Abstract
The brain and nervous system play an important role in pancreatic β-cell function. This study investigated the role of muscarinic agonists or acetylcholine, which is the major neurotransmitter in the vagal nerve, in regulating pancreatic β-cell mass and glucose homeostasis. Administration of the muscarinic agonist bethanechol increased insulin secretion and improved glucose tolerance in insulin-receptor substrate 2 (IRS2)-knockout (IRS-2−/−) mice and diet-induced obesity mice. Oral administration of bethanechol increased β-cell mass and proliferation in wild-type mice, but not IRS-2−/− mice. The muscarinic agonist also increased the incorporation of 5-bromo-2′-deoxyuridine (BrdU) into islets isolated from wild-type mice and pancreatic β-cell line MIN6. The phosphorylation of protein kinase B (Akt) induced by oral administration of bethanechol was observed in wild-type mice, but not IRS-2−/− mice. The secretion of glucagon-like peptide-1 (GLP-1) was also stimulated by bethanechol in wild-type mice, and a GLP-1 antagonist partially inhibited the bethanechol-induced increase in β-cell mass. These results suggest that the muscarinic agonist exerted direct and indirect effects on β-cell proliferation that were dependent on the IRS-2/Akt pathway. The bethanechol-stimulated release of GLP-1 may be indirectly associated with β-cell proliferation.
Similar content being viewed by others
Introduction
The brain and the nervous system are well recognized for their important role in metabolic control. Previous studies have demonstrated how the nervous system regulates glucose homeostasis and contributes towards pancreatic β-cell regeneration1,2,3. In obese and hyperglycaemic ob/ob mice, glucose tolerance and islet proliferation rates were analysed following vagotomy1. It was observed that in vagotomised mice, the islet cell proliferation rate was reduced, and the islet volume was smaller. Another study reported that vagal hyperactivity, which can occur as a result of ventromedial hypothalamic lesions, induced pancreatic β-cell proliferation2. Moreover, it was reported that the activation of obesity-related hepatic extracellular signal-related kinase (ERK) caused the proliferation of pancreatic β-cells through signal transduction to the nervous system3. These results suggest that the vagal nerve system affects the proliferative ability of pancreatic β-cells. In this study, we aim to elucidate the neurotransmitters or receptors that are responsible for increasing the β-cell mass following vagal stimulation and determine whether direct or indirect mechanisms are involved in this activity.
Because the muscarinic receptor agonist acetylcholine is the main neurotransmitter of vagal nerve signals and M3 muscarinic receptor is predominant in the β-cell, several studies have reported the relationship between the M3 muscarinic receptor and pancreatic β cell maintenance. The results are described as follows: (1) Acetylcholine releases insulin in a glucose-dependent manner in the β-cell; (2) The continuous activation of the M3 receptor in transgenic mice improved glucose homeostasis and increased insulin release4, and β-cell-specific knockout mice for the M3 muscarinic receptor decreased insulin release and impaired glucose tolerance5; (3) The continuous activation of the M3 designer receptor improved glucose tolerance and increased pancreatic β-cell through the IRS2/Akt pathway6 and (4) The co-stimulation of carbachol and pituitary adenylate cyclase-activating polypeptide (PACAP) increased β-cell proliferation via FoxM1 in isolated islets7. Because adult β-cells were recently reported to be maintained by self-replication from the existing β cells in the islets8,9, the muscarinic receptor signal increasing the adult β-cell replication for the regeneration of cells in individuals with diabetes mellitus could be a potential therapeutic target.
The present study aimed to elucidate the proliferative mechanism or effect of the muscarinic receptor which remains unclear, in vivo or in islets. In this study, we used bethanechol as a muscarinic agonist that can be administered in vivo. Our results indicated that the muscarinic agonists increased β-cell mass and proliferation. In addition, we investigated the potential involvement of the insulin signal molecules IRS-2/Akt or GLP-1 release in muscarinic agonist-induced pancreatic β-cell proliferation. These molecules are involved in the maintenance of pancreatic β-cell mass10,11,12,13,14,15,16,17.
Results
Administration of muscarinic agonist bethanechol improves glucose homeostasis in diabetic model mice and diet-induced obesity mice
To examine the effect of bethanechol in a mouse model of diabetes, it was administered to IRS-2−/− mice, which show insulin resistance and high glucose levels. Bethanechol (2 µg/g) was injected subcutaneously 15 min prior to oral glucose loading in wild-type mice and IRS-2−/− mice. Bethanechol increased insulin secretion and improved glucose tolerance in both types of mice (Fig. 1A). The bethanechol-induced secretion of insulin in the IRS-2−/− mice was higher than that in the wild-type mice (Fig. 1B). The results of the insulin tolerance test revealed no significant difference in glucose levels between the control and bethanechol groups of wild-type mice; however, 30 min following insulin injection, the glucose level in the bethanechol-injected IRS-2−/− mice was significantly lower than that in the control mice (Fig. 1C).
Administration of bethanechol improves glucose tolerance in a mouse model of diabetes. Experiments were performed in 8- to 10-week-old wild-type (WT) mice and insulin-receptor substrate 2 (IRS-2)−/− mice in standard chow diet–fed condition. (A) Plasma glucose levels during the oral glucose tolerance test (OGTT) following administration of bethanechol (Bch; 2 µg/g body weight). Bch was administered subcutaneously 15 min prior to oral glucose loading (1.5 mg/g body weight) in WT mice (left; n = 10) and IRS-2−/− mice (right; n = 11). (B) Serum insulin levels during the OGTT following administration of Bch (2 µg/g) in WT mice (left; n = 10) and IRS-2−/− mice (right; n = 10). (C) Plasma glucose levels during the insulin tolerance test following administration of Bch (2 µg/g). Bch was administered subcutaneously 15 min prior to insulin injection in WT mice (left; n = 6) and IRS-2−/− mice (right; n = 4). The data represent the mean ± standard error of the mean (SEM); *P < 0.05 vs. control.
To examine the effect of bethanechol on diet-induced obesity (DIO) mice, 7-week-old male mice were fed a high-fat diet (HFD) for 5–6 or 16 weeks, following which an oral glucose tolerance test was performed. The subcutaneous administration of bethanechol (5 µg/g) prior to oral glucose loading improved glucose tolerance (Fig. 2A,C) and increased insulin secretion markedly (Fig. 2B,D). Oral administration of bethanechol (100 µg/g) also improved casual glucose after 1 and 2 h of administration (Fig. 2E), and increased insulin secretion significantly after 1 h in DIO mice (Fig. 2F).
Administration of bethanechol (Bch) improves glucose tolerance and casual glucose in diet-induced obesity mice. A high-fat diet (HFD) was started in 7-week-old C57BL/6J mice and experiments were performed for 5–6 or 16 weeks following HFD feeding. (A) Plasma glucose levels and (B) serum insulin levels in the oral glucose tolerance test (OGTT) following administration of Bch (5 µg/g body weight) in HFD-fed mice for 6 weeks. Bch was administered subcutaneously 15 min prior to oral glucose loading (1.5 mg/g body weight) (n = 5–6). (C) Plasma glucose levels and (D) serum insulin levels in the OGTT following administration of Bch (5 µg/g) in HFD-fed mice for 16 weeks. Bch was administered subcutaneously 15 min before oral glucose loading (1.5 mg/g body weight) (n = 5–6). (E) Casual glucose levels and (F) serum insulin levels following oral administration of Bch (100 µg/g). Bch was administered orally and HFD was stopped for 4 h (n = 5–6). (F) Data are expressed as the increase from the 0-h insulin level to the 1-h insulin level. The data represent the mean ± standard error of the mean (SEM); *P < 0.05 vs. control.
Bethanechol administration caused cholinergic side effects in DIO mice and wild-type (WT) mice. The number of mice exhibiting salivation or lacrimation was counted. Subcutaneous administration of bethanechol (5 µg/g) in the mice fed a HFD for 5–6 or 16 weeks, respectively, induced salivation (41.6% and 100%) and lacrimation (25% and 33.3%) (Supplementary Table). In the mice administered oral bethanechol (100 µg/g), no salivation or lacrimation were observed. Bethanechol (5 µg/g) administered subcutaneously also caused miosis in WT mice (slight contraction from 4 mm to 3–3.5 mm), as measured macroscopically with a loupe (data not shown).
Chronic administration of bethanechol promotes β-cell proliferation
Long-term administration of bethanechol in mice was examined by measuring blood glucose levels and changes in body weight. Bethanechol was added to drinking water at a concentration of 30 µg/mL, and the casual blood glucose and body weight were measured for 20 weeks in WT and IRS-2−/− mice. There were no significant differences in body weight, casual blood glucose or glucose tolerance between mice with or without bethanechol administration, in both WT and the IRS-2−/− mice (Figs 3A,B; S1). The β-cell mass of mice continuously administered bethanechol (30 µg/mL in water) was also evaluated for 6 weeks. In the WT mice, the β-cell mass increased significantly in those receiving bethanechol compared with the controls (control: 0.76 mg; bethanechol: 1.08 mg). However, there was no significant difference in the β-cell mass between the bethanechol-administered IRS-2−/− mice and control IRS-2−/− mice (control: 0.70 mg; bethanechol: 0.84 mg; Fig. 3C).
Chronic administration of bethanechol (Bch) promotes ß-cell proliferation mediated by insulin-receptor substrate 2 (IRS-2). Eight-week-old wild-type (WT) mice and IRS-2−/− mice were administered Bch (30 µg/mL) in drinking water. (A) Casual blood glucose level and (B) body weight in WT mice and IRS-2−/− mice for 20 weeks (n = 12–15). (C) Quantification of the β-cell mass in WT mice and IRS-2−/− mice administered Bch for 6 weeks (left; n = 6–8), and representative pancreatic sections (right). (D) Quantification of 5-bromo-2′-deoxyuridine (BrdU)-positive and insulin-positive cells in WT mice and IRS-2−/− mice administered Bch for 6 weeks (left). Insulin is stained green, nuclei are stained blue and BrdU-positive nuclei are stained red. The white arrows indicate BrdU-positive, insulin-positive cells (right). (E) Oral administration of Bch promoted β-cell proliferation. Eight-week-old WT mice and IRS-2−/− mice were orally administered Bch 1 µg/g once a day for 2 weeks (n = 4). Quantification of the β-cell mass in WT mice and IRS-2−/− mice (left), and representative pancreatic sections (right). The data represent the mean ± standard error of the mean (SEM); *P < 0.05 vs. control.
The incorporation of 5-bromo-2′-deoxyuridine (BrdU) was assessed to determine the effect of the muscarinic agonist on the proliferation of β-cells. As shown in Fig. 3D, bethanechol (30 µg/mL in water) administration increased the number of BrdU-positive cells (control: 0.63%; bethanechol: 1.29%) in the WT mice. In the IRS-2−/− mice, no significant increase in BrdU-positive cells was observed following agonist administration (control: 0.81%; bethanechol: 0.94%; Fig. 3D).
To examine the issue of bethanechol stability in water, bethanechol was given orally at 1 µg/g body weight once a day, and the β-cell mass was measured 2 weeks following the start of administration (Fig. 3E). The WT mice that were treated with bethanechol exhibited an increase in the β-cell mass compared with control mice (control: 1.05 mg; bethanechol: 1.55 mg), whereas no significant increase was observed in the IRS-2−/− mice (control: 1.03 mg; bethanechol: 0.82 mg).
Bethanechol directly stimulates pancreatic β-cell proliferation
To determine whether bethanechol has a direct effect on pancreatic β cells, BrdU incorporation was investigated in the pancreatic β-cell line MIN6. MIN6 cells were cultured in media containing BrdU and the muscarinic agonist for 24 h, following which the cells were fixed, stained with fluorescent isothiocyanate (FITC)-labelled BrdU antibodies and analysed by flow cytometry. BrdU incorporation increased significantly in the carbachol-treated or bethanechol-treated cells in a concentration-dependent manner (Fig. 4A,B). This increase was suppressed completely by the addition of atropine 50 µM (Fig. 4C). The Akt inhibitor perifosine (5 µM) inhibited the bethanechol (1 mM)-induced incorporation of BrdU (Fig. 4D), whereas the mitogen-activated protein kinase (MEK) inhibitor PD98059 (50 µM) did not (Fig. 4E).
Bethanechol (Bch) directly promotes β-cell proliferation. (A–E) MIN6 cells were treated with Bch (1 mM) or carbachol (Cch; 0.5 mM) for 24 h. Cells were simultaneously incubated with the agonist and atropine (50 µM), perifosine (5 µM) or PD98059 (50 µM). 5-Bromo-2′-deoxyuridine (BrdU) was then added to the media and the cells were fixed 20 h after the addition of BrdU. BrdU-positive cells were measured using flow cytometry. (F) Isolated islets from 8-week-old wild-type (WT) mice and insulin-receptor substrate 2 (IRS-2) −/− mice were incubated in media containing Bch (1 mM) or Cch (0.5 mM) and BrdU for 24 h. The islets were fixed and BrdU incorporation was measured using a BrdU cell proliferation assay kit. (A) Cch-induced BrdU incorporation in MIN6 cells (n = 10). (B) Bch-induced BrdU incorporation in MIN6 cells (n = 6). (C) Effect of atropine (50 µM) on Bch- or Cch-induced BrdU incorporation in MIN6 cells (n = 6). (D) Effect of perifosine (5 µM) on Bch-induced BrdU incorporation in MIN6 cells (n = 4). (E) Effect of PD98059 (50 µM) on Bch-induced BrdU incorporation in MIN6 cells (n = 4). (F) Bch- or Cch-induced BrdU incorporation in isolated islets from WT mice (left; n = 23) and IRS-2−/− mice (right; n = 8). The data represent the mean ± standard error of the mean (SEM); *P < 0.05 vs. control.
Islets were isolated from 8-week-old WT or IRS-2−/− mice to examine the incorporation of BrdU following treatment with muscarinic agonists in a similar manner. Islets were incubated in media containing bethanechol (1 mM) or carbachol (0.5 mM) and BrdU for 24 h, after which BrdU incorporation was measured. Similar to that in MIN6 cells, a significant increase in BrdU incorporation was observed following the stimulation of islets from WT mice with bethanechol (1 mM) or carbachol (0.5 mM) (Fig. 4F). In islets from the IRS-2−/− mice, no BrdU incorporation was observed (Fig. 4F). Collectively, these results suggest that muscarinic agonists directly affected the proliferative ability of pancreatic β-cells through IRS-2.
Phosphorylation of Akt and protein level of cyclin D2 are increased in bethanechol-treated mouse islets
To assess the mechanisms involved in muscarinic agonist-mediated β-cell proliferation, intracellular signalling was investigated in mouse islets. Following oral administration of bethanechol (1 µg/g) for 1 week in WT and IRS-2−/− mice, islets were isolated and the phosphorylation of Akt was analysed by western blotting. The phosphorylation of Akt increased significantly in response to bethanechol in the WT mice, but not in the IRS-2−/− mice (Fig. 5A). The protein level of cyclin D2 also increased in response to bethanechol in the WT mice, but not in the IRS-2−/− mice (Fig. 5B). Bethanechol did not alter the protein levels of transcription factors FoxO1, FoxM1 or PDX1 (Fig. 5C). These results suggest that the IRS-2/Akt/cyclin D2 pathway mediated bethanechol-induced β-cell proliferation.
The muscarinic agonist increases the phosphorylation of Akt and expression of cyclin D2 protein in mouse islets. (A) Phosphorylation of Akt and (B) expression of cyclin D2 protein were evaluated in isolated islets from wild-type (WT) mice and insulin-receptor substrate 2 (IRS-2)−/− mice orally administered bethanechol (Bch; 1 µg/g body weight) once a day for 1 week (n = 4–9). (C) Protein levels of FoxO1, FoxM1 and PDX1 were analysed in WT mice administered Bch (1 µg/g) once a day for 1 week (n = 3–7). The data represent the mean ± standard error of the mean (SEM). *P < 0.05 vs. control.
GLP-1 is released in bethanechol-treated mice and its antagonist inhibits the bethanechol-induced increase in β-cell mass
To analyse the indirect effects of bethanechol, we focused on glucagon-like peptide-1 (GLP-1). The secretion of GLP-1 was measured 15 min following the subcutaneous administration of bethanechol (2 µg/g). GLP-1 secretion increased significantly in the bethanechol-treated WT mice, but there was no significant change in the secretion of GLP-1 in bethanechol-treated IRS-2−/− mice (Fig. 6A).
Bethanechol (Bch) increases the secretion of glucagon-like peptide-1 (GLP-1) and pretreatment with the GLP-1 antagonist suppresses the Bch-induced increase in β-cell mass in mice. (A) Eight-week-old C57BL/6J mice were starved for 18–22 h and Bch (2 µg/g body weight) was subcutaneously administered to wild-type (WT) mice and insulin-receptor substrate 2 (IRS-2)−/− mice (n = 17–19). Serum GLP-1 levels were measured 15 min after Bch administration. (B) Pretreatment with exendin 9–39 suppressed the increase in β-cell mass caused by Bch in C57BL/6J mice. Eight-week-old C57BL/6J mice were administered Bch (10 µg/g) orally for 2 weeks. Exendin 9–39 (30 pmol/g body weight) was intraperitoneally administered 15 min prior to Bch administration. The β-cell mass was quantified (left; n = 4), with representative pancreatic sections (right). The data represent the mean ± standard error of the mean (SEM). *P < 0.05 vs. control.
To investigate the role of GLP-1, the mice were pretreated with the GLP-1 antagonist exendin 9–39 (30 pmol/g, intraperitoneally), 15 min prior to oral administration of bethanechol. Bethanechol was added at 10 µg/g once a day and the β-cell mass was measured 2 weeks following the start of administration. Bethanechol (10 µg/g) administration increased the β-cell mass significantly in the vehicle mice (control: 0.76 mg; bethanechol: 1.39 mg), whereas no significant increase in the β-cell mass was observed following agonist administration in the mice pretreated with exendin 9–39 (control: 0.97 mg; bethanechol: 1.15 mg) (Fig. 6B). However, exendin 9–39 did not completely suppress the increase in β-cell mass in the bethanechol-treated mice; there was still a bethanechol-induced marginal increase in the β-cell mass compared with that in the controls.
Discussion
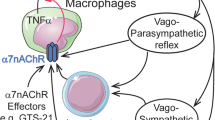
In mice, islets are largely dominated by parasympathetic neurons18. Generally, in the pancreatic islets, the parasympathetic neurons promote insulin secretion and the sympathetic neurons inhibit insulin secretion19,20,21; the brain and the vagal nervous system play an important role in pancreatic β-cell proliferarion. Because acetylcholine is the major neurotransmitter stored in vagal nerve endings, we aimed to elucidate the association between muscarinic receptor agonists and β-cell maintenance. Our results demonstrated that the muscarinic receptor agonist bethanechol improved glucose homeostasis in IRS-2−/− and DIO mice, and increased the pancreatic β-cell proliferation. These proliferative effects were caused via simultaneous activation of the muscarinic receptor and the GLP-1 receptor signal (Fig. S2).
Because vagal hyperactivity induces pancreatic β-cell proliferation, we hypothesised that chronic activation of muscarinic receptors in pancreatic β-cells might increase the β-cell mass. To test this hypothesis, we subjected mice to continuous, chronic administration of bethanechol, which significantly increased β-cell mass and BrdU incorporation (Fig. 3C–E). Furthermore, bethanechol-induced incorporation of BrdU was elevated significantly in islets isolated from the mice (Fig. 4F) and MIN6 cells (Fig. 4B), suggesting that this muscarinic agonist directly affects the proliferative ability of pancreatic β-cells.
We confirmed that the M1 and M3 muscarinic receptors were expressed, and the M3 receptor was predominant in the murine β-cells (Fig. S3). The β-cell mass increased in the transgenic mice with chronic activation of the Gq-coupled designer receptor which was created based on the M3 muscarinic receptor6, and mice treated with scopolamine butylbromide (a cholinergic antagonist) during lactation show lowered expression of the M3 receptor and decreased β-cell mass22. These findings suggest that the Gq-signalling of the M3 receptor was responsible for the β-cell mass expansion. However, a previous investigation on the effect of continuous stimulation of the β-cell M3 receptor on the β-cell mass and replication in transgenic mice demonstrated that it did not have a significant effect on the increase in the β-cell mass4. Pancreatic β-cell-specific knockout mice for the M3 muscarinic receptor do not exhibit obvious differences in the β-cell mass and cell size compared with WT mice23. Therefore, the direct effect of bethanechol on β-cell proliferation could not be caused by the M3 receptor signal alone. Because bethanechol activates all muscarinic receptor subtypes, activation of other muscarinic Gq receptor (e.g. M1) in the β-cell is also needed in bethanechol-induced β-cell proliferation.
It is well recognised that insulin signal molecules are important in the regulation of β-cell proliferation and mass expansion. Previous reports have suggested that IRS-2 and Akt proteins play a dominant role in regulating β-cell proliferation and maintaining β-cell mass13,14,15,24. Akt1 increases the levels of cyclins D1 and D2, and the cyclin/CDK4/Akt complex is responsible for β-cell proliferation25. Gq-coupled receptor-signalling also increases β-cell mass through IRS-2/Akt pathway6. To identify the mechanisms of bethanechol-induced β-cell proliferation, we examined the role of insulin signal molecules. Bethanechol did not increase the β-cell mass in the IRS-2−/− mice (Fig. 3C,E), and it phosphorylated Akt protein and increased the protein levels of cyclin D2 in an IRS-2-dependent manner (Fig. 5). Our findings suggest that the bethanechol-induced β-cell proliferation was mediated by the IRS-2/Akt/cyclin D2 pathway. Although ERK1 and ERK2 are reported to be upstream of the function of IRS-2 in the Gq-coupled receptor pathway6, the MEK inhibitor did not inhibit the bethanechol-induced incorporation of BrdU in MIN6 cells (Fig. 4E). The muscarinic agonist-induced β-cell proliferation might occur independently of ERK. A recent report indicated that co-stimulation of carbachol and PACAP promotes β-cell proliferation via FoxM1 in isolated islets7. Whereas we demonstrated that carbachol or bethanechol alone could increase BrdU uptake in islets or MIN6 cells (Fig. 4A,B,F), bethanechol administration did not affect the protein levels of FoxM1 (Fig. 5), and it did not lead to translocation of FoxM1 to the nucleus in murine islets (Fig. S4). It is possible that bethanechol regulates the activity of FoxM1 rather than changing its protein level or localisation.
Besides the direct effects of bethanechol to the β-cell, the indirect mechanisms may also be involved in this bethanechol-induced β-cell proliferation in vivo. Bethanechol might increase the secretion of other hormones involved in the regulation of β-cell mass, which include GLP-1, insulin-like growth factors, growth hormone, hepatocyte growth factor, parathyroid hormone-related protein, the epidermal growth factor ligand family and lactogens. It is reported that β-cell proliferation requires Gs-signalling (PACAP receptor), in addition to Gq-signalling (M3 muscarinic receptor)7. Muscarinic receptor subtypes M1, M2 and M3 are expressed in the distal intestine26,27 and our findings showed that bethanechol enhanced the release of GLP-1 (Fig. 6A), which is known to increase β-cell mass and activate Gs-signalling16,17. The GLP-1 antagonist partially suppressed the increase in β-cell mass in the bethanechol-treated mice (Fig. 6B). These results suggest that the GLP-1 receptor pathway is a factor in the muscarinic receptor-independent pathway. Therefore, the effects of the vagal nerve or bethanechol in pancreatic β cells may be exerted through the Gq- and Gs-signalling pathways (Fig. S2).
Moreover, the indirect effects of bethanecol also affect the enhancement of insulin release. We indicated that the subcutaneous administration of bethanechol increased insulin release in the IRS-2−/− mice more than that in the WT mice (Fig. 1B), resulting in improved glucose tolerance in the IRS-2−/− mice relative to the wild-type mice (Fig. 1A). However, the glucose-stimulated secretion of insulin was similar in the islets of the IRS-2−/− and WT mice (Fig. S5). Other unknown endogenous secretory proteins are associated with the enhancement of insulin release in the IRS-2−/− mice. To identify these secretory factors in the IRS-2−/− mice, we performed mass spectrometry-based proteomics analyses of plasma obtained from the control or IRS-2−/− mice; these experiments remain under investigation.
In conclusion, we demonstrated the beneficial effects of bethanechol on glucose homeostasis and pancreatic β-cell maintenance. The administration of bethanechol improved glucose homeostasis, and it directly or indirectly stimulated β-cell proliferation. The GLP-1 receptor pathway may be indirectly associated with β-cell proliferation. Therefore, muscarinic agonists and their downstream molecules could be potential targets for novel diabetic therapies.
Methods
Animals and animal care
The C57BL/6J WT mice were obtained from CLEA Japan. We backcrossed IRS-2−/− mice28 with C57BL/6J mice more than 10 times. All experiments were performed using male mice maintained on a standard chow diet. The chronic effects of bethanechol were investigated in IRS-2−/− mice and C57BL/6 J mice. Bethanechol was administered continuously (30 µg/mL in drinking water) or once-daily (1 µg/g given orally) in the IRS-2−/− mice and WT mice. In the exendin 9–39 experiment, 30 pmol/g exendin 9–3929 was administered intraperitoneally 15 min prior to bethanechol 10 µg/g administration orally in C57BL/6J mice for 2 weeks. In the experiment involving DIO mice, 7-week-old mice were fed a HFD. All animal procedures were performed in accordance with the institutional animal care guidelines and guidelines of the Animal Care Committee of Yokohama City University. The protocol was approved by the Yokohama City University Institutional Animal Care and Use Committee (permit no. F-A-18-020). The animals were housed in rooms maintained at a constant room temperature (25 °C) and on a 12-h light (from 07:00 AM onwards) and 12-h dark (from 7:00 PM onwards) cycle30.
Glucose tolerance and insulin tolerance tests
The plasma glucose levels and blood insulin levels were determined using GlutestNeoSuper (Sanwa Chemical Co.,) and an insulin kit (Morinaga), respectively. All mice were fasted for 18–22 hours prior to the oral glucose tolerance test followed by oral administration of glucose (1.5 mg/g body weight). An insulin tolerance test was performed by the intraperitoneal injection of mice with human insulin (0.75 mU/g body weight)31.
GLP-1 measurement
All mice were denied access to food for 18–22 h prior to subcutaneous administration of bethanechol (2 µg/g body weight). The active GLP-1 levels were measured 15 min after bethanechol administration using a GLP-1(Active) ELISA kit (Shibayagi). Blood was drawn into a syringe containing aprotinin (final concentration, 500 kIU/mL; Wako Pure Chemical Industries, Ltd.) as a dipeptidyl peptidase-IV inhibitor.
Histologic analysis
Mice were intraperitoneally injected with BrdU (100 µg/g; Nacalai Tesque, Inc) for 3 days and sacrificed. Three pancreatic tissue sections (100 µm apart) from each animal were prepared by fixation and paraffin-embedding. The sections were immunostained with antibodies to insulin, muscarinic acetylcholine receptor M1 (Santa Cruz), BrdU (Dako), and muscarinic acetylcholine receptor M3 (Bioss). Biotinylated secondary antibodies, a Vectastain elite ABC kit and a diaminobenzidine substrate kit (Vector) were used to examine the sections under bright-field microscopy to determine the β-cell mass. Alexa Fluor 488- and 555-conjugated secondary antibodies (Invitrogen) were used for fluorescence microscopy analysis. All images were captured using a BZ-9000 microscope (Keyence). The percentage area of the pancreatic tissues occupied by β cells was calculated using BIOREVO software (Keyence)31. In the BrdU staining experiment, 22–78 islets in each mouse were analysed to assess the frequency of BrdU-positive cells among the insulin-positive cells.
Cell culture and treatment
MIN6 cells (kindly provided by Professor Jun-ichi Miyazaki, Division of Stem Cell Regulation Research, Osaka University, Graduate School of Medicine, Osaka, Japan) were used between passages 25 and 40 at ∼80% confluence. The MIN6 cells were grown in Dulbecco’s modified Eagle medium (DMEM), containing 25 mM glucose supplemented with 10% (v/v) heat-inactivated fetal bovine serum (FBS), and equilibrated in 5% CO2 and 95% air at 37 °C32. Prior to the experiments, the medium was removed and the cells were washed twice with phosphate-buffered saline. Complete details of each treatment are provided in the corresponding figure legend.
BrdU incorporation in islets and MIN6 cells
Islets were isolated from 8-week-old mice using a method described previously31. The isolated islets were cultured in RPMI 1640 medium (Wako Pure Chemical Industries) containing 5.6 mM glucose supplemented with 1% FBS. Following incubation of the islets for 24 h in medium containing 1 mM bethanechol, 0.5 mM carbachol and BrdU, BrdU incorporation was measured with a BrdU cell proliferation assay (Calbiochem) in accordance with the manufacturer’s protocol.
BrdU incorporation was also investigated in the MIN6 pancreatic β-cell line using the FITC-BrdU Flow kit (BD Pharmingen) in accordance with the manufacturer’s protocol. Cells were cultured with serum-free DMEM containing 5.5 mM glucose for 24 h prior to stimulation. Cells were stimulated with muscarinic agonists for 24 h in the same medium, followed by the addition of BrdU. The cells were fixed 20 h later, stained with FITC-BrdU antibodies, and 20,000 cells were analysed by flow cytometry (FACS Canto II, BD Biosciences). The proportion of BrdU-positive cells was calculated using FACS DIVA software (BD Biosciences).
Immunoblotting
For immunoblotting, >100 isolated islets were lysed in ice-cold radioimmunoprecipitation buffer containing a complete protease inhibitor cocktail (Roche Diagnostics). The lysed islets were subjected to centrifugation and the extracts were subjected to immunoblotting with antibodies to the following proteins: Akt, phospho-Akt, forkhead transcription factor (FoxO1) (Cell Signalling Technology); cyclin D2, forkhead box protein M1 (FoxM1) (Santa Cruz); pancreatic and duodenal homeobox 1 (PDX1) (Merck); or β actin (Abcam). Densitometry was performed using Multi Gauge V3.0 software (FujiFilm).
Statistical analyses
All data are expressed as the mean ± standard error. All statistical analyses were performed using JMP 11.2.0 software. The data were analysed using Student’s t-tests or analysis of variance. A P value < 0.05 was considered to indicate a statistically significant difference.
References
Edvell, A. & Lindstrom, P. Vagotomy in young obese hyperglycemic mice: effects on syndrome development and islet proliferation. The American journal of physiology 274, E1034–1039 (1998).
Kiba, T. et al. Ventromedial hypothalamic lesion-induced vagal hyperactivity stimulates rat pancreatic cell proliferation. Gastroenterology 110, 885–893 (1996).
Imai, J. et al. Regulation of pancreatic beta cell mass by neuronal signals from the liver. Science 322, 1250–1254, https://doi.org/10.1126/science.1163971 (2008).
Gautam, D. et al. Beneficial metabolic effects caused by persistent activation of beta-cell M3 muscarinic acetylcholine receptors in transgenic mice. Endocrinology 151, 5185–5194, https://doi.org/10.1210/en.2010-0519 (2010).
Gautam, D. et al. Beneficial metabolic effects of M3 muscarinic acetylcholine receptor deficiency. Cell Metab 4, 363–375, https://doi.org/10.1016/j.cmet.2006.09.008 (2006).
Jain, S. et al. Chronic activation of a designer G(q)-coupled receptor improves beta cell function. The Journal of clinical investigation 123, 1750–1762, https://doi.org/10.1172/JCI66432 (2013).
Yamamoto, J. et al. Neuronal signals regulate obesity induced beta-cell proliferation by FoxM1 dependent mechanism. Nature communications 8, 1930, https://doi.org/10.1038/s41467-017-01869-7 (2017).
Dor, Y., Brown, J., Martinez, O. I. & Melton, D. A. Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature 429, 41–46, https://doi.org/10.1038/nature02520 (2004).
Dor, Y. & Melton, D. A. How important are adult stem cells for tissue maintenance? Cell cycle (Georgetown, Tex.) 3, 1104–1106 (2004).
Gunton, J. E. et al. Loss of ARNT/HIF1beta mediates altered gene expression and pancreatic-islet dysfunction in human type 2 diabetes. Cell 122, 337–349, https://doi.org/10.1016/j.cell.2005.05.027 (2005).
Halperin, F. et al. Insulin augmentation of glucose-stimulated insulin secretion is impaired in insulin-resistant humans. Diabetes 61, 301–309, https://doi.org/10.2337/db11-1067 (2012).
Kubota, N. et al. Insulin receptor substrate 2 plays a crucial role in beta cells and the hypothalamus. The Journal of clinical investigation 114, 917–927, https://doi.org/10.1172/jci21484 (2004).
Cantley, J. et al. Pancreatic deletion of insulin receptor substrate 2 reduces beta and alpha cell mass and impairs glucose homeostasis in mice. Diabetologia 50, 1248–1256, https://doi.org/10.1007/s00125-007-0637-9 (2007).
Bernal-Mizrachi, E., Wen, W., Stahlhut, S., Welling, C. M. & Permutt, M. A. Islet beta cell expression of constitutively active Akt1/PKB alpha induces striking hypertrophy, hyperplasia, and hyperinsulinemia. The Journal of clinical investigation 108, 1631–1638, https://doi.org/10.1172/jci13785 (2001).
Tuttle, R. L. et al. Regulation of pancreatic beta-cell growth and survival by the serine/threonine protein kinase Akt1/PKBalpha. Nat Med 7, 1133–1137, https://doi.org/10.1038/nm1001-1133 (2001).
Stoffers, D. A. et al. Insulinotropic glucagon-like peptide 1 agonists stimulate expression of homeodomain protein IDX-1 and increase islet size in mouse pancreas. Diabetes 49, 741–748 (2000).
Drucker, D. J. Glucagon-like peptides: regulators of cell proliferation, differentiation, and apoptosis. Molecular endocrinology (Baltimore, Md.) 17, 161–171, https://doi.org/10.1210/me.2002-0306 (2003).
Rodriguez-Diaz, R. et al. Innervation patterns of autonomic axons in the human endocrine pancreas. Cell Metab 14, 45–54, https://doi.org/10.1016/j.cmet.2011.05.008 (2011).
Ahren, B. I. G protein-coupled receptors as potential targets for treatment of type 2 diabetes. Nat Rev Drug Discov 8, 369–385, https://doi.org/10.1038/nrd2782 (2009).
Ahren, B. Autonomic regulation of islet hormone secretion–implications for health and disease. Diabetologia 43, 393–410, https://doi.org/10.1007/s001250051322 (2000).
Ahren, B. Islet nerves in focus–defining their neurobiological and clinical role. Diabetologia 55, 3152–3154, https://doi.org/10.1007/s00125-012-2727-6 (2012).
Malta, A. et al. Neonatal treatment with scopolamine butylbromide prevents metabolic dysfunction in male rats. Scientific reports 6, 30745, https://doi.org/10.1038/srep30745 (2016).
Gautam, D. et al. A critical role for beta cell M3 muscarinic acetylcholine receptors in regulating insulin release and blood glucose homeostasis in vivo. Cell Metab 3, 449–461, https://doi.org/10.1016/j.cmet.2006.04.009 (2006).
Assmann, A., Hinault, C. & Kulkarni, R. N. Growth factor control of pancreatic islet regeneration and function. Pediatric diabetes 10, 14–32, https://doi.org/10.1111/j.1399-5448.2008.00468.x (2009).
Fatrai, S. et al. Akt induces beta-cell proliferation by regulating cyclin D1, cyclin D2, and p21 levels and cyclin-dependent kinase-4 activity. Diabetes 55, 318–325 (2006).
Ito, Y. et al. Quantitative analysis of the loss of muscarinic receptors in various peripheral tissues in M1-M5 receptor single knockout mice. British Journal of Pharmacology 156, 1147–1153, https://doi.org/10.1111/j.1476-5381.2009.00113.x (2009).
Anini, Y. & Brubaker, P. L. Muscarinic receptors control glucagon-like peptide 1 secretion by human endocrine L cells. Endocrinology 144, 3244–3250, https://doi.org/10.1210/en.2003-0143 (2003).
Kubota, N. et al. Disruption of insulin receptor substrate 2 causes type 2 diabetes because of liver insulin resistance and lack of compensatory beta-cell hyperplasia. Diabetes 49, 1880–1889 (2000).
Sundstrom, L. et al. The acute glucose lowering effect of specific GPR120 activation in mice is mainly driven by glucagon-like peptide 1. PloS one 12, e0189060, https://doi.org/10.1371/journal.pone.0189060 (2017).
Nakamura, A. et al. Control of beta cell function and proliferation in mice stimulated by small-molecule glucokinase activator under various conditions. Diabetologia 55, 1745–1754, https://doi.org/10.1007/s00125-012-2521-5 (2012).
Terauchi, Y. et al. Glucokinase and IRS-2 are required for compensatory beta cell hyperplasia in response to high-fat diet-induced insulin resistance. The Journal of clinical investigation 117, 246–257, https://doi.org/10.1172/JCI17645 (2007).
Miyazaki, J. et al. Establishment of a pancreatic beta cell line that retains glucose-inducible insulin secretion: special reference to expression of glucose transporter isoforms. Endocrinology 127, 126–132, https://doi.org/10.1210/endo-127-1-126 (1990).
Acknowledgements
We thank Dr. Junichi Miyazaki (University of Osaka) for providing us with the MIN6 cells. We also thank Misa Katayama for secretarial assistance. This work was supported in part by Grant-in-Aid for Scientific Research (B) 16H05329, and (B) 24390235 from the Ministry of Education, Culture, Sports, Science, and Technology (MEXT) of Japan (to Y.T.), and Grant-in-Aid for Scientific Research (C) 16K09762 and (C) 23591315 from MEXT of Japan, a Grant-in-Aid from Yokohama General Promotion Foundation (to Y.I.).
Author information
Authors and Affiliations
Contributions
Y.I. designed and performed experiments, analysed the data, and wrote the manuscript. E.S. and M.K. performed, experiments. Y.T. wrote the manuscript, reviewed and edited the manuscript, and contributed to discussions. Y.T. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
Yasuo Terauchi obtained research support from MSD K.K.; Ono Pharmaceutical Co., Ltd.; Nippon Boehringer Ingelheim Co., Ltd.; Novartis Pharma K.K.; Takeda Pharmaceutical Co., Ltd.; Mitsubishi Tanabe Pharma Corp.; Daiichi Sankyo Co., Ltd.; Sanwa Kagaku Kenkyusho Co., Ltd.; Novo Nordisk Pharma Ltd.; Eli Lilly Japan K.K.; Sanofi K.K.; Dainippon Sumitomo Pharma Co., Ltd.; Shionogi & Co., Ltd.; Bayer Yakuhin, Ltd.; Astellas Pharma, Inc.; Pfizer Japan, Inc.; and AstraZeneca K.K. Yuzuru Ito obtained research support from MSD life science foundation, AstraZeneca K.K., Mitsubishi Tanabe Pharma Corp. and Novartis Pharma K.K. Mitsuyo Kaji and Eri Sakamoto declare that there is no conflict of interest regarding to this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ito, Y., Kaji, M., Sakamoto, E. et al. The beneficial effects of a muscarinic agonist on pancreatic β-cells. Sci Rep 9, 16180 (2019). https://doi.org/10.1038/s41598-019-52691-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52691-8
- Springer Nature Limited
This article is cited by
-
Quercetin prevents insulin dysfunction in hypertensive animals
Journal of Diabetes & Metabolic Disorders (2022)
-
Unravelling innervation of pancreatic islets
Diabetologia (2022)
-
Intestinal Electrical Stimulation Enhances Release of Postprandial Incretin Hormones Via Cholinergic Mechanisms
Obesity Surgery (2021)