Abstract
Vitamin D status, assessed by serum concentration of 25(OH)D, is the prime candidate marker for many disease-association studies, but the interplay between the subsequent 1,25-dihydroxyvitamin D (1,25(OH)2D) and 24,25-dihydroxyvitamin D (24,25(OH)2D) metabolites is unclear. In this study, we conducted an analysis from a large cohort of healthy, physically fit, young army recruits (n = 940). We found a significant, inverse relationship between serum 25(OH)D and 1,25(OH)2D:24,25(OH)2D vitamin D metabolite ratio (VMR) (r2Exp = 0.582, p < 0.0001), and demonstrated a significant association with increasing PTH concentration (p < 0.001). Circannual rhythms were evident for all vitamin D metabolites and VMRs except for 1,25(OH)2D when fitted to Cosinor curves. We estimated 1,25(OH)2D:24,25(OH)2D VMR of ≥35 to be the threshold value for vitamin D insufficiency, and ≥51 to be predictive of vitamin D deficiency. Our three-dimensional model provides mechanistic insight into the vitamin D-PTH endocrine system, and further substantiates the role of 24,25(OH)2D in human physiology. The model sets a new paradigm for vitamin D treatment strategy, and may help the establishment of vitamin D-adjusted PTH reference intervals. The study was approved by the UK Ministry of Defence research ethics committee (MODREC 165/Gen/10 and 692/MoDREC/15). ClinicalTrials.gov Identifier NCT02416895.
Similar content being viewed by others
Introduction
The vitamin D pathway is a dynamic system, and its functional role in bone health and other diseases is the subject of intense research. Associations of vitamin D deficiency with a wide spectrum of disease states have drawn attention from the scientific community and increasing awareness of the general population. Despite vitamin D deficiency being a global public health concern, the approach through improving vitamin D status by supplementation, dietary intake and increased sunlight exposure, has resulted in mixed outcomes1,2,3. The contradictory evidence has prompted studies on the metabolites of vitamin D. The most abundant metabolite in circulation is 25-hydroxyvitamin D (25(OH)D), which exists in two major forms: 25-hydroxycholecalciferol (25(OH)D3) and 25-hydroxyergocalciferol (25(OH)D2). Measurement of serum total 25(OH)D (D3 + D2) is the barometer of vitamin D status; concentrations ≤30 nmol/L and between 30–50 nmol/L are defined as deficient and insufficient, respectively by the U.S Institute of Medicine (IOM)4 and the UK National Osteoporosis Society (NOS)5. 1,25-dihydroxyvitamin D (1,25(OH)2D) is synthesised by the hydroxylation of 25(OH)D through the actions of 1α-hydroxylase produced in the renal tubules. 1,25(OH)2D is the most biologically active form of vitamin D and circulates in pmol/L concentration; it controls intestinal absorption of calcium and phosphate, stimulates osteoclast activity, and helps regulate the release of parathyroid hormone (PTH). Although 1,25(OH)2D is derived from 25(OH)D, there is no direct correlation in serum concentrations between the two vitamin D metabolites except in patients with chronic kidney disease (CKD)6, where a greater association is observed between 1,25(OH)2D and 25(OH)D, dependent upon the severity of the renal impairment. The lack of a direct relationship, despite their close proximity in the metabolic pathway, is due to the tight regulation of the hydroxylation enzymes expressed by the actions of CYP27B1 and CYP24A1. CYP24A1 produces 24-hydroxylase that converts 25(OH)D into 24,25-dihydroxyvitamin D (24,25(OH)2D). The transcription of the CYP24A1 gene is stimulated by the phosphate-regulating hormone fibroblast growth factor-23 (FGF23), and when PTH is suppressed. The combination results in an increase in serum 24,25(OH)2D. We have previously described a concentration-dependent relationship between serum 25(OH)D and 24,25(OH)2D7. We have also reported a patient, presenting with idiopathic infantile hypercalcaemia (IIH), who was diagnosed with biallelic CYP24A1 mutations resulting in the inability to produce 24,25(OH)2D from 25(OH)D, and had an elevated serum 1,25(OH)2D and a persistent state of hypercalcaemia. The use of 25(OH)D:24,25(OH)2D vitamin D metabolite ratio (VMR) can be a valuable tool in identifying such pathological conditions resulting from impaired CYP24A1 function8,9. The use of VMR in the population can provide an assessment of the vitamin D catabolic status; thus allowing a targeted approach to vitamin D supplementation10.
In this report, we describe a novel approach to the interpretation of serum 25(OH)D and 1,25(OH)2D concentrations that incorporates 24,25(OH)2D values. Using data from a large cohort of young healthy adults as our reference population, we report the intricate relationships between active and catabolic forms of vitamin D metabolites, and the influence on PTH.
Results
Results from 940 participants were included in the data analysis. Statistical analyses on 25(OH)D and 24,25(OH)2D were performed on the respective total (sum of D3 + D2) values, the distributions were untrimmed and no outlier was removed. Summary of the distribution of biochemical profile is shown in Table 1. 25(OH)D2 was found in 57.8% of the subjects, mean (range) of 4.2 nmol/L (0.6–29.1). 24,25(OH)2D2 was found in 0.4% of the subjects, mean (range) 1.5 nmol/L (1.2–1.8).
24,25(OH)2D and 25(OH)D
The mean concentration of 24,25(OH)2D was on average 9.5-fold lower than 25(OH)D. Linear regression analysis (Fig. 1a) showed a directly proportional relationship between 24,25(OH)2D and 25(OH)D concentrations: \([24,25{({\rm{O}}{\rm{H}})}_{2}{\rm{D}}]\,=\,0.0946\,\times \,[25({\rm{O}}{\rm{H}}){\rm{D}}]\,-\,0.42;\,{r}^{2}\,=\,0.7206\). Using this equation, we derived serum 24,25(OH)2D concentration of ≥4.3 nmol/L to be equivalent to the IOM vitamin D replete status (i.e. 25(OH)D of 50 nmol/L), and 24,25(OH)2D concentration of ≤2.4 nmol/L is equivalent to deficiency status (i.e. 25(OH)D of ≤30 nmol/L).
Non-parametric correlations of (a) 24,25(OH)2D (b) 1,25(OH)2D (c) 25(OH)D:24,25(OH)2D VMR and (d) 1,25(OH)2D:24,25(OH)2D VMR, against their respective 25(OH)D concentration. Solid lines in (a,b) represent linear regression line. LOWESS fitted curve in (c,d) (99% point fit). The mean 24,25(OH)2D and 1,25(OH)2D concentrations, 25(OH)D:24,25(OH)2D VMR and 1,25(OH)2D:24,25(OH)2D VMR represent 8.7%, 222.4%, 20.8% and 60.9% of their respective 25(OH)D concentration. Assay lower limit of quantification (LLoQ): 25(OH)D and 24,25(OH)2D = 0.1 nmol/L, 1,25(OH)2D = 12 pmol/L.
1,25(OH)2D and 25(OH)D
Despite a direct enzymatic conversion of 25(OH)D to 1,25(OH)2D, we showed no correlation in serum concentrations between these two vitamin D metabolites (Fig. 1b). This finding is consistent with published studies; 1,25(OH)2D is able to directly inhibit the expression of 1α-hydroxylase, and indirectly inhibit by suppressing PTH and stimulating FGF23 production11,12. This negative feedback system provides an essential safeguard mechanism against hypercalcaemia, hence 1,25(OH)2D concentration is unaffected by the circulatory concentration of 25(OH)D.
25(OH)D:24,25(OH)2D VMR and vitamin D status
The 25(OH)D:24,25(OH)2D VMR showed an indirect relationship with 25(OH)D (Fig. 1c); LOWESS fitting showed a steady increase in 25(OH)D:24,25(OH)2D VMR with the decline in 25(OH)D concentration. One-way ANOVA showed a significant increase in 25(OH)D:24,25(OH)2D VMR (p > 0.001) at 25(OH)D below 50 nmol/L (Fig. 2). The greatest increase was observed when 25(OH)D concentration decreased below ≤30 nmol/L. The decrease in relative production of serum 24,25(OH)2D in response to the decline in 25(OH)D suggests down-regulation of CYP24A1.
1,25(OH)2D:24,25(OH)2D VMR and vitamin D status
Vitamin D status, as indicated by 25(OH)D concentrations, revealed an exponential negative correlation (r2Exp = 0.582) with 1,25(OH)2D:24,25(OH)2D VMR (Fig. 1d). Post hoc analysis identified a significant increase in 1,25(OH)2D:24,25(OH)2D VMR at 25(OH)D ≤ 60 nmol/L (Fig. 3). Using the Jacobson and Truax13,14 method to determine the cut-off value for clinically significant change7, we estimated 1,25(OH)2D:24,25(OH)2D VMR of ≥35 to be the predictive threshold value for vitamin D insufficiency, and ≥51 to be predictive threshold for vitamin D deficiency. The threshold values were determined from subject samples collected in the winter months (January to April) due to the seasonal variation of 25(OH)D. Receiver Operating Characteristic (ROC) curves generated from data collected between January to April produced area under the curve (AUC) values of 0.88 and 0.86, indicating the VMR cut-offs are excellent at discriminating individuals with vitamin D insufficiency and deficiency. The 1,25(OH)2D:24,25(OH)2D VMR at 35 and 51 achieved true positive rate (sensitivity) at 80% and 78%, respectively, and false positive rate (specificity) of 82% and 74%, respectively (Fig. 4a,b).
Distribution of 1,25(OH)2D:24,25(OH)2D VMR by 25(OH)D intervals. It demonstrates the exponential increase in 1,25(OH)2D:24,25(OH)2D VMR with the decrease in serum 25(OH)D. Box and whiskers represent the median, interquartile range and 95% population intervals. Each interval contains an equal number of subjects.
Diagnostic performance of 1,25(OH)2D:24,25(OH)2D VMR in the assessment of vitamin D status during winter months (Jan–April) (n = 402). Receiver Operating Characteristic (ROC) curve depicts diagnostic sensitivity and specificity levels. (O) represents decision threshold for (a) vitamin D replete (i.e. 25(OH)D ≥ 50 nmol/L), 1,25(OH)2D:24,25(OH)2D VMR threshold value of 35 (sensitivity = 80%, specificity = 78%), (b) vitamin D insufficiency (i.e. 25(OH)D ≥ 30 nmol/L), 1,25(OH)2D:24,25(OH)2D VMR threshold value of 51 (sensitivity = 82%, specificity = 74%). The diagonal lines represent the line of no discrimination.
1,25(OH)2D:24,25(OH)2D VMR and PTH
Circulating PTH is influenced by 25(OH)D and 1,25(OH)2D, and vice versa. We hypothesised that PTH concentration changes with 1,25(OH)2D:24,25(OH)2D VMR and 25(OH)D. To test our hypothesis, median PTH concentrations were established from grid analysis based on groupings of 1,25(OH)2D:24,25(OH)2D VMR and 25(OH)D in ascending order (Table 2). A decrease in PTH concentration was observed from the high 1,25(OH)2D:24,25(OH)2D VMR (100+) and low 25(OH)D (<30 nmol/L) group, to the low 1,25(OH)2D:24,25(OH)2D VMR (<30) and high 25(OH)D (100+ nmol/L) group. Using Kruskal-Wallis independent non-parametric analysis to test the distribution of PTH across all groups, a highly significant (p > 0.001) change in PTH concentration was found across the 1,25(OH)2D:24,25(OH)2D VMR and 25(OH)D categories, hence the null hypothesis was rejected. Using Spearman’s rank correlation coefficient (2-tailed) to assess monotonic functions between variables, significant positive correlations were evident between VMRs and PTH (1,25(OH)2D:24,25(OH)2D VMR rho = 0.249, p > 0.001 and 25(OH)D:24,25(OH)2D VMR rho = 0.134, p > 0.001); whereas vitamin D metabolites showed significant negative correlations with PTH (25(OH)D rho = −0.287, p > 0.001, 24,25(OH)2D rho = −0.282, p > 0.001 and 1,25(OH)2D rho = −0.87, p > 0.001). The statistical significance remain unchanged after adjustment for BMD and BMI as covariates.
Circannual variations in vitamin D metabolites and VMRs
Cosinor-fit curves (Fig. 5) show significant circannual rhythm for 25(OH)D (p < 0.001), 24,25(OH)2D (p < 0.01), 25(OH)D:24,25(OH)2D VMR (p < 0.001), 1,25(OH)2D:24,25(OH)2D VMR (p < 0.001) and PTH (p < 0.05). No significant rhythm was observed for 1,25(OH)2D (p = 3.125). The rhythm observed for 25(OH)D is consistent with previous reports15,16. 24,25(OH)2D showed a similar peak (July–Aug) and nadir (Jan–Mar) pattern as for 25(OH)D. 25(OH)D:24,25(OH)2D VMR and 1,25(OH)2D:24,25(OH)2D VMR exhibited patterns in the opposite direction, with peak (Mar–April) and nadir (Aug–Sept) suggesting that the production of 24,25(OH)2D is relatively higher during summer/early autumn months. Acrophase, defined as the lag time between rhythm-adjusted mean and peak cycle value, was on average (SD) of 8.1(0.3) months for all vitamin D metabolites except for 1,25(OH)2D. A low amplitude, circasemiannual PTH secretory rhythm was observed, with an acrophase of 3.5 months.
Discussion
This is the first study to demonstrate a relationship between serum concentrations of 25(OH)D and 1,25(OH)2D when expressed as a relative ratio with serum 24,25(OH)2D. We provide evidence that the conversion of 25(OH)D to 1,25(OH)2D is associated with the catabolism of 25(OH)D to 24,25(OH)2D, which can be assessed by the measurement of serum 24,25(OH)2D and its derived VMR.
The inverse exponential correlation between 1,25(OH)2D:24,25(OH)2D VMR and 25(OH)D provides insight into the dynamics of vitamin D metabolites in healthy, young adults; when vitamin D status is sufficient, serum concentrations of 1,25(OH)2D and 24,25(OH)2D are maintained in relative proportion and showed no significant change beyond the sufficient threshold. In contrast, when vitamin D status is insufficient, a progressive and highly significant increase in 1,25(OH)2D:24,25(OH)2D VMR is evidence that the production of serum 1,25(OH)2D is favoured over 24,25(OH)2D as the availability of vitamin D precursors in circulation diminishes. Our data imply two possible regulatory functions of the 24,25(OH)2D pathway; in hypervitaminosis, the pathway is ‘switched on’ to allow excess 25(OH)D to be converted to 24,25(OH)2D. The 24-hydroxylase pathway results in the formation of calcitroic acid for excretion. In hypovitaminosis, the 24,25(OH)2D pathway is partially inactivated to conserve 25(OH)D and to maintain an adequate supply of substrate for conversion to 1,25(OH)2D. Although the biological activity of 24,25(OH)2D is yet to be fully elucidated, its role in vitamin D catabolism appears certain. Low serum concentrations of 24,25(OH)2D and elevated 25(OH)D:24,25(OH)2D VMR is useful in identifying patients with loss-of-function CYP24A1 mutations8,9,17. In our previous publication7, we described a case of biallelic CYP24A1 mutation in a patient presenting with hypercalcaemia, elevated serum 1,25(OH)2D concentration (293 pmol/L, reference range 43–144 pmol/L), and elevated 25(OH)D:24,25(OH)2D VMR of 32. On diagnosis, the patient’s 1,25(OH)2D:24,25(OH)2D VMR was 212 (1.6 times the upper 97.5th percentile of 132), which was attributed to supplementation with vitamin D. One month after treatment for hypercalcaemia and cessation of vitamin D supplement, serum 1,25(OH)2D was within the reference range, the 1,25(OH)2D:24,25(OH)2D VMR decreased to 130 (below the 97th percentile), and the 25(OH)D:24,25(OH)2D VMR remained elevated at 35.
A major finding of this study was the link between the vitamin D metabolites and VMRs with the distribution of PTH. To the best of our knowledge, this is the first such report in a human population study. It is widely accepted that the PTH concentration is associated with 25(OH)D, but not with the active 1,25(OH)2D. This is due to the tight regulatory mechanisms, and the regulatory processes that take place via the vitamin D receptor (VDR) to activate intracellular transport of calcium and stimulate PTH secretion. Using our 1,25(OH)2D:24,25(OH)2D VMR and 25(OH)D model (Fig. 1d), we have shown that individuals with low 25(OH)D (≤50 nmol/L), normal 1,25(OH)2D but high 1,25(OH)2D:24,25(OH)2D VMR (≥101) have significantly higher PTH concentration than those at the opposite end of the spectrum. An interpretation of our finding supports a biological role of 24,25(OH)2D other than as a catabolic metabolite of vitamin D. Relative high production of 24,25(OH)2D may reduce the bioactivity of 25(OH)D and 1,25(OH)2D, particularly extra-renal production of 1,25(OH)2D, to down-regulate the secretion of PTH whilst maintaining 1,25(OH)2D concentrations within the strict boundaries required for appropriate calcium homeostasis. Relatively low 24,25(OH)2D could enhance the anabolic effects of vitamin D metabolism, by stimulating PTH production. The biological action of 24,25(OH)2D on the inhibition of PTH secretion was first reported in animal and in vitro models in the late seventies18,19. More recently there is increasing evidence supporting physiological functions of 24,25(OH)2D on bone and cartilage20,21,22 in promoting fracture healing, and protection against cartilage damage. The existence of a 24,25(OH)2D-specific nuclear or membrane receptor has been reported23, but its function has yet to be elucidated. Given that CYP24A1, the enzyme responsible for the production of 24,25(OH)2D, is present in most tissues with VDR, understanding the mechanisms controlling the production of 24,25(OH)2D relative to other vitamin D metabolites may have significance beyond vitamin D catabolism, potentially shaping vitamin D supplementation strategies.
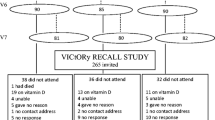
Mapping the circannual rhythms of vitamin D metabolites and VMRs is an important component of this study. We have published reports on longitudinal studies (Macdonald et al.)15,16,24, decribing the changes in serum 25(OH)D and 24,25(OH)2D throughout a year in vitamin D supplemented or non-supplemented subjects. In the VICtORy (Vitamin D and CardiOvascularRisk)15 and VICtORy RECALL16 randomised controlled studies performed using a group of postmenopausal women residing in the northeast of UK, the placebo group showed a two-fold increase in serum 25(OH)D in peak summer months (July–August), compared to the nadir in late winter months (January–March). Our younger cohort of healthy individuals in this study showed similar trends; 24,25(OH)2D had a propensity to fluctuate with 25(OH)D throughout the year, with changes between summer and winter months, as indicated by a lower 25(OH)D:24,25(OH)2D VMR during January to March than during July to September. Serum 1,25(OH)2D displayed no rhythm and was within the reference range throughout the year. The circannual variation of 1,25(OH)2D:24,25(OH)2D VMR was dependent on 24,25(OH)2D, with a peak-to-nadir difference of 19; such sharp demarcation between seasons would inevitably create uncertainty when using 1,25(OH)2D:24,25(OH)2D VMR in diagnostic decision-making. In contrast, 25(OH)D:24,25(OH)2D VMR is less susceptible to seasonal fluctuation, allowing the use of the VMR with fixed reference intervals irrespective of the time of the year.
One strength of our data is the chosen cohort; with participants attending blood sampling visits at strictly controlled time intervals and that the vitamin D metabolites were measured using gold-standard methodologies. The participants are well-defined, largely from a similar social-economic background, and exposed to the same level of fitness training, diet, and frequency of outdoor activities. The relative homogeneity of the subjects of our study population in combination with our inclusion criteria allowed us to confidently form a reference population and identify important changes in analytes. The limitations are that our findings are observational and based on baseline sampling at the start of training. Also, our cohort represents young adults of Caucasian extraction (92.9%), and cannot be extrapolated to the wider population of mixed ethnicity. The predictive threshold values were established based on the equivalent vitamin D status as described by IOM, and not based on our own data as the study was not randomly controlled. We did not measure vitamin D binding protein (VDBP) and free 25(OH)D due to the ethnic homogeneity of our population, and we did not exclude factors that may influence VDBP levels (e.g. oral contraceptive use in female recruits). We also acknowledge the use of VMR in reverse (i.e. 24,25(OH)2D:25(OH)D - as described in25) can be an alternative approach to express the relationship. Lastly, the sample data used in the current study is a subset of the Army cohort used to establish the reference intervals of serum 24,25(OH)2D7. Whilst there is a degree of overlap, the overall content of this report, analytical approaches and conclusions described are independent of the previous report.
In conclusion, the present analysis characterises the absolute and relative concentrations of the active and catabolic form of vitamin D metabolites in a well-defined young, healthy and physically fit population. The use of VMRs provides insight into the metabolic pathway and the variations exhibited throughout the year. We propose a three-dimensional model incorporating 1,25(OH)2D, 24,25(OH)2D and 25(OH)D measurements and report a strong correlation between metabolites that are linked with PTH. Such modelling could help establish vitamin D-adjusted PTH reference intervals, and ultimately contribute to the goal of a “Treat to target” approach to vitamin D supplementation.
Methods
Study design
The study received ethics approval from the UK Ministry of Defence Research Ethics Committee and was conducted in accordance with the Declaration of Helsinki (2013). The characteristics of the subjects included in the study are shown in Table 3. In total, 2252 new British Army recruits at the start of phase one training volunteered for the study. Written informed consent was obtained from all study participants, and each required to complete a detailed health questionnaire, including medical history and the use of supplements. All recruits undertook physical and cognitive testing, and a detailed medical examination prior to joining the army. The British Army entry requirements restrict individuals with chronic medical conditions; therefore, our study population represents a medically screened, disease-free, and physically fit population. In the analysis, we excluded individuals who reported the use of calcium and vitamin D supplements (including multivitamins and cod liver oil), and excluded participants who reported injury and illness prior to recruitment; conditions such as being underweight, eating disorders, or those with a history of bone fracture. 940 participants were included in the final statistical analyses. The majority of participants were from Caucasian population (92.9%), with a minority from a diverse ethnicity (Asian 1.6%, Black 1.7%, Chinese 0.1%, mixed 3%, others 0.7%).
Sample collection
Blood samples were collected during the period of June 2014 and March 2016. Venous blood samples were obtained from the participants at the start of 14-week long basic military training. Sample collections were scheduled on a monthly basis to balance the seasonal variations. Each intake comprised, on average (range), 86 (43–120) participants. Blood samples were collected into serum gel separator tube and EDTA plasma container (BD Vacutainer). Samples were centrifuged immediately after collection at 3,000 × g for 10 minutes. Plasma/serum layers were aliquoted into a separate polystyrene tube and stored at −20 °C until analysis. All samples were anonymised to the researchers at the point of access.
Ethical approval
The study was approved by the UK Ministry of Defence research ethics committee (MODREC 165/Gen/10 and 692/MoDREC/15). ClinicalTrials.gov Identifier NCT02416895.
LC-MS/MS measurements of serum 25(OH)D and 24,25(OH)2D
Liquid chromatography tandem mass spectrometry (LC-MS/MS) was performed as described7,26,27,28. The method quantified 25(OH)D3, 25(OH)D2, 24,25(OH)2D3 and 24,25(OH)2D2 simultaneously from a single injection. 25(OH)D3 and 25(OH)D2 were calibrated using commercial standards (Chromsystems, München, Germany) traceable to standard reference material SRM972a from the National Institute of Science and Technology (NIST)25,29, and showed linearity between 0–200 nmol/L. The inter/intra-assay coefficient of variation (CV) was ≤9%, the lower limit of quantification (LLoQ) of 0.1 nmol/L. The assay showed <8% accuracy bias against NIST reference method on the Vitamin D external quality assessment (DEQAS) scheme. 24,25(OH)2D3 and 24,25(OH)2D2 were calibrated using in-house spiked standards traceable to NIST SRM972a. The assay is linear between 0–25 nmol/L; inter/intra-assay CV was ≤11%, LLoQ of 0.1 nmol/L for 24,25(OH)2D3 and 0.8 nmol/L for 24,25(OH)2D2.
Measurements of serum 1,25(OH)2D
The DiaSorin LIAISON® XL 1,25(OH)2D chemiluminescent immunoassay (Stillwater, MN, USA) method was used. The sandwich assay utilises a recombinant fusion protein for the capture of 1,25(OH)2D molecule and a murine monoclonal antibody detection system. The assay measures total 1,25(OH)2D between 12–480 pmol/L, the inter/intra-assay CV was ≤9.2%. The mean assay recovery was 94 ± 2%. On the Vitamin D external quality assessment (DEQAS) scheme, the assay showed ≤8.5% bias against method-specific mean and ≤9.1% bias against all method mean.
Biochemical analysis
Intact PTH and albumin-adjusted calcium (ACa) were analysed on the COBAS® (Roche Diagnostics, Mannheim, Germany) platform. PTH in EDTA plasma was measured using electrochemiluminescence immunoassay (ECLIA), the inter-assay CV was ≤3.8% across the analytical range of 1.2–5000 pg/mL. Total calcium and albumin were measured based on spectrophotometric methods. The inter-assay CV for Ca was ≤1.6%, albumin was ≤1.1%. ACa value is calculated using the equation \(ACa=(\,-\,0.8\times [Albumin]-4)+[Total\,Ca]\).
Statistical analysis
Descriptive statistics, scatterplots, ROC and LOWESS curves were constructed and analysed by Statistical Package for the Social Science (SPSS) version 22.0.0.1 (IBM, New York, USA) and GraphPad Prism 7 (GraphPad, San Diego, CA, USA). Univariate and multivariable linear regression analyses and one-way ANOVA were used to estimate associations. LOWESS curve fitting was used to explore nonlinear relationships between variables. Kruskal-Wallis independent analysis and Spearman’s rho were used to establish associations in non-parametric variables. Statistical significance was defined as p < 0.05. Frequency distribution histograms of the data were visually examined and checked for transcriptional and pre/post analytical errors before exclusion for statistical analysis. Confidence interval (CI) was established at 95% of the population. Circannual rhythm analysis was performed by population-mean cosinor analysis, based on cosinor-fitting equation \(y={\rm{MESOR}}+{\rm{Amplitude}}\times \,\cos ({\rm{Frequency}}(x)+{\rm{acrophase}})\). Midline estimate statistic of rhythm (MESOR), defined as the rhythm-adjusted mean value. Acrophase is the difference (time) between MESOR and peak value in the cosine curve.
Data Availability
The datasets generated and analysed during the current study are not publicly available due to data protection. Data request is subject to approval by the UK Ministry of Defence.
References
Bolland, M. J., Grey, A. & Avenell, A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. The lancet. Diabetes & endocrinology (2018).
Martineau, A. R. et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 356, i6583 (2017).
Khaw, K. T. et al. Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. The lancet. Diabetes & endocrinology 5, 438–447 (2017).
Ross, A. C. et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96, 53–58 (2011).
Francis, R. M. et al. National Osteoporosis Society practical clinical guideline on vitamin D and bone health. Maturitas 80, 119–121 (2015).
Levin, A. et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71, 31–38 (2007).
Tang, J. C. Y. et al. Reference intervals for serum 24,25-dihydroxyvitamin D and the ratio with 25-hydroxyvitamin D established using a newly developed LC-MS/MS method. J Nutr Biochem 46, 21–29 (2017).
Molin, A. et al. CYP24A1 Mutations in a Cohort of Hypercalcemic Patients: Evidence for a Recessive Trait. J Clin Endocrinol Metab 100, E1343–1352 (2015).
Kaufmann, M. et al. Clinical utility of simultaneous quantitation of 25-hydroxyvitamin D and 24,25-dihydroxyvitamin D by LC-MS/MS involving derivatization with DMEQ-TAD. J Clin Endocrinol Metab 99, 2567–2574 (2014).
Binkley, N. et al. Can vitamin D metabolite measurements facilitate a “treat-to-target” paradigm to guide vitamin D supplementation? Osteoporos Int 26, 1655–1660 (2015).
Armbrecht, H. J., Boltz, M. A. & Hodam, T. L. PTH increases renal 25(OH)D3-1alpha -hydroxylase (CYP1alpha) mRNA but not renal 1,25(OH)2D3 production in adult rats. Am J Physiol Renal Physiol 284, F1032–1036 (2003).
Collins, M. T. et al. Fibroblast growth factor-23 is regulated by 1alpha,25-dihydroxyvitamin D. J Bone Miner Res 20, 1944–1950 (2005).
Jacobson, N. S., Roberts, L. J., Berns, S. B. & McGlinchey, J. B. Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. J Consult Clin Psychol 67, 300–307 (1999).
Jacobson, N. S. & Truax, P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 59, 12–19 (1991).
MacDonald, H. M., Wood, A. D., Tang, J. C. & Fraser, W. D. Comparison of vitamin D(2) and vitamin D(3) supplementation in increasing serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. Am J Clin Nutr 96, 1152–1153, author reply 1153–1154 (2012).
Macdonald, H. M. et al. Longevity of daily oral vitamin D3 supplementation: differences in 25OHD and 24,25(OH)2D observed 2 years after cessation of a 1-year randomised controlled trial (VICtORy RECALL). Osteoporos Int 28, 3361–3372 (2017).
Ketha, H., Kumar, R. & Singh, R. J. LC-MS/MS for Identifying Patients with CYP24A1 Mutations. Clin Chem 62, 236–242 (2016).
Chertow, B. S., Baker, G. R., Henry, H. L. & Norman, A. W. Effects of vitamin D metabolites on bovine parathyroid hormone release in vitro. Am J Physiol 238, E384–388 (1980).
Henry, H. L., Taylor, A. N. & Norman, A. W. Response of chick parathyroid glands to the vitamin D metabolites, 1,25-dihydroxycholecalciferol and 24,25-dihydroxycholecalciferol. J Nutr 107, 1918–1926 (1977).
Boyan, B. D. et al. 24R,25-Dihydroxyvitamin D3 Protects against Articular Cartilage Damage following Anterior Cruciate Ligament Transection in Male Rats. PloS one 11, e0161782 (2016).
Gal-Moscovici, A., Gal, M. & Popovtzer, M. M. Treatment of osteoporotic ovariectomized rats with 24,25(OH)2D3. Eur J Clin Invest 35, 375–379 (2005).
St-Arnaud, R. & Glorieux, F. H. 24,25-Dihydroxyvitamin D–active metabolite or inactive catabolite? Endocrinology 139, 3371–3374 (1998).
St-Arnaud, R. CYP24A1-deficient mice as a tool to uncover a biological activity for vitamin D metabolites hydroxylated at position 24. J Steroid Biochem Mol Biol 121, 254–256 (2010).
Macdonald, H. M. et al. 25-Hydroxyvitamin D Threshold for the Effects of Vitamin D Supplements on Bone Density Secondary Analysis of a Randomized Controlled Trial. J Bone Miner Res (2018).
Wise, S. et al. Interlaboratory Comparison for the Determination of 24,25-Dihydroxyvitamin D(3) in Human Serum Using Liquid Chromatography with Tandem Mass Spectrometry. J AOAC Int (2017).
Owens, D. J. et al. Efficacy of High-Dose Vitamin D Supplements for Elite Athletes. Med Sci Sports Exerc 49, 349–356 (2017).
Saleh, L. et al. Impact of a single oral dose of 100,000 IU vitamin D3 on profiles of serum 25(OH)D3 and its metabolites 24,25(OH)2D3, 3-epi-25(OH)D3, and 1,25(OH)2D3 in adults with vitamin D insufficiency. Clin Chem Lab Med (2017).
Tang, J. et al. Profiles of 25 hydroxyvitamin D and its metabolite 24,25 dihydroxyvitamin D and 1,25 dihydroxyvitamin D in vitamin D3 supplementations studies. In The 43rd Annual European Calcified Tissue Society Congress (Bone Abstracts Vol 5 OP19, Rome, Italy, 2016).
Phinney, K. W. et al. Development of an Improved Standard Reference Material for Vitamin D Metabolites in Human Serum. Analytical chemistry 89, 4907–4913 (2017).
Acknowledgements
The authors would like to acknowledge Samuel Oliver, Mark Ward, Claire Potter, Xin Hui Aw Yong, Alexander Carswell and Daniel Kashi (Bangor University) for the collection of Army samples.
Author information
Authors and Affiliations
Author notes
A comprehensive list of consortium members appears at the end of the paper
Consortia
Contributions
J.C.Y.T. wrote the main manuscript text. J.C.Y.T. and S.J. performed data analysis. S.J., J.G., N.P.W., W.D.F. and J.C.Y.T. oversaw the project, interpretation of data, drafting and revising of the manuscript. J.C.Y.T. and the Bioanalytical Facility team performed sample analysis. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, J.C.Y., Jackson, S., Walsh, N.P. et al. The dynamic relationships between the active and catabolic vitamin D metabolites, their ratios, and associations with PTH. Sci Rep 9, 6974 (2019). https://doi.org/10.1038/s41598-019-43462-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43462-6
- Springer Nature Limited
This article is cited by
-
A newly developed and validated LC–MS/MS method for measuring 7-dehydrocholesterol (7DHC) concentration in human skin: a tool for vitamin D photobiology research
Photochemical & Photobiological Sciences (2022)
-
Vitamin D Measurement, the Debates Continue, New Analytes Have Emerged, Developments Have Variable Outcomes
Calcified Tissue International (2020)