scores) and correlation analyses using the Pearson’s coefficient (r) in logarithm (10)-transformation concentrations of LPA species and growth factors (BDNF, IGF-1 and IGF-2, and NT-3) to ensure statistical assumption for positive skewed distribution. The statistical analyses were carried out with the GraphPad Prism version 5.04 (GraphPad Software, San Diego, CA, USA), and IBM SPSS Statistical version 22 (IBM, Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
Ethics statements
Written informed consents were obtained from each participant after a complete description of the study. All the participants had the opportunity to discuss any questions or issues. The study and protocols for recruitment were approved by the Ethics Committee of the Hospital Regional Universitario de Malaga (CP14/00173, CP14/00212 and PI13/02261) in accordance with the Ethical Principles for Medical Research Involving Human Subjects adopted in the Declaration of Helsinki by the World Medical Association (64th WMA General Assembly, Fortaleza, Brazil, October 2013) and Recommendation No. R (97) 5 of the Committee of Ministers to Member States on the Protection of Medical Data (1997), and Spanish data protection act [Regulation (EU) 2016/679 of the European Parliament and of the Council 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation). All collected data were given code numbers in order to maintain privacy and confidentiality.
Results
Table 1 shows a socio-demographic description of the 89 participants of both gender included in this study. We selected 55 patients in abstinence from AUD outpatient programs and 34 healthy control subjects matched for sex, age and BMI with AUD patients. Significant differences were observed between the two sample groups with respect to marital status (p < 0.05) education degree (p < 0.05) and occupation (p < 0.001). The mean age of the AUD group was 48 years and the 82% of the participants were men with a BMI of 26. AUD group displayed higher prevalence of separations and divorces, secondary educational level, and unemployment rate than the control group.
Alcohol-related variables and cognitive deficits in AUD group
The variables related to AUD group were evaluated and described in Table 2. The mean age at first drink of alcohol was 15.3 years, while the average age of the AUD onset was 30.2 years with 14.8 years of problematic alcohol use. The mean of addiction criteria was 8 (based on DSM-5) and they had a length of 79 days of abstinence at the moment of the evaluation.
Regarding other abused substances, a 74.2% of the AUD group were smokers and there was a high prevalence of other substance use disorders (SUDs) (41.8%), being cocaine the most prevalent substance use (22.5%). In addition to the SUDs, there was observed an elevated prevalence of other psychiatric disorders (63.6%). Thus, lifetime mood and anxiety disorders were diagnosed in a 27% and 21.3% of AUD group, respectively. Unlike the control participants, the 85.5% of the abstinent alcohol patients received psychiatric medication during the last 12 months: antidepressants (52.7%), anxiolytics (41.8%) and anticraving (29.1%). Finally, the 70.9% of the AUD group were treated with disulfiram.
The neuropsychological evaluation revealed that a 22% of the AUD group showed some deficits related to frontal cognition (assessed with FAB); 33% of them suffer memory deficits (assessed with MFE) and 31% showed some impairment of both frontal cognition and memory deficits.
Plasma concentrations of LPA species in abstinent alcohol patients
The impact of the alcohol dependence was studied in the total sample using a two-way ANCOVA with “group” (AUD group and control group) and “sex” as factors, and age and BMI as covariates (Supplementary Table S2).
Plasma concentration of the total LPA was significantly affected by “group” and by “sex” factors, but there was no interaction effect between both factors. Plasma concentration of total LPA was significantly affected by the factor “group” [F(1,82) = 4.629; p = 0.034]. There was a significant reduction in total LPA plasma concentration in the AUD group compared with the control group [60.847 (95% CI 52.190–69.503) nmol/L and 74.922 (95% CI 65.190–84.512) nmol/L, respectively]. Regarding LPA species, plasma concentration of 16:0-LPA [F(1,82) = 5.640; p = 0.020], 18:0-LPA [F(1,82) = 5.166; p = 0.026] and 18:1-LPA [F(1,82) = 7.114; p = 0.009] were significantly affected by the factor “group”. Specifically, 16:0-LPA, 18:0-LPA and 18:1-LPA plasma concentrations were significantly lower in the AUD group than in the control group [16:0-LPA: 8.094 (95% CI 6.979–9.210) nmol/L and 10.096 (95% CI 8.861–11.332) nmol/L; 18:0-LPA: 2.958 (95% CI 2.727–3.199) nmol/L and 3.372 (95% CI 3.105–3.639) nmol/L; and 18:1-LPA: 5.998 (95% CI 25.258–6.738) nmol/L and 7.489 (95% CI 6.670–8.308) nmol/L; respectively]. By contrast, 18:2-LPA and 20:4-LPA plasma concentrations were not affected by the “group” factor or interaction effect between “group” and “sex” factors.
Regarding the impact of “sex”, the plasma concentration of total LPA [F(1,82) = 8.377; p = 0.005], 16:0-LPA [F(1,82) = 10.539; p = 0.002], 18:2-LPA [F(1,82) = 8.755; p = 0.004] and 20:4-LPA [F(1,82) = 4.548; p = 0.036] were significantly different between men and women. Thus, women had higher total LPA concentrations than men [77.360 (66.023–88.698) nmol/L and 58.409 (95% = 52.205–64.613) nmol/L, respectively]. Similarly, we observed significantly higher concentrations of 16:0-LPA, 18:2-LPA and 20:4-LPA in women than in men [16:0-LPA, 10.465 (9.004–11.926) nmol/L and 7.726 (95% CI 6.926–8.525) nmol/L; 18:2-LPA, 39.012 (95% CI 32.234–45.790) nmol/L and 27.429 (95%CI 23.720–31.138) nmol/L; and 20:4-LPA, 17.405 (95% CI 14.572–20.237) nmol/L and 13.916 (95% CI 12.916–15.466) nmol/L; respectively] (see Supplementary Table S3). Estimated marginal means for “group” and “sex” factors are represented in Fig. 1.
Plasma concentrations of LPA species in the sample according to the group and sex. (A) Bars are estimated marginal means and 95% confidence intervals (95%) representing total LPA (nmol/L) according to the group; (B) bars are estimated marginal means and 95% confidence intervals (95%) representing LPA species (nmol/L) according to the group; (C) bars are estimated marginal means and 95% confidence intervals (95%) representing total LPA (nmol/L) according to the sex; (D) bars are estimated marginal means and 95% confidence intervals (95%) representing LPA species (nmol/L) according to the group. Data were analyzed by two-way analysis of covariance (ANCOVA) and *p < 0.05 and **p < 0.010 denote a significant main effect of group factor or sex.
Plasma concentrations of LPA species in comorbid psychiatric disorders in abstinent alcohol patients
As shown in the clinical description of the sample (Table 2), mood and anxiety disorders were the most prevalent comorbid psychiatric disorders in the AUD group. Thus, we examined the effect of mood and anxiety comorbid disorders in total LPA and LPA species in the AUD group using a two-way ANCOVA with “comorbidity/mood or anxiety disorders” (comorbid subgroup and non-comorbid subgroup) and “sex” as factors, and age and BMI as covariates. However, we did not observe main effects or interaction effects on LPA concentrations (Supplementary Table S4, S5).
Plasma concentrations of LPA species in cognitive impairments in abstinent alcohol patients
We investigated cognitive functioning following chronic alcohol consumption, in memory assessed by MFE scale and in the frontal lobe assessed by FAB scale, in plasma concentrations of total LPA and LPA species in the AUD group.
The AUD group showed a MFE score mean of 29.25 ± 16.47, indicating no deficits related in memory impairment. Moreover, a FAB score mean in AUD group was 15.25 ± 2.23, indicating a mild deficit in frontal lobe assessment (dysexecutive syndrome). Correlation analyses using Spearman correlation (rho) were performed in plasma concentrations of total LPA and LPA species with MFE and FAB scores, respectively (see Supplementary Table S6). In addition, a negative correlation was found between the MFE scores and FAB scores FAB scores (r = − 0.493, p < 0.001).
As shown in Fig. 2, there were significant and positive correlations between the executive tasks evaluated with FAB scores and the plasma concentrations of total LPA, and the plasma concentrations of 16:0-LPA, 18:1-LPA and 20:4-LPA species. It is important to note that all the correlation analyses were double checked using a bootstrapped approach technique, and the Spearman correlation between total FAB and 18:0-LPA was not robust enough to be taken as a significant correlation result. Despite this fact, there were positive correlations between the executive tasks and other LPA species determined except for 18:0-LPA and 18:2-LPA. By contrast, we found no associations between memory impairments assessed with MFE and plasma concentrations of LPA species in the alcohol group. These data suggest a significant association between executive functions and circulating LPA species in the AUD group.
Correlations between LPA species and FAB scores in AUD group controlled by age and sex. (A) Total LPA (nmol/L) with FAB scores; (B) 16:0-LPA (nmol/L) with FAB scores; (C) 18:0-LPA (nmol/L) with FAB scores; (D) 18:1-LPA (nmol/L) with FAB scores; (E) 18:2-LPA (nmol/L) with FAB scores; (F) 20:4-LPA (nmol/L) with FAB scores. Dots are individual values. (rho) Spearman’s correlation coefficient; (p) p value for statistical significance.
Correlation of plasma concentrations of LPA species with growth factors
Moreover, correlation analyses using Pearson correlation (r) were performed with the logarithms of plasma concentrations of LPA (total LPA and LPA species) and growth factors (BDNF, IGF-1 and IGF-2, and NT-3) in the AUD group (Supplementary Table S7).
As shown in Fig. 3, the statistical analyses found positive and significant correlations between plasma concentrations of BDNF and total LPA, 18:2-LPA and 20:4-LPA. However, there were no significant correlations between BDNF and 16:0-LPA, 18:0-LPA or 18:1-LPA.
Correlations between LPA species and plasma concentrations of BDNF in AUD patients. (A) log BDNF (nmol/L) with log total LPA (nmol/L); (B) log BDNF (nmol/L) with log 16:0-LPA (nmol/L); (C) log BDNF (nmol/L) with log 18:0-LPA (nmol/L); (D) log 18:1-LPA (nmol/L) with log BDNF (nmol/L); (E) log BDNF (nmol/L) with log 18:2-LPA (nmol/L); (F) log BDNF (nmol/L) with log 20:4-LPA (nmol/L). Dots are individual values. (r) Pearson’s correlation coefficient; (p) p value for statistical significance.
Unlike BDNF, there were negative significant correlations between plasma concentrations of IGF-1 and IGF-2 plasma concentrations with some LPA species (Fig. 4). Specifically, IGF-1 correlated negatively with total LPA and all LPA species, except for 18:0-LPA; while IGF-2 only correlated negatively with 18:2-LPA.
Significant correlations between LPA species and plasma concentrations of IGF-1 in AUD patients. (A) log IGF-1 (nmol/L) log with total LPA (nmol/L); (B) log IGF-1 (nmol/L) with log 16:0-LPA (nmol/L); (C) log IGF-1 (nmol/L) with log 18:1-LPA (nmol/L); (D) log IGF-1 (nmol/L) with log 18:2-LPA (nmol/L); (E) log IGF-1 (nmol/L) with log 20:4-LPA (nmol/L); (F) log IGF-2 (nmol/L) with log 18:1-LPA (nmol/L). Dots are individual values. (r) Pearson’s correlation coefficient; (p) p value for statistical significance.
Discussion
Preclinical studies in animal models of alcohol dependence corroborate the participation of LPA and its LPA1 receptor in the spontaneous alcohol preference and alcohol drinking of mice, as well as in alcohol-associated changes in emotional memory and social/maternal behavior34,42. Another preclinical study using ethanol fed mice has described specific alterations on some fatty acids-related lipids43. These results are in agreement with the present study in AUD patients. Thus, our results showed that abstinent AUD patients displayed lower circulating levels of total LPA, 18:0-LPA and 18:1-LPA when compared with a control group. In addition to the present results, other studies have reported a deregulation of circulating fatty acids in AUD patients41,44, suggesting that fatty acid metabolism including other fatty-acid derived signals might be affected after alcohol exposure. Thus, it has been described higher concentrations of oleic acid in a group of patients with alcohol dependence that in the control group44. Following this rationale, we have recently described that AUD patients have elevated plasma concentrations of SEA and OEA, the stearic acid and oleic acid-derived acylethanolamides respectively involved in energy homeostasis and alcohol consumption41,45. Interestingly, we observed that total LPA and some LPA species, including 16:0-LPA, 18:2-LPA and 20:4-LPA, were affected by sex. Our results are in accordance with previous studies in healthy subjects that have reported sex differences with increased LPA concentrations in women30,35. However, we found differences in LPA concentrations between men and women in the control and AUD groups, suggesting that the presence of a sexual dimorphism in the circulating species of this lipid is not a specific factor associated to the impact of alcohol consumption.
Because our AUD sample displayed a high prevalence of SUDs (41.8%) and mental disorders (63.6%), we also evaluated the existence of a possible association between circulating LPA levels and the presence of SUDs and/or comorbid mental disorders. However, we did not find any significant association, maybe due to the small sample size. The elevated lifetime in psychiatric comorbid disorders in our sample is consistent with other reports in AUD populations46,47. Although we did not find significant differences in LPA plasma profiles between AUD patients with and without comorbid disorders, there is a growing body of evidence about the implication of fatty acids in certain mental disorders. Thus, serum levels of 16:0-LPA are upregulated in patients with major depressive disorders compared with a control group48. Other study show reduced plasma levels of arachidonic acid in bipolar depression patients49 and fatty acid deficiency in postmortem brain tissues samples50. In addition, the role of LPA species in the etiology of several neuropsychiatric disorders through the LPA1 receptor has also been examined both in human and preclinical models. The LPA deregulation has been studied in complex disorder such as schizophrenia in preclinical models31,51 and schizophrenia patients52. Finally, ATX as the primary biological source of LPA, represents a high-value psychiatric condition target53. ATX has been described as a possible biomarker of patients with major depression disorder diagnosis, since the serum levels of this enzyme are reduced in depressive patients compared with healthy controls54.
However, we found a clear association between LPA plasma concentrations and mild cognitive impairment. In our study, the AUD group displayed a mild deficit in tasks related to executive functions according with alcohol-related cognitive impairments. According to our results, executive functions are particularly affected in AUD population, although there are other neuropsychological processes including memory, emotional and psychosocial skills, visuospatial cognition and psychomotor impaired functions altered in alcohol dependence patients55,56. Other studies have reported increased difficulties in motivational processes in addiction treatment patients causing an underestimated impact on the efficacy and management on these clinical treatments14,57. Although there were no significant correlations between LPA plasma concentrations and memory impairments in our results, the negative correlation found between lobe function and memory scores, is consistent with early reports suggesting that general memory dysfunctions are related with other types of memory and to executive performance58. For that reason, it is of great interest the correlation found between 16:0-LPA, 18:0-LPA, 18:1-LPA and 20:4-LPA and the scores obtained in executive function assessment test. These results suggest that some LPA species might be good reliable markers for the detection of executive dysfunction associated with AUD. These findings support previous studies that have described a relation between dysfunctional levels of LPA signaling and neuropsychological impairments. For example, it has been reported that the plasma levels of LPA negatively correlated with mild cognitive impairments assessed with MoCA test in diabetic patients59. Regarding preclinical models, the lack of LPA1 receptor has been associated to cognitive alterations, using spatial memory tasks60,61. Moreover, a molecular study focused on lysophosphatidic acid acyltransferases (LPAATs) group of enzymes involved in the production of phosphatidic acid from LPA, shows that the inhibition of lipid metabolism is associated with physiological consequences such as cognitive dysfunction62.
In the present study, we also evaluated the correlation between the LPA species and growth factors. We found a positive correlation between total plasma concentrations of LPA (or that of polyunsaturated LPA) with circulating levels of the trophic factor BNDF, suggesting that both polyunsaturated LPA species and BDNF might contribute to normal cognitive processing. There is a clear association between the decrease in the circulating levels of these mediators, the impairment of cortical/hippocampal LPA and BDNF signaling, and alcohol associated cognitive impairment18,19,29,42. However, the mechanisms of this association are unknown. A potential interesting mechanism might be associated with neuroinflammatory processes. In this regard, previous studies with polyunsaturated fatty acids (i.e. arachidonic acid and their metabolites) have demonstrated a tight association between their ability to modulate both inflammation and BDNF production63.
Finally, we found that plasma levels of IGF-1 correlated negatively with total LPA, 16:0-LPA, 18:1-LPA, 18:2-LPA and 20:4-LPA and IGF-2 correlated negatively with 18:1-LPA. Previous studies have reported that insulin-like growth factors (i.e., IGF-1 and IGF-2) are associated with the maintenance of the cognitive functioning specially in attention and executive functions64,65. However since these growth factors are also decreased by alcohol, but they do not correlate with cognitive impairment or with comorbid mental disorders17, it is difficult to determine the nature of this association. One possible explanation might be derived of the shift on liver metabolism imposed by alcohol. Alcohol-associated cognitive impairment in the IGF-1 signaling could be a potential mechanism in the neuroinflammatory processes.
Limitations of the present study
These finding described an important effect of alcohol consumption on LPA plasma concentrations, as well as an important association with executive functions and cognitive impairment. Moreover, we are aware about the existence of limitations in the present observational study. First, the recruitment of the sample was conducted from outpatient programs and there are uncontrolled social and environmental variables (e.g., diet, medication control) that could affect the validity of the results. Second, larger samples of male and female AUD patients and additional experimental groups should be included (e.g., patients with mental disorders but without substance use disorders for analyzing in depth the contribution of LPA to alcohol-induced brain damage). Third, longitudinal studies are also needed to monitor changes in these metabolites during abstinence at different times in the same patients. Finally, because a high percentage of AUD patients were under different pharmacological treatment, we cannot exclude the influence of specific medications on the circulating concentrations of the different LPA species.
Conclusions
In agreement with previous preclinical studies supporting a role of the fatty acid related lipids and the lysophosphatidic acid receptor 1 (LPA1) in alcohol consumption34,42,43, the present results further suggest that LPA species are lipid mediators associated with AUD. The main findings of this study indicate that (a) The total circulating concentration of LPA, 16:0-LPA, 18:0-LPA and 18:1-LPA were decreased in the AUD group when compared to the control group; (b) The total circulating concentration of LPA, 16:0-LPA, 18:2-LPA and 20:4-LPA were decreased in men compared to women (c) The plasma concentrations of the LPA species were not significantly affected by the presence of lifetime comorbid mood and anxiety disorders; (d) In the AUD group, 22% of the patients had cognitive deficits related to executive functions, while 32.6% displayed deficits related to memory impairments; (e) The executive tasks scores of the AUD group correlated with plasma concentrations of total LPA, 16:0-LPA, 18:1-LPA and 20:4-LPA; (f) There is a clear positive correlation between plasma concentrations of BDNF and total LPA, 18:2-LPA and 20:4-LPA; (g) There is a strong inverse correlation between IGF-1 and total LPA, 16:0-LPA, 18:1-LPA, 18:2-LPA and 20:4-LPA. Overall, these data suggest that LPA species are affected by chronic alcohol consumption, and they are associated with cognitive impairments similar to trophic factors such as BDNF18.
References
Whiteford, H. A., Ferrari, A. J., Degenhardt, L., Feigin, V. & Vos, T. The global burden of mental, neurological and substance use disorders: An analysis from the Global Burden of Disease Study 2010. PLoS One 10, e0116820. https://doi.org/10.1371/journal.pone.0116820 (2015).
WHO. Global Status Report on Alcohol and Health 2018: Executive Summary (WHO, Geneva, 2018).
Louvet, A. & Mathurin, P. Alcoholic liver disease: Mechanisms of injury and targeted treatment. Nat. Rev. Gastroenterol. Hepatol. 12, 231–242. https://doi.org/10.1038/nrgastro.2015.35 (2015).
Hayes, V., Demirkol, A., Ridley, N., Withall, A. & Draper, B. Alcohol-related cognitive impairment: Current trends and future perspectives. Neurodegener. Dis. Manag. 6, 509–523. https://doi.org/10.2217/nmt-2016-0030 (2016).
Hasin, D. S. & Grant, B. F. The co-occurrence of DSM-IV alcohol abuse in DSM-IV alcohol dependence: Results of the National Epidemiologic Survey on Alcohol and Related Conditions on heterogeneity that differ by population subgroup. Arch. Gen. Psychiatry 61, 891–896. https://doi.org/10.1001/archpsyc.61.9.891 (2004).
Schwarzinger, M. et al. Contribution of alcohol use disorders to the burden of dementia in France 2008–13: A nationwide retrospective cohort study. Lancet Public Health 3, e124–e132. https://doi.org/10.1016/S2468-2667(18)30022-7 (2018).
Weitlauf, C. & Woodward, J. J. Ethanol selectively attenuates NMDAR-mediated synaptic transmission in the prefrontal cortex. Alcohol Clin. Exp. Res. 32, 690–698. https://doi.org/10.1111/j.1530-0277.2008.00625.x (2008).
Boden, J. M. & Fergusson, D. M. Alcohol and depression. Addiction 106, 906–914. https://doi.org/10.1111/j.1360-0443.2010.03351.x (2011).
Samet, S. et al. Effects of independent and substance-induced major depressive disorder on remission and relapse of alcohol, cocaine and heroin dependence. Addiction 108, 115–123. https://doi.org/10.1111/j.1360-0443.2012.04010.x (2013).
Garcia Marchena, N. et al. Psychiatric comorbidity and plasma levels of 2-acyl-glycerols in outpatient treatment alcohol users. Analysis of gender differences. Adicciones 29, 83–96. https://doi.org/10.20882/adicciones.728 (2016).
Sanvisens, A. et al. Patients with alcohol use disorder: Initial results from a prospective multicenter registry in the Spanish Network on Addiction Disorders. CohRTA Study. Adicciones 30, 292–300. https://doi.org/10.20882/adicciones.931 (2018).
Bates, M. E., Voelbel, G. T., Buckman, J. F., Labouvie, E. W. & Barry, D. Short-term neuropsychological recovery in clients with substance use disorders. Alcohol Clin. Exp. Res. 29, 367–377 (2005).
Mukherjee, S. Alcoholism and its effects on the central nervous system. Curr. Neurovasc. Res. 10, 256–262 (2013).
Cabe, N. et al. Cognitive impairments in alcohol dependence: From screening to treatment improvements. Encephale 42, 74–81. https://doi.org/10.1016/j.encep.2015.12.012 (2016).
Pitel, A. L. et al. Genuine episodic memory deficits and executive dysfunctions in alcoholic subjects early in abstinence. Alcohol Clin. Exp. Res. 31, 1169–1178. https://doi.org/10.1111/j.1530-0277.2007.00418.x (2007).
Oscar-Berman, M. & Marinkovic, K. Alcohol: Effects on neurobehavioral functions and the brain. Neuropsychol. Rev. 17, 239–257. https://doi.org/10.1007/s11065-007-9038-6 (2007).
Garcia-Marchena, N. et al. Decreased plasma concentrations of BDNF and IGF-1 in abstinent patients with alcohol use disorders. PLoS One 12, e0187634. https://doi.org/10.1371/journal.pone.0187634 (2017).
Silva-Pena, D. et al. Alcohol-induced cognitive deficits are associated with decreased circulating levels of the neurotrophin BDNF in humans and rats. Addict. Biol. 24, 1019–1033. https://doi.org/10.1111/adb.12668 (2019).
Silva-Pena, D. et al. Oleoylethanolamide modulates BDNF-ERK signaling and neurogenesis in the hippocampi of rats exposed to delta(9)-THC and ethanol binge drinking during adolescence. Front. Mol. Neurosci. 12, 96. https://doi.org/10.3389/fnmol.2019.00096 (2019).
Estivill-Torrus, G. et al. Absence of LPA1 signaling results in defective cortical development. Cereb. Cortex 18, 938–950. https://doi.org/10.1093/cercor/bhm132 (2008).
Castilla-Ortega, E. et al. 1-Oleoyl lysophosphatidic acid: A new mediator of emotional behavior in rats. PLoS One 9, e85348. https://doi.org/10.1371/journal.pone.0085348 (2014).
Yamada, M. et al. Lysophosphatidic acid induces anxiety-like behavior via its receptors in mice. J. Neural. Transm. (Vienna) 122, 487–494. https://doi.org/10.1007/s00702-014-1289-9 (2015).
Eichholtz, T., Jalink, K., Fahrenfort, I. & Moolenaar, W. H. The bioactive phospholipid lysophosphatidic acid is released from activated platelets. Biochem. J. 291(Pt 3), 677–680. https://doi.org/10.1042/bj2910677 (1993).
Sano, T. et al. Multiple mechanisms linked to platelet activation result in lysophosphatidic acid and sphingosine 1-phosphate generation in blood. J. Biol. Chem. 277, 21197–21206. https://doi.org/10.1074/jbc.M201289200 (2002).
Tigyi, G. Aiming drug discovery at lysophosphatidic acid targets. Br. J. Pharmacol. 161, 241–270. https://doi.org/10.1111/j.1476-5381.2010.00815.x (2010).
Yung, Y. C., Stoddard, N. C. & Chun, J. LPA receptor signaling: Pharmacology, physiology, and pathophysiology. J. Lipid Res. 55, 1192–1214 (2014).
Choi, J. W. & Chun, J. Lysophospholipids and their receptors in the central nervous system. Biochim. Biophys. Acta Mol. Cell. Biol. Lipids 1831, 20–32 (2013).
Zheng, Z. Q., Fang, X. J. & Qiao, J. T. Dual action of lysophosphatidic acid in cultured cortical neurons: Survival and apoptogenic. Sheng Li Xue Bao 56, 163–171 (2004).
Matas-Rico, E. et al. Deletion of lysophosphatidic acid receptor LPA1 reduces neurogenesis in the mouse dentate gyrus. Mol. Cell. Neurosci. 39, 342–355. https://doi.org/10.1016/j.mcn.2008.07.014 (2008).
Michalczyk, A., Budkowska, M., Dołęgowska, B., Chlubek, D. & Safranow, K. Lysophosphatidic acid plasma concentrations in healthy subjects: Circadian rhythm and associations with demographic, anthropometric and biochemical parameters. Lipids Health Dis. 16, 140. https://doi.org/10.1186/s12944-017-0536-0 (2017).
Mirendil, H. et al. LPA signaling initiates schizophrenia-like brain and behavioral changes in a mouse model of prenatal brain hemorrhage. Transl. Psychiatry 5, e541. https://doi.org/10.1038/tp.2015.33 (2015).
Herr, K. J., Herr, D. R., Lee, C. W., Noguchi, K. & Chun, J. Stereotyped fetal brain disorganization is induced by hypoxia and requires lysophosphatidic acid receptor 1 (LPA1) signaling. Proc. Natl. Acad. Sci. USA 108, 15444–15449. https://doi.org/10.1073/pnas.1106129108 (2011).
Moreno-Fernandez, R. D. et al. Stress, depression, resilience and ageing: A role for the LPA-LPA1 pathway. Curr. Neuropharmacol. 16, 271–283. https://doi.org/10.2174/1570159X15666170710200352 (2018).
Castilla-Ortega, E. et al. Both genetic deletion and pharmacological blockade of lysophosphatidic acid LPA1 receptor results in increased alcohol consumption. Neuropharmacology 103, 92–103. https://doi.org/10.1016/j.neuropharm.2015.12.010 (2016).
Hosogaya, S. et al. Measurement of plasma lysophosphatidic acid concentration in healthy subjects: Strong correlation with lysophospholipase D activity. Ann. Clin. Biochem. 45, 364–368. https://doi.org/10.1258/acb.2008.007242 (2008).
APA. DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, Text Revision 78–85 (American Psychiatric Association, Washington, DC, 2000).
Torrens, M., Serrano, D., Astals, M., Perez-Dominguez, G. & Martin-Santos, R. Diagnosing comorbid psychiatric disorders in substance abusers: Validity of the Spanish versions of the Psychiatric Research Interview for Substance and Mental Disorders and the Structured Clinical Interview for DSM-IV. Am. J. Psychiatry 161, 1231–1237. https://doi.org/10.1176/appi.ajp.161.7.1231 (2004).
Hasin, D. et al. Diagnosis of comorbid psychiatric disorders in substance users assessed with the Psychiatric Research Interview for Substance and Mental Disorders for DSM-IV. Am. J. Psychiatry 163, 689–696. https://doi.org/10.1176/ajp.2006.163.4.689 (2006).
Rodriguez del Alamo, A., Catalan Alonso, M. J. & Carrasco Marin, L. FAB: A preliminar Spanish application of the frontal assessment battery to 11 groups of patients. Rev. Neurol. 36, 605–608 (2003).
Lozoya-Delgado, P., Ruiz-Sánchez de León, J. M. & Pedrero-Pérez, E. J. Validación de un cuestionario de quejas cognitivas para adultos jóvenes: Relación entre las quejas subjetivas de memoria, la sintomatología prefrontal y el estrés percibido. Rev. Neurol. 54, 137–150 (2012).
Garcia-Marchena, N. et al. Plasma concentrations of oleoylethanolamide and other acylethanolamides are altered in alcohol-dependent patients: Effect of length of abstinence. Addict. Biol. 22, 1366–1377. https://doi.org/10.1111/adb.12408 (2017).
Sanchez-Marin, L. et al. Systemic blockade of LPA1/3 lysophosphatidic acid receptors by ki16425 modulates the effects of ethanol on the brain and behavior. Neuropharmacology 133, 189–201. https://doi.org/10.1016/j.neuropharm.2018.01.033 (2018).
Zhao, Z., Yu, M., Crabb, D., Xu, Y. & Liangpunsakul, S. Ethanol-induced alterations in fatty acid-related lipids in serum and tissues in mice. Alcohol. Clin. Exp. Res. 35, 229–234. https://doi.org/10.1111/j.1530-0277.2010.01338.x (2011).
Teubert, A., Thome, J., Büttner, A., Richter, J. & Irmisch, G. Elevated oleic acid serum concentrations in patients suffering from alcohol dependence. J. Mol. Psychiatry 1, 13 (2013).
Bilbao, A. et al. Role of the satiety factor oleoylethanolamide in alcoholism. Addict. Biol. 21, 859–872. https://doi.org/10.1111/adb.12276 (2016).
Hasin, D. S., Stinson, F. S., Ogburn, E. & Grant, B. F. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry 64, 830–842. https://doi.org/10.1001/archpsyc.64.7.830 (2007).
Saha, T. D. et al. Concurrent use of alcohol with other drugs and DSM-5 alcohol use disorder comorbid with other drug use disorders: Sociodemographic characteristics, severity, and psychopathology. Drug Alcohol Depend. 187, 261–269. https://doi.org/10.1016/j.drugalcdep.2018.03.006 (2018).
Kim, E. Y. et al. Serum lipidomic analysis for the discovery of biomarkers for major depressive disorder in drug-free patients. Psychiatry Res. 265, 174–182. https://doi.org/10.1016/j.psychres.2018.04.029 (2018).
Chiu, C. C. et al. Polyunsaturated fatty acid deficit in patients with bipolar mania. Eur. Neuropsychopharmacol. 13, 99–103 (2003).
McNamara, R. K. et al. Deficits in docosahexaenoic acid and associated elevations in the metabolism of arachidonic acid and saturated fatty acids in the postmortem orbitofrontal cortex of patients with bipolar disorder. Psychiatry Res. 160, 285–299. https://doi.org/10.1016/j.psychres.2007.08.021 (2008).
Roberts, C. et al. Neurochemical changes in LPA1 receptor deficient mice—a putative model of schizophrenia. Neurochem. Res. 30, 371–377. https://doi.org/10.1007/s11064-005-2611-6 (2005).
Gotoh, L. et al. Levels of lysophosphatidic acid in cerebrospinal fluid and plasma of patients with schizophrenia. Psychiatry Res. 273, 331–335. https://doi.org/10.1016/j.psychres.2019.01.052 (2019).
Herr, D. R., Chew, W. S., Satish, R. L. & Ong, W. Y. Pleotropic roles of autotaxin in the nervous system present opportunities for the development of novel therapeutics for neurological diseases. Mol. Neurobiol. https://doi.org/10.1007/s12035-019-01719-1 (2019).
Itagaki, K. et al. Reduced serum and cerebrospinal fluid levels of autotaxin in major depressive disorder. Int. J. Neuropsychopharmacol. 22, 261–269. https://doi.org/10.1093/ijnp/pyz005 (2019).
Sullivan, E. V., Harris, R. A. & Pfefferbaum, A. Alcohol’s effects on brain and behavior. Alcohol Res. Health 33, 127–143 (2010).
Oscar-Berman, M. et al. Profiles of impaired, spared, and recovered neuropsychologic processes in alcoholism. Handb. Clin. Neurol. 125, 183–210. https://doi.org/10.1016/B978-0-444-62619-6.00012-4 (2014).
Bernardin, F., Maheut-Bosser, A. & Paille, F. Cognitive impairments in alcohol-dependent subjects. Front. Psychiatry 5, 78. https://doi.org/10.3389/fpsyt.2014.00078 (2014).
Montejo, ÁL. & Rico-Villademoros, F. Psychometric properties of the Psychotropic-Related Sexual Dysfunction Questionnaire (PRSexDQ-SALSEX) in patients with schizophrenia and other psychotic disorders. J. Sex Marital Ther. 34, 227–239 (2008).
Zhang, J. B. et al. Plasma phospholipids are associated with mild cognitive impairment in type 2 diabetic patients. Curr. Alzheimer Res. 14, 592–597. https://doi.org/10.2174/1567205013666161201200722 (2017).
Santin, L. J. et al. Behavioral phenotype of maLPA1-null mice: Increased anxiety-like behavior and spatial memory deficits. Genes Brain Behav. 8, 772–784. https://doi.org/10.1111/j.1601-183X.2009.00524.x (2009).
Castilla-Ortega, E. et al. Aggravation of chronic stress effects on hippocampal neurogenesis and spatial memory in LPA(1) receptor knockout mice. PLoS One 6, e25522. https://doi.org/10.1371/journal.pone.0025522 (2011).
Bradley, R. M. & Duncan, R. E. The lysophosphatidic acid acyltransferases (acylglycerophosphate acyltransferases) family: One reaction, five enzymes, many roles. Curr. Opin. Lipidol. 29, 110–115. https://doi.org/10.1097/MOL.0000000000000492 (2018).
Das, U. N. Is there a role for bioactive lipids in the pathobiology of diabetes mellitus?. Front Endocrinol. (Lausanne) 8, 182. https://doi.org/10.3389/fendo.2017.00182 (2017).
Alfimova, M. V., Lezheĭko, T. V., Gritsenko, I. K. & Golimbet, V. E. Association of the insulin-like growth factor II (IGF2) gene with human cognitive functions. Genetika 48, 993–998 (2012).
Green, C. J. et al. The role of IGF-I, IGF-II, and IGFBP-3 in male cognitive aging and dementia risk: The Caerphilly Prospective Study. J. Alzheimer’s Dis. 41, 867–875. https://doi.org/10.3233/jad-132183 (2014).
Acknowledgements
The authors are grateful to G. Rubio, F. Arias, M. Soria and J.J. Ruiz for their valuable assistance throughout the clinical part of the study.
Funding
The present study has been supported by the following programs and research projects: Subprograma Redes Temáticas RETICS (Red de Trastornos Adictivos RD16/0017/001 and RD12/0028/0021) funded by Instituto de Salud Carlos III (ISCIII), Ministerio de Economía y Competitividad (MINECO) and the European Regional and European Regional Development Funds/European Social Fund (ERDF/ESF); Proyectos de Investigación en Salud (PI16/01953, PI16/01698 and PI17/02026) funded by ISCIII and ERDF/ESF; Proyectos de Investigación en Drogodependencias (PND2017/043, PND2018/033, PND2018/044 and PND2019/040) funded by Delegación del Gobierno para el Plan Nacional sobre Drogas, Ministerio de Sanidad, Secretaría de Estado de Sanidad and ERDF/ESF; Proyecto de Investigación en Salud (PI-0140-2018) funded by Consejería de Salud y Bienestar Social, Junta de Andalucía and ERDF/ESF. NGM holds a “Sara Borrell” research contract (CD19/00019) funded by ISCIII and ERDF/ESF. FJP, AS and JS hold a “Miguel Servet II” research contract (CPII19/00022, CPII19/00031 and CPII17/00024, respectively) funded by ISCIII and ERDF/ESF. RTF holds a Grant (2017 SGR 138) funded by Departament d’Economia i Coneixement de la Generalitat de Catalunya (CIBEROBN), ISCIII and ERDF/ESF.
Author information
Authors and Affiliations
Contributions
R.D.T., F.R.F. and A.S. were responsible for the study concept and design. N.G.M. and F.J.P. performed the statistical analysis and the interpretation of findings. N.G.M., N.P., A.S. and F.R.F. drafted the manuscript. M.F.L., N.R.O., P.A. and D.S.P. coordinated the recruitment of the participants in the study and contributed to the acquisition of psychiatric and neuropsychological data by means of the interviews and generated the database. N.P., M.M. and R.D.T. supervised and performed the quantification of LPA species in the human samples; F.J.P. and J.S. supervised and performed the quantification of the growth factors in the human samples. L.S., F.R.F. and A.S. provide critical revision of the manuscript from important intellectual content. All authors critically reviewed the content and approved the final version for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
García-Marchena, N., Pizarro, N., Pavón, F.J. et al. Potential association of plasma lysophosphatidic acid (LPA) species with cognitive impairment in abstinent alcohol use disorders outpatients. Sci Rep 10, 17163 (2020). https://doi.org/10.1038/s41598-020-74155-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-74155-0
- Springer Nature Limited
This article is cited by
-
LPA1 receptors in the lateral habenula regulate negative affective states associated with alcohol withdrawal
Neuropsychopharmacology (2023)
-
Plasma concentrations of lysophosphatidic acid and the expression of its receptors in peripheral blood mononuclear cells are altered in patients with cocaine use disorders
Translational Psychiatry (2023)