Abstract
Patients with previous diabetic foot ulcer are prone to re-ulceration and (re)amputation, to various comorbidities, have significantly impaired quality of life and increased mortality. We aimed to evaluate the risk of foot related complications and mortality in a high-risk population of patients with healed diabetic foot syndrome over a decade. 91 patients with recently healed diabetic foot ulcer were invited for follow-up at 1, 6 and 11 years after inclusion. Patient characteristics at inclusion were: 40 women, 65 ± 11 years, diabetes type 1 (n = 6) or 2 (n = 85), BMI 28.5 ± 4.4 kg/m2, and HbA1c 68 ± 17 mmol/mol. Comorbidities included neuropathy (n = 91), peripheral artery disease (PAD), history of minor (n = 25) or major (n = 5, 5.5%) amputation, nephropathy (n = 40) and retinopathy (n = 53). Ulceration recurred in 71 (65%) patients, time to first recurrence was 1.8 ± 2.4 years (mean ± SD). 21 patients had to undergo (re)amputation (minor n = 19, major n = 2), time to amputation was 3.6 ± 1.9 years. Over time, 3 further major amputations were required in patients with an initial minor amputation. Thirty-three (36%) of the initially included patients completed the follow-up period of 11.0 ± 0.6 years. 58 patients (64%) died during the observational period, time to death was 5 ± 3 years in this group. We found overall high mortality of 64% throughout the follow-up period of 11 years in high-risk patients with healed diabetic foot syndrome. Presence of PAD, prior amputation and nephropathy as well as poor glycemic control were significantly predictive for death.
Similar content being viewed by others
Introduction
Diabetic foot syndrome (DFS) is a late complication in both patients with type 1 and type 2 diabetes mellitus with a prevalence of 4 to 10%. The lifetime risk of patients with diabetes mellitus to develop DFS is as high as 25%1,2,3. Patients with DFS are two to three times more likely to die than patients without DFS4,5,6,7,8.
Patients with DFS are predisposed to various comorbidities, such as peripheral artery disease (PAD), cardiovascular disease (CVD), neuropathy, retinopathy, and nephropathy, and have significantly impaired quality of life3,9,10,11,12. Wound healing of diabetic ulcers is often a long process requiring substantial resources of health care systems13. Even after accomplished wound healing, reulcerations occur frequently and commonly lead to minor or major amputation of lower extremities14,15.
Several studies to evaluate outcomes in patients with DFS exist4,5,14,15,16,17,18, but data on the outcome of patients with healed diabetic foot ulcer are limited. We therefore aimed to investigate the risk of foot related complications, comorbidities and mortality in a high-risk population of patients with healed DFS over a time period of 11 years.
Patients and Methods
Study design and patients
Between May 2000 and September 2001, patients with type 1 and type 2 diabetes and recently healed diabetic foot ulcer who presented at the diabetes foot clinic of the Medical University of Graz were invited to participate in the study. Two patients did not consent for personal reasons; 91 were consecutively included in the study. The population of 91 patients was initially randomized to monthly chiropodist care vs. standard foot care program for 12 months. Thereafter routine care was continued in both groups. Patients were followed up 1, 6 and 11 years after inclusion or until death. There was no drop-out or patient lost to follow-up. The following assessments were performed during all follow-up visits: medical history included type, duration and treatment of diabetes, macro- and microvascular comorbidities, amputations of lower limbs and smoker status. Physical examination of the feet included the assessment of peripheral neuropathy, peripheral arterial disease (PAD), recent (re)amputations and (re)ulcerations. Laboratory assessments included HbA1c, creatinine and microalbuminuria. Screening for diabetic retinopathy was performed by an ophthalmologist and data from patient letters were transcribed. The methods and definitions are described in detail elsewhere17. Initial visit and follow-up visits were performed by a diabetes specialist and a diabetes nurse. Between study visits regular diabetes or diabetic foot related care was provided to the patients either at Medical University of Graz, at other clinics or at the family doctor as preferred by the patients. Intervals of these appointment was at the discretion of the treating physician.
The study was approved by ethics committee of Medical University of Graz and performed in accordance with the principles of Good Clinical Practice and the Declaration of Helsinki. All participants gave written informed consent prior to any study related activities. The study was retrospectively registered at the German Clinical Trials Register (DRKS00015224).
Statistical analysis
We performed the statistical analysis in SAS 9.2 and STATA 15.1. In all variables, data with the response ‘unknown’ were treated as missing.
We tabulated descriptive statistics as mean ± standard deviation (SD) if not indicated otherwise. We conducted logistic regression analysis to identify significant predictors of amputation and mortality. We used stepwise regression backward selection method and ‘gvselect’ program of stata to select significant predictors. The results of multiple logistic regression were reported in terms of adjusted odds ratios (AOR) with corresponding 95% confidence intervals (CI) and p-values. We excluded ‘type of diabetes’, ‘stroke’. ‘myocardial infarction’, and ‘body mass index (kg/m2)’ from the final logistic regression model because of high collinearity between these variables. We generated Kaplan-Meier curves for ‘gender’ and other significant predictors to assess time to amputation and mortality, respectively. We did not adjust for multiple comparisons.
Prior presentation of data
Parts of this study were presented at the American Diabetes Association’s 75th Scientific Session, Boston, 5–8 June 2015 and the 51st Annual Meeting of the European Association of for the Study of Diabetes, Stockholm, Sweden, 13–18 September 2015.
Results
Patient characteristics at baseline are indicated in Table 1. During the follow-up period of 11.0 ± 0.6 years, ulceration recurred in 71 patients of the initially included 91 patients. Time to first recurrence was 1.8 ± 2.4 years. Subsequent ulcers after initial reulceration occurred in 35 cases on the same foot and in 37 cases in both feet during the observation period. 21 patients had to undergo (re)amputation during follow-up (minor n = 19, major n = 2), time to amputation was 3.6 ± 1.9 years. Over the follow-up period, 3 consecutive major amputations were required in patients with an initial minor amputation. 58 patients (63.7%) died during the observational period; mean time to death was 5 ± 3 years in this group. Causes of death were cardiovascular (62.1%), infectious (20.7%), malignant (6.9%) or renal (1.7%) disease. Two of the fatal infections were due to DFS. One (1.7%) of the 58 deceased patients committed suicide. Cause of death was unknown for 6.9% of the cohort.
Predictors for mortality
In the regression model for death with the predictors PAD, previous amputations, HbA1c, nephropathy as well as the control variable age were significant predictors for death. The odds ratios, confidence intervals (CI), and p-values for all tested variables are indicated in Table 2.
Predictors for amputation
The regression model for amputation yielded significant results for the predictor retinopathy and the control variable age. The other factors, including gender, insulin therapy, PAD, CVD, smoking, nephropathy, BMI and HbA1c > 58 mmol/mol were not associated with an increased risk of amputation. Initial treatment allocation (monthly chiropodist vs. standard care) also did not affect amputation risk. The odds ratios, confidence intervals, and p-values for all tested variables are indicated in Table 2. The presence of nephropathy was associated a lower risk for amputations.
Factors associated with survival and amputation
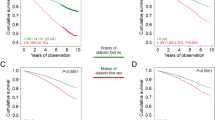
Figure 1 displays the Kaplan-Meier curves for survival and amputation. Overall survival probabilities and survival probabilities with respect to gender, peripheral artery disease (PAD) status, nephropathy and HbA1c were assessed. Additionally, overall risk of amputation and risk of amputation in relation to gender and retinopathy status were investigated. Survival probability for all patients after 11 years of follow-up was 36%, highly irrespective of gender (females: 32.5%, males: 39.2%; see Fig. 1A,B). In contrast, PAD status significantly influenced the survival probability of the patients. Patients without PAD had a survival probability after 11 years of follow-up of about 57.8%, whereas survival probability was only 13.6% for patients with PAD (Fig. 1C). Good glycemic control at inclusion obviously had a legacy effect at 11 years of follow-up: patients with an initial A1c value ≤ 58 mmol/mol had a survival probability of 55%, whereas survival probability for patients with an A1c value > 58 mmol/mol ( > 7.5%) was only 26% (Fig. 1D). The same impact on survival probability was seen for presence of nephropathy (48% for patients without, and about 24% for patients with nephropathy; Fig. 1E).
Kaplan Meier Curves for Survival and Amputation. (A) Overall survival, (B) Survival by gender (female patients - solid line, male patients - dashed line), (C) Survival by peripheral artery disease (PAD) status (no PAD - solid line, PAD - dashed line), (D) Survival by glycemic control (HbA1c < = 58 mmol/mol (solid line) vs. >58 mmol/mol (dashed line)), (E) Survival by nephropathy status (no nephropathy - solid line, nephropathy - dashed line), (F) Survival by previous amputation status (No previous amputation - solid line, minor amputation - dashed line, major amputation - dotted line), (G) Overall amputation rates (H) Amputation by gender (female patients - solid line, male patients - dashed line), (I) Amputation by retinopathy status (no retinopathy - solid line, retinopathy - dashed line).
Overall amputation risk was 23% at 11 years of follow-up; gender was not associated with risk for amputation (females: 20%, males 26%; Fig. 1F,G). Presence of retinopathy increased the risk for future amputations: 30% for patients with retinopathy vs. only 17% for patients without retinopathy (Fig. 1H).
Discussion
The present study followed a cohort of patients with diabetes mellitus and recently healed diabetic foot syndrome for a period of 11 years. Our main focus was to investigate mortality and amputation rates and predisposing factors in this high-risk population. In our population 63.7% died during the observational period, with cardiovascular events (62.1%) being the main cause of death.
Long-term outcomes after ulceration in diabetic patients have been investigated in several studies5,16,18,19 Iversen et al. have observed mortality rates of 49% over a ten-year follow-up period and also in this population events were the main cause of death also in this population (48.7%)5. Apelqvist et al. have reported survival rates of 92%, 73% and 58% for patients with recently healed DFS at 1, 3 and 5 years of observation14. This is in rough agreement with the resulting survival rates of about 95%, 80% and 65% after 1, 3 and 5 years in our investigation.
Iversen et al. have concluded that older age, male sex, lower education, smoking and larger waist circumference were predictive factors for death in patients with DFS5, whereas Morbach et al. have reported higher age, male gender, chronic kidney disease including necessity of dialysis and PAD to be predictive for death16. We investigated the relation of mortality risk and predisposing factors and found that presence of PAD, prior amputations and nephropathy as well as poor glycemic control status significantly predicted fatal events over a period of 11 years. We further investigated predictors for future amputations and identified the presence of retinopathy and age as significant predictors. Interestingly, nephropathy was inversely associated with future risk for amputations, however, this seems to be due to the competing risk of death, an outcome that is significantly increased by the presence of nephropathy.
Individuals with diabetes mellitus have a two-fold higher risk of all-cause and CVD mortality than individuals without diabetes20. Our data indicate annual mortality rates of approximately 6% in patients with diabetic foot syndrome and PAD. This rate is considerably higher than mortality rates reported in recent cardiovascular outcome trials such as EMPA-REG, EXSCEL, LEADER or SUSTAIN. These trials have included mainly subjects with established coronary artery disease and observed annual mortality rates were approximately 2% in such patients considered to be at high-risk for cardiovascular events or death21,22,23,24. However, the population of patients with diabetes and PAD that is at even higher mortality risk is rather underrepresented in current cardiovascular outcome trials so far. Future trials should be designed to better represent this high-risk population and investigate whether they might also benefit from treatment that mitigates cardiovascular risk.
Moreover patients with PAD experience less intensive risk factor management than patients with CVD which might attribute to higher mortality rates in this population25.
We found overall high mortality (64%) throughout the follow-up period of 11 years in patients with healed diabetic foot syndrome. Presence of PAD, prior amputations, nephropathy and poor glycemic control were significantly predictive for death.
Data Availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Singh, N., Armstrong, D. G. & Lipsky, B. A. Preventing foot ulcers in patients with diabetes. JAMA 293, 217–228 (2005).
Walters, D. P., Gatling, W., Mullee, M. A. & Hill, R. D. The distribution and severity of diabetic foot disease: a community study with comparison to a non-diabetic group. Diabet Med 9, 354–358 (1992).
Winkley, K. et al. Five-year follow-up of a cohort of people with their first diabetic foot ulcer: the persistent effect of depression on mortality. Diabetologia 55, 303–310 (2012).
Walsh, J. W., Hoffstad, O. J., Sullivan, M. O. & Margolis, D. J. Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabet Med 33, 1493–1498 (2016).
Iversen, M. M. et al. History of foot ulcer increases mortality among individuals with diabetes: ten-year follow-up of the Nord-Trondelag Health Study, Norway. Diabetes Care 32, 2193–2199 (2009).
Ramsey, S. D. et al. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care 22, 382–387 (1999).
Boyko, E. J., Ahroni, J. H., Smith, D. G. & Davignon, D. Increased mortality associated with diabetic foot ulcer. Diabet Med 13, 967–972 (1996).
Moulik, P. K., Mtonga, R. & Gill, G. V. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care 26, 491–494 (2003).
Vileikyte, L. Diabetic foot ulcers: a quality of life issue. Diabetes Metab Res Rev 17, 246–249 (2001).
Armstrong, D. G., Lavery, L. A., Wrobel, J. S. & Vileikyte, L. Quality of life in healing diabetic wounds: does the end justify the means? J Foot Ankle Surg 47, 278–282 (2008).
Jeffcoate, W. J., Chipchase, S. Y., Ince, P. & Game, F. L. Assessing the outcome of the management of diabetic foot ulcers using ulcer-related and person-related measures. Diabetes Care 29, 1784–1787 (2006).
Wilcox, T., Newman, J. D., Maldonado, T. S., Rockman, C. & Berger, J. S. Peripheral vascular disease risk in diabetic individuals without coronary heart disease. Atherosclerosis (2018).
Boulton, A. J., Vileikyte, L., Ragnarson-Tennvall, G. & Apelqvist, J. The global burden of diabetic foot disease. Lancet 366, 1719–1724 (2005).
Apelqvist, J., Larsson, J. & Agardh, C. D. Long-term prognosis for diabetic patients with foot ulcers. J Intern Med 233, 485–491 (1993).
Larsson, J., Agardh, C. D., Apelqvist, J. & Stenstrom, A. Long-term prognosis after healed amputation in patients with diabetes. Clin Orthop Relat Res, 149–158 (1998).
Morbach, S. et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care 35, 2021–2027 (2012).
Plank, J. et al. Evaluation of the impact of chiropodist care in the secondary prevention of foot ulcerations in diabetic subjects. Diabetes Care 26, 1691–1695 (2003).
Young, M. J., McCardle, J. E., Randall, L. E. & Barclay, J. I. Improved survival of diabetic foot ulcer patients 1995–2008: possible impact of aggressive cardiovascular risk management. Diabetes Care 31, 2143–2147 (2008).
Apelqvist, J., Bakker, K., van Houtum, W. H. & Schaper, N. C., International Working Group on the Diabetic Foot Editorial, B. Practical guidelines on the management and prevention of the diabetic foot: based upon the International Consensus on the Diabetic Foot (2007) Prepared by the International Working Group on the Diabetic Foot. Diabetes Metab Res Rev 24(Suppl 1), S181–187 (2008).
Preis, S. R. et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 119, 1728–1735 (2009).
Zinman, B. et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med 373, 2117–2128 (2015).
Holman, R. R. et al. Effects of Once-Weekly Exenatide on Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 377, 1228–1239 (2017).
Marso, S. P. et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 375, 311–322 (2016).
Marso, S. P. et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 375, 1834–1844 (2016).
Hiatt, W. R. et al. Ticagrelor versus Clopidogrel in Symptomatic Peripheral Artery Disease. N Engl J Med 376, 32–40 (2017).
Acknowledgements
The authors thank the nurses and physicians at the Division of Endocrinology and Diabetology, Medical University of Graz for their contribution in the performance of the study and the participants for their participation.
Author information
Authors and Affiliations
Contributions
J. Mader, W. Haas, F. Aberer, K. Horvath, G. Köhler, M. Pandis, J. Plank, designed and performed the study, interpreted data and contributed to discussions. J. Mader, F. Aberer, H. Sourij and B. B drafted the manuscript. B. Boulgaropoulos contributed to discussions and interpreted data. P. Baumann and F. Aziz performed statistical analysis and contributed to discussions. T. Pieber designed the study and supervised the project. H. Sourij designed the study, interpreted data, contributed to discussions, supervised the project and is the guarantor of this work. All authors critically revised the article and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
J. Mader is a member in the advisory board of Boehringer Ingelheim, Becton-Dickinson, Eli Lilly, Medtronic and sanofi-aventis, received speaker honoraria from Abbott Diabetes Care, Astra Zeneca, Eli Lilly, Nintamed, NovoNordisk A/S, Roche Diabetes Care, sanofi-aventis, Servier and Takeda and is shareholder of decide Clinical Software GmbH. KH received speaker honoraria from NovoNordisk A/S and Novartis. F. Aberer has received speaker honoraria from Astra Zeneca and Boehringer Ingelheim. G. Köhler is advisory board member and on speaker’s bureau of Abbott Diabetes Care, Boehringer Ingelheim, Eli Lilly, NovoNordisk and Sanofi. T. Pieber is an advisory board member of Novo Nordisk A/S, a consultant for Roche Diabetes Care, Novo Nordisk A/S, Eli Lilly & Co, Infineon, Carnegie Bank, on speaker’s bureau of Novo Nordisk A/S and Astra Zeneca and is shareholder of decide Clinical Software GmbH. H. Sourij is an advisory board member and on speaker’s bureau of Amgen, Astra Zeneca, Boehringer Ingelheim, Eli Lilly, MSD, NovoNordisk and Sanofi. H. Sourij received unrestricted research grants from Astra Zeneca, Boehringer Ingelheim, MSD, Novo Nordisk and Sanofi. The remaining authors have no duality of interest to disclose.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mader, J.K., Haas, W., Aberer, F. et al. Patients with healed diabetic foot ulcer represent a cohort at highest risk for future fatal events. Sci Rep 9, 10325 (2019). https://doi.org/10.1038/s41598-019-46961-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-46961-8
- Springer Nature Limited
This article is cited by
-
Independent association of history of diabetic foot with all-cause mortality in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian Multicenter Study
Cardiovascular Diabetology (2024)
-
Management patterns and outcomes of patients hospitalized with diabetic foot ulcers at one tertiary care hospital
Internal and Emergency Medicine (2023)
-
Impact of time in range during hospitalization on clinical outcomes in diabetic patients with toe amputation: a propensity score matching analysis
BMC Surgery (2022)
-
The associations of statin intake and the trabecular bone score and bone mineral density status in elderly Iranian individuals: a cross-sectional analysis of the Bushehr Elderly Health (BEH) program
Archives of Osteoporosis (2021)
-
Angiopoietin-like 2 is a potential biomarker for diabetic foot patients
BMC Endocrine Disorders (2020)