Abstract
Low back pain patients are sometimes offered fusion surgery if intervertebral translation, measured from static, end of range radiographs exceeds 3 mm. However, it is essential to know the measurement error of such methods, if selection for back surgery is going to be informed by them. Fifty-five healthy male (34) and female (21) pain free participants aged 21–80 years received quantitative fluoroscopic (QF) imaging both actively during standing and passively in the lateral decubitus position. The following five imaging protocols were extracted from 2 motion examinations, which were repeated 6 weeks apart: 1. Static during upright free bending. 2. Maximum during controlled upright bending, 3. At the end of controlled upright bending, 4. Maximum during controlled recumbent bending, 5. At the end of controlled recumbent bending. Intervertebral flexion translations from L2-S1 were determined for each protocol and their measurement errors (intra subject repeatability) calculated. Estimations using static, free bending radiographic images gave measurement errors of up to 4 mm, which was approximately twice that of the QF protocols. Significantly higher ranges at L4-5 and L5-S1 were obtained from the static protocol compared with the QF protocols. Weight bearing ranges at these levels were also significantly higher in males regardless of the protocol. Clinical decisions based on sagittal translations of less than 4 mm would therefore require QF imaging.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Low back pain is responsible for the world’s largest number of days lost to disability1 and although its diagnosis is often problematical, it is agreed that mechanics generally, and segmental stability in particular, plays a significant role2,3,4. However, the measurement of segmental stability in patients is problematical due to lack of a unified concept of the condition. Yet while biomechanical measurements alone are not considered to be good predictors of prognosis, patients with sufficiently severe symptoms may be offered fusion surgery if intervertebral translation exceeds 4 mm5. There are many imaging methods for determining this, but practicality and economics dictates that it is generally performed using standing end-range radiographs6.
For this measurement, a radiograph is taken in the neutral standing position and then with the patient flexing forward as far as possible. This is repeated with the patient bending backwards into extension. On the resulting images lines are drawn on adjacent vertebrae from which to measure the translation or sliding movement between vertebrae. This is generally preferred by clinicians to angular movement for the assessment of stability7. However, it has long been recognised that inaccuracies and population variations using this technique may limit its usefulness and make selection of a cut off for excessive translation difficult8. Static views have also been found to underestimate intervertebral translation compared to dynamic imaging and the lateral decubitus position to better detect excessive motion in spondylolisthesis cases9,10. Furthermore, complexity increases if the patient also has spinal stenosis11 or if revision surgery is being considered12.
Recently, advances in fluoroscopic imaging have made it possible to register and track multi segmental vertebral image sequences throughout the entire motion. This method is called quantitative fluoroscopy (QF) and has been able to identify motion patterns that discriminate patients with chronic, nonspecific back pain from pain free controls13,14,15,16,17. It has also been used to measure positional changes at individual levels, where for translation, it has been reported to have an accuracy of 0.1 mm and inter-observer repeatability of 1.1 mm (agreement) and ICC 0.533–0.988 (reliability)18,19. Given the ubiquity of fluoroscopes in general hospitals, these might be repurposed to provide an alternative method for measuring inter vertebral translation in such patients.
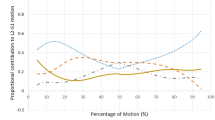
Continuous standardised motion measurement has a number of potential advantages. First, although the motion is not ‘naturally performed’, controlled motion enables standardisation for trunk range, velocity, ramp up and ramp down speeds and is therefore potentially more reproducible. Second, QF can be conducted either actively weight-bearing or passively in recumbence, to avoid muscle contraction, or guarding, and to test the passive structures with minimal uncontrolled movement variation20. Third, the option of a passive recumbent examination has the advantage of additional patient comfort, where upright bending may be inhibited by pain. Fourth, the range of translation may be measured at the end of the maximum range of the segment, which may not coincide with its range at the end of the trunk bending motion (Fig. 1).
As QF allows for a number of protocols for measuring intervertebral translation it was thought useful to assess the measurement properties of these in terms of random and intra subject variability for measuring maximum displacement. In addition, a direct comparison of end range vs through range translation is lacking, as is measurement during free and guided bending21. The main aim of this study was to compare the intra subject variability, or measurement error, of 5 methods for measuring intervertebral flexion translation to determine the level of difference that could be detected by each. The evaluation of extension was not included as the standing range of lumbar spine extension is small (20°)22.
Methods
Participants
Fifty-five healthy control participants were recruited from staff, students and visitors of the AECC University College (Bournemouth, UK). To be eligible, participants had to be aged 21–80 years, BMI < 30, with no history of previous back or abdominal surgery or spondylolisthesis, no medical radiation exposure of >8 mSV in the previous 2 years and no current pregnancy. Participants also had to have been free of any back pain that limited their normal activity for more than 1 day in the previous year. All imaging was carried out in accordance with AECC UC Local Rules and ethical approval was obtained from the National Research Ethics Service (South West 3, 10/H0106/65). Written Informed consent was obtained from all individual participants included in the study. All images of models were submitted with the express permission and signed informed consent of the model for publication of identifying information/images in an online open-access publication.
Data collection
Participants (median age 30 years, range 21 to 69), received fluoroscopic imaging of their lumbar spines during both lying (passive recumbent) and standing (weight-bearing guided) flexion. In passive recumbent flexion. For passive imaging they lay unconstrained in the lateral decubitus position on a motorised table that flexed their upper body to 40° flexion and return during fluoroscopic screening (Atlas Clinical Ltd.) (Fig. 2a). They were then imaged whilst weight-bearing, standing with their right side against the motion frame using the same controller apparatus as for the recumbent procedure (Fig. 2b).
With their pelvises stabilised and during active voluntary motion, participants were guided through a standardised range of 60° standing flexion and return by a moving arm. The motion controllers accelerated at 6°s−2 for the first second followed by a uniform 6°s−1 thereafter. The guiding arm was then removed, and the participants were asked to bend forward freely to the end of their comfortable range (weight-bearing unguided flexion) (Fig. 2c). Single fluoroscopic images were obtained at the beginning and end of the weight-bearing unguided flexion motion. Fluoroscopic motion sequences were recorded at 15 Hz using a Siemens Arcadis Avantic digital C-arm fluoroscope (Siemens GMBH) and stored in DICOM format. They were then exported to a computer workstation and analysed using manual first image registration (Fig. 3) and thereafter using bespoke frame-to-frame tracking using codes written in Matlab (V2011a, The Mathworks Inc). These measurements were repeated 6 weeks later by the same operator using the same equipment at approximately the same time of day for the determination of intra-subject measurement error21.
Image analysis
Sagittal plane translation was calculated using the method of Frobin et al. in vertebral body units (VBU) which were converted to millimetres for presentation by multiplying the result by 35 - the standard chosen for vertebral body depth in millimetres23. In order to address the degree of translation that could be considered excessive, sagittal plane translation of each intervertebral level from L2-S1 was determined and the levels pooled to provide means and upper reference ranges of variation (+1.96 SD) for the following five measurement protocols:
- 1.
Maximum IV translation during passive recumbent flexion
- 2.
IV translation at maximum bend of passive recumbent flexion
- 3.
Maximum IV translation during guided weight-bearing flexion
- 4.
IV translation at maximum bend of guided weight-bearing flexion
- 5.
IV translation at maximum bend of unguided weight-bearing flexion (reflective of traditional static radiograph acquisition)
Statistical analysis
All data were tested for normality using the Shapiro-Wilk test. The significance of differences was calculated using 2-way paired t-tests for normally distributed data and the Wilcoxon test for non-normal data. Repeatability was calculated using the following formula, where Sw is the within-subject standard deviation. The repeatability coefficient, or measurement error, estimates the magnitude of the within-subject change that can be expected 95% of the time and represents the Minimum Detectable Change (MDC95)21. Source data for this study] are available by application to the corresponding author.
The association between test-retest differences and their means were assessed using Kendall’s tau. As no significant and/or substantial associations were found, the data were not transformed for the calculation of MDC95.
Results
Fifty-five participants (21F, 34M) were recruited and all provided complete data. These data were mainly distributed non-normally, resulting in a nonparametric approach to statistical comparisons. Participants’ characteristics were: height 1.75 m (range 1.53–1.90), weight 74.9 kg (range 47.6–112.4) and BMI 24.2 (range 16.9–31.8). The median effective dose received per participant was 0.27 mSv for weight bearing motion (range 0.20–0.68), 0.18 mSv for recumbent motion (range 0.11–0.31) and 0.04 mSv for single frame maximum bend images (range 0.01–0.09).
The median translations for pooled L2-S1 levels were less than 2 mm regardless of protocol while the static uncontrolled protocol gave significantly higher translation ranges than any of the controlled protocols (p < 0.001, (Wilcoxon) (Table 1). Intra class correlations were moderate to substantial, showing acceptable reliability for all protocols, however, the measurement error was highest (3.36 mm) for the static uncontrolled protocol, compared with the highest error of the controlled protocols (2.14 mm). This reflects an error in excess of 200% of the baseline translation for the static protocol compared with a maximum of 163% for controlled weight bearing. Weight bearing measurements, both guided and unguided, gave slightly higher ranges than passive recumbent testing, but similar values when measured at the end of the motion and during it.
When taken level by level, the median baseline translation of L2-3 was significantly greater during guided weight bearing continuous measurement than unguided weight bearing static measurement (p < 0.001), whereas the converse was true for L4-5 and L5-S1 (p < 0.001) (Wilcoxon) (Fig. 4).
The measurement errors at L4-5 and L5-S1 for static uncontrolled measurements at around 4 mm were approximately double those of controlled ones (around 2 mm), however, for L2-3 and L3-4 these differences were less marked (Fig. 5).
The baseline median translation range at L5-S1, when measured using the static, uncontrolled maximum bend protocol, was significantly higher for males than for females (P < 0.001) (Mann Whitney). In addition, for the weight bearing controlled bending protocols, L3-4 and L4-5 ranges were higher for males (p < 0.01), while recumbent sequences measured during the motion gave higher ranges at L2-3 for females (p < 0.05). Age above and below the inter-quartile ranges did not have any significant effect on translation range for any level or protocol. It should also be noted that L5-S1 translation, measured using controlled motion protocols, returned very small values when measured during motion as opposed to at its end, while weight bearing measurements returned more variation and less consistency than recumbent ones (Fig. 6a–e).
Box plots showing median intervertebral translations from L2-5 at baseline (hatched box) and follow-up (clear box) measured (a) at end of uncontrolled weight bearing flexion (b) during controlled weight bearing flexion (c) at end of controlled weight bearing flexion (d) during recumbent flexion (e) at end of recumbent flexion.
Discussion
This research found that static radiographs gave twice the measurement error of QF and higher L4-5 and L5-S1 ranges when used to measure flexion translation. In effect, this means that it is not possible to detect translation of under 4 mm using static radiographs, 2.5 mm using weight bearing QF or 2.0 mm using recumbent QF. Furthermore, the normative ranges for each protocol are different for males and females, but not in older people. A cut-off at 4 mm for inferring instability is consistent with much of the literature as reviewed by Leone et al., however, as recognised by Nizard et al., population variation and lack of standardisation have made any such cut off somewhat tenuous5,24. Nevertheless, Posner et al.’s criterion for selecting patients with instability for fusion treatment, which defines a cut off of 8% of vertebral body depth for anterior translation is generally accepted, although this would amount to only 2.8 mm using a standard intervertebral body depth of 35 mm25,26,27.
In this study, measurement at the end of uncontrolled motion using static radiographs was more variable than using QF. At L4-5 and L5-S1, this returned approximately twice the measurement error of the QF protocols, while static, uncontrolled weight bearing measurements were similar to guided weight bearing QF measurements at L2-3 and L3-4.
The least population variability and measurement error was found when participants were imaged during passive recumbent motion, as has been recommended for the detection of excessive translation in spondylolisthesis10.
The 4 mm measurement error for weight bearing, static, unguided, end of range measurements was especially applicable to L4-5 and L5-S1. These levels are frequently of interest in terms of translatory slip, however, this may be uncommon in back pain populations. A recent study of aberrant motion in chronic, nonspecific back pain did not find translation to be greater in patients than healthy controls17. Even in patients with spondylolisthesis, excessive translation is also not necessarily a feature, while in older individuals with degenerative spinal stenosis, bone loss, arthritic outgrowth and vertebral mal-alignment may make the measurement of translation using any current form of radiographic imaging additionally problematical5,28.
The tendency for static views, acquired at the end of trunk motion, to give different values from QF may be thought to be because the range of trunk motion at the end of a weight-bearing unguided flexion motion could be greater than 60°, which is the standard range of flexion used for standing guided weight-bearing QF19. However, free bending resulted in only approximately 0.5 mm greater translation than controlled bending to 60°. Indeed, the median ranges of translation found in this study, by all of the protocols, compare favourably with those found in a separate study of healthy volunteers29. However, although studies of intervertebral translation in back pain patients have concluded that it is related to age and disc height, it does not differentiate patients from controls17,30,31. This may be partially a result of the uncontrolled variation associated with current measurement methods. However, composite disc degeneration throughout the lumbar spine has been associated with disproportionate sharing of angular motion between the lumbar spine segments in chronic, nonspecific back pain patients16. Thus, it may be that it is the distribution of degenerated discs in the lumbar spine, rather than large changes in ranges of motion at individual levels, that is most closely associated with symptoms in chronic, nonspecific low back pain32.
Finally, the qualitative use of fluoroscopy tends to be associated with prolonged exposures, raising the expectation of higher radiation dosage. However, the QF protocols are, by definition, quantitative and in this study resulted in effective radiation dosages of less than 0.3 mSv each. This is considerably less than the 1.3 mSv quoted as the typical effective dose expected for a series of X-rays of the lumbar spine for diagnostic purposes33,34. This makes continued of the use of plain radiographs difficult to justify for most cases where degrees of increased translation that are not measurable might be acted upon.
Limitations
The present study did not include extension motion; however, its purpose was to compare radiographic techniques for their measurement properties while minimising radiographic exposure. The levels considered also did not include L1 because the intensifier diameter was too small to permit it.
Further work
These methods, although tested on a healthy asymptomatic population here, have also been utilised to evaluate back pain populations16,17. Therefore, this study should be repeated in symptomatic cohorts to establish repeatability and variability of translation.
Conclusion
Quantitative fluoroscopic measurement of lumbar intervertebral flexion translation in healthy control participants during passive recumbent QF gave significantly lower values than static, weight-bearing unguided imaging. It also resulted in lower population variation and approximately half the measurement error, which for static images during uncontrolled motion was in the region of 4 mm. Thus, clinical decisions based on smaller amounts of sagittal translation would require QF imaging.
References
Hoy, D. et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Annals of Rheumatic Diseases 73, 968–974 (2014).
Borenstein, D. Mechanical low back pain - a rheumatologist’s view. Nature review. Rheumatology 9, 643–653 (2013).
Barz, T. et al. A conceptual model of compensation/decompensation in lumbar segmental instability. Medical Hypotheses 83, 312–316 (2014).
Panjabi, M. M. A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. European Spine Journal 15, 668–676 (2006).
Leone, A., Guglielmi, G., Cassar-Pullicino, V. N. & Bonomo, L. Lumbar intervertebral instability: a review. Radiology 245, 62–77 (2007).
Mannion, A. F. et al. Development of appropriateness criteria for the surgical treatment of symptomatic lumbar degenerative spondylolisthesis (LDS). European Spine Journal 23, 1903–1917 (2014).
Iguchi, T. et al. Lumbar instability and clinical symptoms. Which is the more critical factor for symptoms: sagittal translation or segment angulation? J Spinal Disord Tech 17, 284–290 (2004).
Dvorak, J., Panjabi, M. M., Chang, D. G., Theiler, R. & Grob, D. Functional radiographic diagnosis of the lumbar spine. Flexion-extension and lateral bending. Spine 16, 562–571 (1991).
Dombrowski, M. E. et al. ISSLE Prize in Bioengineering Science 2018: dynamic imaging of degenerative spondylolisthesis reveals mid-range dynamic lumbar instability not evident on static clinical radiographs. European Spine Journal 27, 752–762, https://doi.org/10.1007/s00586-018-5489-0 (2018).
Wood, K. B., Popp, C. A., Transfeldt, E. E. & Geissele, A. E. Radiographic evaluation of instability in spondylolisthesis. Spine 19, 1697–1703 (1994).
Liang, H.-F., Liu, S.-H., Chen, Z.-X. & Fei, Q.-M. Decompression plus fusion versus decompression alone fordegenerative lumbar spondylolisthesis: s systematic review and meta-analysis. European Spine Journal 26, 3084–3095 (2017).
Eisenstein, S. B. A. In 10th International Conference for the Failed Back. 1–11.
Teyhen, D. S., Flynn, T. W., Childs, J. D. & Abraham, L. D. Arthrokinematics in a subgroup of patients likely to benefit from a lumbar stabilization exercise program. Physical Therapy 87, 313–325 (2007).
Mellor, F. E., Thomas, P., Thompson, P. & Breen, A. C. Proportional lumbar spine inter-vertebral motion patterns: A comparison of patients with chronic non-specific low back pain and healthy controls. European Spine Journal 23, 2059–2067, https://doi.org/10.1007/s00586-014-3273-3 (2014).
Ahmadi, A., Maroufi, N., Behtash, H., Zekavat, H. & Parianpour, M. Kinematic analysis of dynamic lumbar motion in patients with lumbar segmental instability using digital videofluoroscopy. European Spine Journal 18, 1677–1685 (2009).
Breen, A. & Breen, A. Uneven intervertebral motion sharing is related to disc degeneration and is greater in patients with chronic, non-specific low back pain: an in vivo, cross-sectional cohort comparison of intervertebral dynamics using quantitative fluoroscopy. Eur Spine J 27, 145–153, https://doi.org/10.1007/s00586-017-5155-y (2018).
Breen, A., Mellor, F. & Breen, A. Aberrant intervertebral motion in patients with treatment-resistant nonspecific low back pain: a retropective cohort study and control comparison. European Spine Journal 27, 2831–2839, https://doi.org/10.1007/s00586-018-5666-1 (2018).
Breen, A. & Breen, A. Accuracy and repeatability of quantitative fluoroscopy for the measurement of sagittal plane translation and instantaneous axis of rotation in the lumbar spine. Medical Engineering and Physics 38, 607–614 (2016).
Breen, A. C. et al. Measurement of inter-vertebral motion using quantitative fluoroscopy: Report of an international forum and proposal for use in the assessment of degenerative disc disease in the lumbar spine. Advances in Orthopaedics, 1–10, https://doi.org/10.1155/2012/802350 (2012).
Santos, E. R. G., Goss, D. G., Morcom, R. K. & Fraser, R. D. Radiological assessment of interbody fusion using carbon fibre cages. Spine 28, 997–1001 (2003).
Bland, J. M., Altman & D. G. Statistics Notes: Measurement error. British Medical Journal 313 (1996).
Van Herp, G., Rowe, P., Salter, P. & Paul, J. P. Three-dimensional lumbar spinal kinematics: a study of range of movement in 100 healthy subjects aged 20 to 60+ years. Rheumatology 39, 1337–1340 (2000).
Frobin, W., Brinckmann, P., Biggemann, M., Tillotson, M. & Burton, K. Precision measurement of disc height, vertebral height and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clinical Biomechanics 12, S22–S30 (1997).
Nizard, R. S., Wybier, M. & Laredo, J.-D. Radiologic Assessment of Lumbar Intervertebral instability and degenerative spondylolisthesis. Radiologic Clinics of North America 39, 55–71 (2001).
Posner, I. R. A., White, A. A., Edward, W. T. & Hayes, W. C. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine 7, 374–389 (1982).
Yone, K. & Sakou, T. Usefulness of Posner’s Definition of Spinal Instability for Selectionof Surgical Treatment for Lumbar Spinal Stenosis. Journal of Spinal Disorders 12, 40–44 (1999).
Frobin, F., Brinckmann, P., Lievseth, G., Biggemann, M. & Reikeras, O. Precision measurement of segmental motion from flexion-extension radiographs of the lumbar spine. Clinical Biomechanics 11, 457–465 (1996).
Yao, Q., Wang, S., Shin, J.-H., Li, G. & Wood, K. Motion characteristics of the lumbar spinous processes with degenerative disc disease and degenerative spondylolisthesis. European Spine Journal 22, 2702–2709 (2013).
Staub, B. N., Holman, P. J., Reitman, C. A. & Hipp, J. Sagittal plane lumbar intervertebral motion during seated flexion-extension radiogaphs of 658 asymptomatic nondegenerated levels. Journal of Neurosurgery Spine 23, 731–738 (2015).
Iguchi, T. et al. Intimate relationship between instability and degenerative signs at L4-5 segment examined by flexion-extension radiography. European Spine Journal 20, 1349–1354 (2011).
Taghipour-Darzi, M., Takamjani, E. E., Salavati, M., Mobini, B. & Zekavat, H. The validity of vertebral translation and rotation in differentiating patients with lumbar segmental instability. Physiotherapy Research International 17, 227–234 (2012).
Von Forell, G. A., Stephens, T. K., Samartzis, D. & Bowden, A. E. Low Back Pain: A Biomechanical Rationale Based on “Patterns” of Disc Degeneration. Spine 40, 1165–1172 (2015).
Public Health England. Patient dose information: guidance; Available from: https://www.gov.uk/government/publications/medical-radiation-patient-doses/patient-dose-information-guidance (2008).
Breen, A., Hemming, R., Mellor, F. & Breen, A. Intrasubject repeatability of in vivo intervertebral motion parameters using quantitative fluoroscopy. Eur Spine J 28, 450–460, https://doi.org/10.1007/s00586-018-5849-9 (2019).
Acknowledgements
Prof. Alan Breen received a project grant from the European Chiropractors Union Research Fund (ECURF), and Dr Rebecca Hemming received a Seedcorn Bursary from the Cardiff Institute of Tissue Engineering and Repair (CITER).
Author information
Authors and Affiliations
Contributions
The studies were designed by Ax.B, Al.B. and R.A. Data and Figures were acquired by Ax.B., E.C. and Al.B. Data were analysed by them and R.H. The manuscript was drafted by Ax.B. and edited by R.H., R.A., E.C. and Al.B. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
I declare that the authors have no competing interests as defined by Nature Research, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Breen, A., Claerbout, E., Hemming, R. et al. Comparison of intra subject repeatability of quantitative fluoroscopy and static radiography in the measurement of lumbar intervertebral flexion translation. Sci Rep 9, 19253 (2019). https://doi.org/10.1038/s41598-019-55905-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-55905-1
- Springer Nature Limited
This article is cited by
-
What is the most appropriate method for the measurement of the range of motion in the lumbar spine and how does surgical fixation affect the range of movement of the lumbar spine in adolescent idiopathic scoliosis? A systematic review protocol
Systematic Reviews (2022)
-
An in vivo study exploring correlations between early-to-moderate disc degeneration and flexion mobility in the lumbar spine
European Spine Journal (2020)