Abstract
Our aim was to assess the potential of flash glucose monitoring (FGM) for diagnostic workup of suspected post-bariatric hypoglycaemia (PBH). Patients (N = 13) with suspected PBH underwent a food and symptoms diary (FSD) record along with FGM over 14 days. Targeted data analysis confirmed the occurrence of low glucose events in parallel to meal-triggered symptoms. Glycaemic variability, as assessed by Mean Absolute Glucose change (MAG change), was increased, while a higher risk of glycaemic excursions towards both hyper and hypoglycaemia (ADRRFGMGT) was observed in those with more frequent and severe hypoglycaemia. The herein described hypoglycaemia risk index (LBGIFGMGT) with a cut-off value of 4.6 showed to have 100% sensitivity and 100% specificity for PBH. This pilot proof-of-concept study highlighted that FSD coupled with FGM followed by targeted data analysis, provides relevant insights towards PBH diagnosis and grading in a user-friendly and easy to implement study protocol. Furthermore, LBGIFGMGT demonstrated to be an excellent index for PBH diagnosis. The unexpected improvement of glucose profile noticed along the monitoring time also unravels a possible application for PBH management.
Similar content being viewed by others
Introduction
Bariatric surgery is the most effective treatment currently available for patients with morbid obesity, which was proved to achieve long-term weight loss and sustained remission of obesity-related comorbidities1,2. Despite benefits of bariatric surgery largely surpass the risks of the procedures, early and late complications can still occur3.
Post-bariatric hypoglycaemia (PBH) is a rare yet emerging clinical condition that was first consistently described in 20104. PBH has been mainly reported as a late complication of Roux-en-Y gastric bypass (RYGB)5,6,7,8 although occasionally presenting after other bariatric surgery procedures9,10,11,12. PBH is characterized by the occurrence of recurrent postprandial hypoglycaemic events in the presence of normal fasting glucose8,13,14 and has the potential to impair considerably the patients’ well-being and quality of life15.
PBH diagnosis is currently grounded on the exclusion of other causes for hypoglycaemia in a patient previously submitted to bariatric surgery, since there are no established diagnostic criteria currently available8. In addition, despite many hypotheses have been raised, the aetiology of PBH remains uncertain5,7,8.
Identifying PBH as a possible cause for post-bariatric patient complaints can be challenging, as hypoglycaemia can present as a large spectrum of unspecific clinical features, including autonomic and neuroglycopenic symptoms such as tremor, sweating, loss of consciousness and even seizures8,14, which depending of the predominant signs can lead the clinicians to consider several different conditions in the differential diagnosis ranging from dumping syndrome to epilepsy4.
Depending on the criteria used for diagnosis, PBH prevalence can range from 0.2% if based on hospitalization records due to hypoglycaemia4 to 6.6% if grounded on symptomatic reports only16, so the actual prevalence of PBH is difficult to ascertain. Therefore, an elusive clinical presentation along with the absence of established criteria for PBH diagnosis or clinical management guidelines make this condition particularly challenging.
Our aim was to assess the potential for the use of flash glucose monitoring (FGM) with targeted data analysis in the clinical workup of patients with PBH, based on the outcomes of its implementation in a pilot proof-of-concept study.
Results
Subjects (N = 13) previously submitted to RYGB surgery that self-reported symptoms suggestive of hypoglycaemia were divided into two sub-groups No PBH (interstitial fluid glucose [IFG] < 54 mg/dl < 1%) and PBH (IFG < 54 mg/dl ≥ 1%) according to FGM profile. Detailed patient case descriptions are presented to illustrate the two different conditions despite similar clinical presentations.
Anthropometric, metabolic and demographic patient characteristics
Before surgery, all subjects fulfilled the international clinical criteria to undergo bariatric surgery for primary treatment of obesity and related comorbidities2. No significant differences in anthropometric and metabolic parameters were observed between patient subgroups before or after surgery (p > 0.05) (Table 1).
Food and symptoms diary and flash glucose monitoring targeted data analysis
FGM and food and symptoms diary (FSD) data were analysed for a median total time corresponding to sensor lifetime (14 days) subtracted of the first 48 h and the time of data loss due to missed scanning within an 8-h interval (No PBH: 11.87 [11.78–11.91] days, median [P25–P75]; PBH: 11.90 [11.80–11.95]) (Table 2).
FGM data analysis revealed that short-term (mean absolute glucose change [MAG change]17), intra-daily (continuous overlapping net glycaemic action [CONGA1]) and inter-daily glucose variability (mean of daily differences [MODD]) patterns were similar in both sub-groups (Table 2).
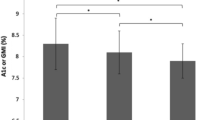
In contrast, glucose deviations from target range were significantly different between groups (average daily risk ratio [adjusted] [ADRRFGMGT]), with PBH sub-group presenting significant deviations from target range that were more pronounced towards the low glucose range (low blood glucose index [adjusted] [LBGIFGMGT]) rather than to the high glucose range (High Blood Glucose Index [adjusted] [HBGIFGMGT]) (Table 2, Fig. 1a).
(a) Individual LBGIFGMGT of the patient study group (N = 13), according to FGM profile No PBH (IFG < 54 mg/dl < 1%, n = 5) and PBH (IFG < 54 mg/dl ≥ 1%, n = 8), based on established criteria for level 2 hypoglycaemia; Data is represented as mean ± standard error of the mean;**p < 0.01. (b) ROC curve analysis of the value of LBGIFGMGT (ROC curve AUC = 1.000; p = 0.003) to assess BPH severity. At the optimal cut-off value of 4.6, LBGIFGMGT had 100% sensitivity and 100% specificity for the assessment of PBH severity (No PBH: LBGIFGMGT ≤ 4.6; PBH: LBGIFGMGT > 4.6). PBH post-bariatric hypoglycaemia, ROC receiver operating characteristic, LBGIFGMGT low blood glucose index (adjusted), AUC area under the curve.
Additionally, LBGIFGMGT as a surrogate of hypoglycaemia risk proved to be an excellent index to confirm PBH using a cut-off value of over 4.6 (area under the receiver operating characteristic [ROC] curve [AUC] = 1.000, standard deviation = 0.000, 95% CI 1.000, 1.000, p = 0.003), being 100% sensitive and 100% specific for PBH in individuals with compatible symptoms (Fig. 1b, Supplementary Table S1 online).
Detailed case descriptions
Two patients with obesity without type 2 diabetes underwent a standardized RYGB procedure performed by the same surgeons and were followed-up by the same multidisciplinary team. After undergoing RYGB, both subjects achieved a successful weight reduction of over 50% of excess weight (excess Body Mass Index [BMI] loss [%EBMIL]: A: 99.4%; B: 52.9%) with improvement of comorbid conditions. Both subjects spontaneously reported the onset of symptoms suggestive of hypoglycaemia over 4 years after surgery, with no evidence of glucose intolerance or type 2 diabetes while off any drugs with glucose-lowering potential (glycated haemoglobin [HbA1c]: A: 4.9%; B: 5.3%) (Table 3).
Patient A is a 37 years-old Caucasian female that underwent laparoscopic RYGB for the treatment of obesity grade II (BMI 35.3 kg/m2) with gastro-oesophageal reflux disease and osteoarthritis (OA) as obesity comorbidities. Almost 5 years after RYGB surgery with a BMI of 25.1 kg/m2, unremarkable biochemical and metabolic profiles and fully resolved obesity comorbidities, the patient spontaneously reported during a routine medical appointment the onset of episodic postprandial sweating and near fainting since the past 3 months. At that time, the patient was only under multivitamin supplements (Table 3).
Patient B is a 52 years-old Caucasian female submitted to laparoscopic RYGB for the treatment of obesity grade III (weight 108 kg, BMI 43.3 kg/m2), dyslipidaemia and OA, who despite still being obese experienced a 10-point reduction in BMI with normalization of the lipid profile after the procedure. Four years after surgery, the patient was attended at the emergency department for loss of consciousness with hypoglycaemia documented by paramedics. Past medical history was otherwise irrelevant, apart from primary hypothyroidism diagnosed 20-years earlier for which she was under levothyroxine replacement therapy with a normal thyroid function in addition to the multivitamin supplements (Table 3).
Both patients depicted surrogate measures (updated homeostasis model assessment indexes [HOMA2]) of preserved beta cell function (HOMA2-%β: A: 83.9%; B: 109.7%; reference value: > 72.5% for female18) and normal peripheral insulin resistance (HOMA2-IR: A: 0.75; B: 1.33; reference value: < 1.41 for female18) and sensitivity (HOMA2-%S: A: 132.7%; B: 75.1%; reference value: > 63.7% for female18) (Table 3).
Analysing the FSD and FGM records for similar time periods (patient A: 11.87 days; patient B: 11.88, Table 4), patient A and patient B had 3 and 12 low glucose events (LGEs), respectively. In both patients, LGE occurred in the postprandial period with a 60 to 90 min interval after a glucose excursion (LGE preceded by interstitial fluid glucose [IFG] >140 mg/dl: A: 100% [3 of 3]; B: 83.3% [10 of 12]) leading to either low (LGE with IFG nadir < 54 mg/dl: A: 100% [3 of 3]; B: 91.7% [11 of 12]) or very low (LGE with IFG nadir < 40 mg/dl: A: 0% [0 of 3]; B: 33.3% [4 of 12]) glucose nadirs (Table 4). Paired FSD and FGM data analysis revealed that patient A and B experienced 1 of 3 and 3 of 12 symptomatic LGE, respectively. Symptomatic reports not matching LGE were exclusively reported by patient B (2 of 5). Symptoms were either neuroglycopenic (A: none; B: 2) or neuroglycopenic plus autonomic (A: 1; B: 3), with none of the patients reporting the exclusive occurrence of autonomic symptoms (Table 4).
Greater glucose excursions were observed in patient B (IFG maximal excursion: A: 111.7 ± 2.4 mg/dl; B: 130.1 ± 18.7 mg/dl) and lead to longer lasting glucose fluctuations (time from IFG peak to nadir: A: 69.7 ± 4.4 min; B: 90.9±6.0 min) (Table 4). Central tendency measures of IFG records, median and interquartile range (A: 90 [79–111] mg/dl; B: 88 [78–114] mg/dl), depicted no apparent differences between study subjects. Both patients presented a higher glucose variability during daytime as compared to overnight periods (Fig. 2a,b) along with overall similar intra-daily glucose variability (CONGA1: A: 2.4; B: 2.9) (Table 4).
Flash glucose monitoring data graphical illustration. Daily glucose profile (a,b) and Poincaré plot (c,d) of patients A (a,c) and B (b,d) and hypoglycaemia risk per day (e) and per weekday (f). Poincaré plots (c,d) relate each record (IFGti) with the previous one (IFGti−1). Glycaemic target range (70–140 mg/dl) is marked in dots (a–d) and hypoglycaemia risks are illustrated by different colours (e,f) low 0.1–1.0; moderate 1.0–4.1; high > 4.1. IFG interstitial fluid glucose, LBGIFGMGT Low Blood Glucose Index (adjusted).
The deviations from target glucose range (%time out of range: A: 10.19%; B: 22.52%; ADRRFGMGT: A: 50.2; B: 67.1), including percentage of time above (A: 7.23%; B: 11.99%) or below target (Time IFG < 70 mg/dl: A: 2.95%; B: 10.53%; Time IFG < 54 mg/dl: A: 0.00%; B: 2.92%), and risks of high (HBGIFGMGT: A: 2.4; B: 3.3) or low glucose (LBGIFGMGT: A: 2.3; B: 5.2) diverged between the two patients (Table 4). A higher dispersion of IFG consecutive records, suggestive of fast short-term glucose fluctuations (MAG change: [A: 2.7; B: 3.0; reference values: 0.5–2.2] mmol/l × h−117), was observed in both post-RYGB patients, although higher for Patient B (Fig. 2c,d) (Table 4).
This trend is illustrated by the Poincaré plots with greater dispersion of values towards both low and high glucose levels and around the x = y line, depicting the higher tendency for fast glucose changes and risk of hypoglycaemia in Patient B, despite the similitude of central tendency measures represented by the ellipses (mean ± SD: A: 100 ± 30 mg/dl; B: 100±38) (Fig. 2c,d).
Summary measures of inter-daily glucose variability (MODD: A: 1.2; B: 1.6) were not visibly different between the two patients (Table 4). However, graphical representation of hypoglycaemia risk throughout the monitoring period depicted a moderate hypoglycaemia risk for Patient A and a higher hypoglycaemia risk in the initial days of FGM for Patient B (Fig. 2e,f). These findings were similar to those observed in study subgroup analysis (Table 2).
Discussion
Herein we describe 13 patient cases presenting with PBH5,6,7,8 and two of them in further detail. PBH is a condition for which there are no established diagnosis criteria nor recommended investigation protocols8. The only consensus is that hypoglycaemia as cause of patient symptoms must be confirmed in accordance to the Whipple triad8 and other endocrine and non-endocrine causes for hypoglycaemia, including insulinoma and glucose lowering drugs, should be ruled out in patients with past-medical history of bariatric surgery before assuming the diagnosis of PBH. Since patients typically present with normal fasting glucose and postprandial hypoglycaemia that occurs most often 60 to 180 min after a meal8,14, the use of provocative tests with oral glucose7 or liquid13 and even solid19 mixed meals as tools to diagnose PBH has been proposed. However, these provocative tests represent an artificial scenario and a positive test with reactive hypoglycaemia is often observed in post-bariatric patients without further evidence of the condition, thus overestimating PBH diagnosis8. Therefore, given the aforementioned unmet needs, we hypothesized that a FSD coupled with FGM could be a useful tool for diagnosis and risk stratification of patients presenting clinical features suggestive of PBH.
To test this hypothesis, patients were requested to record food intake and symptoms experienced while monitoring IFG with the commercially available FGM system instead of using a continuous glucose monitoring (CGM) system. The medical device used in this study allows to retrieve CGM-like data with an overall good accuracy, including over periods of fast glycaemic excursions, despite being slightly less accurate in the low glucose range and having a relatively high lower limit of detection (2.2 mmol/l, 40 mg/dl) when compared to other glucose monitoring systems20,21, therefore carrying the potential risk of underestimating the occurrence of severe hypoglycaemia. For the purpose of this study, using the FGM system had the advantages of being widely available in community pharmacies, relatively inexpensive, easy to use, not requiring finger prick calibration and having a patient-friendly software20. Furthermore, as the FGM device used does not provide hypo or hyperglycaemic alerts, thus avoiding a source of bias raised by hypoglycaemia awareness generated by system alarms instead of driven by patient symptoms20.
Paired analysis of symptom entries and FGM data made evident the discrepancy between symptoms and IFG levels, with symptoms compatible with hypoglycaemia not always matching low IFG. This came as no surprise, since hypoglycaemia symptoms are highly unspecific and overlap with those typical of dumping syndrome, a common complication of upper gastrointestinal surgery14. This finding highlights the potential of this protocol for screening patients with suspected PBH in order to document hypoglycaemia as the cause of patient symptoms, while avoiding further investigation if not confirmed.
A more detailed analysis of FSD and IFG records allowed to disclose the key clinical elements of PBH, namely the occurrence of postprandial LGE after a high glucose excursion, along with reassuring steady overnight and fasting glucose profiles. This glucose pattern tends to characterize PBH, in contrast to other conditions presenting with fasting hypoglycaemia, such as insulinomas8,11,13,14.
Targeted FGM data analysis provided further insights into glucose dynamics. Summary measures, such as mean and standard deviation, but also median, percentile distribution and the time spent in each glycaemic range are widely available since these are computed by FGM and CGM devices’ software. However, these summary measures often fail to depict glycaemic fluctuation trends22. In contrast, our data analysis protocol provides additional insights into glycaemic variability patterns, including speed of glycaemic variation (MAG change), overall magnitude of deviations towards hyper and hypoglycaemic range (HBGIFGMGT and LBGIFGMGT respectively) and daily patterns (ADRRFGMGT and MODD). These parameters revealed to be significantly different in our study sub-group subjects. Moreover, assessing glycaemic variability is clinically relevant since it can be associated with adverse cardiovascular outcomes23.
In fact, MAG change allowed to document the presence of high glucose variability17. Indeed, high glycaemic variability has been broadly reported after RYGB24,25 in addition to rapid glycaemic fluctuations26 towards both hyper and hypoglycaemia (ADRRFGMGT27), which are well recognized risk factors for PBH13,28. Moreover, the percentages of time out of glucose target range and the risk variables computed with FGM retrieved data (LBGIFGMGT29,30, HBGIFGMGT29,30 and ADRRFGMGT27) revealed two distinct hypoglycaemia risk profiles. A higher LBGIFGMGT29,30 or HBGIFGMGT29,30 reflect a greater tendency for hypoglycaemia or hyperglycaemia even if not consummated, which is clinically relevant when considering primary prevention. Furthermore, intra-daily overall glucose variability26 (CONGA131) matched the glucose unpredictability32, as graphically suggested by the daily glucose profiles curves and Poincaré plots, with greater glucose excursions during daytime as compared to the more steady glucose values observed overnight as previously reported13. This occurred despite the apparent absence of relevant inter-daily glycaemic profiles variability (MODD33).
In addition, FGM data also enabled to assess the frequency and severity of LGE. In particular, this allowed to differentiate the profiles of patient A and B, with patient B experiencing more frequent and severe hypoglycaemic events. Noteworthy, the same patient had a higher BMI and a lower %EBMIL. Despite some evidence suggesting that post-RYGB patients with lower BMI are more likely to experience hypoglycaemia16,34, overeating to correct or prevent hypoglycaemia with subsequent weight gain is a well-known phenomenon among patients with diabetes, described in PBH as well6,35. A mismatch between symptoms and frequency or severity of hypoglycaemia was also observed, as the patient with the most severe and recurrent LGE was proportionally the least symptomatic, thus suggesting that frequent hypoglycaemic events also raise the risk of hypoglycaemia unawareness in patients without diabetes8,15.
Moreover, from glucose profile analysis, it was also noticeable that the risk of hypoglycaemia in the patient with the more severe PBH profile was higher in the first days of FGM monitoring. Long-term usage of FGM systems was reported to decrease the occurrence of hypoglycaemia that has been attributed to increased self-awareness over glucose fluctuations, ultimately leading to patient behaviour modification36. Thus, our data further supports the potential use of this protocol for PBH management by promoting patient elicited behavioural changes and modification of eating habits and eventually by allowing tailored dietary interventions by healthcare practitioners.
Noteworthy is the fact that the aforementioned indexes of glycaemic variability that allowed the detailed characterization of the patients’ glucose profile are the end result of the calculation of new mathematical models after the originally described in the literature30 for symmetrizing glucose values, which resulted in new risk variables (LBGIFGMGT, HBGIFGMGT and ADRRFGMGT). The mathematical function was recalculated to match the glucose limits of the device (40–500 mg/dl; 2.2–27.8 mmol/l)20, with a higher lower detection limit of 40 mg/dl (2.2 mmol/l) than the 20 mg/dl (1.1 mmol/l) considered in the original model and a lower upper detection limit of 500 mg/dl (27.8 mmol/l), against the original one (600 mg/dl; 33.3 mmol/l). This model adjustment was necessary to prevent underestimation of hypoglycaemia and hyperglycaemia risks. Additionally, the target glucose range was adjusted to the physiological glucose range (70–140 mg/dl; 3.9–7.8 mmol/l), since this differs from the target glucose range used in the original model for patients with diabetes (70–180 mg/dl; 3.9–10.0 mmol/l)30.
To the best of our knowledge, this proof-of-concept study is the first to demonstrate the potential use of the FGM technology for the differential diagnosis and management of PBH. Besides enabling PBH diagnosis, this protocol has potential for fine tuning patient care by allowing risk stratification and setting the grounds for improved clinical management. Nevertheless, this protocol still requires further validation by assessing glycaemic dynamics in different bariatric patient populations, including matched asymptomatic surgical and non-surgical controls in order to validate the metrics herein computed in addition to its added value as a diagnostic tool.
PBH remains an unmet clinical challenge. The use of a FSD coupled with FGM for clinical assessment of patients with suspected PBH including the usefulness of LBGIFGMGT index as a diagnostic tool was herein demonstrated. Our results highlight that a user-friendly and easy to implement study protocol followed by targeted data analysis is able to retrieve relevant insights towards PBH diagnosis, grading or even patients’ management, by eliciting modifications of patient habits and allowing tailored dietary intervention.
Methods
Subject selection and study protocol
Subjects (N=13) previously submitted to RYGB surgery that self-reported symptoms suggestive of hypoglycaemia were enrolled on convenience basis, as first come first offer, to undergo a comprehensive clinical assessment to confirm or exclude the PBH, in line with our previous studies37. Two patient cases are reported in further detail to illustrate the clinical utility of the proposed protocol.
After an initial standard of practice evaluation to exclude other causes of hypoglycaemia, including endocrine disorders and drugs, patients were requested to fill a FSD while using a commercially available FGM system (FreeStyle Libre, Abbott Diabetes Care, Maidenhead, UK)20. This FGM medical device performs automatic measurements of IFG every 15 min for 14 consecutive days corresponding to the lifespan of a single disposable sensor. In addition, the device can provide estimates of IFG whenever the patient forces a reading20.
Subjects were given instruction on how to fill the FSD by providing information on time of onset and symptoms description in as much detail as possible and to scan the FGM sensor every 6 h to minimize data loss, as the maximum sensor storage capacity is 8 h. Entries of palpitations, tremor, anxiety, sweating, hunger or tingling/paraesthesia were classified as autonomic symptoms, whereas visual disturbances, headaches, weakness, slurred speech, confusion, concentration difficulties, drowsiness, altered consciousness or seizures were classified as neuroglycopenic symptoms, in line with previous position statements8.
This study protocol was submitted and approved by the Hospital Ethics Committee (Comissão de Ética do Centro Hospitalar Entre o Douro e Vouga) in compliance with the ethical standards of the World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Informed written consent was obtained from subjects before undertaking any study procedure. Additional consent to publish identifying information was also obtained from each individual participant.
Study sub-groups
Study subjects were divided into two sub-groups of patients according to FGM profile in No PBH (IFG < 54 mg/dl < 1%) and PBH (IFG < 54 mg/dl ≥ 1%), based on established criteria for level 2 hypoglycaemia38.
Biochemical measurements
Updated homeostasis model assessment indexes (HOMA2) values were calculated using fasting glucose and insulin levels assessed in the same day or within the previous 3 months of FGM fitting. Venous blood was collected from the antebrachial vein after a minimum 8 h overnight fast into EDTA tubes (S-Monovette 9.0 ml, K2 EDTA Gel, 1.6 mg/ml, Sarstedt). Blood glucose was measured in whole blood with a glucometer and converted into plasma glucose using the WHO conversion factor of 1.12 (FPG = WBG × 1.12)39. Plasma insulin levels were measured by electrochemiluminescence sandwich immunoassay (ECLIA) (Cobas 8000, model e602, Roche Diagnostics, USA), against liquid human serum-based controls: Liquichek Immunoassay Plus Control, Level 1 #361 and Level 3 #363, Bio-Rad.
Data analysis and mathematical modelling
Subjects’ data was retrieved from our clinical register and included age, gender, type of bariatric surgery procedure performed, comorbidities before the surgery, anthropometrics, biochemical profile routinely performed before and after surgery as standard of care and time elapsed since surgery until symptoms onset.
Percentage of excess BMI loss (EBMIL) was determined as EBMIL (%) = (preoperative BMI – BMI at FGM evaluation)/(preoperative BMI – 25) × 100. HOMA2 were calculated using the HOMA Calculator version 2.2.3 (https://www.dtu.ox.ac.uk, accessed April 2019) as surrogate measures of beta cell function (HOMA2-%β) and peripheral insulin sensitivity (HOMA2-%S) and resistance (HOMA2-IR).
Upon completion of the monitoring period, the sensor was removed and FGM raw data downloaded for targeted analysis. To ensure maximal data accuracy, including study participants’ adaptation to the device and equally timed records, IFG measurements during the first 48 h of monitoring and estimated glucose values provided by forced readings on patient demand were excluded from statistical analysis.
The glucose range target was set between 70 and 140 mg/dl (3.9–7.8 mmol/l) and the percentage of time under each glycaemic range (< 54; < 70; [70–140]; > 140 mg/dl; < 3.0; < 3.9; [3.9–7.8]; > 7.8 mmol/l) was determined by adding all the periods of at least two consecutive reads (duration ≥15 min) in each interval, therefore excluding all isolated reads corresponding to brief deviations lasting less than 15-min long towards another interval. Time gaps derived from IFG data loss due to overridden memory capacity, which is limited to 8 h without the need for sensor scanning, were taken into account and were not included to calculate the percentage of time spent in each glucose range.
A LGE was considered whenever a IFG < 70 mg/dl (< 3.9 mmol/l; hypoglycaemia alert or level 1 hypoglycaemia) with concurrent hypoglycaemia symptoms within a time lag between symptoms and IFG < 70 mg/dl of ± 30 min or whenever a IFG < 54 mg/dl (< 3.0 mmol/l; clinically substantial hypoglycaemia or level 2 hypoglycaemia) was recorded independently of symptoms, in accordance with the thresholds recommended by the American Diabetes Association38 and with the international consensus on CGM data interpretation40. LGEs were manually recorded to reduce the risk of bias, since patients with PBH often experience consecutive LGEs triggered by successive meals as attempts to correct a first hypoglycaemic episode that eventually result in “rebound hypoglycaemia”. In an automated data analysis process, these would be considered a single protracted LGE, while manual data analysis allows to disclose consecutive LGEs.
Median and interquartile range of the IFG data retrieved by FGM were determined as traditional central tendency measures suitable to describe non-Gaussian distributed data as continuous glucose patterns (Table 5)22. For mathematical computation of the FGM data, MAG change17,41, CONGA131 and MODD33 were calculated as previously described, to outline short-term, hourly and inter-daily glycaemic variability respectively26 (Table 5).
Additionally, glucose values were computed into low blood glucose index (LBGI)29,30, high blood glucose index (HBGI)29,30 and average daily risk ratio (ADRR)27, aimed to symmetrize glucose records while highlighting glucose deviations from the target range towards hypo-, hyperglycaemia or in both directions, respectively (Table 5), since glycaemic excursions towards hyperglycaemia are much more impactful in central tendency measures than deviations into the hypoglycaemic range. For this, the original risk analysis function used to compute these indexes was adjusted to the specific characteristics of the FGM system used. This classic function (Eq. (1)) was originally modelled using data from patients with diabetes assessed with glucose meters with detection ranges distinct from the currently used FGM system30,42. The function was recalculated following the original rationale42 to comply with the range of the device used (40–500 mg/dl; 2.2–27.8 mmol/l)20 and physiological glucose range (70–140 mg/dl; 3.9–7.8 mmol/l), which resulted in Eq. (2) (rational detailed in Table 6) and in adjusted indexes (LBGIFGMGT, HBGIFGMGT and ADRRFGMGT) (Table 5).
Graphical and statistical analysis
Ellipses in Poincaré plots were computed with centre on mean glucose and standard deviation as axes to depict overall glucose fluctuation32. Raw data was analysed using IBM SPSS Statistics Version 25 for Windows, for percentiles; GNU Octave version 4.4.0, for Poincaré plot computation; GraphPad Prism version 8.0.1 for Windows, GraphPad Software, San Diego, California USA, www.graphpad.com, for all other illustrations; and Excel 2016, Microsoft Office 365 ProPlus, for remaining calculations.
Data was independently analysed by two double-blinded researchers (CBL and SSP) and cross-matched for verification and validation of the protocol hereby summarized, with no differences found in the results.
For group data analysis, variables are expressed as median (interquartile range). Variables were assumed to be non-normally distributed due to small sample size and groups were compared using Mann-Whitney test. Categorical variables are represented as proportions and were compared using Fisher’s exact test. The differences between the two sub-groups were considered statistically significant when two-tailed p value was below 0.05.
The area under the ROC curve was used to determine the power of LBGIFGMGT to estimate PBH. Based on the AUC of the ROC curve, a diagnostic tool can be considered excellent (for values ranging from 0.90 to 1.00), good (0.80 to 0.90), fair (0.70 to 0.80), poor (0.60 to 0.70) or fail (below 0.60)43.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on request.
References
Hofso, D., Jenssen, T., Hager, H., Roislien, J. & Hjelmesaeth, J. Fasting plasma glucose in the screening for type 2 diabetes in morbidly obese subjects. Obes. Surg. 20, 302–307. https://doi.org/10.1007/s11695-009-0022-5 (2010).
Fried, M. et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes. Surg. 24, 42–55. https://doi.org/10.1007/s11695-013-1079-8 (2014).
Tack, J. & Deloose, E. Complications of bariatric surgery: Dumping syndrome, reflux and vitamin deficiencies. Best Pract. Res. Clin. Gastroenterol. 28, 741–749. https://doi.org/10.1016/j.bpg.2014.07.010 (2014).
Marsk, R., Jonas, E., Rasmussen, F. & Naslund, E. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986–2006 in Sweden. Diabetologia 53, 2307–2311. https://doi.org/10.1007/s00125-010-1798-5 (2010).
Patti, M. E., Li, P. & Goldfine, A. B. Insulin response to oral stimuli and glucose effectiveness increased in neuroglycopenia following gastric bypass. Obesity (Silver Spring) 23, 798–807. https://doi.org/10.1002/oby.21043 (2015).
Rariy, C. M., Rometo, D. & Korytkowski, M. Post-gastric bypass hypoglycemia. Curr. Diabetes Rep. 16, 19. https://doi.org/10.1007/s11892-015-0711-5 (2016).
Craig, C. M., Liu, L. F., Deacon, C. F., Holst, J. J. & McLaughlin, T. L. Critical role for GLP-1 in symptomatic post-bariatric hypoglycaemia. Diabetologia 60, 531–540. https://doi.org/10.1007/s00125-016-4179-x (2017).
Eisenberg, D., Azagury, D. E., Ghiassi, S., Grover, B. T. & Kim, J. J. ASMBS position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery. Surg. Obes. Relat. Dis. 13, 371–378. https://doi.org/10.1016/j.soard.2016.12.005 (2017).
Belligoli, A. et al. Incidence and predictors of hypoglycemia 1 year after laparoscopic sleeve gastrectomy. Obes. Surg. https://doi.org/10.1007/s11695-017-2742-2 (2017).
Michaels, A. D. et al. Hypoglycemia following bariatric surgery: Our 31-year experience. Obes. Surg. https://doi.org/10.1007/s11695-017-2734-2 (2017).
Abrahamsson, N., Eden Engstrom, B., Sundbom, M. & Karlsson, F. A. Hypoglycemia in everyday life after gastric bypass and duodenal switch. Eur. J. Endocrinol. 173, 91–100. https://doi.org/10.1530/EJE-14-0821 (2015).
Vilarrasa, N. et al. Hyperinsulinemic hypoglycemia after bariatric surgery: Diagnosis and management experience from a Spanish multicenter registry. Obes. Facts 9, 41–51. https://doi.org/10.1159/000442764 (2016).
Tharakan, G. et al. Roles of increased glycemic variability, GLP-1 and glucagon in hypoglycaemia after Roux-en-Y gastric bypass. Eur. J. Endocrinol. https://doi.org/10.1530/EJE-17-0446 (2017).
van Beek, A. P., Emous, M., Laville, M. & Tack, J. Dumping syndrome after esophageal, gastric or bariatric surgery: Pathophysiology, diagnosis, and management. Obes. Rev. 18, 68–85. https://doi.org/10.1111/obr.12467 (2017).
van Meijeren, J., Timmer, I., Brandts, H., Janssen, I. & de Boer, H. Evaluation of carbohydrate restriction as primary treatment for post-gastric bypass hypoglycemia. Surg. Obes. Relat. Dis. 13, 404–410. https://doi.org/10.1016/j.soard.2016.11.004 (2017).
Nielsen, J. B., Pedersen, A. M., Gribsholt, S. B., Svensson, E. & Richelsen, B. Prevalence, severity, and predictors of symptoms of dumping and hypoglycemia after Roux-en-Y gastric bypass. Surg. Obes. Relat. Dis. 12, 1562–1568. https://doi.org/10.1016/j.soard.2016.04.017 (2016).
Hill, N. R. et al. Normal reference range for mean tissue glucose and glycemic variability derived from continuous glucose monitoring for subjects without diabetes in different ethnic groups. Diabetes Technol. Ther. 13, 921–928. https://doi.org/10.1089/dia.2010.0247 (2011).
Ghasemi, A. et al. Cut-off points of homeostasis model assessment of insulin resistance, beta-cell function, and fasting serum insulin to identify future type 2 diabetes: Tehran lipid and glucose study. Acta Diabetol. 52, 905–915. https://doi.org/10.1007/s00592-015-0730-3 (2015).
Stano, S. et al. Effect of meal size and texture on gastric pouch emptying and glucagon-like peptide 1 after gastric bypass surgery. Surg. Obes. Relat. Dis. https://doi.org/10.1016/j.soard.2017.09.004 (2017).
Bailey, T., Bode, B. W., Christiansen, M. P., Klaff, L. J. & Alva, S. The performance and usability of a factory-calibrated flash glucose monitoring system. Diabetes Technol. Ther. 17, 787–794. https://doi.org/10.1089/dia.2014.0378 (2015).
Boscari, F. et al. FreeStyle Libre and Dexcom G4 Platinum sensors: Accuracy comparisons during two weeks of home use and use during experimentally induced glucose excursions. Nutr. Metab. Cardiovasc. Dis. 28, 180–186. https://doi.org/10.1016/j.numecd.2017.10.023 (2018).
Rodbard, D. Optimizing display, analysis, interpretation and utility of self-monitoring of blood glucose (SMBG) data for management of patients with diabetes. J. Diabetes Sci. Technol. 1, 62–71. https://doi.org/10.1177/193229680700100111 (2007).
Gorst, C. et al. Long-term glycemic variability and risk of adverse outcomes: A systematic review and meta-analysis. Diabetes Care 38, 2354–2369. https://doi.org/10.2337/dc15-1188 (2015).
Nosso, G. et al. Diabetes remission after bariatric surgery is characterized by high glycemic variability and high oxidative stress. Nutr. Metab. Cardiovasc. Dis. 27, 949–955. https://doi.org/10.1016/j.numecd.2017.07.004 (2017).
Nielsen, J. B., Abild, C. B., Pedersen, A. M., Pedersen, S. B. & Richelsen, B. Continuous glucose monitoring after gastric bypass to evaluate the glucose variability after a low-carbohydrate diet and to determine hypoglycemia. Obes. Surg. 26, 2111–2118. https://doi.org/10.1007/s11695-016-2058-7 (2016).
Monnier, L., Colette, C. & Owens, D. R. The application of simple metrics in the assessment of glycaemic variability. Diabetes Metab. https://doi.org/10.1016/j.diabet.2018.02.008 (2018).
Kovatchev, B. P., Otto, E., Cox, D., Gonder-Frederick, L. & Clarke, W. Evaluation of a new measure of blood glucose variability in diabetes. Diabetes Care 29, 2433–2438. https://doi.org/10.2337/dc06-1085 (2006).
Halperin, F., Patti, M. E., Skow, M., Bajwa, M. & Goldfine, A. B. Continuous glucose monitoring for evaluation of glycemic excursions after gastric bypass. J. Obes. 2011, 869536. https://doi.org/10.1155/2011/869536 (2011).
Kovatchev, B. P., Straume, M., Cox, D. J. & Farhy, L. S. Risk analysis of blood glucose data: A quantitative approach to optimizing the control of insulin dependent diabetes. Comput. Math. Methods Med. 3, 1–10 (2000).
Kovatchev, B. P., Cox, D. J., Gonder-Frederick, L. A. & Clarke, W. Symmetrization of the blood glucose measurement scale and its applications. Diabetes Care 20, 1655–1658. https://doi.org/10.2337/diacare.20.11.1655 (1997).
McDonnell, C. M., Donath, S. M., Vidmar, S. I., Werther, G. A. & Cameron, F. J. A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol. Ther. 7, 253–263. https://doi.org/10.1089/dia.2005.7.253 (2005).
Kovatchev, B. & Cobelli, C. Glucose variability: Timing, risk analysis, and relationship to hypoglycemia in diabetes. Diabetes Care 39, 502–510. https://doi.org/10.2337/dc15-2035 (2016).
Molnar, G. D., Taylor, W. F. & Ho, M. M. Day-to-day variation of continuously monitored glycaemia: A further measure of diabetic instability. Diabetologia 8, 342–348. https://doi.org/10.1007/bf01218495 (1972).
Vaurs, C. et al. Post-prandial hypoglycemia results from a non-glucose-dependent inappropriate insulin secretion in Roux-en-Y gastric bypassed patients. Metabolism 65, 18–26. https://doi.org/10.1016/j.metabol.2015.10.020 (2016).
Suhl, E., Anderson-Haynes, S. E., Mulla, C. & Patti, M. E. Medical nutrition therapy for post-bariatric hypoglycemia: Practical insights. Surg. Obes. Relat. Dis. https://doi.org/10.1016/j.soard.2017.01.025 (2017).
Bolinder, J., Antuna, R., Geelhoed-Duijvestijn, P., Kröger, J. & Weitgasser, R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: A multicentre, non-masked, randomised controlled trial. The Lancet 388, 2254–2263. https://doi.org/10.1016/S0140-6736(16)31535-5 (2016).
Marques, A. R. et al. Insights from the impact of meal composition on glucose profile towards post-bariatric hypoglycemia management. Obes. Surg. https://doi.org/10.1007/s11695-019-04147-1 (2019).
American Diabetes Association. Glycemic targets: Standards of medical care in diabetes—2019. Diabetes Care 42, S61–S70. https://doi.org/10.2337/dc19-S006 (2019).
Kotwal, N. & Pandit, A. Variability of capillary blood glucose monitoring measured on home glucose monitoring devices. Indian J. Endocrinol. Metab. 16, S248-251. https://doi.org/10.4103/2230-8210.104052 (2012).
Danne, T. et al. International consensus on use of continuous glucose monitoring. Diabetes Care 40, 1631–1640. https://doi.org/10.2337/dc17-1600 (2017).
Hermanides, J. et al. Glucose variability is associated with intensive care unit mortality. Crit. Care Med. 38, 838–842. https://doi.org/10.1097/CCM.0b013e3181cc4be9 (2010).
Kovatchev, B. P., Straume, M., Cox, D. J. & Farhy, L. S. Risk analysis of blood glucose data: A quantitative approach to optimizing the control of insulin dependent diabetes. J. Theor. Med. 3, 1–10 (2000).
Fan, J., Upadhye, S. & Worster, A. Understanding receiver operating characteristic (ROC) curves. Can. J. Emerg. Med. 8, 19–20 (2006).
Acknowledgements
The authors thank the patients who have participated in the study for trusting the clinical team on the off-label approach endeavoured towards the management of their condition. The authors also acknowledge Rita Magalhães, Department of Chemistry and Biochemistry, Faculty of Sciences, University of Porto, Porto, Portugal, and Henrique Vasconcelos, Department of Community Medicine, Information and Health Decision Sciences, Faculty of Medicine, University of Porto, Porto, Portugal for technical assistance with software. UMIB is funded by FCT (UID/MULTI/0215/2016, UID/MULTI/0215/2019, UIDB/00215/2020 and UIDP/00215/2020).
Author information
Authors and Affiliations
Contributions
C.B.L., M.G., M.N. and M.P.M. conceived and designed the study. M.G., M.N. and M.P.M. performed patients’ enrolment, assessment and data acquisition. C.B.L., S.S.P. and T.M. developed analysis protocol. P.O. and J.P.M.C. developed mathematical and statistical modelling. C.B.L. and S.S.P. analysed the data. C.B.L., S.S.P., M.G. and M.P.M. discussed the results and implications. C.B.L. drafted the manuscript. All authors have critically revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lobato, C.B., Pereira, S.S., Guimarães, M. et al. Use of flash glucose monitoring for post-bariatric hypoglycaemia diagnosis and management. Sci Rep 10, 11061 (2020). https://doi.org/10.1038/s41598-020-68029-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-68029-8
- Springer Nature Limited