Abstract
Nonsurgical periodontal therapy with adjunctive use of systemic antimicrobials (for 7–14 days) showed improved clinical, microbiological and immunological results over the mechanical protocol alone. Considering the increasing risk for antimicrobial resistance with longer antibiotic regimes, it is important to establish the optimal antibiotic protocol with a maximum antimicrobial benefit and minimum risk for adverse effects. The aim of the study was to evaluate the microbiological and inflammatory outcomes 12-months after a 3-/7-day systemic antibiotic protocol [amoxicillin (AMX) + metronidazole (MET)] adjunctive to subgingival debridement in severe periodontitis compared to mechanical treatment alone. From the initially treated 102 patients, 75 subjects (Placebo group: n = 26; 3-day AMX + MET group: n = 24; 7-day AMX + MET group: n = 25) completed the 12-month examination. Clinical parameters, eight periodontal pathogens and inflammatory markers were determined at baseline and 3-, 6-, 12-months after therapy using real-time PCR and ELISA respectively. After 6 months, several periodontopathogens were significantly more reduced in the two antibiotic groups compared to placebo (p < 0.05). After 1 year, both antibiotic protocols showed significant reductions and detection of the keystone pathogen P. gingivalis compared to placebo. Antibiotic protocols, smoking, disease severity, baseline-BOP, -CAL and -IL-1β, as well as detection of T. denticola at 12-months significantly influenced the residual number of deep sites. The present data indicate that the systemic use of both short and longer antibiotic protocols (AMX + MET) adjunctive to nonsurgical periodontal therapy lead to higher microbiological improvements compared to subgingival debridement alone. The two investigated antibiotic protocols led to comparable microbiological and inflammatory results.
Similar content being viewed by others
Introduction
Since periodontitis is a biofilm-induced inflammatory multifactorial chronic disease, periodontal treatment aims at reducing the supra- and subgingival biofilm by institution of an adequate oral hygiene and meticulous debridement of the roots (i.e. subgingival debridement-SD) in order to resolve tissue inflammation and arrest disease progression1. Despite the fact that SD has been shown to be successful in reducing periodontal pathogens in the subgingival area2,3, evidence exists that major periodontal pathogens like Aggregatibacter actinomycetemcomitans or Porphyromonas gingivalis may not be completely eliminated by mechanical debridement alone and their persistence has been associated with further tissue breakdown4,5,6. Vice versa, the absence of certain periodontal pathogens has been associated with lower risk for further attachment-loss7,8,9. Consequently, systemic antimicrobials had been introduced in the late 80ies as adjuncts to mechanical debridement to reinforce SD and sustain the host-defence system by reaching the pathogens not always accessible for mechanical instruments (i.e. root-concavities, furcations) or in other mouth areas (i.e. pharynx, tongue)10.
In this sense, several antimicrobials and various combinations thereof had been implemented in the non-surgical periodontal treatment showing improved clinical, microbiological and immunological results over the mechanical protocol alone11,12,13,14,15. The use of a combination of amoxicillin (AMX) and metronidazole (MET) dominates the literature in this topic14,15,16, indicating a synergistic efficiency against gram-negative anaerobes in particular17,18,19,20,21. Statistically significantly better clinical outcomes regarding probing pocket depth (PD) reduction and clinical attachment level (CAL) gain11,13,22,23,24,25,26,27,28,29,30,31,32,33 as well as significant reduction of periodontal pathogens and of inflammatory cytokines were observed for the systemic use of AMX + MET adjunctive to SD compared to mechanical treatment alone22,23,24,25,26,27,28,29,30,31,32,34,35. However, it is important to emphasize that for initially shallow (PD < 4 mm) and moderate (PD 4–5 mm) sites in patients with chronic periodontitis, the adjunctive use of AMX + MET has been shown to have only minimal additional clinical benefits (PD reduction and CAL gain)13,36. On the other hand, initially deep sites (PD > 6 mm) have demonstrated substantial additional clinical improvements (i.e. 0.74 mm PD reduction and 0.61 mm CAL gain after 12 months)13, thus decreasing significantly the need for subsequent surgical periodontal therapy22,25,30,37. Moreover, it has been shown that patients taking the antimicrobials at the initial phase of the periodontal treatment, exhibited significantly greater clinical improvements in initially deep sites compared to those taking the antimicrobials after healing or at the second stage25,37.
Despite the abundance of studies on AMX + MET in non-surgical periodontal therapy, there seems to be no consensus regarding the optimal dosage and duration of the medication: doses of each of the antimicrobials range from 200 to 500 mg for durations of 3–14 days20,21,22,23,24,25,26,27,28,29,30,32,33,38,39,40,41. In the light of an increasing risk for antimicrobial resistance with longer antibiotic regimes, it is important to establish the optimal antibiotic protocol with a maximum antimicrobial benefit and minimum risk for adverse events (i.e. antibiotic resistance, hypersensitivity, renal/liver toxicity, e.t.c). This has to consider the pharmacological principle that antimicrobials should be taken in a minimum bactericidal concentration for a minimum duration42 and is in concordance with the current worldwide concern regarding the critical levels of antibiotic resistance as a result of the indiscriminative use of antimicrobials12,43,44. Since the discovery of antimicrobials in the 1940s, the abundance of antibiotic-resistant genes has significantly increased45. Evidence also indicates that oral microbiota represent a reservoir for transferable antimicrobial resistant genes46,47,48,49 having the potential to transfer antimicrobial resistance in patients undergoing antibiotic therapy as well50. Thus, it seems mandatory, that not only in various field of general medicine the antibiotic prescription and protocol should be reanalysed and clearly defined51, but also in dentistry and especially in periodontal therapy there is an urgent need to establish the optimal antibiotic protocol and the class of patients that may really benefit from it.
Studies evaluating the clinical, microbiological and immunological efficacy of a short-term administration of AMX + MET compared to the standard protocol (e.g. use for at least 7 days) in non-surgical periodontal therapy are scarce. Lately, we have evaluated the clinical outcomes at 6 and 12 months of a 3-day regimen of AMX + MET adjunctive to SD in severe chronic periodontitis showing that both antibiotic protocols (3 and 7 days) led to statistically significant better clinical improvements compared to SD alone33,41. The aim of the present analysis, was therefore to evaluate the microbiological and inflammatory biomarkers outcomes following non-surgical periodontal therapy in conjunction with systemic administration of AMX + MET for 3 or 7 days in patients with severe chronic periodontitis (stage III–IV, grade B periodontitis). The present article represents the microbiological and inflammatory analyses of a previous RCT33,41.
Results
Patients
Hundred two subjects (mean age 43.37 ± 9.85, 65 female, 35 smokers, n = 34/group) were enrolled in the study and 27 patients dropped-out at the 12-month evaluation. Reasons for exclusion from the final analysis were antibiotic intake for other medical reasons, non-compliance with the appointments schedule and moved out of town. No statistically significant differences (p > 0.05) between the groups were detectable at baseline (i.e. for gender distribution, smoking status, clinical parameters: PD, CAL, BOP, FMPS, number of deep sites with PD ≥ 6 mm, e.t.c.) (Table 1 in Cosgarea et al.)33. Excellent patient compliance with the pills intake and only minor adverse events were registered in all three treatment groups33. The main outcomes at 12 months indicated statistically significantly better clinical improvements (i.e. PD-reduction, CAL-gain) for the 7-day antimicrobial-protocol as compared to placebo, while statistically significantly fewer residual deep sites (PD ≥ 6 mm) were present in the 3-day Antimicrobial-group as compared to placebo41. Additionally, statistically significantly more patients reached a periodontal status with low risk for disease progression (≤ 4 sites with PD ≥ 5 mm) in the two antimicrobial-groups as compared to placebo41.
Microbiological results
Detection of the main periodontal pathogens A. actinomycetemcomitans and P. gingivalis as related to their presence/absence prior treatment are presented in Table 1. A. actinomycetemcomitans was detectable at 6 and 12 months in a higher number of patients in the placebo group as opposed to the antimicrobial-groups (group B and C); moreover, antimicrobials were not able to completely eradicate (i.e. below the detection limit) this periodontal pathogen in neither of the antimicrobial-groups. Similar observations were seen for P. gingivalis (Table 1).
Nonetheless, patients initially positive on P. gingivalis showed at 6 months statistically significantly fewer residual deep sites (PD ≥ 6 mm) in the two antimicrobial-groups compared to the placebo group (p < 0.05); this was maintained up to 12 months in the 3-day antimicrobial-group (p < 0.05) (Table 2). Significantly more treated sites resulted in pocket closure (PD < 4 mm) at 6 months in the two antimicrobial-groups compared to placebo (p < 0.05, Table 2). The 3-day antimicrobial-group showed significantly more (p = 0.044) healed sites compared to placebo also at 12 months. However, no statistically significant differences were obtained between the two groups receiving antimicrobials (p > 0.05). Only patients positive on P. gingivalis at 6 months had statistically significantly more deep sites in the placebo group as opposed to the 3-day antimicrobial-group (p = 0.001).
Both initially negative and positive patients for A. actinomycetemcomitans showed at 6 months statistically significantly less deep sites in the two antimicrobial-groups compared to placebo. Nonetheless, only those initially negative had at 12 months still significantly less deep sites in the 3-day -group compared to placebo (Table 2). Similar findings were observed for the patients negative for A. actinomycetemcomitans at 6/12 months.
Patients initially negative on T. denticola had significantly less deep sites at 6 and 12 months in the 3-day antimicrobial-group compared to placebo, while those in the 7-day antimicrobial-group showed only at 6 months significantly less such sites. Subjects positive on T. denticola at 6 months had in both antimicrobial-groups significantly less deep sites than placebo, while at those positive at 12 months showed a borderline significance (p = 0.05) for the 3-day antimicrobial-group (Table 2).
Initial presence or absence (prior treatment) or at the follow-ups of A. actinomycetemcomitans, P. gingivalis or T. denticola did not have any influence on the number of sites reaching pocket closure neither at 6 nor at 12 months (Table 2).
At 12 months compared to baseline, quantitative microbial analyses showed statistically significant reductions in the proportions of P. gingivalis, T. forsythia, C. rectus and F. allocis in all treatment groups (Table 3). T. denticola was statistically significantly reduced at 12 months compared to baseline only in the antimicrobial-groups, while A. actinomycetemcomitans was reduced only in the 7-day antimicrobial-group and only at the 6 months evaluation; at 12 months, there were no significant reductions compared to baseline in none of the groups (p > 0.05). Nonetheless, group comparisons revealed no significant quantitative differences at baseline for neither of the microorganisms, with the exception of A. actinomycetemcomitans, which was present in significantly higher quantities in the placebo compared to the 3-day group (Table 3). Following, at 12 months, statistically significantly higher reductions in the mean counts of the P. gingivalis were seen in both antimicrobial-groups compared to placebo. F. nucleatum and F. allocis were statistically significantly reduced only in the 7-day AB group compared to placebo. Neither at 6 nor at 12 months, no statistically significant differences were seen between the two antibiotic groups for any of the microorganisms (p > 0.05, Table 2).
At 12 months statistically significantly, less patients were positive on P. gingivalis and F. allocis compared to baseline in the two antimicrobial-groups (Table 4), while T. denticola was less detectable in all treatment groups (p < 0.05). Detection of A. actinomycetemcomitans did not show any statistically significant reduction in any of the treatment groups neither at 6 nor at 12 months (p > 0.05, Table 4). Group comparisons revealed that even if at 6 months several bacteria (P. gingivalis, T. denticola, T. forsythia, F. nucleatum, C. rectus, F. allocis) were statistically significantly less detectable in the 7-day antimicrobial-group compared to placebo, at 12 months no significant differences were registered between the groups. Only P. gingivalis was significantly less detectable in both antimicrobial-groups compared to placebo while F. allocis only in the 7-day antimicrobial-group (Table 4).
Immunomarkers
Compared to baseline, IL-1β was statistically significantly reduced at 3 and 6 months in the two antimicrobial-groups. However, this was maintained up to 12 months only in the 7-day AB (Table 5). Nonetheless, at baseline, statistically significantly higher counts of IL-1β were detected in group C compared to the control group. At 12 months, only MMP-8 was statistically significantly reduced in the 7-day antimicrobial-group. Intergroup comparisons revealed no statistically significant differences between the three groups at 12 months (Table 5).
Table 6 depicts the results of the Poisson regression analyses showing that antimicrobials, female gender, smoking status, severe forms periodontitis (≥ 10 sites with PD ≥ 6 mm at baseline) and initial CAL-loss, BOP at baseline, detection of A. actinomycetemcomitans and T. denticola at 12 months as well as initial detection if IL-1β statistically significantly influenced the residual number of deep sites at 12 months (p < 0.05).
Discussion
The present analyses have evaluated the effect of two systemic antibiotic protocols adjunctive to SD over SD alone on the microbial and inflammatory parameters. Furthermore, the clinical efficacy in terms of pocket closure (PD < 4 mm) and residual deep sites (PD ≥ 6 mm) at 12 months as related to the presence/absence of P. gingivalis, T. denticola and A. actinomycetemcomitans prior to treatment or at follow-ups was also assessed.
At 6 months, all three treatment protocols succeeded in reducing significantly the counts of P. gingivalis, T. forsythia, T. denticola, P. micra and F. allocis. However, these substantial bacterial load reductions were maintained up to 12 months in all three groups only for P. gingivalis, T. forsythia and F. alocis. The pathogens T. denticola, P. micra and F. nucleatum were still statistically significantly reduced after 1 year only in the two antimicrobial-groups. Moreover, the quantitative reductions of the keystone pathogen P. gingivalis were statistically significantly higher at all timepoints in the two antimicrobial-groups as compared to placebo. Considering the fact that the baseline plaque-scores did not differ statistically significantly between the three treatment groups41, the better microbial outcomes for the antimicrobial-groups may probably be attributed to the systemic intake of antimicrobials and not to a supra- and subgingival manual biofilm reduction. These results corroborate to those of other studies, where AMX + MET led to statistically significantly higher reductions of the bacterial counts of P. gingivalis, T. forsythia or T. denticola after 3, 6 and/or 12 months18,23,52,53,54,55.
Contrary to the findings of other research groups54,55, A. actinomycetemcomitans could not be significantly reduced in any of the groups at 12 months. This may be related to differences in detection methods (i.e. culturing techniques, checkerboard DNA-DNA hybridisation vs. rtPCR)55. However, significant quantitative reductions of A. actinomycetemcomitans were observed at 3 and 6 months respectively only in the AB groups, being in line with reports of other authors23,53,56. Moreover, confirming our results, Eick et al.52, showed no statistically significant reduction of A. actinomycetemcomitans after 3–6 months after SD with systemic AMX + MET (each 500 mg 3TID for 7 days) neither in patients with chronic nor aggressive periodontitis.
At 12 months, antimicrobials were not able to supress A. actinomycetemcomitans or P. gingivalis below the detection limit. Almost half of the subjects initially positive on P. gingivalis were still positive at 12 months in the two antimicrobial-groups, while 82% of the patients in the placebo group were still positive. The discrepancy between the groups was smaller for A. actinomycetemcomitans. These results are in line with those of Eick et al.52, showing at 3–6 months post-therapeutically statistically significant reductions of several periodontal pathogens (i.e. P. gingivalis, T. forsythia, T. denticola, P. intermedia, e.t.c.) except for A. actinomycetemcomitans. Despite the fact that statistically significant reductions were detected for these pathogens, there were still non-neglectable percentages of patients harbouring these bacteria52. This corroborates with detection frequencies observed in our study. Moreover, previous reports from other authors have reported that A. actinomycetemcomitans had not been completely eliminated by subgingival debridement6.
Another explanation would be that, in light of the worldwide indiscriminate use of antimicrobials and implicitly increasing antibiotic resistance44, patients may harbour nowadays more resistant strains of these periodontal pathogens as compared to subjects in earlier studies. It has been shown that the reservoir for antibiotic-resistant genes has been increasing over the past century12,45. This fact adds on to the capacity of the oral microbiota to transfer antimicrobial resistance46,47,48,49. For example, Streptococcus cristaceus has acquired in vivo doxycycline resistance from a resistant strain of Streptococcus oralis, both isolated from the subgingival biofilm of patients under doxycycline therapy50. So far, no such direct evidence exists for bacteria of the red complex or A. actinomycetemcomitans, but it is very likely that these bacteria as well may have acquired in time resistance to commonly used antimicrobials. Additionally, other authors have already reported high percentages (74.2%) of patients with periodontal pathogens resistant to at least one of the most commonly used antimicrobials in periodontal treatment57.
Interestingly, several patients initially negative for A. actinomycetemcomitans became positive at 12 months. This may be attributed to the nature of this pathogen being a facultative aerobic bacterium. Pooled samples of subgingival plaque were taken from the deepest site in each quadrant, where most probably anaerobic pathogens were present in higher proportions. After therapy, those sites reduced their depths, resulting in shallow pockets with more aerobic conditions, making thus the detection of A. actinomycetemcomitans more probable. Additionally, the sampling method may also have had an impact on the microbiological results, which may possibly reflect an artefact. With the employed sampling strategy, only the chosen deep sites are being examined and their results are being extrapolated on the entire mouth. It is well known that high levels and proportions of periodontal pathogens may also be present in shallow gingival crevices58 which had not been assessed. Since A. actinomycetemcomitans is facultative anaerobic, it may have as well been present in more shallow sites as opposed to those here analysed (PD ≥ 6 mm), thus leading to false negative results. Another possibility would be the reemergence of A. actinomycetemcomitans from other anatomical areas in the oro-pharynx. Data show that A. actinomycetemcomitans is presents even in periodontally healthy patients in high numbers on the cheek mucosa (62%), in saliva (59%) and tonsils (41%)59. For P. gingivalis, the majority of the patients in the placebo group remained positive at 12 months (83%, Table1), while about 50% of the patients in the two antimicrobial-groups became negative; thus, statistically significantly fewer patients in the AB groups harboured this pathogen at 12 months as compared to placebo. These results are in line with those of Rooney et al. who obtained a rare recovery of A. actinomycetemcomitans and P. gingivalis19. Additionally, data from a recent systematic review60 indicate comparable percental reductions in the subjects positive on P. gingivalis and A. actinomycetemcomitans: P. gingivalis difference for percental detection rates between test and control group in Dakic et al.: 28% (3 months), 32% (6 months), 34% (12 months) versus our study: 20–40% (3, 6, 12 months); respectively for A. actinomycetemcomitans in Dakic et al.: 30% (3 months), 25% (6 months) with no difference between the groups at 12 months60. Comparable results were seen in our study: 10–40% difference between the groups at 3 and 6 months, with a slight (10%) to no difference at 12 months between placebo and the two antimicrobial-groups.
From a clinical point of view, statistically significantly fewer residual deep sites (PD ≥ 6 mm) and more sites reached pocked closure at 12 months in the 3-day antimicrobial-group as opposed to placebo. Interestingly, this could not be observed for the 7-day AB-protocol. Analysing the impact of A. actinomycetemcomitans or P. gingivalis on these clinical parameters, only patients initially negative for A. actinomycetemcomitans and initially positive for P. gingivalis exhibited at 12 months significantly less residual deep sites as opposed to placebo; nonetheless, at 6 months, A. actinomycetemcomitans positive patients showed in both antimicrobial-groups statistically significantly fewer residual sites compared to placebo. This underlines the fact that antimicrobials had a statistically significant positive effect also on patients negative for this periodontal pathogen compared to those not receiving the medication, and is in line with reports of other studies23. These results are further supported by the recent findings of a systematic review that stressed out the efficacy of AMX + MET in improving clinical outcomes irrespective of the initial detection of A. actinomycetemcomitans15.
Moreover, the results of the present regression analysis showed that neither presence of A. actinomycetemcomitans and P. gingivalis at baseline nor at 12 months were associated with a higher risk for residual deep sites at 12 months (p < 0.05). These results corroborate those of Mombelli et al., who have also observed that the presence/absence of A. actinomycetemcomitans did not influence the effect of antimicrobials on persisting active sites with PD > 4 mm56. Antimicrobials seemed to be highly efficient in both A. actinomycetemcomitans positive and negative patients. Additionally, antimicrobial-groups had significantly more sites reaching pocket closure (PD < 4 mm) at 6 months compared to placebo which is in line with Kolakovic et al.61, who obtained in a meta-analysis a 4.43 higher chance for pocket closure at 6 months in the AMX + MET group compared to control. Moreover, the results in our study were maintained up to 1 year. Further subgroup analyses based on the presence/absence of selected periodontal pathogens could not show any statistically significant influence on the number of sites reaching pocket closure (p > 0.05), despite the fact that the patients receiving placebo had fewer healed sites (PD < 4 mm) as opposed to those receiving systemic medication.
Nonsurgical periodontal therapy with the two antibiotic protocols yielded a decrease in the levels of proinflammatory markers (IL-1β, IL-8, MMP-8) and an increase of the cytokine IL-10, that is associated with periodontal health. Cytokine analysis resulted in a significant reduction of the proinflammatory immunomarker IL-1β at 3 and 6 months compared to baseline only in the two antimicrobial-groups. This could be observed in the 7-day antimicrobial-group also at 12 months, which however, had at baseline significantly higher levels of IL-1β. Additionally, the initial detection of IL-1β was shown to statistically significantly influence the residual number of deep sites at 12 months. The other proinflammatory cytokines (IL-8, MMP-8) showed reductions at 6 and 12 months only in the two antimicrobial-groups. Nonetheless, these reductions did not reach statistical significance except for MMP-8, that was statistically significantly reduced compared to baseline in the 7-day antimicrobial-group; however, MMP-8 intergroup comparisons revealed no significant differences between the three groups at 12 months. These results compare well to those of Jentsch et al., where slightly higher median values for IL-1β and comparable results for MMP-8 were reported for the AMX + MET group at 3 and 12 months respectively62.
The present cytokine reductions in the two antimicrobial-groups, may indeed account for the additional general anti-inflammatory effect of systemic antimicrobials, especially since no statistically significant group differences for baseline plaque scores had been detected41.
The current study represents a secondary analysis of the microbiological and inflammatory data of a clinically designed RCT33,41, which may be a limitation for the power of the current results. Considering the fact that the study was initially designed to find a difference between the control and the test groups for a clinical parameter (5 sites with PD ≥ 6 mm), the presented results and subgroup analyses should be interpreted with caution. Nevertheless, these microbiologic and immunologic data corroborate the primary clinical outcomes of the present trial33,41 supporting the finding that both antibiotic protocols adjunctive to mechanical debridement elicit better clinical, microbiological and immunological effects in severe forms of chronic periodontitis (stage III-IV, grade B). It is important to emphasize that the study was designed to evaluate the efficacy of the two antibiotic regimes adjunctive to non-surgical periodontal therapy compared to mechanical debridement alone. The protocol had not been designed to determine the equivalence or non-inferiority of the use of a 3-day over the 7-day antibiotic protocol adjunctive to mechanical debridement and thus no clear clinical recommendations related to the preferential use of a 3-day AB course over a 7-day one can be made. Moreover, considering the global increase in antimicrobial resistance, antimicrobial usage adjunctive to non-surgical periodontal therapy should be carefully taken prescribed only in selected patients with generalised severe forms of periodontitis that may really profit from it63.
In conclusion, the present data indicate that the systemic use of both 3- and 7- day AMX + MET adjunctive to non-surgical periodontal therapy may induce superior microbiological outcomes compared to subgingival debridement alone. The two investigated antibiotic protocols led to comparable microbiological and inflammatory results.
Methods
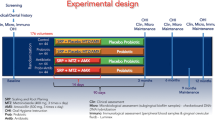
This study was a prospective, randomized, placebo controlled, double-masked clinical trial. Following hypothesis was tested: “the systemic use of AMX and MET administered for 3 or 7 days as adjunct to SD leads to superior clinical results compared with SD alone”33. The clinical results after 6 and 12 months were previously published41. The study protocol (according to the Declaration of Helsinki 1964, revision 2008) was approved by the Ethical Committee of the Faculty of Medicine and Pharmacy of Cluj-Napoca (Trial registration number #514/09.01.2012, registration date: 20.02.2012) and was registered in the ISRCTN registry (trial registration number: ISRCTN17605083, registration date: 16.6.2015, https://www.isrctn.com/ISRCTN17605083).
Subjects and clinical protocol
The clinical protocol was described in detail previously33. Briefly, 102 subjects seeking dental treatment at the University clinic (University Cluj-Napoca) were included and treated between January 2012 and January 2014. Included patients were over 30 years old, had a minimum of 12 natural teeth in the oral cavity and clinical (at least two sites/quadrant with PD ≥ 6 mm) and radiographic signs of generalized severe chronic periodontitis64 (generalized stages III–IV, grade B periodontitis)65, good level of oral hygiene [Full-mouth plaque-scores (FMPS) ≤ 25% prior to SD66], systemically healthy. Subjects smoking at least 10 cigarettes/day for the last 5 years were defined as smokers67. Patients with systemic/local antibiotic therapy within the preceding 3 months, or any type of medication with a possible influence on the periodontium, pregnant/lactating patients or those who had non-surgical periodontal therapy within the previous 12 months were excluded. Informed written consent to participate in the study was obtained from all participants.
Medical history, clinical periodontal parameters (at 6 sites/tooth: PD, CAL), bleeding on probing (BOP) and FMPS66 were recorded before and 3, 6 and 12 months after non-surgical periodontal therapy. Additionally, gingival crevicular fluid (GCF) and subgingival biofilm samples from the deepest pocket in each quadrant were taken at the same timepoints. All recordings, sampling and oral hygiene instructions were performed by one examiner (RJ) blinded to treatment allocation. SD (i.e. elimination of the subgingival calculus and biofilm) was performed within 24h63,68 was performed within 24 h at all sites with PD ≥ 4 mm by one experienced periodontist (RC), blinded to group allocation33,41. A computer-generated block-randomisation list divided the patients afterwards in three treatment groups:
- Group A::
-
SD + placebo [placebo three times/day (TID) for 7 days].
- Group B::
-
SD + systemic AMX + MET (both 500 mg 3TID for first 3 days, placebo 3TID for the rest 4 days).
- Group C::
-
SD + systemic AMX + MET (both 500 mg 3TID for 7 days) (Fig. 1).
Figure 1 Flowchart of the study. Included subjects were instructed for adequate oral hygiene and nonsurgically treated (SD: subgingival debridement). Immediately after SD, patients were randomised to medication (AMX-amoxicillin, MET-metronidazole, TID-times per day). Patients were reevaluated at 3, 6 and 12 months when clinical periodontal parameters, microbiological and immunological outcomes were determined. Appropriate subject numbers at the follow-ups are given. The final number of subjects included in the per-protocol analysis (PP-analysis) is provided.
Patient allocation was performed after SD by another clinician (RT) [for details regarding the bottle pills please see33].
At the follow-up appointments (3, 6, 12 months), the above mentioned parameters were recorded and only supragingival calculus was removed. Any residual periodontal pockets (pockets with PD = 4 mm + BOP, or PD ≤ 5 mm) were not re-instrumented.
GCF and microbial sampling and analysis
In each quadrant, the site with the deepest PD was selected for GCF and microbial sampling. After isolation with cotton rolls and careful removal of supragingival plaque with cotton pellets, a standard paper-strip (Periopaper, Oraflow, USA) was placed at the entrance of the periodontal pocket for 30 s. After removal of the paper strip, a sterile paper-point was inserted for 30 s into the gingival crevice until mild resistance was felt. The four paper strips and four paper points obtained at one timepoint were each pooled into a sterile empty transportation container. GCF-samples were stored at − 70 °C and microbial samples at − 20 °C until assayed.
The host-derived biomarkers IL-1β, IL-10, IL-8 and MMP-8 were determined by commercially available ELISA-kits (R&D Systems Europe Ltd., Abingdon, UK) according to the manufacturer’s instruction. The detection levels of 2 pg/sample for IL-1β, IL-10 and IL-8 and 0.1 ng/sample for MMP-8. Samples were eluted over night at 4 °C into 750bµl phosphate-buffered saline (PBS, SigmaAldrich, St. Louis, MO, USA) and then centrifuged at 400 g for 2 min. For ELISA, 100 µl aliquots of the supernatant were removed and used. The detection levels of the used test kits were 5 pg/sample (IL1β, IL-8, IL-10, MMP-8)69.
Real-time polymerase-chain-reaction (rtPCR) was used to detect the periodontal pathogens A. actinomycetemcomitans, P. gingivalis, Tannerella forsythia, Treponema denticola, Parvimonas micra, Fusobacterium nucleatum, Campylobacter rectus and Filifactor allocis. Bacterial DNA was extracted with Chelex 100 (Bio Rad Laboratories, Inc., Berkeley, CA, USA) and rt PCR was carried out (ABI 7500 rtPCR System, Applied Biosystems, Foster City, CA, USA). rtPCR amplifications were carried out using a 25 µl reaction volume [2.5 µl DNA template and 22.5 µl substrate mixture: 1.25 µl of each primer, 12.5 µl GoTaq qPCR Master Mix, 2 × Promega Corporation (Madison, WI, USA), 5 µl nucleic acid free H2O]. Each batch of specimens contained negative (H2O) and positive controls (2.5 µl genomic DNA of the respective reference strains in different concentrations). The cycling steps consisted of an initial denaturation step at 95 °C for 2 min, 45 cycles at 95 °C for 15 s and at 60 °C for 60 s. The specificity of the amplification was assayed using melting curves and the detection level was 100 bacteria/sample69.
Statistical analyses
Statistical analyses were performed by an experienced professional statistician (CH) using the statistical software program (SPSS statistics 21, IBM, NY, USA). The present study was initially designed to find a difference between the control and the test groups for clinical parameters as the primary outcome33,41. Shortly, the statistical unit was the patient and the primary outcome variable of the study was the difference in the number of sites per patient with PD ≥ 6 mm calculated between baseline and 12 months41. The power of the study was calculated for a difference of at least 5 sites with a PD ≥ 6 mm (standard deviation of 6 sites) between both AB and placebo groups. A study power of 92% for a statistical significance level of 0.05 was achieved for 30 subjects/ group; considering an attrition of 13%, 34 subjects/group were initially included.
For the clinical variables, intra-group clinical comparisons between the follow-ups were analysed by means of paired t-Test and Wilcoxon Signed Ranks Test. Comparisons between the groups at the various timepoints were performed adjusting for baseline values and smoking using ANCOVA and Bonferroni corrections.
Quantitative analysis of the microorganisms and inflammatory markers were first checked for normal distribution using Kolmogorov Smirnov test. Depending on these results, intra-group comparisons between the various timepoints were performed by means of paired t-Test and Wilcoxon Signed Ranks Test. For qualitative changes of the immunomarkers, the Chi-square test was used, while for microbial changes McNemar Test was implemented. Inter-group comparisons were performed by means of ANCOVA, Mann–Whitney U and Kruskal–Wallis tests. Frequencies/number of patients positive for the microorganisms and immunomarkers were determined and intragroup comparisons were performed using McNemar test.
The residual number of sites with PD ≥ 6 mm as well as the number of sites reaching the clinical endpoint of pocket closure (< 4 mm) at 12 months were specifically determined for patients being positive/negative at baseline or at 6- and 12 months for the pathogens A. actinomycetemcomitans, P. gingivalis and T. denticola; group comparisons were performed using ANCOVA.
Finally, a Poisson regression analyses was conducted to determine the influence of the 3- or 7-day antimicrobial (AB) protocol, gender, smoking, BOP and FMPS at baseline and 12 months, initial mean PD and CAL, disease severity (≥ 10 sites with PD ≥ 6 mm), detection of A. actinomycetemcomitans, P. gingivalis, T. denticola, F. allocis and IL-1β at baseline on the residual number of deep sites (PD ≥ 6 mm) at 12 months.
Data availability
Study protocol data are available https://www.isrctn.com/ISRCTN17605083. Data results are available from ralucacosgrea@gmail.com.
Code availability
The study has been registered in the ISRCTN registry (registration date 16.06.2015, registration number: study ID ISRCTN17605083) and is available on the website http://www.isrctn.com/ISRCTN17605083.
References
Socransky, S. S. & Haffajee, A. D. The bacterial etiology of destructive periodontal disease: current concepts. J. Periodontol. 63, 322–331. https://doi.org/10.1902/jop.1992.63.4s.322 (1992).
Bodinka, A. et al. Polymerase chain reaction for the identification of Porphyromonas gingivalis collagenase genes. Oral Microbiol. Immunol. 9, 161–165. https://doi.org/10.1111/j.1399-302x.1994.tb00053.x (1994).
van Winkelhoff, A. J., Rams, T. E. & Slots, J. Systemic antibiotic therapy in periodontics. Periodontol. 2000 10, 45–78. https://doi.org/10.1111/j.1600-0757.1996.tb00068.x (1996).
Mombelli, A., Gmur, R., Gobbi, C. & Lang, N. P. Actinobacillus actinomycetemcomitans in adult periodontitis. I. Topographic distribution before and after treatment. J. Periodontol. 65, 820–826. https://doi.org/10.1902/jop.1994.65.9.820 (1994).
Mombelli, A., Schmid, B., Rutar, A. & Lang, N. P. Persistence patterns of Porphyromonas gingivalis, Prevotella intermedia/nigrescens, and Actinobacillus actinomyetemcomitans after mechanical therapy of periodontal disease. J. Periodontol. 71, 14–21. https://doi.org/10.1902/jop.2000.71.1.14 (2000).
Renvert, S., Wikstrom, M., Dahlen, G., Slots, J. & Egelberg, J. Effect of root debridement on the elimination of Actinobacillus actinomycetemcomitans and Bacteroides gingivalis from periodontal pockets. J. Clin. Periodontol. 17, 345–350. https://doi.org/10.1111/j.1600-051x.1990.tb00029.x (1990).
Dahlen, G., Wikstrom, M. & Renvert, S. Treatment of periodontal disease based on microbiological diagnosis. A 5-year follow-up on individual patterns. J. Periodontol. 67, 879–887. https://doi.org/10.1902/jop.1996.67.9.879 (1996).
Grossi, S. G. et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J. Periodontol. 65, 260–267. https://doi.org/10.1902/jop.1994.65.3.260 (1994).
Haffajee, A. D. & Socransky, S. S. Microbial etiological agents of destructive periodontal diseases. Periodontology 2000(5), 78–111 (1994).
Baer, P. N. & Socransky, S. S. Periodontosis: case report with long-term follow-up. Periodontal Case Rep. 1, 1–6 (1979).
Teughels, W. et al. Adjunctive effect of systemic antimicrobials in periodontitis therapy. A systematic review and meta-analysis. J. Clin. Periodontol. https://doi.org/10.1111/jcpe.13264 (2020).
Jepsen, K. & Jepsen, S. Antibiotics/antimicrobials: systemic and local administration in the therapy of mild to moderately advanced periodontitis. Periodontol 2000 71, 82–112. https://doi.org/10.1111/prd.12121 (2016).
Keestra, J. A., Grosjean, I., Coucke, W., Quirynen, M. & Teughels, W. Non-surgical periodontal therapy with systemic antibiotics in patients with untreated chronic periodontitis: a systematic review and meta-analysis. J. Periodontal Res. 50, 294–314. https://doi.org/10.1111/jre.12221 (2015).
McGowan, K., McGowan, T. & Ivanovski, S. Optimal dose and duration of amoxicillin-plus-metronidazole as an adjunct to non-surgical periodontal therapy: a systematic review and meta-analysis of randomized, placebo-controlled trials. J. Clin. Periodontol. 45, 56–67. https://doi.org/10.1111/jcpe.12830 (2018).
Nibali, L., Koidou, V. P., Hamborg, T. & Donos, N. Empirical or microbiologically guided systemic antimicrobials as adjuncts to non-surgical periodontal therapy? A systematic review. J. Clin. Periodontol. 46, 999–1012. https://doi.org/10.1111/jcpe.13164 (2019).
Heitz-Mayfield, L. J. Systemic antibiotics in periodontal therapy. Aust. Dent. J. 54(Suppl 1), S96-101. https://doi.org/10.1111/j.1834-7819.2009.01147.x (2009).
van Winkelhoff, A. J., Abbas, F., Pavicic, M. J. & de Graaff, J. Chronic conjunctivitis caused by oral anaerobes and effectively treated with systemic metronidazole plus amoxicillin. J. Clin. Microbiol. 29, 723–725 (1991).
Winkel, E. G., Van Winkelhoff, A. J., Timmerman, M. F., Van der Velden, U. & Van der Weijden, G. A. Amoxicillin plus metronidazole in the treatment of adult periodontitis patients. A double-blind placebo-controlled study. J. Clin. Periodontol. 28, 296–305 (2001).
Rooney, J., Wade, W. G., Sprague, S. V., Newcombe, R. G. & Addy, M. Adjunctive effects to non-surgical periodontal therapy of systemic metronidazole and amoxycillin alone and combined. A placebo controlled study. J. Clin. Periodontol. 29, 342–350 (2002).
Matarazzo, F., Figueiredo, L. C., Cruz, S. E., Faveri, M. & Feres, M. Clinical and microbiological benefits of systemic metronidazole and amoxicillin in the treatment of smokers with chronic periodontitis: a randomized placebo-controlled study. J. Clin. Periodontol. 35, 885–896. https://doi.org/10.1111/j.1600-051X.2008.01304.x (2008).
Guerrero, A. et al. Adjunctive benefits of systemic amoxicillin and metronidazole in non-surgical treatment of generalized aggressive periodontitis: a randomized placebo-controlled clinical trial. J. Clin. Periodontol. 32, 1096–1107. https://doi.org/10.1111/j.1600-051X.2005.00814.x (2005).
Cionca, N., Giannopoulou, C., Ugolotti, G. & Mombelli, A. Amoxicillin and metronidazole as an adjunct to full-mouth scaling and root planing of chronic periodontitis. J. Periodontol. 80, 364–371. https://doi.org/10.1902/jop.2009.080540 (2009).
Cionca, N., Giannopoulou, C., Ugolotti, G. & Mombelli, A. Microbiologic testing and outcomes of full-mouth scaling and root planing with or without amoxicillin/metronidazole in chronic periodontitis. J. Periodontol. 81, 15–23. https://doi.org/10.1902/jop.2009.090390 (2010).
RibeiroEdel, P. et al. Full-mouth ultrasonic debridement associated with amoxicillin and metronidazole in the treatment of severe chronic periodontitis. J. Periodontol. 80, 1254–1264. https://doi.org/10.1902/jop.2009.080403 (2009).
Griffiths, G. S. et al. Amoxicillin and metronidazole as an adjunctive treatment in generalized aggressive periodontitis at initial therapy or re-treatment: a randomized controlled clinical trial. J. Clin. Periodontol. 38, 43–49. https://doi.org/10.1111/j.1600-051X.2010.01632.x (2011).
Heller, D. et al. Impact of systemic antimicrobials combined with anti-infective mechanical debridement on the microbiota of generalized aggressive periodontitis: a 6-month RCT. J. Clin. Periodontol. 38, 355–364. https://doi.org/10.1111/j.1600-051X.2011.01707.x (2011).
Mestnik, M. J. et al. The effects of adjunctive metronidazole plus amoxicillin in the treatment of generalized aggressive periodontitis: a 1-year double-blinded, placebo-controlled, randomized clinical trial. J. Clin. Periodontol. 39, 955–961. https://doi.org/10.1111/j.1600-051X.2012.01932.x (2012).
Mestnik, M. J. et al. Short-term benefits of the adjunctive use of metronidazole plus amoxicillin in the microbial profile and in the clinical parameters of subjects with generalized aggressive periodontitis. J. Clin. Periodontol. 37, 353–365. https://doi.org/10.1111/j.1600-051X.2010.01538.x (2010).
Silva, M. P. et al. Clinical and microbiological benefits of metronidazole alone or with amoxicillin as adjuncts in the treatment of chronic periodontitis: a randomized placebo-controlled clinical trial. J. Clin. Periodontol. 38, 828–837. https://doi.org/10.1111/j.1600-051X.2011.01763.x (2011).
Feres, M. et al. Metronidazole alone or with amoxicillin as adjuncts to non-surgical treatment of chronic periodontitis: a 1-year double-blinded, placebo-controlled, randomized clinical trial. J. Clin. Periodontol. 39, 1149–1158. https://doi.org/10.1111/jcpe.12004 (2012).
Varela, V. M. et al. Systemic antimicrobials adjunctive to a repeated mechanical and antiseptic therapy for aggressive periodontitis: a 6-month randomized controlled trial. J. Periodontol. 82, 1121–1130. https://doi.org/10.1902/jop.2011.100656 (2011).
Yek, E. C. et al. Efficacy of amoxicillin and metronidazole combination for the management of generalized aggressive periodontitis. J. Periodontol. 81, 964–974. https://doi.org/10.1902/jop.2010.090522 (2010).
Cosgarea, R. et al. Non-surgical periodontal treatment in conjunction with 3 or 7 days systemic administration of amoxicillin and metronidazole in severe chronic periodontitis patients. A placebo-controlled randomized clinical study. J. Clin. Periodontol. 43, 767–777. https://doi.org/10.1111/jcpe.12559 (2016).
Goutoudi, P., Diza, E. & Arvanitidou, M. Effect of periodontal therapy on crevicular fluid interleukin-1beta and interleukin-10 levels in chronic periodontitis. J. Dent. 32, 511–520. https://doi.org/10.1016/j.jdent.2004.04.003 (2004).
de Lima Oliveira, A. P. et al. Effects of periodontal therapy on GCF cytokines in generalized aggressive periodontitis subjects. J. Clin. Periodontol. 39, 295–302. https://doi.org/10.1111/j.1600-051X.2011.01817.x (2012).
Haffajee, A. D., Socransky, S. S. & Gunsolley, J. C. Systemic anti-infective periodontal therapy. A systematic review. Ann. Periodontol. 8, 115–181. https://doi.org/10.1902/annals.2003.8.1.115 (2003).
Fritoli, A. et al. The effect of systemic antibiotics administered during the active phase of non-surgical periodontal therapy or after the healing phase: a systematic review. J. Appl. Oral Sci. 23, 249–254. https://doi.org/10.1590/1678-775720140453 (2015).
Ehmke, B., Moter, A., Beikler, T., Milian, E. & Flemmig, T. F. Adjunctive antimicrobial therapy of periodontitis: long-term effects on disease progression and oral colonization. J. Periodontol. 76, 749–759. https://doi.org/10.1902/jop.2005.76.5.749 (2005).
Flemmig, T. F., Milian, E., Karch, H. & Klaiber, B. Differential clinical treatment outcome after systemic metronidazole and amoxicillin in patients harboring Actinobacillus actinomycetemcomitans and/or Porphyromonas gingivalis. J. Clin. Periodontol. 25, 380–387 (1998).
Rodrigues, A. S. et al. Clinical and microbiologic evaluation, by real-time polymerase chain reaction, of non-surgical treatment of aggressive periodontitis associated with amoxicillin and metronidazole. J. Periodontol. 83, 744–752. https://doi.org/10.1902/jop.2011.110333 (2012).
Cosgarea, R. et al. One year results of a randomized controlled clinical study evaluating the effects of non-surgical periodontal therapy of chronic periodontitis in conjunction with three or seven days systemic administration of amoxicillin/metronidazole. PLoS ONE 12, e0179592. https://doi.org/10.1371/journal.pone.0179592 (2017).
Vogelman, B. & Craig, W. A. Kinetics of antimicrobial activity. J. Pediatr. 108, 835–840 (1986).
Levy, S. B. & Marshall, B. Antibacterial resistance worldwide: causes, challenges and responses. Nat. Med. 10, S122–S129. https://doi.org/10.1038/nm1145 (2004).
Palmer, A. C. & Kishony, R. Understanding, predicting and manipulating the genotypic evolution of antibiotic resistance. Nat. Rev. Genet. 14, 243–248. https://doi.org/10.1038/nrg3351 (2013).
Knapp, C. W., Dolfing, J., Ehlert, P. A. & Graham, D. W. Evidence of increasing antibiotic resistance gene abundances in archived soils since 1940. Environ. Sci. Technol. 44, 580–587. https://doi.org/10.1021/es901221x (2010).
Ready, D. et al. Potential role of Veillonella spp. as a reservoir of transferable tetracycline resistance in the oral cavity. Antimicrob. Agents Chemother. 50, 2866–2868. https://doi.org/10.1128/AAC.00217-06 (2006).
Roberts, A. P. & Mullany, P. Oral biofilms: a reservoir of transferable, bacterial, antimicrobial resistance. Expert Rev. Anti Infect. Ther. 8, 1441–1450. https://doi.org/10.1586/eri.10.106 (2010).
Villedieu, A. et al. Prevalence of tetracycline resistance genes in oral bacteria. Antimicrob. Agents Chemother. 47, 878–882. https://doi.org/10.1128/aac.47.3.878-882.2003 (2003).
Villedieu, A. et al. Genetic basis of erythromycin resistance in oral bacteria. Antimicrob. Agents Chemother. 48, 2298–2301. https://doi.org/10.1128/AAC.48.6.2298-2301.2004 (2004).
Warburton, P. J., Palmer, R. M., Munson, M. A. & Wade, W. G. Demonstration of in vivo transfer of doxycycline resistance mediated by a novel transposon. J. Antimicrob. Chemother. 60, 973–980. https://doi.org/10.1093/jac/dkm331 (2007).
Celestin, A. R. et al. Novel method suggests global superiority of short-duration antibiotics for intra-abdominal infections. Clin. Infect. Dis. 65, 1577–1579. https://doi.org/10.1093/cid/cix569 (2017).
Eick, S. et al. Microbiological analysis and the outcomes of periodontal treatment with or without adjunctive systemic antibiotics-a retrospective study. Clin. Oral Investig. 22, 3031–3041. https://doi.org/10.1007/s00784-018-2392-3 (2018).
Faveri, M. et al. Clinical and microbiologic effects of adjunctive metronidazole plus amoxicillin in the treatment of generalized chronic periodontitis: smokers versus non-smokers. J. Periodontol. 85, 581–591. https://doi.org/10.1902/jop.2013.130278 (2014).
Mombelli, A. et al. Microbiologic response to periodontal therapy and multivariable prediction of clinical outcome. J. Periodontol. 88, 1253–1262. https://doi.org/10.1902/jop.2017.170286 (2017).
Soares, G. M. et al. Metronidazole alone or with amoxicillin as adjuncts to non-surgical treatment of chronic periodontitis: a secondary analysis of microbiological results from a randomized clinical trial. J. Clin. Periodontol. 41, 366–376. https://doi.org/10.1111/jcpe.12217 (2014).
Mombelli, A. et al. Are there specific benefits of amoxicillin plus metronidazole in Aggregatibacter actinomycetemcomitans-associated periodontitis? Double-masked, randomized clinical trial of efficacy and safety. J. Periodontol. 84, 715–724. https://doi.org/10.1902/jop.2012.120281 (2013).
Rams, T. E., Degener, J. E. & van Winkelhoff, A. J. Antibiotic resistance in human chronic periodontitis microbiota. J. Periodontol. 85, 160–169. https://doi.org/10.1902/jop.2013.130142 (2014).
Socransky, S. S. & Haffajee, A. D. Periodontal microbial ecology. Periodontol. 2000 38, 135–187. https://doi.org/10.1111/j.1600-0757.2005.00107.x (2005).
Muller, H. P., Heinecke, A., Fuhrmann, A., Eger, T. & Zoller, L. Intraoral distribution of Actinobacillus actinomycetemcomitans in young adults with minimal periodontal disease. J. Periodontal Res. 36, 114–123. https://doi.org/10.1034/j.1600-0765.2001.360208.x (2001).
Dakic, A. et al. Detection of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans after systemic administration of amoxicillin plus metronidazole as an adjunct to non-surgical periodontal therapy: a systematic review and meta-analysis. Front. Microbiol. 7, 1277. https://doi.org/10.3389/fmicb.2016.01277 (2016).
Kolakovic, M., Held, U., Schmidlin, P. R. & Sahrmann, P. An estimate of pocket closure and avoided needs of surgery after scaling and root planing with systemic antibiotics: a systematic review. BMC Oral Health 14, 159. https://doi.org/10.1186/1472-6831-14-159 (2014).
Jentsch, H. F., Buchmann, A., Friedrich, A. & Eick, S. Nonsurgical therapy of chronic periodontitis with adjunctive systemic azithromycin or amoxicillin/metronidazole. Clin. Oral Investig. 20, 1765–1773. https://doi.org/10.1007/s00784-015-1683-1 (2016).
Sanz, M. et al. Treatment of stage I–III periodontitis-The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 47(Suppl 22), 4–60. https://doi.org/10.1111/jcpe.13290 (2020).
Armitage, G. C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 4, 1–6. https://doi.org/10.1902/annals.1999.4.1.1 (1999).
Tonetti, M. S., Greenwell, H. & Kornman, K. S. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J. Periodontol. 89(Suppl 1), S159–S172. https://doi.org/10.1002/JPER.18-0006 (2018).
O’Leary, T. J., Drake, R. B. & Naylor, J. E. The plaque control record. J. Periodontol. 43, 38. https://doi.org/10.1902/jop.1972.43.1.38 (1972).
Ammenheuser, M. M., Hastings, D. A., Whorton, E. B. Jr. & Ward, J. B. Jr. Frequencies of hprt mutant lymphocytes in smokers, non-smokers, and former smokers. Environ. Mol. Mutagen 30, 131–138 (1997).
Kieser, J. B. in Proceedings of the 1st European Workshop on Periodontology (ed Karring, T. & Lang, N. P.) 131–158 (Quintessence Publishing Co., 1994).
Cosgarea, R. et al. Effects of non-surgical periodontal therapy on periodontal laboratory and clinical data as well as on disease activity in patients with rheumatoid arthritis. Clin. Oral Investig. 23, 141–151. https://doi.org/10.1007/s00784-018-2420-3 (2019).
Ainamo, J. & Bay, I. Problems and proposals for recording gingivitis and plaque. Int. Dent. J. 25, 229–235 (1975).
Acknowledgements
The authors would like to thank the study nurses Livia Indolean and Erika Batiz for data entries and error checking.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was funded by the authors` themselves and their institutions.
Author information
Authors and Affiliations
Contributions
R.C. principal investigator, conducted the periodontal therapy (subgingival debridement) in patients, manuscript editing, microbiological and immunological analyses. S.E. supervised and conducted the microbiological determination, statistical check. S.J. manuscript editing, data checking. N.B.A. data analyses, manuscript editing and formatting. R.J. performed all pretreatment procedures (oral hygiene instructions, supragingival debridement). R.T. data entry, patient supervision. G.E.S. data check, manuscript editing, statistical check. C.H. performed statistical analyses. A. S. protocol planning, manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cosgarea, R., Eick, S., Jepsen, S. et al. Microbiological and host-derived biomarker evaluation following non-surgical periodontal therapy with short-term administration of systemic antimicrobials: secondary outcomes of an RCT. Sci Rep 10, 16322 (2020). https://doi.org/10.1038/s41598-020-73054-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-73054-8
- Springer Nature Limited