Abstract
This study aimed to investigate the risk of acute kidney injury (AKI) in hospitalized patients based on admission serum ionized calcium levels. This is a cohort study of all hospitalized adult patients, from January 2009 to December 2013 at a tertiary referral hospital, who had available serum ionized calcium at the time of admission. We excluded patients who had end-stage kidney disease or AKI at admission. We stratified admission serum ionized calcium into 6 groups; ≤ 4.39, 4.40–4.59, 4.60–4.79, 4.80–4.99, 5.00–5.19, and ≥ 5.20 mg/dL. We used serum creatinine criterion of KDIGO definition for diagnosis of AKI. We performed logistic regression analysis to assess the risk of in-hospital AKI occurrence based on admission serum ionized calcium, using serum ionized calcium of 5.00–5.19 mg/dL as the reference group. We studied a total of 25,844 hospitalized patients. Of these, 3,294 (12.7%) developed AKI in hospital, and 622 (2.4%) had AKI stage 2 or 3. We observed a U-shaped association between admission serum ionized calcium and in-hospital AKI, with nadir in-hospital AKI was in serum ionized calcium of 5.00–5.19 mg/dL. After adjustment for confounders, low serum ionized calcium of 4.40–4.59, ≤ 4.39 mg/dL and elevated serum ionized calcium ≥ 5.20 mg/dL were associated with increased risk of AKI with odds ratio of 1.33 (95% CI 1.14–1.56), 1.45 (95% CI 1.21–1.74), and 1.26 (95% CI 1.04–1.54), respectively. Both hypocalcemia, and hypercalcemia at the time of admission were associated with an increased risk of hospital-acquired AKI.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) is a common complication among hospitalized patients with approximate incidence of 20%1,2,3,4. Importantly, AKI is independently associated with in-hospital mortality and de novo or progression of chronic kidney disease2,3,5,6. Early detection and management for AKI and its complications are needed to decrease its dire clinical impacts. Calcium homeostasis is commonly disturbed as a consequence of AKI7. However, whether calcium, specifically ionized calcium plays a role in the development of AKI is unclear.
Ionized calcium is an essential mineral required for many physiologic functions in the body, from cellular function, intracellular messenger transduction, hormonal activity, to cardiac function and neuronal activity8,9,10,11. From the kidney standpoint, AKI in the setting of hypercalcemia can arise via several mechanisms such as volume depletion from polyuria (decreased collecting duct cells response to vasopressin) and direct alterations of intravascular tone12,13,14. Besides, persistent hypercalcemia can lead to calcium deposits in the kidneys or nephrocalcinosis15. Previous studies have shown associations between electrolyte disturbances and a higher incidence of AKI among hospitalized patients, specifically an imbalance in total calcium, phosphate, and calcium-phosphorus product16,17. These abnormalities seem to directly or indirectly correlate with serum ionized calcium18. Therefore, serum ionized calcium might be a useful marker to predict AKI and might also be independently associated with AKI. However, data on the impact of serum ionized calcium on incidence of AKI among hospitalized patients is limited.
Our study aimed to assess the association between admission serum ionized calcium and risk of in-hospital AKI among hospitalized patients retrieving data from an electronic medical record system.
Materials and methods
Study population
This historical cohort study, conducted at Mayo Clinic, Rochester, MN, USA, included all hospitalized adult patients from January 1st, 2009 to December 31st, 2013 who had available serum ionized calcium within 24 hours of hospital admission. We excluded individuals with end-stage kidney disease (ESKD), patients whose AKI was present at the time of admission, and those whose serum creatinine was not available during hospitalization. For patients with recurrent admissions, only the first hospital admission during the study period was analyzed. Mayo Clinic Institutional Review Board reviewed and approved this project (IRB number 15-000024) and waived informed consent due to the minimal risk nature of this study. The study was conducted in accordance with the relevant guidelines and regulations.
Data collection
Institutional electronic medical record system was used to automated retrieval of data collection for clinical characteristics, demographic information, and laboratory data. The predictor of interest was the admission serum ionized calcium, defined as the first serum ionized calcium measured within 24 hours of hospital admission. Estimated glomerular filtration rate (eGFR) was calculated based on age, sex, race, and baseline serum creatinine, using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation19. The Charlson Comorbidity Index was calculated to assess comorbidity burden at the time of admission20. Principal diagnoses were grouped based on admission ICD-9 codes. ESKD was identified using ICD-9 diagnosis code or eGFR of ≤ 15 mL/min/1.73 m2.
Clinical outcomes
The outcome of interest was the occurrence of acute kidney injury (AKI) within 7 days of hospital admission. AKI was diagnosed by the KDIGO serum creatinine criterion, which was defined as an absolute increase in serum creatinine of ≥ 0.3 mg/dL within 48 h or ≥ 1.5 times baseline within 7 days after admission date21. Severe AKI was considered as AKI KDIGO stage 2 or 3. The most recent outpatient serum creatinine prior to the admission was regarded as baseline serum creatinine. If outpatient baseline serum creatinine was absent, the Modification of Diet in Renal Disease equation was used to back-estimate baseline serum creatinine level, assuming normal baseline GFR of 75 mL/min/1.73 m2, as suggested by the guideline21.
Statistical analysis
Variables were summarized as mean ± standard deviation (SD) for continuous variables and as number with percentage for categorical variables. ANOVA and Chi-squared test was used to compare clinical characteristics and outcomes among admission serum ionized calcium groups, as appropriate. Based on its distribution, admission serum ionized calcium was categorized into six groups; ≤ 4.39, 4.40–4.59, 4.60–4.79, 4.80–4.99, 5.00–5.19, and ≥ 5.20 mg/dL. Restricted cubic spline with 5 knots based on serum ionized calcium was fitted to visualize the possible non-linear relationship between serum ionized calcium at admission and risk of in-hospital AKI. Then, multivariate logistic regression analysis was performed to obtain adjusted odds ratio (OR) of in-hospital AKI occurrence based on admission serum ionized calcium groups, using serum ionized calcium of 5.00–5.20 mg/dL as the reference group because AKI least occurred in the hospital when admission serum ionized calcium was within this range. The adjusting variables were priori-defined and included age, sex, race, baseline eGFR, Charlson Comorbidity Index, comorbidity conditions, admission type, admission service, principal diagnosis, medications, the use for vasopressor and mechanical ventilator at hospital admission, admission serum phosphate, serum magnesium, and serum albumin. P-value was two-tailed with the value of < 0.05 considered statistically significant. All analyses were performed using JMP statistical software (version 14.0, SAS Institute, Cary, NC). The restricted cubic spline was constructed using STATA (version 14.1, StataCorp LLC, Texas, USA).
Results
Patient cohort and clinical characteristics
Figure S1 showed the sample selection process of patients included in the study. During the study period, 33,255 patients had available serum ionized calcium measurement at the time of admission. 1,409 ESKD patients, 5,967 patients who had AKI at hospital admission, and 35 patients who had no serum creatinine measurement during hospitalization were excluded. A total of 25,844 patients were studied. The mean age was 61 ± 17 years. Fifty-five percent of enrolled individuals were male. The mean eGFR was 85 ± 23 mL/min/1.73 m2. The mean admission serum ionized calcium was 4.8 ± 0.3 mg/dL. The distribution of admission serum ionized calcium was as follows: 8% in serum ionized calcium of ≤ 4.39 mg/dL, 13% in 4.40–4.59 mg/dL, 31% in 4.60–4.79 mg/dL, 29% in 4.80–4.99 mg/dL, 13% in 5.00–5.19 mg/dL, and 6% in ≥ 5.20 mg/dL. Table 1 showed the clinical characteristics of patients based on various admission serum ionized calcium groups.
Admission serum ionized calcium levels and risk of hospital-acquired acute kidney injury
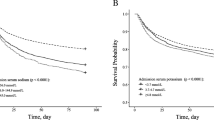
Of 25,844 patients studied, 3,294 (12.7%) developed AKI in hospital; 10.3% in stage 1, 1.3% in stage 2, and 1.1% in stage 3. 167 (0.6%) patients required renal replacement therapy in the hospital. The incidence of hospital-acquired AKI was 16.5% in patients with admission serum ionized calcium of ≤ 4.39, 14.8% in 4.40–4.59, 12.5% in 4.60–4.79, 11.6% in 4.80–4.99, 10.4% in 5.00–5.19, and 15.0% in ≥ 5.20 mg/dL (Table 2). The restricted cubic spline in Fig. 1 demonstrated a U-curve for the association between admission serum ionized calcium and the risk of hospital-acquired AKI. Both decreased serum ionized calcium of ≤ 4.59 mg/dL and elevated serum ionized calcium of ≥ 5.20 mg/dL were significantly associated with increased risk of hospital-acquired AKI, compared with serum ionized calcium of 5.00–5.19 mg/dL (Table 3a). There was no difference in the risk of hospital-acquired AKI when serum ionized calcium ranged from 4.60–5.19 mg/dL, the normal range of serum ionized calcium. Decreased serum ionized calcium of ≤ 4.79 mg/dL and elevated serum ionized calcium of ≥ 5.20 mg/dL were significantly associated with increased risk of severe hospital-acquired AKI (Table 3b).
The subgroup analysis based on admission type showed that, among patients with elective hospital admission, only decreased serum ionized calcium ≤ 4.59 mg/dL was significantly associated with increased risk of hospital-acquired AKI, whereas, among patients with urgent/emergent admissions, both decreased serum ionized calcium of ≤ 4.79 mg/dL and elevated serum ionized calcium of ≥ 5.20 mg/dL were significantly associated with increased risk of hospital-acquired AKI (Table S1). However, there was no interaction between serum ionized calcium and admission type on the risk of hospital-acquired AKI (p-interaction = 0.18).
The subgroup analysis based on admission service showed that among patients admitted in medical service, only decreased serum ionized calcium ≤ 4.59 mg/dL was significantly associated with increased risk of hospital-acquired AKI, whereas, among patients admitted in surgical service, both decreased serum ionized calcium of ≤ 4.59 mg/dL and elevated serum ionized calcium of ≥ 5.20 mg/dL were significantly associated with increased risk of hospital-acquired AKI (Table S2). However, there was no interaction between serum ionized calcium and admission service on the risk of in-hospital AKI (p-interaction = 0.73).
Discussion
The findings of our study showed an independent association between admission level of serum ionized calcium and the risk of in-hospital AKI with a U-curve association. Ionized calcium ≤ 4.59 mg/dL or ≥ 5.20 mg/dL was significantly associated with higher occurrence of in-hospital AKI. For subgroup analysis of the risk of in-hospital severe AKI, our results suggested that ionized calcium ≤ 4.79 mg/dL or ≥ 5.20 mg/dL was significantly associated with higher risk of severe AKI.
Previous studies have demonstrated the AKI risk among patients with various serum calcium levels14,15,22. However, total calcium measurements have considerable limitations in the identification of actual calcium abnormalities, such as its dependency on serum albumin level10. Our study is the largest cohort to demonstrate the U-curve association between serum ionized calcium and risk of in-hospital AKI. We postulated that abnormality in calcium affects vascular tone, including renal vessels. The imbalance between renal vasoconstriction and vasodilatation, in turn, could result in AKI. Hypercalcemia interferes with the kidneys’ ability to concentrate urine leading to volume depletion with predisposition to AKI15. Nonetheless, it could be the degree of severity of the disease that explains this association. Low serum ionized calcium might be related to severity of the illness or sepsis23,24,25. The inflammatory cytokines during the illness impair PTH secretion from parathyroid gland along with resistance to PTH at the end-organs26. Furthermore, calcitriol production is also suppressed during this severe illness27. These result in low serum ionized calcium. At the same time, severity of the disease is also associated with higher risk of AKI. Among critically ill patients with AKI, recent study demonstrated that low serum ionized calcium levels were independent predictors of all-cause mortality8. Further studies are needed to understand more about the mechanistic pathways of this association.
Our study has several limitations. First, the design of the study is observational and retrospective. Hence, causal relationship cannot be established. In addition, some critical information, such as the causes of serum ionized calcium derangements, urine output, and urine electrolytes, were not available or incomplete in our database and, therefore, we were not able to report them. There might be some residual confounders that we unaccounted for when we analyzed the association. Second, we had only single level of serum ionized calcium at the admission so we could not explore whether the time course of changes in serum ionized calcium might influentially affect the risk of AKI. Third, as serum ionized calcium levels at hospital admission were the predictor of interest, only patients with available admission serum ionized calcium were included. However, serum ionized calcium levels were measured in a limited proportion of hospitalized patients at the time of hospital admission (Figure S1). As shown in Table S3, patients with admission serum ionized calcium had lower baseline kidney function, higher comorbidity burden, and were more primarily admitted for cardiovascular and hematology/oncology disease than those without admission serum ionized calcium. Given a potential selection bias, the generalizability of the study finding to patients without admission serum ionized calcium measurement remains unknown. However, strengths of our study should be emphasized. First, we investigated the non-linearity association with restricted cubic spline. Furthermore, we also explored for risk of severe AKI defined as AKI stage 2 and 3 apart from any AKI. Since AKI is associated with increased mortality among hospitalized patients2,3,5,6, future studies are needed to assess whether the incorporation of ionized calcium levels in a prognostic model at the time of hospital admission will help identify high-risk patients for AKI during hospitalization. Besides, further trials to investigate the benefit of protocol for correction of abnormal serum ionized calcium levels on the risk of AKI in hospitalized patients may be necessary.
To summarize, admission ionized calcium either ≤ 4.59 mg/dL or ≥ 5.20 mg/dL is significantly associated with a higher risk of in-hospital AKI while admission serum ionized calcium of either ≤ 4.79 mg/dL or ≥ 5.20 mg/dL is significantly associated with higher risk of in-hospital severe AKI.
References
1Levey, A. S. & James, M. T. Acute Kidney Injury. Ann Intern Med 167, Itc66–itc80, https://doi.org/10.7326/aitc201711070 (2017).
Zuk, A. & Bonventre, J. V. Acute kidney injury. Annu. Rev. Med. 67, 293–307. https://doi.org/10.1146/annurev-med-050214-013407 (2016).
Thongprayoon, C., Cheungpasitporn, W., Akhoundi, A., Ahmed, A. H. & Kashani, K. B. Actual versus ideal body weight for acute kidney injury diagnosis and classification in critically Ill patients. BMC Nephrol. 15, 176. https://doi.org/10.1186/1471-2369-15-176 (2014).
Kashani, K., Cheungpasitporn, W. & Ronco, C. Biomarkers of acute kidney injury: The pathway from discovery to clinical adoption. Clin. Chem. Lab. Med. 55, 1074–1089. https://doi.org/10.1515/cclm-2016-0973 (2017).
Mehta, R. L. et al. International Society of Nephrology’s 0 by 25 initiative for acute kidney injury (zero preventable deaths by 2025): A human rights case for nephrology. Lancet 385, 2616–2643. https://doi.org/10.1016/S0140-6736(15)60126-X (2015).
Cheng, X., Wu, B., Liu, Y., Mao, H. & Xing, C. Incidence and diagnosis of Acute kidney injury in hospitalized adult patients: A retrospective observational study in a tertiary teaching Hospital in Southeast China. BMC Nephrol. 18, 203. https://doi.org/10.1186/s12882-017-0622-6 (2017).
Auron, A. & Alon, U. S. Hypercalcemia: A consultant’s approach. Pediatr. Nephrol. 33, 1475–1488. https://doi.org/10.1007/s00467-017-3788-z (2018).
Wang, B., Li, D., Gong, Y., Ying, B. & Cheng, B. Association of serum total and ionized calcium with all-cause mortality incritically ill patients with acute kidney injury. Clin. Chim. Acta 494, 94–99. https://doi.org/10.1016/j.cca.2019.03.1616 (2019).
Hästbacka, J. & Pettilä, V. Prevalence and predictive value of ionized hypocalcemia among critically ill patients. Acta Anaesthesiol. Scand. 47, 1264–1269. https://doi.org/10.1046/j.1399-6576.2003.00236.x (2003).
10Thongprayoon, C. et al. Hospital mortality and long-term mortality among hospitalized patients with various admission serum ionized calcium levels. Postgrad. Med., 1–6, https://doi.org/10.1080/00325481.2020.1728980 (2020).
Thongprayoon, C., Cheungpasitporn, W., Chewcharat, A., Mao, M. A. & Kashani, K. B. Serum ionised calcium and the risk of acute respiratory failure in hospitalised patients: A single-centre cohort study in the USA. BMJ Open 10, e034325. https://doi.org/10.1136/bmjopen-2019-034325 (2020).
Kruger, J. M., Osborne, C. A., Nachreiner, R. F. & Refsal, K. R. Hypercalcemia and renal failure: Etiology, pathophysiology, diagnosis, and treatment. Vet. Clin. N. Am. Small Anim. Pract. 26, 1417–1445. https://doi.org/10.1016/S0195-5616(96)50135-X (1996).
Baker, S. Jr., Cohen, A. J., Fray, J. C. & Laurens, N. J. Role of calcium and albumin in the autoregulation of renal perfusate flow. J. Physiol. 311, 1–9. https://doi.org/10.1113/jphysiol.1981.sp013569 (1981).
Thongprayoon, C., Cheungpasitporn, W., Mao, M. A., Sakhuja, A. & Erickson, S. B. Admission calcium levels and risk of acute kidney injury in hospitalised patients. Int. J. Clin. Pract. 72, e13057. https://doi.org/10.1111/ijcp.13057 (2018).
Moysés-Neto, M. et al. Acute renal failure and hypercalcemia. Ren. Fail. 28, 153–159. https://doi.org/10.1080/08860220500531005 (2006).
Cheungpasitporn, W., Thongprayoon, C. & Erickson, S. B. Admission hypomagnesemia and hypermagnesemia increase the risk of acute kidney injury. Ren. Fail. 37, 1175–1179. https://doi.org/10.3109/0886022X.2015.1057471 (2015).
Thongprayoon, C., Cheungpasitporn, W., Mao, M. A., Harrison, A. M. & Erickson, S. B. Elevated admission serum calcium phosphate product as an independent risk factor for acute kidney injury in hospitalized patients. Hosp. Pract. 47, 73–79. https://doi.org/10.1080/21548331.2019.1568719 (2019).
Paunier, L. Effect of magnesium on phosphorus and calcium metabolism. Monatsschr Kinderheilkd 140, S17-20 (1992).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Charlson, M., Szatrowski, T. P., Peterson, J. & Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 47, 1245–1251 (1994).
21Group., K. D. I. G. O. K. A. K. I. W. KDIGO clinical practice guidelines for acute kidney injury. Kidney Int. suppl 2, 1–138 (2012).
Aihara, S. et al. Hypercalcemia and acute kidney injury induced by eldecalcitol in patients with osteoporosis: A case series of 32 patients at a single facility. Ren. Fail. 41, 88–97. https://doi.org/10.1080/0886022x.2019.1578667 (2019).
Ridefelt, P. & Helmersson-Karlqvist, J. Albumin adjustment of total calcium does not improve the estimation of calcium status. Scand. J. Clin. Lab. Invest. 77, 442–447. https://doi.org/10.1080/00365513.2017.1336568 (2017).
Hu, Z. D., Huang, Y. L., Wang, M. Y., Hu, G. J. & Han, Y. Q. Predictive accuracy of serum total calcium for both critically high and critically low ionized calcium in critical illness. J. Clin. Lab. Anal. 32, e22589. https://doi.org/10.1002/jcla.22589 (2018).
D'Orazio, P., Visnick, H. & Balasubramanian, S. Accuracy of commercial blood gas analyzers for monitoring ionized calcium at low concentrations. Clin. Chim. Acta Int. J. Clin. Chem. 461, 34–40. https://doi.org/10.1016/j.cca.2016.07.010 (2016).
Prosnitz, A. R. et al. Changes in vitamin D and parathyroid hormone metabolism in incident pediatric Crohn’s disease. Inflamm. Bowel Dis. 19, 45–53. https://doi.org/10.1002/ibd.22969 (2013).
de Brito Galvao, J. F., Nagode, L. A., Schenck, P. A. & Chew, D. J. Calcitriol, calcidiol, parathyroid hormone, and fibroblast growth factor-23 interactions in chronic kidney disease. J. Vet. Emerg. Crit. Care (San Antonio) 23, 134–162. https://doi.org/10.1111/vec.12036 (2013).
Author information
Authors and Affiliations
Contributions
C.T., W.C. and K.B.K. originated the idea, and designed study. C.T., W.C., A.C., M.A.M., T.B., S.V., and S.T. collected data. C.T. analyzed the data. C.T. and A.C. were responsible for writing the manuscript. W.C., M.A.M., T.B., S.V., S.T., and K.B.K. supported the editing of the manuscript and added important comments to the manuscript. K.B.K. supervised the study. All authors had access to the data, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thongprayoon, C., Cheungpasitporn, W., Chewcharat, A. et al. Impact of admission serum ionized calcium levels on risk of acute kidney injury in hospitalized patients. Sci Rep 10, 12316 (2020). https://doi.org/10.1038/s41598-020-69405-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69405-0
- Springer Nature Limited