Abstract
The present prospective follow-up study aimed to evaluate the effects of GRK5 polymorphisms on ritodrine efficacy and adverse drug events (ADEs) in pregnant women undergoing preterm labor. A total of 162 women undergoing preterm labor were included in the study. Seven single nucleotide polymorphisms (SNPs) in the GRK5 gene (rs915120, rs2230345, rs2230349, rs7923896, rs1020672, rs4752308, and rs4752292) were assessed. Homozygous variant carriers of rs4752292 and rs1020672 had 0.6 times the hazard of delivery compared to wild-type allele carriers (95% confidence interval [CI], 0.41~0.99 and 0.38~0.99, respectively). In addition, homozygous variant carriers of rs4752292 and rs1020672 had 2.4-fold more (95% CI, 1.10~4.98) and 2.3-fold more (95% CI, 1.04~5.06) ADEs compared to those with the wild-type homozygotes, respectively. Among demographic variables, gestational age and modified Bishop score were significant factors associated with time to delivery, while body weight and maximum ritodrine infusion rate were significant factors associated with ADEs. In silico analysis showed that both rs4752292 and rs1020672 had the potential to affect mRNA splicing by alteration of splicing motifs. The present study shows that ritodrine efficacy and ADEs are associated with GRK5 gene polymorphisms in pregnant women undergoing preterm labor.
Similar content being viewed by others
Introduction
Preterm birth, defined as birth before the usual 37 weeks of pregnancy, is one of the main causes of perinatal mortality and morbidities that persist into childhood1. As of now, upon diagnosis of preterm labor, tocolytic agents have been frequently utilized for the prolongation of pregnancy. Although the pathogenesis of preterm labor and functional mechanism of tocolytics are yet to be fully understood, it has been reported that many tocolytics act via G-protein coupled receptor (GPCR) signal-mediated pathways involved in myometrium relaxation and contraction2. Control of uterine contractility involves numerous neurotransmitters and hormones, which act through membranous receptors that activate intracellular signaling pathways. Beta adrenergic receptors activated by catecholamines exhibit a key function in the mediation of uterine relaxation, as can be observed by the role of beta agonists such as ritodrine in preterm labor treatment3,4.
Beta agonists bind and activate beta 2 adrenergic receptors located on the outer membrane of myometrial cells, increasing cAMP levels and thus resulting in a decrease of intracellular Ca2+ levels and uterine contraction5. Our previous study showed that ADRB2 polymorphisms affected beta agonist efficacy in pregnant women undergoing preterm labor6. Genetic polymorphisms in the beta adrenergic receptor are assumed to alter the binding affinity of beta agonists and consequently, the corresponding intracellular signaling pathways.
In addition, one of the important mechanisms mediating events following GPCR activation is receptor desensitization. Receptor desensitization is an adaptive process where cell responsiveness to extensive agonist stimulation is decreased, whereas reaction to other agonists or activators is unaffected. Desensitization commences with GPCR uncoupling, mediated by two different types of serine/threonine kinases; G protein-coupled receptor kinases (GRKs) and second messenger-dependent kinases, including cAMP-dependent protein kinase A (PKA) or protein kinase C (PKC)7. GRKs trigger homologous desensitization via the selective phosphorylation of agonist-bound GPCRs, while PKA and PKC initiate heterologous desensitization8. In the process of desensitization after beta agonist action, beta receptor phosphorylation is initiated by GRKs and beta arrestin binds to the complex. Sterically blocking G protein activation leads to beta adrenergic receptor endocytosis and desensitization. Therefore, GRKs are important regulators of GPCR function and mediate receptor desensitization, internalization, and signaling8.
GPCR kinases are a class of protein kinases encoded by GRK genes, which are composed of the genes GRK1 to GRK7. The seven GRK subtypes can be classified into three groups in a sequence homology-dependent fashion9. Members of the GRK1 family (GRK1 and GRK7) show retina-specific expression, while those of the GRK2 family (GRK2 and GRK3) exhibit a broader distribution. Among the GRK4 family members, GRK4 is localized to the testis, while GRK5 and GRK6 display ubiquitous expression8,9.
In vivo studies on GRK gene polymorphisms have been carried out in the context of several disease areas including cardiovascular disease, neuropsychiatric disease, and diabetes10,11,12,13,14. Uterine smooth muscle is regulated by the beta adrenergic pathway, and among the GRKs, GRK5 is highly expressed in the human myometrium15,16. However, there has been limited study of the effects of GRK5 polymorphisms on the myometrium.
Therefore, this study aimed to investigate the relationship between GRK5 polymorphisms and ritrodine efficacy and adverse drug events (ADEs) in pregnant women undergoing preterm labor.
Methods
Participants and data collection
The study was conducted at Ewha Womans University Mokdong Hospital in a prospective fashion, from January 2010 to December 201417. Criteria for eligibility of participation were as follows: age ≥18 years, preterm labor with intact membranes, gestational age of 20–36 weeks, and uterine contractions at a frequency of three per 10 min with cervical changes. Patients with the following high-risk conditions upon admission were excluded; pre-eclampsia, placental abruption, fetal distress, fetal/placental/amniotic abnormalities, placenta previa, severe spontaneous premature rupture of membranes, clinical chorioamnionitis or major vaginal bleeding. Patients treated with ritodrine to prevent uterine contractions during McDonald operation or treated with tocolytics other than ritodrine were excluded. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee and Institutional Review Board of Ewha Womans University Medical Center (IRB number: 217-1-26). Informed consent was obtained from each participant before the study.
The outcomes of therapy and clinical information were recorded and collected from electronic medical records. The primary endpoints were time to delivery and proportion of women who remained undelivered. In addition, ritodrine-induced ADEs were investigated as a secondary endpoint. ADEs were defined as cases of drug cessation or dose reduction due to presence of tachycardia, palpitations, dyspnea, shortness of breath, or pulmonary edema. Patient information included maternal age, body weight, height, gestational age, comorbidity, modified Bishop score, smoking status, time of initiation and termination of ritodrine therapy, ritodrine dose, and type of adverse event. All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
Drug administration
Ritodrine (Lavopa®; JW Pharmaceutical, Seoul, Korea) was administered via intravenous infusion at an initial rate of 0.05 mg/min which was increased by 0.05 mg/min every 10 min until the desirable uterine response was obtained. Intravenous treatment was discontinued during uterine quiescence. Patients who achieved uterine quiescence received maintenance therapy with an infusion of 0.05 mg/min for 12–48 h.
Genotyping
Blood samples were collected for genotyping during admission. Genomic DNA was extracted from ethylenediaminetetraacetic acid (EDTA)-blood samples using the QIAamp DNA Blood Mini Kit (QIAGEN GmbH, Hilden, Germany) following the manufacturer’s recommendations. GRK5 SNPs were selected based on previous studies and genetic information from UCSC genome browser10,13. In addition, genetic information about the GRK5 gene was incorporated into the software Haploreg ver 4.2 for the selection of GRK5 SNPs with a minor allele frequency (MAF) of ≥20% in the Japanese and Han Chinese populations. The linkage disequilibrium blocks were constructed following the D’-method18. One SNP in 5’ UTR (rs7923896), two missense SNPs (rs2230345 and rs2230349), and four intronic SNPs (rs915120, rs1020672, rs4752308 and rs4752292) were selected. A total of seven SNPs were genotyped using SNaPShot Multiplex kits.
Statistical analysis
The interval from start of ritodrine therapy to delivery was analyzed using the Kaplan-Meier survival data analysis method (log-rank test). Cox’s proportional-hazards model was used for exploratory multivariate analysis. Categorical variables were analyzed using the chi-squared test or the Fisher’s exact test. A multivariable logistic regression model was used to identify independent predictors using factors with a p-value < 0.1 in univariate analysis. The fit of the prediction model was assessed using the Hosmer-Lemeshow goodness-of-fit test. Discrimination of the model was further assessed via area under receiver operating curve (AUROC) analysis, which assessed the ability of risk factors to predict ritodrine-induced ADEs. On the basis of Rozenberg et al.’s study19 and the assumption that overall observed MAFs of chosen SNPs were 30%, the post-hoc power analysis was conducted with PROC Power of SAS 9.4 (SAS Institute, Cary, NC, USA). All statistical tests were conducted with a two-tailed alpha of 0.05. The data were analyzed using the Statistical Package for Social Sciences Version 20.0 for Windows (SPSS, Chicago, IL, USA).
In silico analyses
To predict the possible effects of given variants on splicing, different computational tools were used. Netgene220 and Splice Site Prediction by Neural Network (NNSPLICE)21 were used for splice site predictions. Alternations of the splicing factor binding site pattern caused by the given mutation were evaluated using Exonic Splicing Enhancer (ESE) finder 3.022 and Human Splicing Finder (HSF) 3.123. We used the default threshold values, and a score for a given sequence was considered to be potentially significant, if it was above the threshold values.
Results
A total of 216 women treated with ritodrine were enrolled. Sixteen who had already experienced severe symptoms, 10 who were scheduled for the McDonald operation, eight who had underlying cardiovascular diseases, and 20 without blood samples were excluded. A total of 162 patients were ultimately included in our study, and the post hoc power analysis showed that our study had 77% power to detect a clinically meaningful decrease of 35% in time to delivery. The mean maternal age was 31.0 (± 3.7) years, and the mean gestational age at initiation of drug therapy was 29.6 (± 3.9) weeks. The maximum infusion rate was 0.10 ± 0.06 mg/min. Multiple gestation pregnancies were observed in 12.1% of the study population. There was no current smoker. Among demographic variables, gestational age (p < 0.001), modified and Bishop score (p = 0.012) were significantly associated with median time to delivery (Table 1).
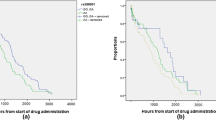
The effects of seven SNPs in the GRK5 gene on ritodrine efficacy were evaluated. All of the allele frequencies were consistent with the Hardy-Weinberg equilibrium. Two polymorphisms (rs1020672 and rs4752292) were in linkage disequilibrium (LD) in our study population (r2 = 0.8). In univariate analysis, rs4752292 (T > G) and rs1020672 (C > T) were significantly associated with time to delivery. Homozygous variant carriers of rs4752292 and rs1020672 had a longer median time to delivery than those with the other genotypes (Table 1, Fig. 1).
For multivariate analysis, two models were constructed using factors with P < 0.1 from the results of univariate analysis in addition to age, because rs1020672 and rs4752292 were in LD. The SNP rs4752292 was used in Model I and the SNP rs1020672 in Model II. The models revealed that homozygous variant carriers of rs4752292 and rs1020672 had 0.6 times the hazard of delivery compared to wild-type allele carriers (95% confidence interval [CI], 0.41~0.99 and 0.38~0.99, respectively). In addition, women at a gestational age ≥28 weeks and modified Bishop score ≥2 had 6.8~8.9 and 1.8~1.9 times the hazard of delivery, respectively, compared to the other women in the study (Table 2).
In terms of the proportion of women who remained undelivered at 24 h and/or at seven days after start of ritodrine therapy, a statistically significant difference was present in rs4752292 carriers at seven days and in rs1020672 carriers at 24 h and at seven days. Carriers of the GG genotype of rs4752292 had an approximately 20.6% greater proportion who remained undelivered at seven days compared to wild-type allele carriers (p = 0.002). On the other hand, carriers of the homozygous variant TT of rs1020672 were 100% undelivered at 24 h and 14.5% greater proportion who remained undelivered at seven days compared to wild-type allele carriers (Table 3).
In univariate analysis of ritodrine-induced ADEs, weight (p = 0.009), height (p = 0.002), and body surface area (BSA) (p = 0.003) were significant factors associated with incidence of ADEs (Table 4). Women who experienced ADEs had lower weight and height than those without ADEs. Further, the maximum ritodrine infusion rate was a marginally significant factor for ADEs. Among the SNPs studied, rs4752292 was the only significantly associated variant and marginal significance was observed in case of rs1020672.
Multivariate logistic regression was performed using factors with P < 0.1 from the results of univariate analysis in addition to age. As height, weight and BSA were related to each other, multivariate logistic regression was performed only with weight, which could represent the remaining variables, to consider multicollinearity in the analysis. Similar to the multivariate analysis of time to delivery, two models were constructed, because rs1020672 and rs4752292 were in LD. The rs4752292 polymorphism was used in Model I and rs1020672 in Model II. As shown in Table 5, after adjusting for covariates, carriers of the homozygous variant rs4752292 and rs1020672 had 2.35-fold (95% CI, 1.10~4.98) and 2.29-fold (95% CI, 1.04~5.06) higher incidence of ADEs than those with other genotypes. The risk of ADEs increased 1.1-fold per 1 mL/min increase in maximum infusion rate whereas it decreased 0.96-fold per 1 kg increase in body weight. The Hosmer-Lemeshow test revealed good fits of the models (Model I, χ2 = 8.61, P = 0.376; Model II, χ2 = 8.38, P = 0.398). The AUROC values of Model I and Model II were 0.703 (95% CI, 0.605~0.801) and 0.689 (95% CI, 0.589~0.789), respectively (Fig. 2).
Area under receiver operating characteristic curve representing ritodrine-induced adverse drug events. (A) Model I included weight, maximum infusion rate, and rs4752292, and the AUROC value was 0.703 (95% CI, 0.605~0.801). (B) Model II included weight, maximum infusion rate, and rs1020672, and the AUROC value was 0.689 (95% CI, 0.589~0.789).
Analysis of two SNPs (rs4752292 and rs1020672) with Netgene2 and NNSPLICE showed a significant association with ritodrine efficacy and ADEs, and did not show the presence of an altered splicing donor or acceptor. However, the results generated by HSF 3.1 indicated that rs4752292 disrupted two RESCUE-ESE hexamers (AGACAT and CATCAG) and two exon-identity elements (EIEs) hexamers (ACATCA and TCAGAT) (Supplementary Table 1). It also led to the formation of SRp40, SF2/ASF (IgM-BRCA1), and SF2/ASF enhancing motifs (AGACAGC, CAGCAGA, and CAGCAGA); the scores were 83.71 (threshold: 78.08), 77.00 (threshold: 70.51), and 78.10 (threshold: 72.98), respectively. The analysis by ESEfinder 3.0, with a different scoring Falgorithm from that of HSF 3.1, also showed that this mutation increased the score of SRp40 binding from 1.588 to 3.611 (threshold: 2.67), SF2/ASF (IgM-BRCA1) binding from 1.012 to 2.670 (threshold; 1.867), and SF2/ASF binding from 0.762 to 2.826 (threshold: 1.956), creating new enhancer motifs. According to the results of HSF 3.1, rs1020672 was predicted to break two Sironi’s Motif 3 and create four intron-identity elements (IIEs) hexamers (CCTCTT, CTCTTT. CTTTTC, and TTTTCA).
Discussion
The present study is the first to suggest that GRK5 variations are correlated with beta agonist efficacy and risk of ADEs in women undergoing preterm labor, the key finding being that homozygous variant carriers of the GRK5 polymorphisms rs4752292 and rs1020672 showed 0.6 times the hazard of delivery compared to wild-type carriers. The proportion of women who remained undelivered at seven days after initiation of ritodrine therapy was significantly higher in homozygous variant carriers of rs4752292 and rs1020672 than in wild-type allele carriers. All women with the homozygous variant TT of rs1020672 remained undelivered at 24 h. Furthermore, those with variant-type homozygous genotypes in the two SNPs above showing higher ritodrine efficacy experienced 2.3~2.4-fold increased ADEs than others.
In the rat and human myometrium, activation of the beta adrenergic receptor/adenyl cyclase pathway via catecholamines significantly induces myorelaxation during pregnancy. At the end of pregnancy, the beta adrenergic receptor/adenyl cyclase pathway is desensitized, contributing to contraction initiation at parturition2,24,25. Receptor desensitization has been reported to rely on alterations in beta adrenergic receptor coupling rather than in receptor expression24. An animal study showed that the abrupt decrease in adenyl cyclase response to beta agonist stimulation occurring just prior to parturition was caused by concomitant beta adrenergic receptor-Gs protein uncoupling, and increased myometrial GRK activity26. These results supported the notion that GRK may function as a physiological regulator of myometrial beta adrenergic receptor activity. Within the GRK family, GRK5 is abundantly expressed in the myometrium. A study with GRK-specific monoclonal antibodies showed that, among several subtypes of GRK, GRK5 and/or GRK6 mediated β-adrenergic desensitization27. Because of the high basal phosphorylation and autophosphorylation activity of GRK5, it was thought to desensitize the β-adrenergic receptors even without hormonal activation, which importantly involved in maintaining uterine quiescence28. Thus, polymorphisms in GRK5 may have a crucial role in beta agonist response.
In human studies, polymorphisms in GRK have been studied extensively in terms of cardiovascular diseases. GRK5 polymorphisms have shown a significant association with atrial fibrillations and heart failure. The SNP rs4752292, a significant factor identified in our study, has been suggested to be correlated with the risk of postoperative atrial fibrillation29. Kertai et al. confirmed that this GRK5 variation had a strong association with postoperative atrial fibrillation despite using beta blockers in patients undergoing coronary artery bypass graft surgery30. Although rs1020672 has not been previously studied, our results show that this SNP is in LD with rs4752292 and that it has a significant association with ritodrine efficacy.
The SNPs of rs4752292 and rs1020672 are located in intronic regions, which are not thought to be involved in the production of proteins. However, intronic regions may potentially influence mRNA splicing, gene expression, or protein activity; thus, analyzing these regions may be useful31,32. To evaluate the spicing effects of these two SNPs, we employed various computational tools and found that both SNPs were predicted to affect the splicing of the GRK5 gene. Therefore, rs4752292 and rs1020672 may be candidate SNPs that affect ritodrine efficacy and ADEs.
A functional SNP (rs2230345, Gln41Leu) in the GRK5 gene was reported to blunt the effects of catecholamines via enhanced beta receptor desensitization in vitro and in clinical settings10,12,33. A study showed that the polymorphism exhibited improved survival in patients with heart failure taking beta blockers33. Another study on airway smooth muscle, in which GRK5 is highly expressed, revealed that the variant allele of rs2230345 induced increased agonist-promoted desensitization of adenylyl cyclase compared with the wild allele. Hence, it was thought that the Leu41 variant could increase kinase function, which results in loss-of-function in the beta 2 adrenergic signaling pathway, thereby decreasing bronchodilatory effects by beta agonist therapy34. Unfortunately, the variant allele of rs2230345 was rarely found in our study population, although it is known to be prevalent in African Americans.
As the secondary endpoint, we analyzed the association between GRK5 polymorphisms and ADE induced by ritodrine. Similar to their effects on efficacy, the SNPs rs4752292 and rs1020672 were found to be significant factors after adjusting for variables. The result showed that women with homozygous variants of either SNP had 2.3~2.4-fold higher risk of ritodrine-induced ADEs. This suggests that the polymorphisms rs4752292 and rs1020672 may alter desensitization of GPCRs and affect both ritodrine efficacy and ADEs.
Among demographic factors, gestational age and modified Bishop score were significant factors for time to delivery, while weight and maximum ritodrine infusion rate influenced on ritodrine-induced ADEs. However, we could not find the impacts of ex-smoking, due to the lack of information on smoking history. Although the significance of these demographic factors may be expected, more specific studies to understand the mechanisms leading to differences in responses to beta agonists are required.
Based on our results, two SNPs of GRK5 (rs4752292 and rs1020672) showed associations with both efficacy and ADRs of ritodrine. They could be good candidates for discriminating the patients who sufficiently responded to ritodrine or who are particularly vulnerable to ADRs. Additionally, our results can be extended to a study of pharmacogenomic association between GRK5 and β-agonist bronchodilators for treatment of asthma or chronic obstructive pulmonary disease.
Conclusions
The present pharmacogenomics study suggests that genetic polymorphisms in GRK5 affect individual susceptibility to beta 2 adrenergic receptor-targeted therapy in women undergoing preterm labor. Because ethnical diversity of study population was not acquired, further studies including other populations are recommended.
References
WHO. recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta. Obstet. Gynecol. Scand. 56, 247–253 (1977).
Salomonis, N. et al. Identifying genetic networks underlying myometrial transition to labor. Genome Biol. 6, R12 (2005).
Higby, K., Xenakis, E. M. & Pauerstein, C. J. Do tocolytic agents stop preterm labor? A critical and comprehensive review of efficacy and safety. Am. J. Obstet. Gynecol. 168, 1247–56 (1993).
Neilson, J. P., West, H. M. & Dowswell, T. Betamimetics for inhibiting preterm labour. Cochrane Database Syst. Rev. 2, CD004352 (2014).
Scheid, C. R., Honeyman, T. W. & Fay, F. S. Mechanism of beta-adrenergic relaxation of smooth muscle. Nature. 277, 32–36 (1979).
Park, J. Y. et al. Effects of beta2-adrenergic receptor gene polymorphisms on ritodrine therapy in pregnant women with preterm labor: prospective follow-up study. Int. J. Mol. Sci. 15, 12885–12894 (2014).
Freedman, N. J. & Lefkowitz, R. J. Desensitization of G protein-coupled receptors. Recent Prog. Horm. Res. 51, 319–351 (1996).
Pitcher, J. A., Freedman, N. J. & Lefkowitz, R. J. G protein-coupled receptor kinases. Annu. Rev. Biochem. 67, 653–692 (1998).
Willets, J. M., Challiss, R. A. & Nahorski, S. R. Non-visual GRKs: are we seeing the whole picture? Trends Pharmacol. Sci. 24, 626–633 (2003).
Liggett, S. B. et al. A GRK5 polymorphism that inhibits beta-adrenergic receptor signaling is protective in heart failure. Nat. Med. 14, 510–517 (2008).
Garcia-Gorostiaga, I. et al. Genetic variation in alpha-synuclein kinases (CK-2beta and GRK-5) and risk of Parkinson’s disease. Parkinsonism Relat. Disord. 17, 496–497 (2011).
Lobmeyer, M. T. et al. Polymorphisms in genes coding for GRK2 and GRK5 and response differences in antihypertensive-treated patients. Pharmacogenet. Genomics. 21, 42–49 (2011).
Ji, Y. et al. Pharmacogenomics of selective serotonin reuptake inhibitor treatment for major depressive disorder: genome-wide associations and functional genomics. Pharmacogenomics J. 13, 456–463 (2013).
Li, H. et al. A genome-wide association study identifies GRK5 and RASGRP1 as type 2 diabetes loci in Chinese Hans. Diabetes. 62, 291–298 (2013).
Kunapuli, P. & Benovic, J. L. Cloning and expression of GRK5: A member of the G proteincoupled receptor kinase family. Proc. Natl. Acad. Sci. 90, 5588–5592 (1993).
Sato, P. Y., Chuprun, J. K., Schwartz, M. & Koch, W. J. The evolving impact of g protein-coupled receptor kinases in cardiac health and disease. Physiol. Rev. 95, 377–404 (2015).
Park, J. Y. et al. Effects of β2-adrenergic receptor gene polymorphisms on ritodrine therapy in pregnant women with preterm labor: prospective follow-up study. Int. J. Mol. Sci. 15, 12885–12894 (2014).
Gabriel, S. B. et al. The structure of haplotype blocks in the human genome. Science 296, 2225–2229 (2002).
Rozenberg, P., Rudant, J., Chevret, S., Boulogne, A. I. & Ville, Y. Repeat measurement of cervical length after successful tocolysis. Obstet. Gynecol. 104, 995–999 (2004).
Brunak, S., Engelbrecht, J. & Knudsen, S. Prediction of human mRNA donor and acceptor sites from the DNA sequence. J. Mol. Biol. 220, 49–65 (1991).
Reese, M. G., Eeckman, F. H., Kulp, D. & Haussler, D. Improved splice site detection in Genie. J. Comput. Biol. 4, 311–323 (1997).
Cartegni, L., Wang, J., Zhu, Z., Zhang, M. Q. & Krainer, A. R. ESEfinder: A web resource to identify exonic splicing enhancers. Nucleic Acids Res. 31, 3568–3571 (2003).
Desmet, F. O. et al. Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 37, e67 (2009).
Cohen-Tannoudji, J., Vivat, V., Heilmann, J., Legrand, C. & Maltier, J. P. Regulation by progesterone of the high-affinity state of myometrial beta adrenergic receptor and of adenylate cyclase activity in the pregnant rat. J. Mol. Endocrinol. 6, 137–145 (1991).
Litime, M. H., Pointis, G., Breuiller, M., Cabrol, D. & Ferre, F. Disappearance of beta-adrenergic response of human myometrial adenylate cyclase at the end of pregnancy. J Clin. Endocrinol. Metab. 69, 1–6 (1989).
Ferguson, S. S. & Caron, M. G. G protein-coupled receptor adaptation mechanisms. Semin Cell Dev. Biol. 9, 119–127 (1998).
Simon, V., Robin, M. T., Legrand, C. & Cohen-Tannoudji, J. Endogenous G protein-coupled receptor kinase 6 triggers homologous beta-adrenergic receptor desensitization in primary uterine smooth muscle cells. Endocrinology. 144, 3058–3066 (2003).
Brenninkmeijer, C. B., Price, S. A., López Bernal, A. & Phaneuf, S. Expression of G-protein-coupled receptor kinases in pregnant term and non-pregnant human myometrium. J. Endocrinol. 162, 401–408 (1999).
Liu, L. et al. GRK5 polymorphisms and postoperative atrial fibrillation following coronary artery bypass graft surgery. Sci. Rep. 5, 12768 (2015).
Kertai, M. D. et al. G protein-coupled receptor kinase 5 gene polymorphisms are associated with postoperative atrial fibrillation after coronary artery bypass grafting in patients receiving beta-blockers. Circ. Cardiovasc. Genet. 7, 625–633 (2014).
Raponi, M. & Baralle, D. Alternative splicing: good and bad effects of translationally silent substitutions. FEBS J. 277, 836–840 (2010).
Pagani, F. & Baralle, F. E. Genomic variants in exons and introns: identifying the splicing spoilers. Nat. Rev. Genet. 5, 389–396 (2004).
Cresci, S. et al. Adrenergic-pathway gene variants influence beta-blocker-related outcomes after acute coronary syndrome in a race-specific manner. J. Am. Coll. Cardiol. 60, 898–907 (2012).
Wang, W. C., Mihlbachler, K. A., Bleecker, E. R., Weiss, S. T. & Liggett, S. B. A polymorphism of G-protein coupled receptor kinase5 alters agonist-promoted desensitization of beta2-adrenergic receptors. Pharmacogenet. Genomics. 18, 729–732 (2008).
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant (No. NRF-2010-0022544) funded by the Korea Government (MEST), the Korea Health Industry Development Institute (KHIDI) (No. HI14C0306) funded by the Ministry of Health and Welfare, Republic of Korea, and the Research Program (No. HI18C0378) funded by the Ministry of Health and Welfare, Republic of Korea.
Author information
Authors and Affiliations
Contributions
J.E.C., H.S.H., Y.J.K. and H.S.G. participated in research design. J.E.C., J.Y., J.Y.P., Y.J.K. and K.E.L. conducted experiments. J.E.C., J.Y., J.Y.P. and H.S.G. performed data analysis. J.E.C., J.Y., H.S.H. and K.E.L. drafted a manuscript and Y.J.K. and H.S.G. finalized the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, J.E., Yee, J., Hwang, H.S. et al. Influence of GRK5 gene polymorphisms on ritodrine efficacy and adverse drug events in preterm labor treatment. Sci Rep 10, 1351 (2020). https://doi.org/10.1038/s41598-020-58348-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-58348-1
- Springer Nature Limited