Abstract
Immune control point (ICI) inhibitors represent a significant advance in the management and survival of cancers such as melanoma or non-small cell bronchial carcinoma. However, they induce unusual side effects, such as hypophysitis, which are rarely described elsewhere. This nationwide retrospective study describes the characteristics of hypophysitis reported in the French pharmacovigilance database (FPVD). We requested for all cases of ICI-related hypophysitis registered in the FPVD before May 2018. An endocrinologist and a pharmacologist reviewed all cases. About 94 pituitary cases were selected, involving 49 females and 45 men. Ipilimumab alone or in combination was the most represented ICI (56%). Most cases (61%) were grade 3 severity and the majority (90%) were corticotropic deficiency cases. Cases with thyroid and/or gonadotropic involvement were 21% and 1% respectively. Five patients (8%) had panhypopituitarism. Pituitary MRI, when performed, was in favor of hypophysitis in 50%. No patient recovered his previous hormonal function. The mean time of onset was significantly shorter with ipilimumab than other ICIs. ICI-related hypophysitis generate deficits that do not spontaneously recover, even at a distance from the event, unlike thyroiditis. Patients must then benefit from long-term coordinated onco-endocrinological management, adapted to their own specific deficits.
Similar content being viewed by others
Introduction
Recently, immune checkpoint inhibitors (ICIs) have become the preferred treatment for many advanced solid tumours such as melanoma, non-small-cell lung cancer (NSCLC), and clear cell renal cancer1. Ipilimumab was the first authorized ICI, acting via cytotoxic T-lymphocyte antigen-4 (CTLA-4) blockade, followed by nivolumab and pembrolizumab, which both target the programmed death 1 receptor (PD-1), an effector ligand of the immune checkpoint pathway. More recently two other ICIs, atezolizumab and avelumab, which both target the PD1 ligand (PD-L1) have also been authorized for treating such diseases.
The mechanism of action of ICIs is to utilize the patient’s own immune system to destroy tumour cells or inhibit tumour growth, by restoring the decreased cellular immunity as well as boosting the production and proliferation of T lymphocytes. This ingenious mechanism of action has been shown to be efficient in terms of survival and disease-free survival but is jeopardized by the development of numerous and various immune related adverse effects (IRAEs), including endocrinological disorders as well as dermatological, digestive, cardiac, pulmonary, muscular, and haematological disorders, with all organs being potentially affected. Among the endocrinological damages, thyroiditis and hypophysitis seem to be the most common2,3,4,5,6,7. Unlike thyroiditis, hypophysitis does not commonly affect people and has dramatically emerged since the launch of ICI therapies8,9,10,11,12.
In order to achieve real-life data about the characteristics, diagnosis and management of this adverse effect related to the use of the most commonly used ICIs (ipilimumab, nivolumab and pembrolizumab), we performed a retrospective and descriptive analysis of cases of hypophysitis reported inadverse dru reaction the French network of regional pharmacovigilance centres since the marketing of these drugs.
Materials and Methods
Data collection
The data source used was the French Pharmacovigilance Database (FPVD)13. Briefly, the French Pharmacovigilance database was created in 1973 and, since 1985, all spontaneous reports of ADR have been recorded in the FPVD. According to French law, every health professional must report “serious” and/or “unexpected” adverse drug reactions to their regional centres of pharmacovigilance (31 in France). For each ADR report, information about the patient (age, sex, medical history), drug exposure (to the suspected drug and other associated non-suspected drugs) and ADR characteristics (“serious” or “non-serious”, “expected” or “unexpected”, causality score, outcomes) are recorded in the FPVD.
The FPVD was searched in April 2018 for all cases of endocrinological disorders (MedDRA system organ class (SOC) « endocrine disorders ») and hormonal biological abnormalities (within MedDRA SOC « investigations ») involving ipilimumab, nivolumab and/or pembrolizumab. No cases involving atezolizumab or avelumab were recorded. All anonymized recorded cases in the FPVD (General Data Protection Regulation Law) were reviewed by an endocrinologist and a pharmacologist to select confirmed hypophysitis cases and discard those with any aetiology other than iatrogenic. The French Pharmacovigilance Database was approved by the French Data Protection Agency (CNIL). No additional approval was required for studies based on this database, because all records respect the patient’s and notifier’s anonymity. We also attest that all our data originated from this database. Thus, this observational study did not require patient consent or ethics committee approval. Additionally, we certify that this study was approved by the French network of Regional Pharmacovigilance Centres.
Case selection
Hypophysitis patients had to display (i) clinical symptoms such as cephalalgia associated with blurred vision, nausea or vomiting or clinical signs of anterior pituitary failure; and/or (ii) biological results consistent with a trophic hormone deficiency: prolactin (PRL), growth hormone (GH), adrenocorticotropic hormone (ACTH), thyroid-stimulating hormone (TSH), luteinizing hormone (LH) and/or follicle-stimulating hormone (FSH) in females, and testosterone in males; and/or (iii) abnormal MRI consistent with hypophysitis. Suspected cases of peripheral adrenal insufficiency without fludrocortisone supplementation were considered as adrenocorticotropic insufficiency secondary to hypophysitis6.
Variables
We collected the characteristics of the patients (sex, age, previous immune disorder), suspected treatment (drug(s), dose, number of injections), hypophysitis (clinical symptoms, biological abnormalities, imaging, time to onset after start of ICI, outcomes), and patient’s medication (type of hormonal supplementation, weaning). The severity of hypophysitis was graded according to the CTCAE-NCI v4.0 (grade 1: asymptomatic patients, no treatment required; grade 2: symptoms not requiring hospitalization; grade 3: functional impairment limiting activities of daily living and requiring hospitalization; grade 4: life-threatening symptoms; and grade 5: death).
Statistical analysis
The mean, standard deviation and median with minimal and maximal values were used to express quantitative variables, while qualitative variables were expressed with numbers and rates. The comparison of the averages was based on the ANOVA test together with Student’s t test when relevant. SAS software version 9·3 (SAS Institute, Cary, NY) was used to draw the analysis.
Results
Among the 249 cases corresponding to an endocrinological disorder associated with ipilimumab, nivolumab or pembrolizumab, 94 corresponded to hypophysitis (Table 1). Among these latter cases, ipilimumab was the most-involved ICI, either alone (43%) or in combination with nivolumab (14%). Four patients received previous ICI treatment before the diagnosis (6·6%). The patients included 49 females and 45 males, whose mean age was 64·5 years (+/−14·1), and the most frequent indication was melanoma (74·5%). None of these patients displayed a previous immune disorder.
Most of them (88%) expressed clinical symptoms, mainly fatigue and cephalalgia, justifying biological and morphological explorations and finally leading to the diagnosis of hypophysitis. Hyponatremia and arterial hypotension were exceptionally present. Five patients had pan-hypopituitarism. No patient had insipidus diabetes. Pituitary MRI results were available in 40 patients and only half of them demonstrated a hypophysitis aspect, whereas one patient had a pituitary micro-adenoma, another patient had an empty sella turcica, and the remaining patients had normal pituitary imaging. The only two patients with documented abnormal pituitary MRI recovered after hydrocortisone supplementation.
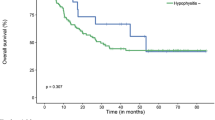
The median delay period for hypophysitis to develop, after the start of ICI treatment, was significantly shorter with ipilimumab alone or combined with nivolumab (83 days; min 14 - max 506) than with nivolumab or pembrolizumab alone (165 days; min 5 - max 686; p = 0·0001) (Table 1). The median number of cycles and the median cumulated dose before hypophysitis were not significantly higher for nivolumab than for the other drugs.
No cases corresponded to grade 1 hypophysitis. Three patients treated with ipilimumab with severe general state deterioration had rapid (24 to 48 hours) fatal outcome after hypophysitis diagnosis, which could eventually be considered as grade 5 hypophysitis, but without enough evidence to exclude disease progression fatality. One patient had concomitant myasthenia and died from respiratory failure. The second patient died from acute liver cytolysis and shock after decompensated adrenocorticotropic failure and the third died from melanoma progression. Nivolumab was also associated with severe (grade 4) hypophysitis in 2 patients of whom one finally died due to lung cancer progression. Patients treated with pembrolizumab had less severe disorders (grade 3 or 2), but one patient had fatal outcomes due to melanoma progression.
Hydrocortisone supplementation was provided to 85 patients (90·4%) and L-thyroxin supplementation to 20 patients (21.3%). Only one case of testosterone supplementation was started concomitantly with hydrocortisone for a man with panhypopituitarism, while in the other cases of panhypopituitarism, 3 women received hydrocortisone plus levothyroxine supplementation, and 1 man received hydrocortisone only. No patient was weaned from hormonal supplementation according to the last available information, except one male patient who had received short-term hydrocortisone treatment and thereafter displayed a normal ACTH stimulation test. The only patient who received no supplementation had her ICI treatment discontinued.
Discussion
To the best of our knowledge, this series of 94 patients with ICI-induced hypophysitis is, as of today, the largest reported series. It provides complementary insights into the previously available data3,4,11,14 and case-series8,10,15, and, especially, reinforces clinical trial data16 by including patients with a potential previous ICI exposure or autoimmune history. In fact, no patient in our series had previous immune disease recorded in his or her medical file, which leads us to confirm, similarto the cas in other IRAEs, that the development of hypophysitis is not triggered by a pre-existing immune condition.
Hypophysitis was initially considered a specific IRAE of ipilimumab considering the presence of pituitary expression of CTLA-4 antigens17. Our series, with 41 cases (28 related to nivolumab and 13 to pembrolizumab), confirms previous literature reports showing that hypophysitis can also occur while anti PD-114 and anti-PD-L1 are present18. It is, however, interesting to note that we observed a significantly shorter delay of onset with ipilimumab than with anti-PD1. Our results and literature data definitely illustrate that hypophysitis can occur regardless of the ICI target (CTLA4, PD1 or PD-L1) and its indication.
In accordance with literature stating that thyroid hormone deficiency appears to be less frequently reported than adrenocorticotropic or gonadotropic deficiencies, our series includes a larger proportion of patients requiring hydrocortisone supplementation than thyroidal supplementation. Clinical signs of adrenocorticotropic failure may be less often detected and underestimated for patients with advanced cancer with marked asthenia, nausea and vomiting. We observed that pituitary MRI contributed less to the findings of our cases than in the cases-series reported in the literature. Faje et al.9 reported that 100% of patients had abnormal MRI, but abnormalities were previously observed in 7/18 patients before symptoms occurred.
Hormonal supplementation weaning appears difficult to achieve, especially for hydrocortisone19 and this was confirmed in our series. However, we are also aware that weaning success assessments may be lowered by too short of a follow-up in prospective studies or a lack of information in retrospective studies; this phenomenon is one of the limitation of our study, with very few patients benefiting from a sufficient retrospective update.
Panhypopituitarism, although rare, should not be ignored. We observed that supplementation with gonadotropic hormones was rarely performed and we propose that it should be more often considered, especially in non-menopausal women to limit the consequences of oestrogens deficiency, such as osteoporosis. Considering the variable delay of hypophysitis development and the therapeutic regimens with ICI administrations every 2 or 3 weeks, the results of the clinical survey regarding hypophysitis appear to be helpful at any time of treatment, regardless of the ICI type. Delayed signs after treatment cessation can also occur20 and, therefore, hypophysitis should be kept in mind for any patient with present or past ICI exposure(s).
The main limitation of our work is the very probable underreporting of ICI-induced hypophysitis because these cases are now expected, especially non-severe cases (grades 1 and 2). This limitation persists despite the fact that since 2011, French health professionals have an obligation to report any suspected drug-induced adverse reaction, regardless of its expectedness or seriousness. Another main limitation is related to the retrospective collection of data, generating missing information, and thus potential uncertainties. However, the practitioners’ expertise in regional pharmacovigilance centres and the specific review of all cases by an endocrinologist warrant the accuracy of a diagnosis of hypophysitis and a good assessment of patients’ clinical histories and condition, but it must be acknowledged that, when detailed ACTH levels or stimulation tests to confirm primary versus secondary adrenal insufficiency were not available (10 cases), reliance on imperfect secondary markers was made. Therefore, it is possible that some misclassification occurred.
Conclusion
Hypophysitis is definitely not a specific IRAE of ipilimumab treatment for melanoma. It occurs with any type of currently available ICI, anti-CTLA4, anti-PD1 or anti PD-L1, at any time of treatment and regardless of the type of cancer. Adrenocorticotropic deficiency may be more frequent than thyroidal deficiency and hormonal supplementation is required and has been proven to be difficult, if not impossible, to wean. Gonadotropic hormonal supplementation should probably be more often considered. The management of patients clearly requires long-term onco-endocrinological care.
Data availability
Restrictions apply to the availability of data generated or analyzed during this study because they were used under the authority of the French Drug Agency (ANSM). The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.
References
Gonzalez-Rodriguez, E. & Rodriguez-Abreu, D. Spanish Group for Cancer, I.-B.: Immune Checkpoint Inhibitors: Review and Management of Endocrine Adverse Events. Oncologist 21(7), 804–816, https://doi.org/10.1634/theoncologist.2015-0509 (2016).
Iglesias, P. Cancer immunotherapy-induced endocrinopathies: Clinical behavior and therapeutic approach. Eur J Intern Med 47, 6–13, https://doi.org/10.1016/j.ejim.2017.08.019 (2018).
Barroso-Sousa, R. et al. Endocrine dysfunction induced by immune checkpoint inhibitors: Practical recommendations for diagnosis and clinical management. Cancer 124(6), 1111–1121, https://doi.org/10.1002/cncr.31200 (2018).
Joshi, M. N., Whitelaw, B. C., Palomar, M. T., Wu, Y. & Carroll, P. V. Immune checkpoint inhibitor-related hypophysitis and endocrine dysfunction: clinical review. Clin Endocrinol (Oxf) 85(3), 331–339, https://doi.org/10.1111/cen.13063 (2016).
Michot, J. M. et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer 54, 139–148, https://doi.org/10.1016/j.ejca.2015.11.016 (2016).
Barroso-Sousa, R. et al. Incidence of Endocrine Dysfunction Following the Use of Different Immune Checkpoint Inhibitor Regimens: A Systematic Review and Meta-analysis. JAMA. Oncol 4(2), 173–182, https://doi.org/10.1001/jamaoncol.2017.3064 (2018).
Illouz, F. et al. Endocrine toxicity of immune checkpoint inhibitors: essential crosstalk between endocrinologists and oncologists. Cancer Med 6(8), 1923–1929, https://doi.org/10.1002/cam4.1145 (2017).
Lammert, A. et al. Hypophysitis caused by ipilimumab in cancer patients: hormone replacement or immunosuppressive therapy. Exp Clin Endocrinol Diabetes 121(10), 581–587, https://doi.org/10.1055/s-0033-1355337 (2013).
Faje, A. Hypophysitis: Evaluation and Management. Clin Diabetes Endocrinol 2, 15, https://doi.org/10.1186/s40842-016-0034-8 (2016).
Carpenter, K. J., Murtagh, R. D., Lilienfeld, H., Weber, J. & Murtagh, F. R. Ipilimumab-induced hypophysitis: MR imaging findings. AJNR Am J Neuroradiol 30(9), 1751–1753, https://doi.org/10.3174/ajnr.A1623 (2009).
Brilli, L. et al. Prevalence of hypophysitis in a cohort of patients with metastatic melanoma and prostate cancer treated with ipilimumab. Endocrine 58(3), 535–541, https://doi.org/10.1007/s12020-017-1289-2 (2017).
Bellastella, G. et al. Revisitation of autoimmune hypophysitis: knowledge and uncertainties on pathophysiological and clinical aspects. Pituitary 19(6), 625–642, https://doi.org/10.1007/s11102-016-0736-z (2016).
Vial, T. French pharmacovigilance: Missions, organization and perspectives. Therapie 71(2), 143–150, https://doi.org/10.1016/j.therap.2016.02.029 (2016).
Baxi, S. et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: systematic review and meta-analysis. BMJ 360, k793, https://doi.org/10.1136/bmj.k793 (2018).
Lupu, J. et al. Transient pituitary ACTH-dependent Cushing syndrome caused by an immune checkpoint inhibitor combination. Melanoma Res 27(6), 649–652, https://doi.org/10.1097/CMR.0000000000000405 (2017).
Torino, F., Corsello, S. M. & Salvatori, R. Endocrinological side-effects of immune checkpoint inhibitors. Curr Opin Oncol 28(4), 278–287, https://doi.org/10.1097/CCO.0000000000000293 (2016).
Iwama, S. et al. Pituitary expression of CTLA-4 mediates hypophysitis secondary to administration of CTLA-4 blocking antibody. Sci Transl Med 6(230), 230ra245, https://doi.org/10.1126/scitranslmed.3008002 (2014).
Kanie, K. et al. Two Cases of Atezolizumab-Induced Hypophysitis. J Endocr Soc 2(1), 91–95, https://doi.org/10.1210/js.2017-00414 (2018).
Park, S. M. et al. Clinical characteristics, management, and outcome of 22 cases of primary hypophysitis. Endocrinol Metab (Seoul) 29(4), 470–478, https://doi.org/10.3803/EnM.2014.29.4.470 (2014).
Joshi, M. N., Whitelaw, B. C. & Carroll, P. V. Mechanisms in Endocrinology: Hypophysitis: diagnosis and treatment. Eur J Endocrinol 179(3), R151–R163, https://doi.org/10.1530/EJE-17-0009 (2018).
Author information
Authors and Affiliations
Contributions
J.G.C., N.P. and P.G. conceived the study. J.G.C., N.P., F.R., M.S., S.B., M.Y.O. and P.G. did the literature search. J.G.C., N.P. and M.Y.O. analyzed the data. F.R., M.S., S.B., M.Y.O., G.W. and M.K. contributed to study protocol. J.G.C., N.P., G.W., M.K. and P.G. contributed to key data interpretation. JGC, NP, MYO, and PG wrote the manuscript. F.R., M.S., S.B., G.W. and M.K. critically revised the manuscript. All contributors approved the final accepted version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.G.C., N.P., F.R., M.S., S.B., M.Y.O., M.K. and P.G. declare no financial competing interests. GW consulted for Novartis and Theramex and received punctual compensations. Nadine PETITPAIN: unpaid membership as expert of the French Drug Agency (ANSM), Unpaid member of the coordination committee of an academic interventional clinical trial (NCT02250729) funded by a consortium of 15 companies marketing pholcodine containing drugs (Bouchara-Recordati, Hepatoum, Biocodex/Leurquin, Pierre Fabre, Sanofi, Urgo, Zambon, Alliance, Bells healthcare, Boots, Ernest Jackson, GSK, Medgenix, Pinewood, Vemedia). Franck ROUBY: unpaid membership as expert of the French Drug Agency (ANSM), unpaid expert (Co-investigator) for clinical Trials (Biogen, Theranexus, Inflectis Bioscience, Roche Genentech, Abbvie, Roche). Marion SASSIER: unpaid membership as expert of the French Drug Agency (ANSM), Samy BABAI: unpaid membership as expert of the French Drug Agency (ANSM), unpaid expert in a multicentric academic study on tranexamic acid. Mélissa YELEHE-OKOUMA: unpaid membership as expert of the French Drug Agency (ANSM), Pierre GILLET: unpaid membership as expert of the French Drug Agency (ANSM), Unpaid member of the coordination committee of an academic interventional clinical trial (NCT02250729) funded by a consortium of 15 companies marketing pholcodine containing drugs (Bouchara-Recordati, Hepatoum, Biocodex/Leurquin, Pierre Fabre, Sanofi, Urgo, Zambon, Alliance, Bells healthcare, Boots, Ernest Jackson, GSK, Medgenix, Pinewood, Vemedia).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garon-Czmil, J., Petitpain, N., Rouby, F. et al. Immune check point inhibitors-induced hypophysitis: a retrospective analysis of the French Pharmacovigilance database. Sci Rep 9, 19419 (2019). https://doi.org/10.1038/s41598-019-56026-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56026-5
- Springer Nature Limited
This article is cited by
-
Immune Checkpoint Inhibitors and Scleroderma: Data from the European Pharmacovigilance Database
Drugs - Real World Outcomes (2024)
-
Three cases of immune-related hypopituitarism after atezolizumab–bevacizumab treatment for hepatocellular carcinoma
Clinical Journal of Gastroenterology (2023)
-
Tumour microenvironment and pituitary tumour behaviour
Journal of Endocrinological Investigation (2023)
-
Immune-checkpoint inhibitors: long-term implications of toxicity
Nature Reviews Clinical Oncology (2022)
-
Endocrine toxicities of immune checkpoint inhibitors
Nature Reviews Endocrinology (2021)