Abstract
We conducted a two-sample Mendelian randomization study to determine the association of smoking initiation with seven psychiatric disorders. We used 353 independent single-nucleotide polymorphisms associated with cigarette smoking initiation as instrumental variables at genome-wide significance threshold (p < 5 × 10−8) from a recent genome-wide association study in 1,232,091 European-origin participants. Summary-level data for seven psychiatric disorders, including anxiety, bipolar disorder, insomnia, major depressive disorder, posttraumatic stress disorder, suicide attempts, and schizophrenia, was obtained from large genetic consortia and genome-wide association studies. The odds ratios of genetically predicted smoking initiation were 1.96 for suicide attempts (95% CI 1.70, 2.27; p = 4.5 × 10−20), 1.69 for post-traumatic stress disorder (95% CI 1.32, 2.16; p = 2.5 × 10−5), 1.54 for schizophrenia (95% CI 1.35, 1.75; p = 1.6 × 10−10), 1.41 for bipolar disorder (95% CI 1.25, 1.59; p = 1.8 × 10−8), 1.38 for major depressive disorder (95% CI 1.31, 1.45; p = 2.3 × 10−38), 1.20 for insomnia (95% CI 1.14, 1.25; p = 6.0 × 10−14) and 1.17 for anxiety (95% CI 0.98, 1.40; p = 0.086). Results of sensitivity analyses were consistent and no horizontal pleiotropy was detected in MR-Egger analysis. However, the associations with suicide attempts, schizophrenia, bipolar disorder, and anxiety might be related to possible reverse causality or weak instrument bias. This study found that cigarette smoking was causally associated with increased risks of a number of psychiatric disorders. The causal effects of smoking on suicide attempts, schizophrenia, bipolar disorder and anxiety needs further research.
Similar content being viewed by others
Introduction
Psychiatric disorder, known as mental disorder or mental illness, has become an important health issue due to its high morbidity and mortality risk1. It was estimated that over 8 percentage of the global population had at least one major mental disorder in 20152 and global disease burden of mental illness ranked the second, accounting for around 11.2% of disability-adjusted life years in 20133.
Cigarette smoking has been proposed as a risk factor for the majority of psychiatric disorder4,5,6. Observational studies have found that cigarette smoking is associated with an increased risk of a number of psychiatric disorders, including suicide, major depressive disorder, and bipolar disorder, etc7,8. In addition, several meta-analysis of prospective studies revealed a dose–response relationship between smoking and the risk of suicide and schizophrenia9,10,11,12. However, whether these observed associations are causal remains unclear since the findings in observational studies are prone to be biased by reverse causality (prevalent nicotine dependence among psychiatric patients, such as schizophrenic patients13), residual confounding and misclassification.
Genetic variants can be used as instrumental variables to assess the causal exposure-outcome association, which is known as Mendelian randomization (MR) analysis. This approach can reduce confounding and overcome reverse causality because genetic variants are randomly distributed at conception and cannot be affected by disease status. We conducted a two-sample MR study to investigate whether smoking initiation is causally associated with seven major psychiatric disorders. Given that previous studies have suggested a protective effect of smoking against depression14, we additionally assessed the reverse influence of depression on smoking initiation.
Methods
Study design
The present MR analysis sets basis at three key assumptions: (1) the genetic variants used as instrumental variables should be tightly associated with smoking; (2) the genetic variants used instrumental variables should not associated with any confounders of the association between smoking and psychiatric disorders, and (3) the genetic variants should only affect the risk of the psychiatric disorders via smoking (Fig. 1)15. In this study, we included seven major psychiatric disorders, including anxiety, bipolar disorder, insomnia, major depressive disorder, posttraumatic stress disorder, suicide attempts, and schizophrenia16,17,18,19,20,21,22, using the summary-level data from publicly available genome-wide association studies (GWAS). Individual studies included in the GWAS datasets had been approved by an ethical review board. No individual-level data were used in the present MR study.
Schematic diagram of the Mendelian randomization assumptions. The MR design can be used to investigate whether a modifiable risk factor (e.g., smoking) is causally related to the outcome (e.g., psychiatric disease). Three assumptions of the present MR study are: (1) the genetic instrument must be associated with smoking, (2) the instrumental variables must not be related to any confounders, and (3) the instrument must influence the risk of psychiatric diseases only through smoking and not through any direct causal pathway.
Instrumental variable selection
For smoking initiation, we selected 378 single-nucleotide polymorphisms (SNPs) as instrumental variables at the genome-wide significance threshold (p < 5 × 10−8) from a GWAS in 1,232,091 European-origin participants23. We excluded SNPs with linkage disequilibrium (R2 > 0.1), leaving 353 independent instrumental variables for smoking initiation. Genetic principle components, population stratification and relatedness of participants were adjusted for in the GWAS. Cigarette initiation was defined as smoking every day for at least a month, smoking more than 100 cigarettes over total life or smoking regularly. Detailed information about SNPs is shown in Supplementary Table 1.
Source of outcomes
Summary-level genetic data for seven psychiatric disorders were obtained from large-scale GWASs or genetic consortia16,17,18,19,20,21,22. Descriptions of outcome sources, such as the number of controls and cases, population structure and dataset source, are presented in Table 1. The definitions of included disorders are listed in Supplementary Table 2.
Statistical analyses
The random-effects inverse-variance weighted method was used as the main analysis due to the most precise estimation it can provide24. However, because the inverse-variance weighted method is sensitive to invalid instrumental variables and pleiotropy25, several sensitivity analyses were additionally performed, including weighted median, MR Egger, MR-Egger-SIMEX and MR-PRESSO. The weighted median approach can provide a consistent estimate if more than 50% of weight comes from valid instrumental variables25. The MR-Egger regression is a technique to detect and correct for horizontal pleiotropy albeit with low power26. MR-Egger-SIMEX can provide estimation with adjustment for dilution of the MR-Egger estimate using the simulation extrapolation (SIMEX) method, as a supplementary tool for MR-Egger when I2GX < 90%26. The MR pleiotropy residual sum and outlier (MR-PRESSO) method can generate empirical distribution of causal estimates by bootstrap and correct for horizontal pleiotropy via outlier removal27. Heterogeneity was assessed by I2 and Cochran’s Q value in the inverse-variance weighted model and Rucker’s Q’ value in MR-Egger regression. Compared with Cochran’s Q value, a lower Rucker’s Q’ value indicates that the MR-Egger method provides a model with a better fit for examining the particular association. Given that previous studies suggested a protective effect of smoking against depression14, we conducted a reverse MR analysis to assess the influence of having depression on smoking initiation.
To test the direction of causations, we used the MR Steiger directionality28 test to determine whether the observed associations were directionally causal. The rationale of this approach is to compare the variances explained by used SNPs in the exposure and outcomes. If the used instrumental variables explained more variance in smoking initiation than included psychiatric outcomes, the established associations could be directionally reliable. We calculated F statistics29 to examine the weak instrument bias using following formula: F = ((n − k − 1)/k) * (R2/(1 − R2)) where n, k and R2 indicates sample size, number of instrumental variables and variance explained by used SNPs, respectively. A generally quoted criterion is that an instrument is weak if the F statistic is less than 10. To visualize the associaitons and check the assumptions of MR, MR scator plots using three analyses were drawn. The summary statistics data across datasets were harmonized so that the effect allele reflected the allele associated with an increased probability of lifetime smoking initiation. The odds ratios (ORs) of psychiatric disorders with 95% confidence intervals (CIs) represent the increase of one standard deviation in the prevalence of smoking initiation. The power was calculated based on a web-tool30. All p values were two-sided. These analyses in the present study were performed using the mrrobust package in Stata/SE 15.0 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.) and TwoSampleMR package31 in R Software 3.6.0 (R Core Team. R Foundation for Statistical Computing. Vienna, Austria. 2019. https://www.R-project.org). We interpreted the findings based on the strength and consistency of the associations in the main and sensitivity analyses rather than defining the statistical significance threshold based on p values32.
Results
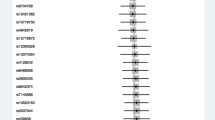
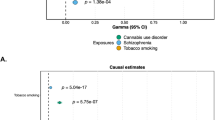
The associations between cigarette smoking initiation and psychiatric disorders are shown in Fig. 2. Genetically predicted smoking initiation was associated with higher odds of all seven included psychiatric disorders. The odds ratios were 1.96 (95% CI 1.70, 2.27; p = 4.5 × 10−20) for suicide attempts, 1.69 (95% CI 1.32, 2.16; p = 2.5 × 10−5) for post-traumatic stress disorder, 1.54 (95% CI 1.35, 1.75; p = 1.6 × 10−10) for schizophrenia, 1.41 (95% CI 1.25, 1.59; p = 1.8 × 10−8) for bipolar disorder, 1.38 (95% CI 1.31, 1.45; p = 2.3 × 10−38) for major depressive disorder, 1.20 (95% CI 1.14, 1.25; p = 6.0 × 10−14) for insomnia and 1.17 (95% CI 0.98, 1.40; p = 0.086) for anxiety in the main analysis. Results remained consistent across sensitivity analyses albeit with larger CIs in weighted median and MR-Egger analyses (Table 2). We detected moderate to high heterogeneity in the analysis of bipolar disorder, schizophrenia, major depressive disorder and insomnia (Supplementary Table 3). However, there was no horizontal pleiotropy in any analysis (p for the MR-Egger intercept > 0.05). We observed I2GX of around 60% in all analyses, indicating possible dilution in the MR-Egger estimation due to violation of the No Measurement Error assumption. After correcting for dilution, the magnitude of all associations in the MR-Egger-SIMEX analysis increased slightly (Table 2). We observed several Rucker’s Q’ values > 700 (p < 0.001), indicating that the MR-Egger approach did not provide a model with a better fit compared to the inverse-variance weighted method. Four to eighteen outliers were detected in the analysis of bipolar disorder, schizophrenia, major depressive disorder, and insomnia. After outlier removal, the significance and magnitude of all associations persisted in MR-PRESSO (Table 2).
Associations of genetically predicted smoking initiation with psychiatric disorders using inverse-variance weighted model. CI indicates confidence interval; OR, odds ratio; SNPs, single-nucleotide polymorphisms. Estimates were estimated using the mrrobust package in Stata/SE 15.0 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.).
We had 100% power in all analyses, except for analysis of anxiety with a power of 45%. In the MR Steiger directionality test, the variance explained by included SNPs is larger in schizophrenia, bipolar disorder and anxiety compared with smoking initiation, suggesting that these observed associations might not be directionally causal. In addition, we found the weak instrument bias might exist in the associations for anxiety, bipolar disorder, suicide attempts and schizophrenia (F statistic < 10). Figure 3 shows the scatter plots for all analyzed associations. The causal associations of smoking with depression and insomnia appeared to be stable given a stronger effect on outcome comparted with exposure. However, other associations might be risked by reverse causation or weak instrument bias, which is also partly revealed in MR Steiger directionality tes. In the reserve MR analysis for depression, the liability to depression was associated with an increased risk of smoking initiation (OR = 1.11; 95% CI 1.02–1.22; p = 0.016). The result remained consistent in the weighted median method, but not in MR-Egger regression (Supplementary Table 4).
Scatter plots of the associations of smoking initiation with seven psychiatric diseases. The Scatter plots were constructed using TwoSampleMR package31 in R Software 3.6.0 (R Core Team. R Foundation for Statistical Computing. Vienna, Austria. 2019. https://www.R-project.org). Betas (SEs) and p values were 0.68 (0.07) and 4.6 × 10−20 in inverse-variance weigthed (IVW), 0.65 (0.10) and 1.8 × 10−10 in weighted median (WM), 0.35 (0.31) and 0.256 in MR-Egger for suicide attempts; 0.53 (0.12) and 2.2 × 10−5 in IVW, 0.56 (0.18) and 2.2 × 10−3 in WM, 0.49 (0.54) and 0.366 in MR-Egger for post-traumatic stress disorder; 0.43 (0.07) and 1.7 × 10−10 in IVW, 0.32 (0.07) and 9.5 × 10−7 in WM, 0.77 (0.29) and 0.008 in MR-Egger for schizophrenia; 0.34 (0.06) and 2.0 × 10−8 in IVW, 0.40 (0.07) and 2.0 × 10−7 in WM, 0.56 (0.26) and 0.035 in MR-Egger for bipolar disorder; 0.32 (0.02) and 1.8 × 10−38 in IVW, 0.29 (0.02) and 1.5 × 10−34 in WM, 0.18 (0.11) and 0.091 in MR-Egger for major depressive disorder; 0.18 (0.02) and 6.2 × 10−14 in IVW, 0.19 (0.03) and 4.8 × 10−12 in WM, 0.08 (0.10) and 0.430 in MR-Egger for insomnia; and 0.16 (0.09) and 0.085 in IVW, 0.16 (0.13) and 0.229 in WM, 0.22 (0.41) and 0.598 in MR-Egger for anxiety.
Discussion
The findings of the present two-sample MR study demonstrated positive associations of smoking initiation with six psychiatric disorders, including suicide attempts, post-traumatic stress disorder, schizophrenia, bipolar disorder, major depressive disorder, and insomnia. There was a suggestive positive association between smoking initiation and anxiety. However, the associations for suicide attempts, schizophrenia, bipolar disorder and anxiety could not be determined due to possible reverse causality or weak instrument bias. There was a reverse association between the liability to depression and increased risk of smoking initiation.
Observational studies have revealed that smoking initiation and other smoking-related traits were associated with overall and specific psychiatric disorders5,6,7,8,12, which is supported by the results of the present MR study. Findings of meta-analyses of cohort, case–control and/or cross-sectional studies have shown that smoking is associated with an increased risk of suicide attempts12,33, post-traumatic stress disorder33, schizophrenia34 and major depressive disorder35 as well as bipolar disorder36. Several prospective studies also found an elevated risk of insomnia among smokers37, especially among heavy smokers38. Observational findings of the association between smoking and anxiety are inconsistent in terms of the directions of the associations39. A previous MR study reported no association between smoking heaviness and anxiety, but that study relied on a single instrumental variable for smoking40. The present MR study, which exploited 348 SNPs as instrumental variables, detected a possible modest positive association between smoking initiation and anxiety but had inadequate power.
The associations of smoking with depression, schizophrenia41, suicide ideation42 and bipolar disorder36 have been revealed in previous MR studies. The present study was based on more recent GWASs and comprehensively investigated the causal associations between smoking initiation and psychiatric traits. We confirmed established causal associations for depression, schizophrenia, suicide ideation and bipolar disorder. Meanwhile, we found some novelty associations for insomnia, post-traumatic stress disorder and a possible association for anxiety. However, it should be cautious to interpret causal associations of smoking initiation with suicide attempts, schizophrenia, bipolar disorder and anxiety due to the limitation of instrumental variables used. More studies are needed to explore these association in a causal fashion.
A bidirectional association has been observed between smoking and several psychiatric disorders, such as bipolar disorder36, schizophrenia43 and anxiety44 in observational studies. It has further been shown that individuals with depressive symptoms or past major depressive disorder were less likely to quit smoking compared with smokers without depression45,46. Even though meta-analyses found no psychiatric side-effects, such as depression and bad mood, derived from smoking cessation47,48 among general smoking quitters, some studies have detected an increased depression risk among those who attempt to quit unsuccessfully49 and somatic adverse reactions among individuals with nicotine replacement therapy50. Thus, considering mutually detrimental influence between smoking and psychiatric diseases, difficulty of smoking cessation among certain populations and possible side-effects of smoking cessation therapies, reducing smoking initiation at the beginning step is an effective strategy for mental illness prevention. However, a recent study suggested the protective effect of smoking against depression14. In our study, we also observed a reverse positive association between depression and smoking initiation, which supported that patients with depressive symptoms were more likely to start cigarette smoking possibly due to a depression-releasing effect derived from smoking. Thus, whether stopping smoking should be recommended among patietns with depression needs to be further assessed.
Mechanisms explaining the comorbidity of smoking (nicotine dependence) with psychiatric diseases have been well acknowledged, especially for the prevalent smoking addiction among schizophrenia patients13. Experimental and genetic evidence shows that nicotine can normalize several deficits, such as attention deficits, among individuals with certain psychiatric problems via nicotinic acetylcholine receptors13. Antidepressant actions via monoamine oxidase inhibition (from unknown components from cigarettes) and nicotine-derived compensation effects of psychiatric medications also rationalize the phenomenon of more smokers among psychiatric patients compared with healthy adults13. Although the mechanisms are not clearly clarified about the increased risk of psychiatric diseases among smokers, pathways listed above may play a role. Another possible mechanism linking smoking and psychiatric disorders is the effects of nicotine on the dopamine system3,51. Nicotine has been also proposed to influence the dopamine system through induction of supersensitivity of D2 receptors, which shows associations with the risk of schizophrenia and other psychotic symptoms3,52. In addition, cigarette smoking has been suggested to increase the risk of anxiety by influencing neurotransmitter systems, the immune system, oxidative and nitrogen stress, mitochondrial function, and epigenetic regulation53. Given genetic and phenotypical overlapping54,55,56 across major psychiatric disorders, above smoking-casued anxiety-related pathways, may play roles in other specific mental diseases.
There are several advantages of our study. The MR approach minimized reverse causality, residual confounding, and misclassification, which potentially exist in observational studies. Population stratification bias was reduced in this study because SNP selection and summary-level data of psychiatric disorders were merely based on individuals of European descent and population structure was adjusted for in the GWASs. Moreover, the consistency in results across sensitivity analyses and no evidence of horizontal pleiotropy in the MR-Egger analysis indicate that our findings are unlikely biased by horizontal pleiotropy. However, our study has some limitations. The major limitation is the insufficient power to support a significant association between smoking initiation and anxiety, which needs to be verified in future studies. We had weak instrument bias or false causal direction in several analyses, which hindered the causal inference on these associations. In addition, because we only used the data from European-descent individuals, it should be cautious to generalize our findings to other populations.
In conclusion, this MR study provided evidence that smoking initiation is causally associated with an increased risk of a number of psychiatric disorders. However, whether smoking increases the risk of suicide attempts, schizophrenia, bipolar disorder and anxiety warrants future study. Reducing smoking initiation might be an effective strategy to prevent psychiatric disorders, but possibly not among patients with depression.
References
Sullivan, P. F. & Geschwind, D. H. Defining the genetic, genomic, cellular, and diagnostic architectures of psychiatric disorders. Cell 177, 162–183 (2019).
World Health Organization. Depression and other common: mental disorders global health estimates. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf. (Accessed 05 January 2020)
Gurillo, P., Jauhar, S., Murray, R. M. & MacCabe, J. H. Does tobacco use cause psychosis? Systematic review and meta-analysis. Lancet Psychiatry 2, 718–725 (2015).
Blanco, C. et al. Cannabis use and risk of psychiatric disorders: prospective evidence from a US National Longitudinal Study. JAMA Psychiatry 73, 388–395 (2016).
Talati, A., Keyes, K. M. & Hasin, D. S. Changing relationships between smoking and psychiatric disorders across twentieth century birth cohorts: clinical and research implications. Mol. Psychiatry 21, 464–471 (2016).
Vigo, D., Thornicroft, G. & Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 3, 171–178 (2016).
Evins, A. E., Korhonen, T., Kinnunen, T. H. & Kaprio, J. Prospective association between tobacco smoking and death by suicide: a competing risks hazard analysis in a large twin cohort with 35-year follow-up. Psychol. Med. 47, 2143–2154 (2017).
An, R. & Xiang, X. Smoking, heavy drinking, and depression among U.S. middle-aged and older adults. Prev. Med. 81, 295–302 (2015).
Li, D. et al. Cigarette smoking and risk of completed suicide: a meta-analysis of prospective cohort studies. J. Psychiatr. Res. 46, 1257–1266 (2012).
De Leon, J. & Diaz, F. J. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr. Res. 76, 135–57 (2005).
Diaz, F. J. et al. Tobacco smoking behaviors in bipolar disorder: a comparison of the general population, schizophrenia, and major depression. Bipolar Disord. 11, 154–165 (2009).
Poorolajal, J. & Darvishi, N. Smoking and suicide: a meta-analysis. PLoS ONE 11, e0156348 (2016).
Dani, J. A. & Harris, R. A. Nicotine addiction and comorbidity with alcohol abuse and mental illness. Nat. Neurosci. 8, 1465–1470 (2005).
Lewis, S. J. Smoking is associated with, but does not cause, depressed mood in pregnancy: a Mendelian randomization study. PLoS ONE 6, e21689 (2011).
Lawlor, D. A. Commentary: two-sample Mendelian randomization: opportunities and challenges. Int. J. Epidemiol. 45, 908–915 (2016).
Otowa, T. et al. Meta-analysis of genome-wide association studies of anxiety disorders. Mol. Psychiatry 21, 1391–1399 (2016).
Nievergelt, C. M. et al. International meta-analysis of PTSD genome-wide association studies identifies sex- and ancestry-specific genetic risk loci. Nat. Commun. 10, 4558 (2019).
Erlangsen, A. et al. Genetics of suicide attempts in individuals with and without mental disorders: a population-based genome-wide association study. Mol. Psychiatry https://doi.org/10.1038/s41380-018-0218-y (2018) ((Epub ahead of print)).
Stahl, E. A. et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat. Genet. 51, 793–803 (2019).
Jansen, P. R. et al. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat. Genet. 51, 394–403 (2019).
Howard, D. M. et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat. Neurosci. 22, 343–352 (2019).
Rufer, D. M. et al. Bipolar disorder and Schizophrenia Working Group of the psychiatric genomics C. Genomic dissection of bipolar disorder and schizophrenia, including 28 subphenotypes. Cell 173, 1705-1715.e16 (2018).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51, 237–244 (2019).
Burgess, S., Bowden, J., Fall, T., Ingelsson, E. & Thompson, S. G. Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants. Epidemiology 28, 30–42 (2017).
Bowden, J., Smith, G. D., Haycock, P. C. & Burgess, S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40, 304–314 (2016).
Bowden, J. et al. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Int. J. Epidemiol. 45, 1961–1974 (2016).
Ong, J. S. & MacGregor, S. Implementing MR-PRESSO and GCTA-GSMR for pleiotropy assessment in Mendelian randomization studies from a practitioner’s perspective. Genet. Epidemiol. 43, 609–616 (2019).
Hemani, G., Tilling, K. & Smith, G. D. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 13, e1007081 (2017).
Burgess, S. & Thompson, S. G. Bias in causal estimates from Mendelian randomization studies with weak instruments. Stat. Methods 30, 1312–1323 (2011).
Cnsgenomics.com. mRnd: power calculations for Mendelian randomization. https://cnsgenomics.com/shiny/mRnd/. (Accessed 05 January 2020)
Hemani, G. et al. The MR-base platform supports systematic causal inference across the human phenome. eLife 7, e34408 (2018).
Sterne, J. A. & Smith, G. D. Sifting the evidence-what’s wrong with significance tests?. BMJ 322, 226–231 (2001).
Fu, S. S. et al. Post-traumatic stress disorder and smoking: a systematic review. Nicotine Tob. Res. 9, 1071–1084 (2007).
Hunter, A., Murray, R., Asher, L. & Leonardi-Bee, J. The effects of tobacco smoking, and prenatal tobacco smoke exposure, on risk of schizophrenia: a systematic review and meta-analysis. Nicotine Tob. Res. 22, 3–10 (2020).
Luger, T. M., Suls, J. & Weg, M. W. V. How robust is the association between smoking and depression in adults? A meta-analysis using linear mixed-effects models. Addict. Behav. 39, 1418–1429 (2014).
Vermeulen, J. M. et al. Smoking and the risk for bipolar disorder: evidence from a bidirectional Mendelian randomisation study. Br. J. Psychiatry 17, 1–7 (2019).
Chen, L. J., Steptoe, A., Chen, Y. H., Ku, P. W. & Lin, C. H. Physical activity, smoking, and the incidence of clinically diagnosed insomnia. Sleep Med. 30, 189–194 (2017).
Brook, J. S., Zhang, C., Rubenstone, E. & Brook, D. W. Insomnia in adults: the impact of earlier cigarette smoking from adolescence to adulthood. J. Addict. Med. 9, 40–45 (2015).
Fluharty, M., Taylor, A. E., Grabski, M. & Munafò, M. R. The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tob. Res. 19, 3–13 (2017).
Taylor, A. E. et al. Investigating the possible causal association of smoking with depression and anxiety using Mendelian randomisation meta-analysis: the CARTA consortium. BMJ Open. 4, e006141 (2014).
Wootton, R. E. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study. Psychol. Med. https://doi.org/10.1017/S0033291719002678(Epubaheadofprint) (2019).
Harrison, R., Munafò, M. R., Smith, G. D. & Wootton, R. E. Examining the effect of smoking on suicidal ideation and attempts: triangulation of epidemiological approaches. Br. J. Psychiatry https://doi.org/10.1192/bjp.2020.68 (2020).
Jackson, J. G., Diaz, F. J., Lopez, L. & de Leon, J. A combined analysis of worldwide studies demonstrates an association between bipolar disorder and tobacco smoking behaviors in adults. Bipolar Disord. 17, 575–597 (2015).
Jiang, F., Li, S., Pan, L., Zhang, N. & Jia, C. Association of anxiety disorders with the risk of smoking behaviors: a meta-analysis of prospective observational studies. Drug Alcohol Depend. 145, 69–76 (2014).
Doyle, F. et al. Systematic review and meta-analysis of the impact of depression on subsequent smoking cessation in patients with coronary heart disease: 1990 to 2013. Psychosom. Med. 76, 44–57 (2014).
Hitsman, B. et al. Past major depression and smoking cessation outcome: a systematic review and meta-analysis update. Addiction 108, 294–306 (2013).
Tsoi, D. T., Porwal, M. & Webster, A. C. Efficacy and safety of bupropion for smoking cessation and reduction in schizophrenia: systematic review and meta-analysis. Br. J. Psychiatry 196, 346–353 (2010).
Taylor, G. et al. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 348, g1151 (2014).
McClave, A. K. et al. Associations between smoking cessation and anxiety and depression among U.S. adults. Addict. Behav. 34, 491–497 (2009).
Mills, E. J., Wu, P., Lockhart, I., Wilson, K. & Ebbert, J. O. Adverse events associated with nicotine replacement therapy (NRT) for smoking cessation. A systematic review and meta-analysis of one hundred and twenty studies involving 177,390 individuals. Tob. Induc. Dis. 8, 8 (2010).
Brody, A. L. et al. Smoking-induced ventral striatum dopamine release. Am. J. Psychiatry 161, 1211–1218 (2004).
Howes, O. D. & Kapur, S. The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr. Bull. 35, 549–562 (2009).
Moylan, S., Jacka, F. N., Pasco, J. A. & Berk, M. How cigarette smoking may increase the risk of anxiety symptoms and anxiety disorders: a critical review of biological pathways. Brain Behav. 3, 302–326 (2013).
Consortium C-DGotPG. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 381, 1371–1379 (2013).
Smoller, J. W. The genetics of stress-related disorders: PTSD, depression, and anxiety disorders. Neuropsychopharmacology 41, 297–319 (2016).
Middeldorp, C. M., Cath, D. C., Dyck, R. V. & Boomsma, D. I. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychol. Med. 35, 611–624 (2005).
Acknowledgements
Summary-level data for seven psychiatric disorders were obtained from large-scale GWASs or genetic consortia, including the Psychiatric Genomics Consortium, the Center for Neurogenomics and Cognitive Research (CNCR), UK Biobank and the Integrative Psychiatric Research (iPSYCH). The SNPs for smoking initiation were obtained from the Sequencing Consortium of Alcohol and Nicotine use (GSCAN). The authors thank all investigators for sharing this data. Funding for this study came from the Swedish Research Council (Vetenskapsrådet; Grant Number 2019-00977) and the Swedish Research Council for Health, Working Life and Welfare (Forte; 2018-00123). Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yuan, S., Yao, H. & Larsson, S.C. Associations of cigarette smoking with psychiatric disorders: evidence from a two-sample Mendelian randomization study. Sci Rep 10, 13807 (2020). https://doi.org/10.1038/s41598-020-70458-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70458-4
- Springer Nature Limited
This article is cited by
-
Determinants of multimorbidity in older adults in Iran: a cross-sectional study using latent class analysis on the Bushehr Elderly Health (BEH) program
BMC Geriatrics (2024)
-
The role of thyroid function in borderline personality disorder and schizophrenia: a Mendelian Randomisation study
Borderline Personality Disorder and Emotion Dysregulation (2024)
-
Deep sequencing of candidate genes identified 14 variants associated with smoking abstinence in an ethnically diverse sample
Scientific Reports (2024)
-
Cigarette Smoking and Psychiatric Illness Among Individuals with COPD: a Systematic Review
Current Addiction Reports (2024)
-
Mendelian randomization studies of depression: evidence, opportunities, and challenges
Annals of General Psychiatry (2023)