Abstract
The strongest genetic risk factor of Behçet’s disease (BD) is HLA-B*51. Our group previously reported that HLA-A*26 is independently associated with the risk of the onset of BD apart from HLA-B*51. Here, we re-evaluated the association between HLA-A*26 and BD in the Japanese population. We also performed a comprehensive literature search and meta-analyzed the extracted published data concerning the relationship between HLA-A*26 and BD to estimate the odds ratio (OR) of HLA-A*26 to BD. In this study, we genotyped 611 Japanese BD patients and 2,955 unrelated ethnically matched healthy controls. Genotyping results showed that the phenotype frequency of HLA-A*26 was higher in BD patients than in controls (OR = 2.12, 95% CI: 1.75–2.56). Furthermore, within the HLA-B*51-negative populations, the phenotype frequency of HLA-A*26 was significantly higher in BD patients than in controls (OR = 3.10, 95% CI: 2.43–3.95). Results obtained from meta-analysis combined with our data showed that the modified OR of HLA-A*26 became 1.80 (95% CI:1.58–2.06), whereas within the HLA-B*51-negative population, the modified OR became 4.02 (95% CI: 2.29–7.05). A subgroup analysis arranged by the geographical regions showed HLA-A*26 is in fact associated with the onset of BD in Northeast Asia (OR = 2.11, 95% CI: 1.75–2.56), but not in the Middle East or in Europe.
Similar content being viewed by others
Introduction
Behçet’s disease (BD) is a recurrent multisystem inflammatory disorder characterized by four classical major symptoms consisting of recurrent aphthous oral ulcers, genital ulcers, ocular uveitis, and Erythema-nodosum-like skin lesions. Occasionally the inflammation of BD occurs in tissues and organs throughout the body including the vascular system, the central nervous system, the gastrointestinal tract, the lungs, the kidneys, and various joints. Despite being worldwide, the distribution of BD is higher in an area along the old Silk Route that extends from far Eastern Asia to the Mediterranean Basin1,2.
The strongest genetic risk factor of the BD is HLA-B*51. The odds ratio (OR) of HLA-B*51 to the BD was 5.78 with 95% confidential Interval (CI) = 5.00–6.673. The susceptible association of HLA-A*26 to the BD was initially reported from Taiwan, followed by various countries and ethnicities4,5,6,7,8,9,10,11. We previously reported that HLA-A*26 was independently and significantly associated with the risk of the onset of BD apart from HLA-B*5112. Several studies have reported that HLA-A*26:01 plays a predominant role in causing intense eye inflammations, which lead to uveitis and visual dysfunction, particularly in the Northeast Asian population4,8. The etiology of HLA-A*26 related BD causing more frequent and intense inflammations in uveal tissues in these populations is still unknown. Because HLA-A*26, as a risk allele of BD, is independent from HLA-B*51, HLA-A*26 mediated genetic pathways might be different from that of HLA-B*51 in how they develop inflammations. Further investigations to clarify the genetic involvement of HLA-A*26 and its correlation with the particular clinical manifestations of BD phenotypes in the Northeast Asian population might lead to one of the clues to understanding why there are regional disparities of phenotypes within BD patients.
In this study, we investigated the relationship between HLA-A*26 and BD by genotyping 611 Japanese BD patients and 2,955 unrelated ethnically matched healthy controls. In addition to our currently obtained genotyping data, we performed a comprehensive literature search and meta-analyzed the extracted published data concerning the relationship between HLA-A*26 and BD to estimate the synthesized OR of HLA-A*26 to BD. Additionally, we investigated the distribution of HLA-A*26 in the world population and summarized the regional and ethnical disparities of HLA-A*26 involvement in BD patients.
Results
HLA-A*26 genotyping
Allele and phenotype frequencies of HLA-A*26 are shown in Table 1. Both allele and phenotype frequencies of HLA-A*26 were significantly higher in the patient group as compared to the healthy controls. Allele frequency: 18.43% in BD vs. 10.93% in controls (OR = 1.84, 95% CI: 1.56–2.18). Phenotype frequency: 35.55% in BD vs. 20.68% in controls (OR = 2.12, 95% CI: 1.75–2.56). In addition to HLA-A*26 allele, -A*11, -A*31, -A*33 were also statistically significant, and the frequencies in the patient group and controls indicated that the genetic association of -A*31 as risk and -A*11, -A*33 as protective type.
HLA-A*26 frequency within the HLA-B*51-negative population
In the current genotyping study, 314 BD patients (51%) and 2,433 controls (82%) did not carry the HLA-B*51 antigen. The allele and phenotype frequencies of HLA-A*26 within the HLA-B*51-negative populations are shown in Table 2. Both allele and phenotype frequencies of HLA-A*26 were significantly higher in the BD group as compared to the controls. Allele frequency: 23.57% in BD vs. 11.16% in controls (OR = 2.48, 95% CI: 2.02–3.04). Phenotype frequency: 45.22% in BD vs. 21.05% in controls (OR = 3.10, 95% CI: 2.43–3.95). Besides HLA-A*26, -A*33 were statistically significant, and the frequency in the patient group and controls indicated HLA-A*33 as protective type.
Retrieved HLA-A*26 and -*B locus haplotype analysis in the Japanese population
2 loci retrieved haplotype frequencies of HLA-A*26 and -*B are shown in Table 3. The haplotype frequency of HLA-A*26-B*51 was 3.2% in BD cases and 0.7% in controls. The difference of the frequencies was statistically significant and the OR was 4.64 (95% CI: 2.98–7.24). Within the HLA-B*51 negative subsets, the entire sets of haplotypes retrieving HLA-A*26 and -*B alleles positively associated with BD susceptibility (OR = 1.59, 95% CI: 1.33–1.90). Within these various haplotypes, the haplotype frequency of HLA-A*26-B*40 was 5.9% in BD cases and 3.9% in controls, and the OR was 1.68 (95% CI: 1.27–2.22). The haplotypes of HLA-A*26-B*39, and A*26-B*55 showed relatively high ORs, 10.97 (95% CI:4.12–29.22) and 15.12 (95% CI: 2.40–95.14), respectively, but these haplotypes were rare both in BD cases and controls in Japanese population.
Literature Search and Meta-analysis
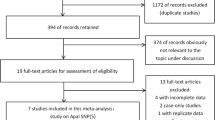
275 studies were identified through electronic search. 2 studies were added by manual database search. 85 studies were excluded after duplicate publications check. Full-texts of 99 studies were reviewed, and the final study included 14 independent case-control studies with 13 ethnicities, 1,104 BD patients and 8,140 healthy controls (Supplementary Fig. S1). Assessment of risk of bias for included studies was done through Newcastle-Ottawa Scale, and all included studies were of high quality with scores ranging from 7 to 9 (Table 4). Publication bias was assessed using a funnel plot (Supplementary Fig. S2). A synthesized analysis of data from a number of publications showed that the OR of HLA-A*26 among BD patients was 1.62 (95% CI: 1.09–2.39). Combined with our genotyping data, the modified OR became 1.80 (95% CI: 1.58–2.06). (Fig. 1). Additionally, within the HLA-B*51-negative populations, the entire OR combined with our genotyping data became 4.02 (95% CI: 2.29–7.05) (Fig. 2).
Regional disparities in the contribution of HLA-A*26 to the onset of BD
Subgroup analysis suggested that the association of HLA-A*26 between the onset of BD was statistically significant in the Northeast of Asia (OR = 2.11, 95% CI: 1.62–2.76) (Fig. 3), but not in the Middle East (OR = 1.39, 95% CI: 0.79–2.45), or in Europe (OR = 1.85, 95% CI: 0.55–6.22) (Supplementary Figs S3 and S4, respectively). The worldwide distribution of HLA-A*26 is shown in Fig. 413.
The worldwide distribution of HLA-A*26. The frequency of HLA-A*26 in regions and countries colored in red and blue are of 10~25%, and 5~10%, respectively. As for the other regions, the frequency was below 5%. The figure, made using mapchart.net, is licensed under CC BY-SA 4.0 license (https://creativecommons.org/licenses/by-sa/4.0/).
Discussion
Despite its worldwide presence, BD has a much higher prevalence in countries along the ancient Silk Route that extends from the Mediterranean basin to the far Eastern Asia. Turkey has the highest prevalence of BD in the world, with 20–420 cases per 100,000 reported14,15,16,17. Compared to that, the prevalence rates range from 7.3–30.5 cases per 100,000 in Korea, China, Iran, Saudi Arabia, and Japan18. Strong genetic association between HLA-B*51 and BD has been identified in numerous ethnicities and counties3,18. We have previously reported that HLA-A*26 was significantly and independently associated with the risk of BD, apart from HLA-B*51 in the Japanese population12. Several studies including various ethnic groups and populations indicated both positive and negative associations between HLA-A*26 and BD4,5,6,7,8,11,12,19,20,21,22,23,24,25,26,27. In our current study, we aimed to summarize how HLA-A*26 is involved in the risk of BD within various geographical regions and ethnicities. In our current genotyping study, within a total of 611 BD patients, almost half of the patients did not carry HLA-B*51 alleles, and within these HLA-B*51-negative populations, almost half of the patients carried HLA-A*26. This indicated that almost a quarter of the total BD patients were independently influenced by HLA-A*26 in the Japanese population. Moreover, the OR of HLA-A*26 to BD was 2.12, and was as high as 3.10 within the HLA-B*51 negative subsets. As shown in Table 3, the haplotype frequencies retrieving HLA-A*26 and -*B locus indicated several supporting findings. According to the pooled database of HLA haplotypes in Japanese population, which include 8,138 families and 31,665 individuals, the haplotype frequency of HLA-A*26:01-B*51:01 was 0.46% and LD value was −0.219 and RD value was −0.324 (http://hla.or.jp, accessed December 2018). That indicated HLA-A*26:01 and B*51:01, the predominant suballeles in both BD patients and controls, were not in the linkage disequilibrium, which supported to re-confirm HLA-A*26 was an independent genetic risk factor apart from HLA-B*51. Within the HLA-B*51 negative subsets, some haplotypes retrieving HLA-A*26 and non- HLA-B*51 alleles showed positive association with susceptibility to BD, i.e., HLA-A*26 -B *39, *40, and *55. Of note, none of these -*B alleles showed significant independent risk association with BD in our current study. This may suggest the existence of other latent genetic risk alleles between HLA-A*26 and these -*B loci, for instance, possible involvement of retrieving HLA-*C, and -*E alleles28. Further studies will be necessary to clarify the possible involvement of these alleles to the susceptibility of BD.
As reported by Hughes, et al., no association was found between HLA-A*26 and BD in their larger number case-control study within the Turkish population. They concluded the lack of association owes to the low frequency of HLA-A*26 in the Turkish population29. On the other hand, Ombrello, et al. reported that the HLA-A*26 allele independently influenced the risk of BD apart from HLA-B*51 within another Turkish population, according to the HLA imputation analysis of their pooled GWAS results. They also clarified that five amino acid residues of HLA-B and two residues of HLA-A were significantly associated with BD. Id est, positions 97, 116, 152, and 67 of HLA-B and positions 161 and 97 of HLA-A have protective or risk effects to BD. Their studies suggested Arg 97 of HLA-A was significantly and independently associated with the risk of BD onset (OR = 1.3, 95% CI:1.1–1.4)26. Residue 97 of the HLA-A molecule is a component of the pocket F, located in the antigen-binding groove, and interact with the C-terminus of the presented peptide. Residue position 2 and the C-terminus of the presented peptide are called main anchor positions which define the binding affinity and specificity of HLA class I molecules30. HLA-A*26:01 has Arg at position 97 and that corresponds to the present risk residue mentioned above. HLA-B*51 has a Bw4 epitope in the α1-binding pocket which interact with the killer immunoglobulin-like receptors (KIR) 3DL1 and 3DS1 to regulate the activities of natural killer (NK) cells and a subset of cytotoxic T lymphocytes (CTLs)31. Their group also suggested a potential role of activating KIR3DS1 alleles in BD patients with ocular manifestations independent of HLA-B*5132. Though HLA-A*26 has a strong linkage with ocular manifestations in the Northeast Asian population, as far as KIR interaction is concerned, HLA-A*26 is not a direct ligand of KIR molecules. In another words, HLA-A*26 does not have an epitope which could be directly recognized by KIR to regulate the activation of NK cells or CTLs. That may suggest a different pathophysiology from HLA-B*51 related KIR interaction underlies the development of BD in the case of HLA-A*26 triggered KIR interaction pathways. Further studies are required to ascertain the hypothesis suggested above.
The worldwide distribution of HLA-A*26 is unique, as it is especially frequent in Northeast Asia, Oman, Georgia, and in the Israeli Jewish population (Fig. 4)13. In Northeast Asia, HLA-A*26 is more commonly found in the Western Pacific Rim, i.e. Taiwan, Ryukyu (Okinawa islands), and the Japan Islands. In our subgroup analysis arranged by geographical areas, positive association between HLA-A*26 and BD was found in Northeast Asia, but not in the Middle East or in Europe. This may owe to the higher distribution of this allele in the Northeast Asian region, especially in the Western Pacific Rim, we might be able to find the association between HLA-A*26 and BD in these areas more apparently.
In spite of the relatively high prevalence of HLA-A*26 in the Jewish population in Israel, no positive association between HLA-A*26 and BD was reported25. We believe this is due to the high heterogeneity of the Israeli Jewish population: A large proportion of them is of Ashkenazi Jewish origin, of which 21.7% were HLA-A*26 positive33. However, as reported in the previous papers, most of the Jewish BD patients were of non-Ashkenazi origin25,34. The lack of BD/HLA-A*26 association in this particular region might owe to the low frequency of HLA-A*26 in the non-Ashkenazi Jewish population. In addition, results of studies concerning the HLA genotyping of BD patients in Georgia and Oman were not found during our research.
In their GWAS results, Abi-Rached, et al. reported that between all three Neanderthals found in the Vindija Cave, northern Croatia, had the HLA-A*02, C*07:02, and C*16 alleles. Moreover, the pooling of these three Neanderthals sequence infers their possession of HLA-B*07, -B*51, and either HLA-A*26 or its close relative A*6635. It was suggested that the presence of HLA-B*51 in Eurasians, together with B*07, C*07:02, C*16:02, might be the result of admixture with the Neanderthals, which occurred after out-of-Africa migration until 40–30,000 years ago35,36. It is believed that the adaptive introgression of the Neandertal alleles has significantly involved in the construction of the modern humans’ immune systems and contributed to mediate the host defense immune mechanism against lethal infectious agents which the ancestors of modern humans newly encountered in the frontiers of the Eurasian continent during the period of the great human expansion. It is of interest that both HLA-B*5137 and HLA-A*26 alleles, which were identified as risk alleles of BD, might have been introgressed from the archaic human species, Neanderthals. Further studies will be needed for the better understanding of these mysterious relationships between HLA-B*51, HLA-A*26, Neanderthal alleles and BD. It is also worth noting that modern human’s ancestors lived in an environment where infectious diseases were mostly endemic, and under the influence of endemic environmental agents, infective microbial organisms led to genetic selection in order to produce more effective pro-inflammatory response to encourage the resistance to specific infections. However, these effective and high-potency immune systems could lead to immune-mediated inflammatory disease as an undesirable adverse effect38. Yersinia Pestis, the cause of Plague, is reported to have evolved near China, 20–15,000 years ago39. Yersinia Pestis has been a lethal infectious agent to human beings, and several studies have suggested HLA-B*51:01 had a protective role in the host response against the Yersinia Pestis infection40. It is assumed that the bottleneck effect following the high mortality rate of plague epidemics might have led the expansion of HLA-B*51:01 associated increased pro-inflammatory phenotypes and reservation of this complex genetically determined trait40. In other words, HLA-B*51 associated BD is suspected to be a secondary and undesirable side effect of the immunological advantages rendered by HLA-B*51 in activating NK cells and CTLs in response to these lethal infections37. Currently, we do not have enough knowledge on how HLA-A*26 contributed to protect modern human ancestors from life-threatening infections in the human immune history, we believe comprehensive investigations and better understanding of HLA-A*26 will lead us to a better understanding of BD pathogenesis.
In conclusion, we have performed the genotyping of Japanese BD patients and confirmed that HLA-A*26 was the susceptibility allele for BD in the Japanese population. Especially in the HLA-B*51-negative BD populations, HLA-A*26 was significantly associated with the onset of BD. A combination of our genotyping data with other data extracted from publications showed the association of BD and HLA-A*26 was geographically significant in Northeast Asia, but not in the Middle East or in Europe.
Methods
BD patients and controls
611 Japanese BD patients and 2,955 unrelated ethnically matched healthy controls were enrolled in this study. The diagnosis of BD was established according to standard criteria41 proposed by the Japan Behçet’s disease Research Committee. All procedures, data collection, and handling were performed according to the principles of the Good Clinical Practice and Declaration of Helsinki. This study was approved by the Research Ethics Committee of the Medical Faculty, Yokohama City University. The study details were explained to all participants before obtaining the informed consent for genetic screening. Blood samples were collected after study participants agreed and signed informed written consent. Banked and de-identified samples were used for this study.
HLA genotyping
We genotyped HLA-A and HLA-B alleles for 611 cases and 737 controls with Luminex reverse sequence-specific oligonucleotides and bead kits (One Lambda). For the remaining 2,218 controls, we performed an imputation analysis of HLA-A and HLA-B with our GWAS data using SNP2HLA42 and a reference panel of 530 pan-Asian samples43. The χ2 test was used to analyze categorical variables.
Literature Search and Meta-analysis
Meta-analysis was performed through the method proposed by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)44, using the Review Manager software (version 5.3) for statistical analysis. This protocol has been registered in the international prospective register of systematic reviews (PROSPERO) as number CRD42017073887. Relevant studies were identified using the PubMed/Medline, Embase, Web of Science, CENTRAL database and through manual literature search in December 2018; no language restriction was used for published studies. Studies fulfilling the following inclusion criteria were included in the meta-analysis: (1) case-control studies; (2) studies reporting an association between HLA and BD; (3) genetic association studies; and (4) independent studies without repeat reports on the same populations or subpopulations. In this study, we performed the quantitative synthesis of the extracted data which contain the results of phenotype frequency, hence extracted data which contain only allele frequency results without phenotype frequency results were included in qualitative synthesis, but not into the quantitative synthesis. Two of the authors (JN and GI) individually assessed the bias of included-studies using the Newcastle-Ottawa Scale45. Pooled ORs and the corresponding 95% CIs were synthesized with the random-effects model. Heterogeneity was assessed using the I2 statistic.
We also performed subgroup analysis to identify the possible underlying heterogeneity according to ethnic and geographic (Northeast Asia, Middle East, and Europe) repartitions of the BD patients in the studies. Publication bias was assessed using a funnel plot of the Review Manager software.
References
Sakane, T., Takeno, M., Suzuki, N. & Inaba, G. Behcet’s disease. The New England journal of medicine 341, 1284–1291, https://doi.org/10.1056/nejm199910213411707 (1999).
Kaklamani, V. G., Vaiopoulos, G. & Kaklamanis, P. G. Behcet’s Disease. Seminars in arthritis and rheumatism 27, 197–217 (1998).
de Menthon, M., Lavalley, M. P., Maldini, C., Guillevin, L. & Mahr, A. HLA–B51/B5 and the Risk of Behçet’s Disease: A Systematic Review and Meta-Analysis of Case–Control Genetic Association Studies. Arthritis and rheumatism 61, https://doi.org/10.1002/art.24642 (2009).
Kang, E. H. et al. Associations between the HLA-A polymorphism and the clinical manifestations of Behcet’s disease. Arthritis research & therapy 13, R49, https://doi.org/10.1186/ar3292 (2011).
Kuranov, A. B. et al. Behcet’s disease in HLA-B*51 negative Germans and Turks shows association with HLA-Bw4-80I. Arthritis research & therapy 16, https://doi.org/10.1186/ar4569 (2014).
Al-Okaily, F. et al. Genetic association of HLA-A*26,-A*31, and-B*51 with Behcet’s disease in Saudi patients. Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders 9, 167–173, https://doi.org/10.4137/CMAMD.S39879 (2016).
Mizuki, N. et al. A strong association between HLA-B*5101 and Behcet’s disease in Greek patients. Tissue antigens 50, 57–60 (1997).
Kaburaki, T. et al. Genetic association of HLA-A*2601 with ocular Behcet’s disease in Japanese patients. Clin Exp Rheumatol 28, S39–44 (2010).
Kurumi, A. Asociation of HLA-A26 with Behçet’s Disease in Japanese patients. Clinical rheumatology 23, 29–36 (2011).
Chung, Y. M. et al. Behcet’s disease with ocular involvement in Taiwan: a joint survey of six major ophthalmological departments. Journal of the Formosan Medical Association = Taiwan yi zhi 89, 413–417 (1990).
Elfishawi, M. M. et al. HLA Class I in Egyptian patients with Behçet’s disease: new association with susceptibility, protection, presentation and severity of manifestations. Immunological investigations, 1–9, https://doi.org/10.1080/08820139.2018.1517364 (2018).
Meguro, A. et al. Genetics of Behcet disease inside and outside the MHC. Ann Rheum Dis 69, 747–754, https://doi.org/10.1136/ard.2009.108571 (2010).
Middleton, D., Menchaca, L., Rood, H. & Komerofsky, R. New allele frequency database: http://www.allelefrequencies.net. Tissue antigens 61, 403–407, https://doi.org/10.1034/j.1399-0039.2003.00062.x (2003).
Azizlerli, G. et al. Prevalence of Behcet’s disease in Istanbul, Turkey. International journal of dermatology 42, 803–806 (2003).
Cakir, N. et al. Prevalence of Behcet’s disease in rural western Turkey: a preliminary report. Clinical and experimental rheumatology 22, S53–55 (2004).
Idil, A. et al. The prevalence of Behcet’s disease above the age of 10 years. The results of a pilot study conducted at the Park Primary Health Care Center in Ankara, Turkey. Ophthalmic epidemiology 9, 325–331 (2002).
Yurdakul, S. et al. The prevalence of Behcet’s syndrome in a rural area in northern Turkey. The Journal of rheumatology 15, 820–822 (1988).
Piga, M. & Mathieu, A. Genetic susceptibility to Behcet’s disease: role of genes belonging to the MHC region. Rheumatology (Oxford, England) 50, 299–310, https://doi.org/10.1093/rheumatology/keq331 (2011).
Pirim, I., Atasoy, M., Ikbal, M., Erdem, T. & Aliagaoglu, C. HLA class I and class II genotyping in patients with Behcet’s disease: a regional study of eastern part of Turkey. Tissue antigens 64, 293–297, https://doi.org/10.1111/j.1399-0039.2004.00280.x (2004).
Piga, M. et al. Genetics of Behcet’s disease in Sardinia: two distinct extended HLA haplotypes harbour the B*51 allele in the normal population and in patients. Clin Exp Rheumatol 30, S51–56 (2012).
Kera, J. et al. Significant associations of HLA-B*5101 and B*5108, and lack of association of class II alleles with Behcet’s disease in Italian patients. Tissue antigens 54, 565–571 (1999).
Mizuki, N. et al. HLA class I genotyping including HLA-B*51 allele typing in the Iranian patients with Behcet’s disease. Tissue antigens 57, 457–462 (2001).
Yabuki, K. et al. HLA class I and II typing of the patients with Behcet’s disease in Saudi Arabia. Tissue antigens 54, 273–277 (1999).
Mizuki, N. et al. Sequencing-based typing of HLA-B*51 alleles and the significant association of HLA-B*5101 and -B*5108 with Behcet’s disease in Greek patients. Tissue antigens 59, 118–121 (2002).
Arber, N., Klein, T., Meiner, Z., Pras, E. & Weinberger, A. Close association of HLA-B51 and B52 in Israeli patients with Behcet’s syndrome. Ann Rheum Dis 50, 351–353 (1991).
Ombrello, M. J. et al. Behcet disease-associated MHC class I residues implicate antigen binding and regulation of cell-mediated cytotoxicity. Proc Natl Acad Sci USA 111, 8867–8872, https://doi.org/10.1073/pnas.1406575111 (2014).
Montes-Cano, M. A. et al. HLA and non-HLA genes in Behcet’s disease: a multicentric study in the Spanish population. Arthritis research & therapy 15, R145, https://doi.org/10.1186/ar4328 (2013).
Seo, J. et al. Association of CD94/NKG2A, CD94/NKG2C, and its ligand HLA-E polymorphisms with Behcet’s disease. Tissue antigens 70, 307–313, https://doi.org/10.1111/j.1399-0039.2007.00907.x (2007).
Hughes, T. et al. Identification of multiple independent susceptibility loci in the HLA region in Behcet’s disease. Nat Genet 45, 319–324, https://doi.org/10.1038/ng.2551 (2013).
Sidney, J., Peters, B., Frahm, N., Brander, C. & Sette, A. HLA class I supertypes: a revised and updated classification. BMC immunology 9, 1, https://doi.org/10.1186/1471-2172-9-1 (2008).
Sanjanwala, B., Draghi, M., Norman, P. J., Guethlein, L. A. & Parham, P. Polymorphic sites away from the Bw4 epitope that affect interaction of Bw4+ HLA-B with KIR3DL1. Journal of immunology (Baltimore, Md.: 1950) 181, 6293–6300 (2008).
Erer, B. et al. Evaluation of KIR3DL1/KIR3DS1 polymorphism in Behcet’s disease. Genes and immunity 17, 396–399, https://doi.org/10.1038/gene.2016.36 (2016).
Brandsen, R. E. et al. SAPHO syndrome. Dermatology (Basel, Switzerland) 186, 176–180, https://doi.org/10.1159/000247340 (1993).
Krause, I. et al. Prevalence and clinical aspects of Behcet’s disease in the north of Israel. Clin Rheumatol 26, 555–560, https://doi.org/10.1007/s10067-006-0349-4 (2007).
Abi-Rached, L. et al. The Shaping of Modern Human Immune Systems by Multiregional Admixture with Archaic Humans. Science (New York, N.Y.), https://doi.org/10.1126/science.1209202 (2011).
Green, R. E. et al. A draft sequence of the Neandertal genome. Science (New York, N.Y.) 328, 710–722, https://doi.org/10.1126/science.1188021 (2010).
Ashouri, E. et al. HLA class I variation in Iranian Lur and Kurd populations: high haplotype and allotype diversity with an abundance of KIR ligands. HLA 88, 87–99, https://doi.org/10.1111/tan.12852 (2016).
Le Souef, P. N., Goldblatt, J. & Lynch, N. R. Evolutionary adaptation of inflammatory immune responses in human beings. Lancet 356, 242–244 (2000).
Morelli, G. et al. Yersinia pestis genome sequencing identifies patterns of global phylogenetic diversity. Nat Genet 42, 1140–1143, https://doi.org/10.1038/ng.705 (2010).
Piga, M. & Mathieu, A. The origin of Behcet’s disease geoepidemiology: possible role of a dual microbial-driven genetic selection. Clinical and experimental rheumatology 32, S123–129 (2014).
Mizushima, Y. Recent research into Behcet’s disease in Japan. International journal of tissue reactions 10, 59–65 (1988).
SNP2HLA. Imputation of Amino Acid Polymorphisms in Human Leukocyte Antigens. http://software.broadinstitute.org/mpg/snp2hla/.
Okada, Y. et al. Risk for ACPA-positive rheumatoid arthritis is driven by shared HLA amino acid polymorphisms in Asian and European populations. Hum Mol Genet 23, 6916–6926, https://doi.org/10.1093/hmg/ddu387 (2014).
Shamseer, L. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed.) 350, g7647, https://doi.org/10.1136/bmj.g7647 (2015).
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Acknowledgements
This study was supported by the Japan Society for the Promotion of Science (JSPS) Postdoctoral Fellowship for Research Abroad (Kaitoku-NIH, #24112 to JN). The funding source had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
J.N. contributed for conception, data extraction, analysis, and drafting. G.I. worked for data extraction and drafting. A.M. and M.O. contributed for data acquisition and interpretation of the results. T.M. and A.M. provided statistical advices. M.T., Y.M., K.Y., T.Y., T.K. and N.M. provided general management of the study. M.O., G.I. and N.M. critically revised the protocol and main manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakamura, J., Meguro, A., Ishii, G. et al. The association analysis between HLA-A*26 and Behçet’s disease. Sci Rep 9, 4426 (2019). https://doi.org/10.1038/s41598-019-40824-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40824-y
- Springer Nature Limited