Abstract
The mandibular proximal ramus segments should be moved and rotated during orthognathic surgery-based skeletofacial reconstruction for the correction of challenging patients with facial asymmetry and malocclusion, but quantitative data regarding this rotation were not sufficient to date. This 3D computer-assisted study measured the proximal ramus segment rotation after 3D simulation-guided two-jaw surgery in patients with facial asymmetric deformity and class III malocclusion (n = 31). Using 3D mandible models and a reliable proximal ramus segment-related plane, angular changes in pitch, roll and yaw directions were measured before and one month after surgery. Significant rotational changes (p < 0.01) were observed in the left and right sides and overall proximal ramus segments after surgery, with absolute differences of 4.1 ± 3.0 (range −7.8 to 6.9), 2.8 ± 2.3 (−8.8 to 5.0), and 2.7 ± 2.4 (−6.6 to 9.9) degrees in pitch, roll, and yaw rotations, respectively. Numbness and mouth opening limiting occurred within the first 6 months after surgery but the patients had an unremarkable long-term postoperative course, with no revisionary surgery required. This study contributes to the multidisciplinary-related literature by revealing that proximal ramus segment rotation and rigid fixation with no postoperative intermaxillary immobilization was practicable in skeletofacial surgery for the successful treatment of asymmetric deformity and class III malocclusion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Skeletofacial surgery is an effective procedure for patients with challenging cases of facial asymmetry and malocclusion1,2,3,4. Positions of the maxilla and mandible, especially the ramus and chin, are frequently found to be deviated in individuals with facial asymmetry4. Traditionally, the intraoperative manipulation of the proximal ramus segment has mainly been based on the surgeon’s experience5,6. As preoperative misdiagnosis and inaccurate planning may contribute to unsuccessful results with the need for redo orthognathic surgery-based skeletofacial reconstruction or revisionary procedures, three-dimensional (3D) simulation has been recognized as a key factor to achieve consistent success in skeletofacial surgical treatment7,8,9,10,11,12. In the 3D planning of facial asymmetry correction, the final maxillomandibular complex incorporates the horizontal, anteroposterior, and vertical translations as well as pitch, roll and yaw rotations13. Using the bilateral sagittal split osteotomy (BSSO) technique, the proximal ramus segment should also be rotated in the three potential directions to achieve a symmetric and balanced face, with center of rotation at the condyle. Alternatively, others have reported the use of the intraoral vertical ramus osteotomy (IVRO) technique but requiring postoperative intermaxillary immobilization14,15.
In this setting, the postoperative changes of the proximal ramus segment have been only sparsely investigated in patients with no evident facial asymmetry by using two-dimensional image-based measurement methods. Limited reports of the condylar head movement in a linear direction (≤1 mm) with some extent of rotation have previously been described14,16,17,18,19,20,21. It was also shown that the condylar angle changes in all three rotational planes after skeletofacial surgery17,22,23,24,25,26, indirectly indicating that the position of the proximal ramus segment was altered, and rotation had occurred. Moreover, this postoperative rotation could produce temporomandibular (TMJ) disorders27,28.
The establishment of 3D technology-based quantitative data related to the rotation of the proximal ramus segment after surgery may provide helpful information for multidisciplinary teams (dentists, orthodontists, oral surgeons, maxillofacial surgeons, ear, nose and throat surgeons, head and neck surgeons, and plastic surgeons) in surgical planning and execution. The purpose of this 3D computer-assisted study is to measure the postoperative rotation of the proximal ramus segment in a sample of patients with facial deformity managed with two-jaw surgery, using the BSSO mandible setback technique with bicortical screws-based rigid fixation and no postoperative intermaxillary immobilization.
Results
Proximal segment rotation measurement
On average, the right and left mandible sides and overall proximal ramus segments had a postoperative rotation of 4.1° each in pitch and 3.3°, 2.4°, and 2.8° in roll, and 3.0°, 2.3°, and 2.7° in yaw directions, respectively. On T0 versus T1 comparative analyses, significant differences (all p < 0.05) were observed for all three types of proximal segment rotations in the right and left sides and overall proximal ramus segments (Table 1). The proximal segment plane (PSP) presented more angle reduction in pitch and roll directions, and more angle increase in yaw direction (Table 1). The intra-examiner reliability was excellent (ICC = 0.904–0.982) for all landmark localizations and measurements (Table 2).
Skeletofacial surgery-related complaints and complications
Fifty-five percent of patients presented with chin or lip numbness at 1-month postsurgery, with full recovery at long-term evaluations. Two patients had hypersensitivity over the chin area 1 year after surgery. One patient had bloody discharge and wound infection which was successfully controlled by antibiotics (Table 3). For TMJ-related conditions, all patients were asymptomatic before surgery. Eighty-seven percent of patients had mouth opening limitation (<4 cm) at 1-month postsurgery, with satisfactory interincisal mouth opening achieved between 6 and 12 months after surgery. One patient reported TMJ soreness during the first 6 months postsurgery (Table 3) but the clinical and radiographic examinations showed no positive findings. All patients were satisfied with the results, with no request or indication for revisionary surgery in this cohort (Figs 1 and 2).
(Left) Preoperative and (right) postoperative cone-beam computed tomography-based craniofacial images of same patient as in Fig. 1. Postoperative measurement of the rotation showed 4.5° and 3.8° in pitch, 3.6° and 7.4° in roll, and 4.4° and 4.9° in yaw on her right and left planes of proximal segment (PSPs), respectively.
Discussion
The orthodontic-surgical technical details (virtual planning, modified surgery-first approach, single splint technique, two-jaw surgery and genioplasty, and with no postoperative intermaxillary immobilization) adopted in this study have been beneficial not only for correction of the occlusal function, but also to achieve facial symmetry, balance, proportion, and improved aesthetics in successive cohorts of skeletofacial surgery-treated patients at our center in recent years11,12,29,30,31,32,33,34,35,36,37,38,39,40. For the particular planning and execution of facial asymmetry correction, 3D simulation helps to demonstrate the rotation of both proximal and distal ramus segments with maintenance of intersegmental space and angulation between proximal and distal segments to achieve the desired facial symmetry. The postoperative amount of this rotation had not been sufficiently investigated to date.
In the current investigation, the extent of rotation of the proximal ramus segment in pitch, yaw, and roll directions was measured by employing a 3D computer-based proximal ramus-specific plane process with a mixed landmark and best-fist method in patients who had visible facial asymmetry with occlusal cant and chin deviation. For this, the difference of the PSP-related points between pre- and post-surgery mandible models was based on integrated 3D models of T0 and T1 (pre- and post-surgery, respectively) by using the surface best-fit method (superimposed on forehead and orbital areas). Before the proximal ramus rotation-related data collection, the precision of this superimposition was ascertained in the upper skeletofacial framework which had no influence of surgery by the color map and root-mean-square deviation (RMSD) tools. Color map- and RMSD-related values and reliability tests revealed that the virtual-guided data collection was accurately and consistently performed. This study contributes to literature by demonstrating that the rotation of the proximal ramus segment in a range within 10° for each of the three directions has resulted not only in the achievement of the desired facial symmetry with no need for revisionary surgery, but also in successful functional results with no compromise of the occlusion and TMJ function, as revealed in long term follow-up evaluations after debonding. This was attained by using a BSSO mandible setback approach along with a three bicortical screws-based rigid fixation technique, with no need of intermaxillary immobilization postsurgery, attenuating the overall mouth open restriction-related stress for patients and their parents during the postoperative period as well as improving wound care with intensive oral hygiene started immediately after anesthetic recovery.
In the relevant literature, direct or indirect rotational changes of the ramus after skeletofacial surgery in patients with skeletal class III and facial asymmetry are also reported5,6,13,14, but differences in sample composition (inclusion of patients with no facial asymmetry), surgical techniques (BSSO and IVRO), and measuring tools (cephalometric- or condyle-based methods) impair a truthful head-to-head comparison between the existing findings and our current results5,6,13,14. Cephalometric- and condyle-based quantitative data might indirectly show the rotation of the proximal ramus segment but it does not provide accurate information to help the decision-making process in the planning and execution of ramus mobilization in the three potential directions as a need-based maneuver to improve facial contour symmetry. The current 3D-based proximal segment-specific numerical findings may therefore act as a reference for preoperative planning and intraoperative guiding of rotational changes of the proximal ramus segment to achieve a balanced occlusion and TMJ functional and facial symmetric result, with no long-term TMJ-related signs and symptoms.
When planning and treating facial asymmetry, yaw rotation of the maxillomandibular complex was frequently performed in order to reach facial symmetry and avoid bony collision9,10,39,40. The roll rotation (medial-lateral movement) of the proximal ramus segment was performed accordingly, but some limitation on yaw rotation in the proximal segment was attempted during the bicortical screw fixation. For such yaw rotation, we showed an average 2.7° absolute difference, with the overall proximal ramus segments showing a mean increase of 1.4° after surgery (10.9 for T0 vs. 12.3 for T1). Evaluating the roll rotation after BSSO for treatment of facial asymmetry, a previous study found a mean change of 1.5° in medial movement19. From our findings, the average change was of 1.6° (81.7 vs. 80.1) in medial rotation for overall proximal ramus segments, with values ranging from 5.0° to −8.8° for lateral and medial rotations, respectively. Particularly for managing patients with prominent facial deviation, roll rotation of the proximal ramus was a key step in order to achieve cheek and contour symmetry (Video S1). In this situation, it was common that one side of ramus was moved inward and the other side moved outward.
It is controversial whether the pitch clockwise rotation of the proximal ramus segment could increase the relapse in BSSO-based mandibular setback, with positive41,42 and negative21,43 correlations being reported. Appraising pitch rotation of the proximal segment using a condyle-based sagittal view method, another group reported a significantly decreased angle (counterclockwise rotation) with a mean of 2.32° after BSSO mandibular setback2. We demonstrated similar findings for mean changes with right and left mandible sides presenting 1.5° (72.1 versus 70.6) and 1.7° (72.1 versus 70.4) in counterclockwise pitch rotation, respectively. Additionally, our data also show that the pitch-related values ranged from 7.8° in counterclockwise to 6.9° in clockwise rotations for overall proximal segments, with clinically acceptable occlusal status in the 1-year follow-up after debonding. Perhaps multiple factors are involved in mandibular stability after BSSO setback, rather than just the pitch rotation in the proximal ramus segment44,45.
In contrast to previous studies, we used absolute difference values to show the rotation on the proximal ramus segment after skeletofacial surgery, with the average of 4.1°, 2.8°, and 2.7° in pitch, roll, and yaw rotations for overall proximal segments, respectively (Table 1). The range of rotation angle indicated the tolerance of movement without creating clinical problems in occlusion, TMJ, and facial contour parameters. From previous BSSO-based recommendations for surgical simulation, the proximal ramus segment rotation should be manipulated within 4° and 3° in pitch and roll directions, respectively6. Our overall findings support this prior reference guide, but for patients with severe facial asymmetry, the clinically acceptable tolerance to additional rotational changes was also observed. These ranging, values-related findings may be specifically valuable for multidisciplinary teams managing difficult clinical scenarios such as malocclusion associated with severe facial asymmetry.
The most frequent postoperative complaints and complications in our patients were numbness and limitation in mouth opening, which resolved in 6 to 12 months postsurgery (Table 3). These are to be expected after skeletofacial surgery, but these clinical repercussions should always be attenuated by surgical maneuvers and postoperative care37,46,47. Other TMJ-related concerns were uncommon in our cohort, supporting a former report21. While the patient-centered outcome of the presence of TMJ-related symptoms and signs is a useful and relevant outcome measure21,37,46,47, further studies may expand the current findings by inclusion of objective evaluations.
Limitations of this study include inherent bias associated with a non-comparative retrospective design. We included different degrees of facial asymmetry, but the full spectrum of potential conditions was not addressed. It was restricted to nonsyndromic young adult patients with class III malocclusion, as it reflects our skeletofacial surgery population11,12,30,31,32,33,34. The potential translational displacement of condylar head was considered minimal and disregarded in our study. Reports have described a condyle move of 0.36 mm inferiorly and 0.03–0.58 mm anteriorly after BSSO mandible setback16,19. In our study, the condyle was consistently returned into the glenoid fossa before rigid fixation. A trivial condylar displacement could happen, but the movement was not determinant in causing clinical repercussions such as postoperative TMJ-related symptoms and malfunctioning, malocclusion, or residual facial asymmetry. Further investigation may address this issue by applying our 3D cone beam computed tomography (CBCT) image-based method for proximal ramus segment plane-specific measurements alongside the condyle-based measurement method. The exact cut off point for rotation of the proximal ramus segment according to each particular type of facial asymmetry may also be further investigated to create a patient-specific skeletofacial surgery approach.
In conclusion, this study provides 3D-based measurements of rotational changes of the proximal ramus segment in patients with facial asymmetry and class III malocclusion, with acceptable TMJ and occlusion functional and facial symmetric results.
Patients and Methods
Study population
This Institutional Review Board-approved (Chang Gung Medical Foundation, protocol 103–2822 B) retrospective study recruited consecutive patients with facial deformity (developmental facial asymmetry and class III malocclusion) who underwent orthodontic treatment and orthognathic surgery by the two senior authors (C.-T.H. and L.-J.L.) at the Chang Gung Craniofacial Research Center between July 2014 and July 2017. All experiments and the study methods were carried out in accordance with the approved guidelines of Institutional Review Board. Written informed consents were obtained from the patients or the guardians of the patients younger than 20 years and image release forms for clinical pictures were obtained accordingly for all patients displayed in this publication.
Demographic, clinical, surgical, and outcome data were collected. Patients were excluded if they had cleft or associated syndromes, had a history of facial surgery, did not undergo adequate 3D imaging, or did not complete the follow-up observation (<12 months after debonding).
The included sample comprised 17 women and 14 men with a mean age of 21.4 years. In clinical evaluation, all 31 patients had a concave facial profile, paranasal depression, and protruding mandible with deviation. Radiographic images revealed a class III skeletal relationship, a negative ANB angle, and negative overjet (Table 4). Facial asymmetry was visible and characterized by occlusal plane canting, a discrepancy between the upper and lower dental midlines, cheek asymmetry, and chin deviation with menton at least 4 mm away from the facial midline48.
Surgical treatment approach
All the included patients received single-splint two-jaw surgery with or without genioplasty according to the previously described CBCT-guided virtual surgical planning (Dolphin 3D software, Dolphin Imaging & Management Solutions, California, USA) and surgical approach principles11,12,30,31,32,33,34. In this center, standard CBCT scans have been performed 2 weeks preoperatively for accurate diagnostic evaluation and surgical planning and 1 month postoperatively for assessment of surgical skeletal changes, which act as guidance for postoperative patient-specific orthodontic-surgical care. Presurgical orthodontic treatment was performed for arch form compatibility and took 6.5 ± 3.2 months, including leveling, alignment, arch coordination, and dental decompensation. The orthodontic treatment continued after surgery.
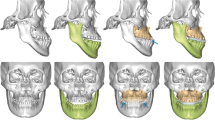
To transfer the 3D planning to actual surgery (Figs 3 and 4), measurements in maxillary pillars bilaterally, face bow-based midline checking (nasal dorsum and tip, lips, maxilla, dental arches, and chin areas), and middle and lower facial third proportions judgments were used as reference. The splitting of BSSO was carefully accomplished to avoid injury to the inferior alveolar nerve (Fig. 3). The maxillomandibular complex with final surgical splint was moved to the desired position (Fig. 4). After Le Fort I fixation with miniplates and screws, the proximal ramus segment was placed in a relaxed position and gently pushed up to ensure the position of the condylar head in the glenoid fossa. Using the 3D simulated image as a guiding template, the desired relationship between the proximal and distal segments was achieved. Percutaneous insertion of 3 bicortical screws 14–16 mm long was performed in the ramus. No interpositional bone graft was used in procedures requiring maintenance of intersegmental gaps. Intermaxillary fixation was released and the occlusion was evaluated. Genioplasty was finally executed as planned, along with intraoperative judgement.
Single-splint two-jaw orthognathic surgery-based skeletofacial reconstruction principle. (a) Both maxilla (Le Fort I segment) and mandible (two proximal ramus segments and one distal segment) were completely osteotomized, fixed in the final occlusion (surgical occlusion splint), and moved as an integrated “maxillo-mandibular complex” (MMC) to the 3D-simulated position. To transfer the virtual simulation to actual surgery, the MMC was moved in six potential directions, including pitch, roll, and yaw rotations (blue arrows) and en-bloc linear horizontal (left or right shifts and advancements or setbacks in the antero-posterior direction) and vertical (extrusion or intrusion) movements (green arrows).
A modified Obwegeser-Dal Pont bilateral sagittal split osteotomy (BSSO) technique was adopted in all included patients. After lingual and buccal corticotomies (3-mm spherical bur and Lindeman side-cutting bur) and sagittal osteotomy (reciprocating saw), a Dautrey osteotome was passed beyond the location of inferior alveolar nerve under direct visualization through anterior opening and driven to complete the splitting of the mandibular ramus.
3D image acquisition
Preoperative (2 weeks before surgery, T0) and postoperative (1 month after surgery, T1) 3D maxillofacial images were acquired using an i-CAT CBCT scanner (Imaging Sciences International, Hatfield, PA, USA) with a low-dose protocol and patient teeth under a light contact condition (120 kV, 5 mA, and 50 Hz). The extended field of view was 22 (height) × 16 (depth) cm, scanning time was 40 s, and voxel size was 0.4 × 0.4 × 0.4 mm. 3D mandible study models were processed and analyzed using the SimPlant O&O software program (Materialize, Leuven, Belgium). By using the standard segmentation function, the skull and the bilateral proximal segments of ramus were outlined.
Anatomical landmarks identification and selection
A threshold segmentation was used for CBCT-based 3D model reconstruction obtained from DICOM (Digital Imaging and Communications in Medicine) files by identifying and delineating the anatomic structures of interest in the CBCT-derived image. The threshold was chosen by an experienced health bioinformatics specialist, and the same skeletofacial landmarks were identified twice, namely on the 3D model and in each slice (for a practical example refer to Supplementary Fig. S1). The distance between the same landmarks on the 3D model and in each slice was then calculated to check the right threshold value that secures the landmarks identification later on (Supplementary Fig. S2). For the tip of coronoid process (TCR) point identification and selection, we adopted the surface of CBCT-based 3D model with an interactive checking of the grayscale in each sliced image (Supplementary Fig. S3). It was initially performed in T0 models and then transferred to T1 models by the best-fit method for identifying the exact same TCR point.
Defining the plane for proximal segment
In order to consistently measure the rotation of the proximal ramus segment in both T0 and T1 mandible models, a representing plane should be created. For this, Frankfurt horizontal plane (FHP)35, TCR point, and the deepest point in the sigmoid notch (DSN) were demarcated (Table 5). Using these reference plane and points, two further landmark points (PR1 and PR2) which were not influenced by the BSSO in ramus were defined on the posterior side of the proximal ramus segment (Fig. 5). A consistent reference plane representing the proximal segment (PSP) of ramus was then defined by PR1, PR2, and DSN points (Fig. 5, Table 5).
Designing the representing plane for proximal ramus segment. Landmarks showed the tip of coronoid process (TCR), deepest point of sigmoid notch (DSN), PR1, and PR2 (definitions in Table 5). The plane of proximal segment (PSP) was defined by PR1, PR2, and DSN points. FH plane means Frankfurt horizontal plane.
Proximal segment rotation measurement
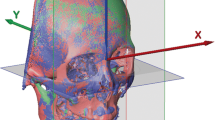
To compare the positional differences of the proximal ramus segment between T0 and T1, image registration and superimposition of the forehead and orbital areas (non-operated parts) were performed using the best-fit method (Figs 6–8). Accuracy of the registration was verified by checking the distance color map (Geomagic 3D software, 3D Systems, Rock Hill, SC, USA) and RMSD (3dMD Vultus software, 3dMD LLC, Atlanta, USA) between the T0 and T1 images, with green color (Fig. 7) and value ≤0.5 mm (Fig. 8) considered acceptable to ensure that the corresponding reference areas had maximum precision31,36. After the registration, the FHP and midsagittal plane (MSP, Table 5) were employed on the skull model for comparisons (Fig. 9). To measure the change in the proximal ramus segment before and after skeletofacial surgery, the same coordinate system was applied for both T0 and T1 mandible models. The PSP in the T0 image was created and transferred to the corresponding position in the T1 image. Thereafter, the two PSPs were used to measure the angular differences by using SimPlant O&O software (Figs 10–14). The PSP reference plane representing the proximal segment was examined for its postoperative rotation in pitch, roll and yaw directions (Table 5) in the right and left sides (n = 31) and overall proximal ramus segments (n = 62). Using ten randomly selected patients (20 mandible sides), the same examiner repeated all landmark localizations and measurements per axis (x, y, and z) in an interval of 2 weeks for error assessment.
T0 preoperative and T1 postoperative images of same clinical example as in Fig. 4. (Left) T0 and T1 images were superimposed on frontal and supraorbital bone. (Right) The color map indicated accurate registration of the two models on frontal and supraorbital bone showing the green color. The magnitude of the differences was greater in the lower facial parts, demonstrating the operative change.
Root-mean-square deviation (RMSD) was used to measure the accuracy of image superimposition, with value inferior to 0.5 mm considered acceptable. Same superimposed model as in Fig. 7.
Rotations of right proximal segment in pitch (the anterior-posterior swing of the proximal segment), roll (the medial-lateral swing, or inward-outward movement of the proximal segment), and yaw (the left-right swing, or open-close movement of the proximal segment). Blue and orange colors represent T0 and T1 images, respectively.
The postoperative course
The patients with no intermaxillary fixation were admitted in regular ward for 2 days following the surgery. A liquid diet was advised in the first week, followed by a soft diet in the second week. All included patients were clinically examined for skeletofacial surgery-related complaints and complications based on established surgical and orthodontic appointments (1, 3, and 6 months postsurgery, and at least 1 year after debonding). The patient-centered outcome of the presence of TMJ-related symptoms and signs was also actively screened, including TMJ clicking, tenderness, mouth opening limitation, numbness, muscle tenderness, and headache49. Need for revision surgery was defined as any revisionary bone and/or soft tissue procedure requested or required to improve occlusal, maxillary, mandibular, and/or chin morphology within the follow-up.
Statistical analysis
In the descriptive analysis, the mean was used for metric variables, and percentages were given for categorical variables. The data distribution was verified through the Kolmogorov-Smirnov test, and the paired t-test was adopted for statistical comparisons. Intra-examiner reliability was analyzed with intraclass correlation coefficients (ICCs) based on absolute agreement definition. Two-sided values of p < 0.05 were considered statistically significant. All analyses were performed using SPSS Version 19.0 (IBM Corp., Armonk, NY, USA).
References
Lonic, D., Sundoro, A., Lin, H. H., Lin, P. J. & Lo, L. J. Selection of a horizontal reference plane in 3D evaluation: Identifying facial asymmetry and occlusal cant in orthognathic surgery planning. Sci Rep 7, 2157 (2017).
Chin, Y. P. et al. The pterygomaxillary junction: An imaging study for surgical information of LeFort I osteotomy. Sci Rep 7, 9953 (2017).
Bergeron, L., Yu, C. C. & Chen, Y. R. Single-splint technique for correction of severe facial asymmetry: correlation between intraoperative maxillomandibular complex roll and restoration of mouth symmetry. Plast Reconstr Surg 122, 1535–41 (2008).
Cheong, Y. W. & Lo, L. J. Facial asymmetry: etiology. evaluation, and management. Chang Gung Med J 34, 341–351 (2011).
Xia, J. J., Gateno, J. & Teichgraeber, J. F. New clinical protocol to evaluate craniomaxillofacial deformity and plan surgical correction. J Oral Maxillofac Surg 67, 2093–2106 (2009).
Liu, Z., Shen, S., Xia, J. J. & Wang, X. A modified method of proximal segment alignment after sagittal split ramus osteotomy for patients with mandibular asymmetry. J Oral Maxillofac Surg 73, 2399–2407 (2015).
Wu, R. T., Wilson, A. T., Gary, S. & Steinbacher, D. M. Complete reoperation in orthognathic surgery. Plast Reconstr Surg 143, 1053e–1059e (2019).
Iorio, M. L., Masden, D., Blake, C. A. & Baker, S. B. Presurgical planning and time efficiency in orthognathic surgery: The use of computer-assisted surgical simulation. Plast Reconstr Surg 128, 179e–181e (2011).
Udomlarptham, N., Lin, C. H., Wang, Y. C. & Ko, E. W. Does two-dimensional vs. three-dimensional surgical simulation produce better surgical outcomes among patients with class III facial asymmetry? Int J Oral Maxillofac Surg 47, 1022–1031 (2018).
Ko, E. W., Lin, C. H., Chen, Y. A. & Chen, Y. R. Enhanced surgical outcomes in patients with skeletal class III facial asymmetry by 3-dimensional surgical simulation. J Oral Maxillofac Surg 76, 1073–1083 (2018).
Wu, T. Y., Lin, H. H., Lo, L. J. & Ho, C. T. Postoperative outcomes of two- and three-dimensional planning in orthognathic surgery: A comparative study. J Plast Reconstr Aesthet Surg. 70, 1101–1111 (2017).
Lin, H. H., Chang, H. W., Wang, C. H., Kim, S. G. & Lo, L. J. Three-dimensional computer-assisted orthognathic surgery: experience of 37 patients. Ann Plast Surg 74, S118–126 (2015).
Kim, S. J., Lee, K. J., Yu, H. S., Jung, Y. S. & Baik, H. S. Three-dimensional effect of pitch, roll, and yaw rotations on maxillomandibular complex movement. J Craniomaxillofac Surg 43, 264–273 (2015).
Ohba, S. et al. The three-dimensional assessment of dynamic changes of the proximal segments after intraoral vertical ramus osteotomy. Cranio 33, 276–284 (2015).
Huh, J. W. et al. Three-dimensional changes of proximal segments in facial asymmetry patients after bilateral vertical ramus osteotomy. Int J Oral Maxillofac Surg 15, S0901-5027(18)30156–5 (2018).
Lee, W. & Park, J. U. Three-dimensional evaluation of positional change of the condyle. after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94, 305–309 (2002).
Becktor, J. P. et al. Transverse displacement of the proximal segment after bilateral sagittal osteotomy. J Oral Maxillofac Surg 60, 395–403 (2002).
Kim, Y. I., Cho, B. H., Jung, Y. H., Son, W. S. & Park, S. B. Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111, 681–687 (2011).
Kim, J. W., Son, W. S., Kim, S. S. & Kim, Y. I. Proximal segment changes after bilateral sagittal split ramus osteotomy in facial asymmetry patients. J Oral Maxillofac Surg 73, 1592–1605 (2015).
Ohba, S. et al. Physiological positioning strategy alters condylar position after mandibular ramus sagittal split osteotomies for mandibular prognathism. Cranio 36, 181–188 (2018).
Choi, B. J. et al. Correlation between intraoperative proximal segment rotation and post-sagittal split ramus osteotomy relapse: a three-dimensional cone beam computed tomography study. Int J Oral Maxillofac Surg 47, 613–621 (2018).
Alder, M. E. et al. Short-term changes of condylar position after sagittal split osteotomy for mandibular advancement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87, 159–165 (1999).
Harris, M. D., Van Sickels, J. E. & Alder, M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J Oral Maxillofac Surg 57, 650–654 (1999).
Stroster, T. G. & Pangrazio-Kulbersh, V. Assessment of condylar position following bilateral sagittal split ramus osteotomy with wire fixation or rigid fixation. Int J Adult Orthodon Orthognath Surg 9, 55–63 (1994).
Schultes, G., Gaggl, A. & Karcher, H. Changes in the dimensions of milled mandibular models after mandibular sagittal split osteotomies. Br J Oral Maxillofac Surg 36, 196–201 (1998).
Ohba, S. et al. Short lingual osteotomy without fixation: a new strategy for mandibular osteotomy known as “physiological positioning”. Br J Oral Maxillofac Surg 52, e9–e13 (2014).
Yamada, K., Hanada, K., Hayashi, T. & Ito, J. Condylar bony change, disk displacement, and signs and symptoms of TMJ disorders in orthognathic surgery patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91, 603–610 (2001).
Hu, J., Wang, D. & Zou, S. Effects of mandibular setback on the temporomandibular joint: a comparison of oblique and sagittal split ramus osteotomy. J Oral Maxillofac Surg 58, 375–380 (2000).
Denadai, R. et al. Facial Appearance and psychosocial features in orthognathic surgery: A FACE-Q- and 3D facial image-based comparative study of patient-, clinician-, and lay-observer-reported outcomes. J Clin Med 8, E909 (2019).
Chortrakarnkij, P. et al. A modified technique of mandibular ramus sagittal split osteotomy for prevention of inferior alveolar nerve injury: A prospective cohort study and outcome assessment. Ann Plast Surg 78, S108–116 (2017).
Ho, C. T., Lin, H. H. & Lo, L. J. Intraoral scanning and setting up the digital final occlusion in 3D planning of orthognathic surgery: Its comparison with the dental model approach. Plast Reconstr Surg 143, 1027e–1036e (2019).
Ho, C. T., Lin, H. H., Liou, E. J. W. & Lo, L. J. Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: A qualitative and quantitative study. Sci Rep 7, 40423 (2017).
Liou, E. J. et al. Surgery-first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg 69, 781–785 (2011).
Huang, C. S. & Chen, Y. R. Orthodontic principles and guidelines for the surgery-first approach to orthognathic surgery. Int J Oral Maxillofac Surg 44, 1457–1462 (2015).
Lin, H. H., Chuang, Y. F., Weng, J. L. & Lo, L. J. Comparative validity and reproducibility study of various landmark-oriented reference planes in 3-dimensional computed tomographic analysis for patients receiving orthognathic surgery. PLoS One 10, e0117604 (2015).
Lo, L. J., Weng, J. L., Ho, C. T. & Lin, H. H. Three-dimensional region-based study on the relationship between soft and hard tissue changes after orthognathic surgery in patients with prognathism. PLoS One 13, e0200589 (2018).
Chortrakarnkij, P., Lonic, D., Lin, H. H. & Lo, L. J. Establishment of a reliable horizontal reference plane for 3-dimensional facial soft tissue evaluation before and after orthognathic surgery. Ann Plast Surg 78, S139–S147 (2017).
Ko, E. W., Huang, C. S. & Chen, Y. R. Characteristics and corrective outcome of face asymmetry by orthognathic surgery. J Oral Maxillofac Surg 67, 2201–2209 (2009).
Lonic, D. et al. Computer-assisted orthognathic surgery for patients with cleft lip/palate: From traditional planning to three-dimensional surgical simulation. PLoS One 11, e0152014 (2016).
Yamaguchi, K., Lonic, D., Ko, E. W. C. & Lo, L. J. An integrated surgical protocol for adult patients with hemifacial microsomia: Methods and outcome. PLoS One 12, e0177223 (2017).
Yang, H. J. & Hwang, S. J. Contributing factors to intraoperative clockwise rotation of the proximal segment as a relapse factor after mandibular setback with sagittal split ramus osteotomy. J Craniomaxillofac Surg 42, e57–63 (2014).
Kim, Y. K. Complications associated with orthognathic surgery. J Korean Assoc Oral Maxillofac Surg 43, 3–15 (2017).
Mobarak, K. A., Krogstad, O., Espeland, L. & Lyberg, T. Long-term stability of mandibular setback surgery: a follow-up of 80 bilateral sagittal split osteotomy patients. Int J Adult Orthodon Orthognath Surg 15, 83–95 (2000).
Mucedero, M., Coviello, A., Baccetti, T., Franchi, L. & Cozza, P. Stability factors after double-jaw surgery in Class III malocclusion. A systematic review. Angle Orthod 78, 1141–1152 (2008).
Beukes, J., Reyneke, J. P. & Becker, P. J. Medial pterygoid muscle and stylomandibular ligament: the effects on postoperative stability. Int J Oral Maxillofac Surg 42, 43–48 (2013).
Jung, H. D., Kim, S. Y., Park, H. S. & Jung, Y. S. Orthognathic surgery and temporomandibular joint symptoms. Maxillofac Plast Reconstr Surg 37, 14 (2015).
Jędrzejewski, M., Smektała, T., Sporniak-Tutak, K. & Olszewski, R. Preoperative, intraoperative, and postoperative complications in orthognathic surgery: a systematic review. Clin Oral Investig 19, 969–977 (2015).
Haraguchi, S., Takada, K. & Yasuda, Y. Facial asymmetry in subjects with skeletal class III deformity. Angle Orthod 72, 28–35 (2002).
Yamaguchi, K., Lonic, D. & Lo, L. J. Complications following orthognathic surgery for patients with cleft lip/palate: A systematic review. J Formos Med Assoc 115, 269–277 (2016).
Acknowledgements
We thank Lien-Shing Niu and Yi-Tan Hung for data collection. The study was supported by a grant from the Ministry of Science and Technology (MOST 107-2622-E-182-001-CC2).
Author information
Authors and Affiliations
Contributions
Conceptualization, T.-Y.W. and H.-H.L.; formal analysis, T.-Y.W. and H.-H.L.; investigation, T.-Y.W. and H.-H.L.; data curation, T.-Y.W., H.-H.L. and R.D.; writing—original draft preparation, T.-Y.W. and R.D.; writing—review and editing, C.-T.H. and L.-J.L.; supervision, C.-T.H. and L.-J.L.; resources, L.-J.L.; project administration, L.-J.L.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, TY., Denadai, R., Lin, HH. et al. The outcome of skeletofacial reconstruction with mandibular rotation for management of asymmetric skeletal class III deformity: A three-dimensional computer-assisted investigation. Sci Rep 9, 13337 (2019). https://doi.org/10.1038/s41598-019-49946-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-49946-9
- Springer Nature Limited