Abstract
Early detection of neuromyelitis optica spectrum disorders (NMOSD), especially after optic neuritis, a presenting manifestation commonly observed also in multiple sclerosis (MS), is crucial for timely treatment and prognosis. Integrated visual pathway assessment with optical coherence tomography (OCT) and visual evoked potentials (VEP) may help in this task, showing in vivo different pathophysiological backgrounds. We evaluated combined VEP and OCT in a cross-sectional, single-centre study assessing 50 consecutive NMOSD patients, 57 MS patients and 52 healthy controls. After optic neuritis, VEP were more frequently absent in NMOSD compared to MS; most NMOSD eyes with recordable VEP showed prolonged latency, but extreme latency delays were less common than in MS. OCT showed predominantly axonal involvement in NMOSD, with 88% eyes (95% CI: 69–97%) displaying retinal nerve fibre layer thickness <60 µm even after first optic neuritis episode. Accuracy of OCT was further enhanced by combination with VEP into a new Z-score derived OCT-VEP index, measuring prevalence of axonal damage or demyelination. Our results suggest that integrated optic nerve assessment may elucidate differences in optic neuritis pathophysiology; conduction slowing with relatively preserved nerve fibre layer suggests MS, while severe neuroaxonal loss after optic neuritis, often hindering VEP response, characterizes NMOSD.
Similar content being viewed by others
Introduction
Recognizing different patterns of damage between neuromyelitis optica spectrum disorders (NMOSD) and multiple sclerosis (MS), especially in patients experiencing optic neuritis (ON), is an important challenge, both for researchers and clinicians, as the two diseases share many clinical and paraclinical features, but differ in critical aspects, first of all prognosis and therapy.
Optical coherence tomography (OCT) studies in NMOSD published since 2008 have shown thinner retinal nerve fibre layer in NMOSD after ON compared to healthy controls1,2,3,4 and compared to MS eyes with history of ON1. In NMOSD eyes without history of ON, however, there are contrasting evidences about OCT involvement, with some studies5,6 showing subclinical abnormalities, but not other ones1,3,7,8.
Visual evoked potentials (VEP) in NMOSD have been less extensively studied to date9,10,11, with just one published study in Caucasian population11. Available results show conflicting evidence about the predominant pattern of VEP involvement in NMOSD patients, whether similar to MS one (with demyelination prevailing on axonal conduction impairment)11 or with specific axonal pattern10. Still to be elucidated is the relationship between functional and structural measures of optic nerve in NMOSD12.
It is known from literature that eyes of MS patients show subclinical RNFL thinning regardless of acute ON events along the course of disease13,14. It is not clear whether NMOSD presents with similar subclinical changes.
The aim of the present study was to explore the value of optic nerve structural and functional metrics, alone or in combination, in characterizing NMOSD and differentiating it from MS, in eyes with and without history of optic neuritis.
Methods
Protocol approval and patient consents
This was a single-centre, observational, cross-sectional study. Participants were recruited from the Department of Neurology of our Institute. The study, approved by San Raffaele Hospital Scientific Institute Ethical Committee, followed the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Participants
The participants in the study consisted of 50 consecutive patients with NMOSD, referring to our centre between December 2013 and May 2015, 57 patients with MS randomly selected from our MS centre population, matched for optic neuritis (ON) frequency and disease duration, and 52 healthy controls with comparable age and gender distribution.
All patients had their diagnosis confirmed by their treating neurologists. Diagnosis of MS was based on the 2010 Polman criteria15. Diagnosis of NMOSD was based on the 2015 Wingerchuk criteria16. Exclusion criteria were the presence of other neurological diseases, concurrent cardiovascular or eye diseases with potential influence on visual function. Eyes with history of ON within last 6 months were excluded from analyses with OCT.
Healthy controls were selected among hospital staff and patients’ families. Inclusion criteria were negative history for neurological, eye and cardiovascular diseases with potential influence on visual function, best corrected high-contrast visual acuity at least 0.8, maximum refraction correction between −6 and +3 spherical dioptres.
Data collection
For each participant, we collected clinical data (diagnosis, antibody status, Expanded Disability Status Scale [EDSS], previous medical history including ON); visual acuity, pattern-reversal VEP and OCT were taken the same day. NMOSD patients were screened for anti-AQP4 and anti-MOG antibodies. AQP4 antibody testing was performed with indirect immunofluorescence on primate cerebellum and cell-based assay. Two AQP4-negative subjects testing positive for anti-MOG antibodies were excluded from the study.
Visual acuity testing was performed with high-contrast (HCVA) and low-contrast (2.5% and 1.25%) Early Treatment of Diabetic Retinopathy Study (ETDRS) tables, according to ICO recommendations17; decimal visual acuity and number of ETDRS table lines read were recorded.
Optical coherence tomography was recorded according to APOSTEL recommendations18 using spectral domain OCT Spectralis (Heidelberg Engineering, Heidelberg, Germany; software v5.8), with peripapillary RNFL raster scans, taken without pupil dilation, centred on the optic nerve head (ART 100 frames, diameter 12°). OSCAR-IB criteria were assessed in all RNFL scans with manual review by a single experienced OCT operator19.
Monocular pattern-reversal VEP with 15′ and 30′ achromatic checks were recorded according to ISCEV standard20 over Oz (10–20 international system), with Cz as reference. Standard stimulus was generated by Micromed Pattern 10 (Micromed, Mogliano Veneto, Italy) device and visualized through LCD monitor. Subjects wear corrective lenses if needed for distance vision. Pattern inversion frequency was 1.7 Hz; at least 30 epochs free from artefacts, contributing to the final average, were recorded; 2–3 consecutive averages were collected for each eye. VEP reproducible components N75, P100 and N145 were marked by the recording technician at the earliest peak of the 2–3 recordings. All measurements were verified by two expert neurologists. P100 latency (when measurable) and inter-peak amplitude were analysed.
Range of normality for VEP and OCT parameters studied was derived from an internal normative, developed on healthy controls, with threshold at 2.5–97.5% percentile. VEP amplitude lower than 3 µV was considered reduced; VEP latency was considered delayed if higher than 120 ms in people under 40 years old, 125 ms in people aged 40–49 years, 130 ms in older people. Peripapillary RNFL thickness lower than 84 µm was classified as reduced. For integrated OCT-VEP analyses, when VEP were absent, amplitude was imputed at 0 µV and latency at 140 ms.
Statistical analysis
VEP and OCT data were grouped by patient diagnosis and history of optic neuritis: NMOSD ON+, NMOSD ON−, MS ON+, MS ON−. Analyses were performed with R statistical environment (version 3.3, R Foundation for Statistical Computing, Vienna, Austria). Categorical variables and proportions were evaluated with Fisher’s exact test. Quantitative data were assessed with Wilcoxon rank-sum test or its parametric equivalents according to data distribution. Regression analysis was performed with generalized mixed linear models (using lme4 packages) and generalized estimating equations (GEE) models, accounting for within-subject effects (using geepack, multcomp and BSagri packages); subsequent pairwise comparisons were performed with Wald test. For all tests the alpha level was set at 0.05.
Results
Demographic, clinical and baseline data of study groups are shown in Table 1.
Table 2 shows main results about visual acuity testing, VEP and OCT parameters in study groups. Antibody testing was available for 45/50 NMOSD subjects. NMOSD subjects did not show differences in OCT and VEP parameters on the basis of anti-AQP4 antibody serostatus (GEE model, p = 0.87 for VEP latency, p = 0.33 for OCT RNFL).
VEP and OCT in eyes with ON history
Among eyes with ON history, the frequency of absent 15′ VEP was significantly higher in NMOSD (63.0% [95% CI: 49.6–74.6%]) compared to MS (7.3% [CI: 2.9–17.3%], p < 0.001, Fisher’s exact test).
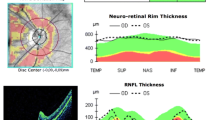
As shown in Fig. 1A, average P100 latency delay was observed in ON+ eyes of both NMOSD and MS patients compared to ON− eyes and to healthy controls (GEE); average latency did not differ between NMOSD and MS (p = 0.97). In ON+ eyes, VEP were delayed in 18/20 (90.0%) NMOSD eyes with recordable VEP (18/54, 33.3% of all eyes) and in 64.7% (33/51) MS eyes with recordable VEP (33/55, 60.0% of all eyes). A smaller proportion of severe P100 latency delay (over 150 ms) was observed in NMOSD compared to MS ON+ eyes (p = 0.016, Fisher). The analysis of 30′ check-size VEP produced analogous results (not shown).
Distribution of visual evoked potentials (VEP) latency (panel A) and retinal nerve fibre layer (RNFL) thickness (panel B). Generalized estimating equation (GEE) model (p < 0.001 overall). Asterisks reflect significance of pairwise comparisons after GEE (*p < 0.05, **p < 0.01, ***p < 0.001). In Panel A, only eyes with non-absent VEP are shown. HC: healthy controls.
Peripapillary RNFL thickness measured with OCT was decreased in both NMOSD and MS ON+ eyes, compared to ON− eyes and to healthy controls (Fig. 1B). Compared to ON− eyes, average RNFL thinning was 50.3 ± 3.9 µm in NMOSD and 9.4 ± 2.1 µm in MS; mean RNFL thickness was lower in NMOSD than in MS (44.1 vs. 78.7 µm, p < 0.001, GEE).
At receiver operating characteristic (ROC) analysis, a threshold of 60 µm was determined to have optimal accuracy to separate NMOSD from MS ON+ eyes, with values lower than 60 µm having 88% (95% CI: 69–97) sensitivity and 93% (CI: 81–98) specificity for NMOSD diagnosis. The same cut-off was found also when limiting the analysis to eyes with a single previous ON episode (N = 14 for NMOSD, N = 36 for MS), with sensitivity of 93% (95% CI: 64–100) and specificity of 92% (CI: 76–98). No significant effect of number of ON episodes on RNFL was observed in subgroup analysis.
Low vision, defined by decimal high-contrast visual acuity (HCVA) less than 0.3217, was significantly more common in NMOSD eyes (p < 0.001, Fisher’s exact test) than in MS. When analysing VEP and RNFL categories in ON+ eyes, stratified by range of visual performance17 (Fig. 2), worse visual performance was accompanied by an increased frequency of absent VEP and reduced RNFL thickness in both NMOSD and MS eyes. However, in NMOSD, even for comparatively good visual performance, very severe RNFL thinning (<60 µm) was observed, while MS eyes with severe visual impairment did not show comparable grades of RNFL reduction. Statistical analysis confirmed the significant effect of NMOSD diagnosis (p < 0.001, GEE) in changing the relationship between RNFL thickness and HCVA after ON.
Relationship of VEP latency (Panel A) and RNFL thickness (Panel B) with visual acuity. Decimal high-contrast visual acuity (HCVA) classes: (near)-blindness (<0.02); profound (<0.05), severe (<0.12), moderate (<0.32), mild (<0.80) visual impairment, normal vision (≥0.80). Stratified by VEP latency and OCT RNFL thickness category.
We compared the contribution of RNFL thickness and HCVA to diagnosis of NMOSD after ON with a multivariate logistic model, which showed RNFL was the only significant predictor (p < 0.001), encompassing the effect of visual acuity: NMOSD diagnosis becomes more probable, with OR 1.16 (95% CI: 1.08–1.29), for every 1 µm RNFL reduction.
Relationship between VEP latency increase and HCVA was affected too by NMOSD diagnosis, with trend for significance considering only the 20 NMOSD ON+ eyes with recordable VEP (p = 0.12, GEE) and much stronger statistical evidence (p < 0.001) including also ON− eyes.
VEP and OCT in eyes without ON history
Mean VEP latency observed in MS eyes without ON history was increased compared to healthy controls (p < 0.001, GEE); RNFL thickness was reduced vs. controls (p < 0.001).
In NMOSD ON− eyes, RNFL thickness did not differ from controls (p = 0.47), but VEP latency displayed an average P100 delay of 6.6 ± 1.4 ms compared to controls (p < 0.001, GEE); comparison of latency distributions (median [IQR]: 122 [10.8] ms in NMOSD vs. 115 [7.0] ms in controls) confirmed that this finding was not due to effect of outliers (not shown).
In our MS cohort we observed a correlation with disease duration, with 0.68 ± 0.30 ms P100 delay (p = 0.022, GEE) and 0.87 ± 0.21 µm RNFL thinning (p < 0.001) for every year of disease duration, while controlling for age and fellow eye ON status. In NMOSD we found VEP latency increasing 0.24 ± 0.07 ms for every year of age (p < 0.001, GEE), while relationship with disease duration, controlling for patient age, showed a trend for significance (+0.28 ± 0.17 ms per year, p = 0.10); no significant role for fellow eye ON status was found (p = 0.29). No statistical relationship between RNFL thickness and age or disease duration in our NMOSD cohort was found.
Integrated VEP-OCT measures
A GEE regression model was designed to compare in NMOSD and MS eyes, including both ON+ and ON− eyes, the relationship between VEP latency and RNFL thickness; for 1 µm RNFL reduction, VEP latency was delayed on average by 0.48 ± 0.10 ms in MS and 0.14 ± 0.08 ms in NMOSD, showing a significant prevalence of axonal involvement in NMOSD vs. MS (p = 0.02, Wald test; Fig. 3A).
Combined OCT-VEP analysis. In Panel A, relationship between RNFL thickness and VEP latency is assessed with a GEE model. Only eyes with non-absent VEP, at least 6 months since last optic neuritis (ON), are included. The linear relationship is significantly different in NMOSD vs. MS (Wald test, p = 0.02). In Panel B, only eyes with history of optic neuritis are included; every bar represents a single eye. OCT-VEP index is calculated as algebraic sum of Z-score for RNFL thickness and Z-score for VEP latency; threshold of −2.5 (dotted line) has the highest accuracy to discriminate NMOSD from MS.
A combined OCT-VEP index was calculated as the algebraic sum of VEP latency and RNFL thickness Z-scores of deviation from healthy controls: in our control cohort, average (± SD) VEP latency was 116.2 ± 5.3 ms, while average RNFL thickness was 96.7 ± 6.3 µm. VEP latency delay increases the index, while RNFL reduction reduces it.
Considering only eyes with history of ON, NMOSD patients showed lower OCT-VEP index values compared to MS (−4.99 ± 1.27 in NMOSD vs. 0.64 ± 3.73 in MS; p < 0.001, t-test), also considering only eyes with recordable VEP (−3.86 ± 0.73 in NMOSD vs. 0.15 ± 3.35 in MS; p = 0.006, t-test). A threshold value of −2.5 for combined OCT-VEP index, derived from ROC curve (not shown), had the highest accuracy (100.0% [95% CI: 83.4–100.0] sensitivity and 88.9% [CI: 75.1–95.8] specificity) in differentiating NMOSD from MS after optic neuritis (Fig. 3B).
Discussion
An important question yet to be fully answered is how to differentiate MS and NMOSD, particularly after optic neuritis, which can be the presenting symptom of both. Multiple clinical features have been described to help formulating a diagnostic hypothesis21 and AQP4 antibody testing is the mainstay of differential diagnosis, with high sensitivity and excellent specificity. To complement antibody testing, evoked potentials and optical coherence tomography, widely available with relatively low cost, if validated, may help raising suspicion of NMOSD, particularly in AQP4-antibody negative subjects, and elucidate details on prevailing pathophysiology mechanisms.
VEP and OCT in eyes with history of ON
In the present study, the frequency of absent VEP in NMOSD after ON, significantly higher than in MS, is consistent with rates between 47% and 64% reported in literature9,10. VEP delay in MS ON+ eyes, often persisting after clinical recovery from optic neuritis, has been recognized by decades. Data on VEP latency in NMOSD are less established. In a Japanese cohort studied by Watanabe9, P100 was delayed over 121 ms (30′ check-size) in only 1/6 (17%) AQP4+ patients with non-absent VEP response, compared to 28/64 (44%) MS patients with delayed latency. Neto10 in Brazilian subjects reported latency delay over a threshold of 117.6 ms (43′ check-size) in 2/20 (10%) NMOSD eyes with recordable VEP; a specific VEP “NMO pattern” with normal latency and isolated amplitude reduction was therefore suggested.
In contrast with these results, in the only study on European population published to date, by Ringelstein and colleagues11, considering both ON+ and ON− eyes, 36/74 (49%) NMO eyes with non-absent VEP had P100 latencies equal or higher than 120 ms (41′ check-size). Among eyes with ON history, a higher rate of VEP delay was found, with average latency of 131.2 ± 20.7 ms.
A thorough comparison of VEP latency delays and frequency of absent responses across studies is not possible due to different criteria for patient selection and to technical differences that may influence these measures. Consistently with previous findings11, we observed VEP latency delay in almost all NMOSD ON+ eyes with recordable VEP. However, after ON we found a lower frequency of severe latency delay (over 150 ms) in NMOSD than in MS.
In the present study, optic neuritis in NMOSD eyes was associated to an average RNFL loss of 35 µm more than in MS, a strong difference already reported in the literature with values of 24 µm according to Ratchford et al.1. Moreover, RNFL thickness lower than 60 µm in eyes with ON history was very highly suggestive of NMOSD diagnosis instead of MS, with 69–97% sensitivity and 81–98% specificity. No effect of number of ON events was found, and the result was corroborated by confirmation in the subgroup of eyes with single ON episode history.
Another finding of the present study is the higher performance of RNFL compared to visual acuity in detecting NMOSD patterns. It appears that the relationship between structural integrity, measured with OCT and VEP, and visual outcome (HCVA) is not conserved across different diseases: severe, destructive, axonal damage22, unparalleled by demyelination, is suggested in NMOSD from extreme RNFL loss, as well as frequent VEP absence. On the other hand, visual outcome in MS may be linked to severe demyelination with relatively preserved axonal integrity.
VEP and OCT in eyes without history of ON
This study confirms the finding of VEP latency and RNFL thickness abnormalities in MS ON− eyes already documented in literature23,24,25. With regard to NMOSD, Ringelstein11 reported delayed average VEP latency, compared to healthy controls, in NMOSD ON− eyes. Several studies have shown normal RNFL thickness in eyes without history of ON1,3,7,8, suggesting that subclinical damage in NMOSD is uncommon. Other studies reported instead axonal damage on optic nerve and retina5,6.
While our study did not show any significant RNFL thickness reduction, we reported average 6.6 ms VEP latency increase in NMOSD ON− eyes, not due to outliers effect; the main explanatory hypotheses for this finding could be minor subclinical ON events or chronic microstructural damage impacting on conduction speed. In the latter case, an increasing latency trend with disease duration may be observed; we found non-conclusive data suggesting this trend (p = 0.10), which may be further analysed with longitudinal studies.
Integrated structural and functional measures
Combination of structural and functional visual pathway assessment techniques showed different prevailing damage patterns in NMOSD vs. MS. In MS, more severe VEP delays were observed facing relatively preserved RNFL, suggesting predominance of demyelination over axonal loss. In NMOSD, severe axonal atrophy predominated, often hindering VEP identifiable responses.
This finding is consistent with the evidence from pathology of direct damage to axons in NMOSD, mediated by anti-AQP4 antibody astrocytopathy22,26, while in MS functional transmission impairment and axonal degeneration occurs mainly as a secondary effect of demyelination27.
Our results appear overall consistent with the reported observation of a more severe GCIPL (ganglion cell-inner plexiform layer) thinning at macular OCT and milder multifocal VEP latency delay after optic neuritis in 19 NMOSD subjects, compared with MS28. Our study further clarifies that more severe axonal atrophy occurs in NMOSD also for equal levels of visual acuity impairment and VEP delay, highlighting different structure-function relationships in the two diseases. With this respect, we quantified the balance between axonal damage and demyelination using a combined OCT-VEP index as a newly proposed marker, which showed promising accuracy in our sample, prompting further validation studies in larger cohorts.
AQP4 antibody status did not have a significant effect on OCT-VEP parameters in our NMOSD cohort, whatever the ON involvement, to suggest the hypothesis that the same pathological process may underlie both AQP4+ and AQP4− NMOSD subtypes.
Strengths and limitations of the study
There are several potential limitations to our study. First, this was a single-centre study with unblinded analysis and a relatively small number of subjects included, with some heterogeneity in disease severity and duration. Studies in newly diagnosed patients could provide more robust evidence for differences in early disease course. Another limitation comes from the lack of availability of OCT recordings in a subset of NMOSD patients, precluding integrated analyses on those subjects. Severe reduction of visual acuity, particularly represented in the NMOSD group, could reduce the quality of VEP and OCT recordings. The potential advantage of technological advancements in OCT (e.g. faster high-resolution acquisition) and VEP (e.g. multifocal stimulation) over standard methods should be explored.
Despite these limitations, this study correlates in vivo structural and functional measures of visual pathway, to inspect the contribution of axonal degeneration and demyelination to MS and NMOSD pathology. A combined structural-functional marker, such as the OCT-VEP index, demonstrated promising accuracy for discrimination of NMOSD from MS after one or more episodes of optic neuritis. Future studies are needed aimed at providing neurologists and neuro-ophthalmologists with extended tools for differential diagnosis and prognosis of optic neuritis.
References
Ratchford, J. N. et al. Optical coherence tomography helps differentiate neuromyelitis optica and MS optic neuropathies. Neurology. 73, 302–308 (2009).
Naismith, R. T. et al. Optical coherence tomography is less sensitive than visual evoked potentials in optic neuritis. Neurology. 73, 46–52 (2009).
Schneider, E. et al. Optical coherence tomography reveals distinct patterns of retinal damage in neuromyelitis optica and multiple sclerosis. PLoS ONE. 8, e66151 (2013).
Fernandes, D. B. et al. Evaluation of inner retinal layers in patients with multiple sclerosis or neuromyelitis optica using optical coherence tomography. Ophthalmology. 120, 387–394 (2013).
Syc, S. B. et al. Optical coherence tomography segmentation reveals ganglion cell layer pathology after optic neuritis. Brain. 135, 521–533 (2012).
Sotirchos, E. S. et al. In vivo identification of morphologic retinal abnormalities in neuromyelitis optica. Neurology. 80, 1406–1414 (2013).
de Seze, J. et al. Optical coherence tomography in neuromyelitis optica. Arch Neurol. 65, 920–923 (2008).
Lange, A. P. et al. Spectral-domain optical coherence tomography of retinal nerve fiber layer thickness in NMO patients. J Neuroophthalmol. 33, 213–219 (2013).
Watanabe, A. et al. Multimodality-evoked potential study of anti-aquaporin-4 antibody-positive and -negative multiple sclerosis patients. J Neurol Sci. 281, 34–40 (2009).
Neto, S. P. et al. Evaluation of pattern-reversal visual evoked potential in patients with neuromyelitis optica. Mult Scler. 19, 173–178 (2013).
Ringelstein, M. et al. Visual evoked potentials in neuromyelitis optica and its spectrum disorders. Mult Scler. 20, 617–620 (2014).
Bennett, J. et al. Neuromyelitis optica and multiple sclerosis: Seeing differences through optical coherence tomography. Mult Scler. 21, 678–688 (2015).
Klistorner, A. et al. Axonal loss in non-optic neuritis eyes of patients with multiple sclerosis linked to delayed visual evoked potential. Neurology. 80, 242–245 (2013).
Narayanan, D. et al. Tracking changes over time in retinal nerve fiber layer and ganglion cell-inner plexiform layer thickness in multiple sclerosis. Mult Scler. 20, 1331–1341 (2014).
Polman, C. H. et al. Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Ann Neurol. 69, 292–302 (2011).
Wingerchuk, D. M. et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 85, 177–189 (2015).
International Council of Ophthalmology (ICO). Visual Acuity Measurement Standard. Italian J Ophthalmol. II/I, 1–15 (1988).
Cruz-Herranz, A. et al. The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology. 86, 2303–2309 (2016).
Tewarie, P. et al. The OSCAR-IB consensus criteria for retinal OCT quality assessment. PLoS ONE. 7, e34823 (2012).
Odom, J. V. et al. ISCEV standard for clinical visual evoked potentials (2009 update). Doc Ophthalmol. 120(1), 111–119 (2010).
Morrow, M. J. & Wingerchuk, D. Neuromyelitis optica. J Neuroophthalmol. 32, 154–166 (2012).
Kawachi, I. & Lassmann, I. Neurodegeneration in multiple sclerosis and neuromyelitis optica. J Neurol Neurosurg Psychiatry. 88, 137–145 (2017).
Sriram, P. et al. Relationship between optical coherence tomography and electrophysiology of the visual pathway in non-optic neuritis eyes of multiple sclerosis patients. PLoS ONE. 9, e102546 (2014).
Park, K. A., Kim, J. & Oh, S. Y. Analysis of spectral domain optical coherence tomography measurements in optic neuritis: differences in neuromyelitis optica, multiple sclerosis, isolated optic neuritis and normal healthy controls. Acta Ophthalmol. 92, e57–e65 (2014).
Petzold, A. et al. Optical coherence tomography in multiple sclerosis: a systematic review and meta-analysis. Lancet Neurol. 9, 921–932 (2010).
Hokari, M. et al. Clinicopathological features in anterior visual pathway in neuromyelitis optica. Ann Neurol. 79, 605–624 (2016).
Dutta, R. & Trapp, B. D. Mechanisms of neuronal dysfunction and degeneration in multiple sclerosis. Prog Neurobiol. 93, 1–12 (2011).
Shen, T. et al. Differing Structural and Functional Patterns of Optic Nerve Damage in Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder. Ophthalmol. 126, 445–453 (2019).
Acknowledgements
We thank Francesco Vitali and Marta Lamperti, neurophysiology technicians, for OCT-VEP recordings. This work was partly supported through an institutional grant from EMD Serono, the biopharmaceutical division of Merck KGaA (Darmstadt, Germany), by Regione Lombardia (POR FESR 2014-2020) within the framework of the NeOn project (ID 239047) and by the Italian Ministry of Education, University and Research through the IVASCOMAR project (CTN01_00177_165430, Cluster Tecnologico Nazionale Scienze della Vita “Alisei”).
Author information
Authors and Affiliations
Contributions
M.V. conceived and designed the study, performed data collection, literature research, statistical analyses, discussion of the findings, and writing of the manuscript. M.P. performed data collection and discussion of the findings. S.G., L.M., M.R., S.M., V.M. contributed and/or supervised data collection and discussion of the findings. G.C. conceived and designed the study, and performed discussion of the findings. L.L. conceived and designed the study, supervised data collection and statistical analyses, performed discussion of discussion of the findings, and writing of the manuscript. All authors revised, edited, and approved the manuscript for submission.
Corresponding author
Ethics declarations
Competing Interests
Dr. Vabanesi, Pisa, Guerrieri, Radaelli, Medaglini declare no competing interests relevant to the manuscript. Dr. Moiola received honoraria for speaking in scientific meetings and for advisory board from Biogen, Teva, Sanofi-Genzyme and Merck. Dr. Martinelli received honoraria for consulting services or speaking activity from Biogen, Merck, Novartis, Teva, Almirall, and Sanofi-Genzyme. Prof. Comi received personal compensation for consulting services and/or speaking activities from Novartis, Teva, Sanofi, Sanofi-Genzyme, Merck, Biogen, Excemed, Serono Symposia International Foundation, Roche, Almirall, Receptos, Celgene, and Forward Pharma. Prof. Leocani received honoraria for consulting services and/or speaking activity from Biogen, Novartis and Excemed.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vabanesi, M., Pisa, M., Guerrieri, S. et al. In vivo structural and functional assessment of optic nerve damage in neuromyelitis optica spectrum disorders and multiple sclerosis. Sci Rep 9, 10371 (2019). https://doi.org/10.1038/s41598-019-46251-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-46251-3
- Springer Nature Limited
This article is cited by
-
Update on the diagnosis and treatment of neuromyelits optica spectrum disorders (NMOSD) – revised recommendations of the Neuromyelitis Optica Study Group (NEMOS). Part I: Diagnosis and differential diagnosis
Journal of Neurology (2023)
-
The difference of the retinal structural and microvascular characteristics in patients with MOGAD-ON and AQP4-ON
BMC Neurology (2022)
-
Neuromyelitis optica spectrum standstill in rheumatic systemic autoimmune diseases
Egyptian Rheumatology and Rehabilitation (2020)
-
Neuromyelitis optica
Nature Reviews Disease Primers (2020)
-
Outcome and risk of recurrence in a large cohort of idiopathic longitudinally extensive transverse myelitis without AQP4/MOG antibodies
Journal of Neuroinflammation (2020)