Abstract
This study aimed to assess the feasibility of GP73 as a diagnostic marker for liver inflammation and fibrosis in chronic HBV patients with normal or slightly raised ALT (<2 ULN) and to develop models based on GP73 and other biochemical parameters to improve diagnostic accuracy. Serum GP73 levels were analyzed in 220 chronic HBV patients with normal or slightly raised ALT who underwent liver biopsy. The results showed that the area under the receiver operating characteristic (ROC) curve (AUC) was 0.806 for predicting significant liver inflammation (≥G2), while it was 0.742 for predicting significant fibrosis (≥S2). These results suggest that GP73 has higher diagnostic value for liver inflammation than liver fibrosis. Combining GP73, AST and ALB, as a diagnostic model for predicting significant liver inflammation, resulted in superior diagnostic performance over GP73 alone (AUC value increased from 0.806 to 0.854, z = 2.299, P = 0.021). By applying this diagnostic model, over 80% of chronic HBV patients with normal or slightly raised ALT will be correctly identified and hence avoid delay in diagnosis and treatment. In conclusion, GP73 would be an additional serum marker for predicting liver inflammation and fibrosis in chronic HBV patients with normal or slightly raised ALT.
Similar content being viewed by others
Introduction
Hepatitis B virus (HBV) is one of the most common infectious diseases in the world with more than 240 million people infected with HBV worldwide. Infection with HBV can be either acute or chronic. In adults, HBV infections have a relatively low rate of chronicity (around 5%), while it results in a high persistence rate in neonates1,2. Although, most chronic infections are asymptomatic, HBV carriers are still at risk of hepatic inflammation and fibrosis, which can lead to advanced liver diseases including cirrhosis and hepatocellular carcinoma3. Therefore, close follow up and monitoring is recommended for HBV carriers to avoid disease progression. Accordingly, it is highly recommended that HBV carriers with moderate or severe chronic hepatitis, indicated by abnormal levels of alanine-aminotransferase (ALT, ULN < 40 U/L), should receive antiviral therapy4. In this context, it is important to note that although the serum level of ALT is the most commonly used parameter for assessing hepatitis activity, it has been reported that 24.6% to 61.9% of chronic HBV infected patients with either normal or slightly raised ALT (<2 ULN) were diagnosed with moderate or severe hepatic inflammation and/or fibrosis5,6,7. Therefore, it is quite possible that patients with ongoing liver injury might not be identified due to having normal levels of ALT, and therefore not receiving the benefit of antiviral therapy. On the other hand, liver biopsy is the current “gold standard” for evaluating hepatic pathology. However, the procedure is limited by its invasive nature and the risk of complications8,9. Therefore, identification of new surrogate biomarkers with high diagnostic and prognostic efficiencies for liver injury is urgently needed.
Golgi Protein-73 (GP73), a novel type II Golgilocalized integral membrane protein also known as GOLPH2 or GOLM1, is predominantly expressed in epithelial cells of many human tissues10. Serum GP73 levels were found to be significantly raised in patients with a variety of acute or chronic liver diseases11,12, and especially in patients with hepatocellular carcinoma13. In our previous studies, we found that changes in serum GP73 levels were closely associated with changes in the degree of liver injury since serum GP73 levels were positively correlated with liver pathological grading and staging in patients with chronic HBV infection14,15. Whether GP73 could be used for liver inflammation and fibrosis in chronic HBV infected patients with normal or slightly raised ALT has not been reported.
In an attempt to identify a non-invasive biomarker for diagnosis of liver inflammation and fibrosis in HBV patients with normal or slightly raised ALT, we investigated the diagnostic performance of serum GP73. Ultimately, we proposed two diagnostic models consisting of combined biochemical parameters to improve the diagnostic accuracy of liver inflammation and fibrosis.
Results
Patient Characteristics
A total of 220 patients with chronic HBV infection and normal or slightly raised ALT (<2 ULN) were enrolled. The demographic and clinical characteristics of the enrolled patients at the time of liver biopsy were listed in Table 1. The majority of the patients (64.6%) had no-activity or minimal (G0-1) liver inflammation, while only 2% had severe inflammation grade (G4). Additionally, nearly half of the patients (48%) had stageS0-1 fibrosis.
Univariate and Multivariate Analysis
Based on inflammation grade, all patients were divided to two groups: 1) patients with no significant inflammation (<G2); and 2) patients with significant inflammation (≥G2). Demographic and biochemical parameters were compared between both groups (Table 2).While all variables, except age, sex, TBIL, ALP, HBV DNA, HBeAg and Anti-HBe, were significantly different between the two groups by univariate analysis, only GP73, ALB and AST were identified by multivariable analysis as independent factors significantly associated with the grade of liver inflammation (Table 2). Similarly, based on fibrosis stage, patients were divided into two groups: 1) patients with no significant fibrosis (<S2); and 2) patients with significant fibrosis (≥S2). When demographic and biochemical parameters were compared between the both groups (<S2 vs. ≥S2), all variables except sex, ALB, ALT, ALP, HBV DNA, HBeAg and Anti-HBe, were significantly different between the two groups by univariate analysis (Table 3). Subsequently, multivariate analysis identified GP73 and PLT count as independent factors significantly associated with the stage of liver fibrosis (Table 3).
Estimation of the Models
Next, we developed two score systems using the logarithmic values (Ln) of significant independent variables and their coefficients for predicting inflammation or fibrosis based on the following binary logistic regression: Model1 (Inflammation Probability) = 14.66 + 2.4 Ln(GP73) + 1.99 Ln(AST) − 7.15 Ln(ALB) (Table 4); and Model2 (Fibrosis Probability) = 9.42 + 1.89 Ln(GP73) − 2.63 Ln(PLT) (Table 5).
Comparison of Diagnostic Efficacy
To estimate the optimal cut off value of GP73 for predicting significant liver inflammation (≥G2) or significant liver fibrosis (≥S2), the ROC curve analysis was used. This analysis identified 85.7 ng/ml as an optimal cut off value of GP73 to distinguish between patients with and without significant liver inflammation among HBV patients with normal of slightly raised ALT levels. A GP73 cut off value of 85.7 ng/ml resulted in an AUC of 0.806 which was significantly higher than that of ALT (0.616) (z = 3.917, P < 0.001), and the sensitivity and specificity were 43.59% and 97.18% respectively (Fig. 1A and Table 6). Interestingly, using 85.7 ng/ml as a cut off for GP73, 34 (43.59%) of the 78 patients with significant inflammation by liver biopsy were correctly identified, while only four (2.82%) of the 142 patients with serum GP73 level higher than 85.7 ng/ml had no significant inflammation by liver biopsy. When significant liver fibrosis was considered, the ROC analysis identified 84.49 ng/ml as an optimal cut off value of GP73 to distinguish between patients with and without significant liver fibrosis. The GP73 cut off value of 84.49 ng/ml resulted in an AUC of 0.742, which also significantly higher than that of ALT (0.556), and the sensitivity and specificity were 30.70% and 96.23% respectively (Fig. 1B and Table 7). Using 84.49 ng/ml as a cut off value for GP73, significant fibrosis could be predicted in only 35 (30.7%) of 114 patients with significant fibrosis determined by liver biopsy, reflecting the low sensitivity of this cut off value.
When ROC analysis was performed on Model1 consisting of combined GP73, ALB and AST for prediction of significant liver inflammation, a cut off value of 5.31 was identified. This cut off value produced an AUC of 0.854 (Fig. 1A and Table 6), which was significantly higher than that of GP73 (0.806) alone (z = 2.299, P = 0.021) for prediction of significant liver inflammation. Sensitivity, specificity, PPV, NPV, and diagnosing accuracy of the cut off value of 5.31 for Model1 were 62.82%, 93.66%, 84.5%, 82.1% and 82.7%, respectively. When the cutoff value was set at 4.18, the sensitivity, specificity, PPV and NPV were 82.05%, 75.35%, 64.64% and 81.06%, respectively. Accordingly, 64 (82.05%) of the 78 patients with significant inflammation by liver biopsy were correctly identified. When Model2 consisting of combined GP73 and PLT for prediction of the stage of liver fibrosis was considered, ROC analysis identified 3.7 is an optimal cut off value. This cut off value produced an AUC of 0.778 (Fig. 1B and Table 7), which was higher than that of GP73 (0.742) alone, however the difference was not significant (z = 1.71, P = 0.087). Sensitivity, specificity, PPV, NPV and diagnosing accuracy of the cut off value of 3.7 for Model2 were 50%, 91.51%, 86.4%, 63% and 69.55% respectively.
Discussion
A critical decision for chronic HBV infected patients is when to initiate antiviral therapy. Usually, the antiviral therapy is initiated in patients showing at least moderate hepatocyte injury (G2) and notably raised ALT levels (>2 ULN)16. However, the level of serum ALT may not reflect the correct nature of the hepatic pathology17. If strict adherence to practice guidelines of chronic hepatitis B is applied, some chronic HBV infected patients with normal or slightly raised ALT (<2 ULN), but with hepatic inflammation and/or fibrosis might not be identified and be deprived the benefit of antiviral treatment. In several clinical settings, GP73 was shown to be upregulated in a variety of liver diseases, including alcohol-induced liver disease, virus-induced hepatitis (e.g., hepatitis B and C), autoimmune hepatitis, liver cirrhosis, and hepatocellular carcinoma cells (HCC)18,19,20. It was reported that serum GP73 levels were correlated with fibrosis stage and would be a robust biomarker for diagnosis of significant fibrosis in patients with chronic HBV infection21,22. However, in our previous studies, we found that the correlation between GP73 and liver inflammation was stronger than that of liver fibrosis15. Interestingly, in the present study, serum GP73 was able to predict significant liver inflammation and fibrosis in chronic HBV infected patients with normal or slightly raised ALT. Serum GP73 level demonstrated a high specificity (97.18%) for predicting liver inflammation when the cutoff value was set at 85.7 ng/ml, and the rate of misdiagnosis was only 2.82%. For predicting liver fibrosis, serum GP73 level also demonstrated a high specificity (96.23%) for predicting liver fibrosis when the cutoff value was set at 84.49 ng/ml. Notably, our current results showed that the sensitivity, NPV and diagnosing accuracy of GP73 for predicting liver inflammation was higher than those for predicting liver fibrosis. Moreover, the AUC of GP73 for predicting liver inflammation was higher than for predicting fibrosis (0.806 vs 0.742). Therefore, these results support our previous findings that serum GP73 level is more closely related to hepatic inflammation than to liver fibrosis. What cause the elevation of serum GP73 in liver diseases, hepatocellular injury or fibrosis is still unknown. It was reported that the primary triggers of GP73 expression was the progressive tissue remodeling and fibrogenesis in chronic liver disease19. It was also reported that the expression of GP73 could be induced by the proinflammatory cytokines IL-623 and interferon gamma (IFN-γ)18 in vitro, with serum GP73 levels possibly upregulated under inflammatory conditions12,24 in vivo. Our findings supported the statement that the elevation of serum GP73 level was triggered by liver inflammatory injury. Since hepatic fibrosisis a common consequence of liver inflammation, we hypothesized that the increased serum GP73 levels in patients with hepatic fibrosis were also attributed to hepatocellular injury. When liver injury occurs, the hepatic macrophages (Kupffer cells) produce a variety of growth and immunomodulating mediators including inflammatory cytokines, especially TNF-α, which has been linked to the pathogenesis of hepatocyte apoptosis and hepatic injury25,26,27. Subsequently, the expression of GP73 in hepatocytes is upregulated by inflammatory cytokines and then released into the extracellular space via proprotein convertase (PC) mediated cleavage, which results in increased GP73 levels in the blood28. Furthermore, in our previous studies, we also found that there were significant positive correlations between serum GP73 levels and the expression levels of TNF-α, IL-2 and IL-12 in chronic HBV infected patients with complete response to IFN treatment29. This supports the link between GP73 and inflammation.
To improve the diagnostic accuracy of liver inflammation or fibrosis in HBV patients with normal or slightly raised ALT level, biomathematical models were established using a combination of factors identified as independent predictors in multivariate analysis. Model1 consisted of a combination of GP73, ALB and AST, which significantly improved the detection of liver inflammation in patients with normal or slightly raised serum ALT, compared to GP73 alone (AUC value increased from 0.806 to 0.854, p < 0.05). The sensitivity of Model1 was increased to 62.82% compared to GP73 (43.59%), while maintaining a high specificity (93.66%). When the cutoff value was set at 4.18, the sensitivity was further increased to 82.05%, although with a relatively low specificity (75.35%). This indicates that over 80% of chronic HBV infected patients with normal or slightly raised ALT could avoid delays in diagnosis and treatment. Model2 consisted of a combination of GP73 and PLT for prediction of significant fibrosis. This model also improved diagnostic performance, however, this improvement was not significantly different from the diagnostic performance of GP73 alone.
In conclusion, GP73 could be used as an additional serum marker for the diagnoses of liver inflammation and fibrosis in chronic HBV infected patients with normal or slightly raised ALT. Moreover, the diagnostic performance of GP73 for liver inflammation is stronger than for liver fibrosis. The combination of serum levels of GP73, AST and ALB establish a diagnostic model that significantly improved the diagnostic performance for liver inflammation in patients with normal or slightly raised serum ALT. By applying Model1, over 80% of chronic HBV infected patients with normal or slightly raised ALT could be correctly identified and avoid delay in diagnosis and treatment.
Patients and Methods
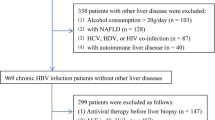
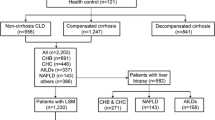
Patients
This retrospective study was carried out in accordance with the institutional ethical guidelines which was approved by the Ethics Committee of the 910 Military hospital, Quanzhou, China. Informed consents were collected from all patients enrolled in this study. Patients with chronic HBV infection who underwent liver biopsy in the Clinical Liver Disease Center (180 Military hospital) between January 2012 and November 2016 were recruited, and medical records were reviewed retrospectively. All patients were selected corresponding to the following criteria: (1) HBsAg and HBV DNA positivity for more than 6 months; (2) normal or slightly raised serum ALT (<2 ULN, ULN < 40 U/L); (3) absence of co-infection with hepatitis C or hepatitis D; (4) absence of HIV, pregnancy, diabetes, thyroid disease, tuberculosis, autoimmune liver diseases and serious cardiac, lung, kidney, nerve and mental diseases, haemochromatosis, or Wilson disease; (5) absence of concomitant drug or alcohol related chronic liver disease; and (6) absence of fatty liver or non-alcoholic steatohepatitis.
Histologic Grading and Staging
After collecting patient written informed consent, ultra-sonographic-guided liver biopsy was performed using 16G disposable needles (C. R. Bard, Inc., Murray Hill, NJ, USA) according to a standardized protocol. A minimum of 15 mm of liver tissue with at least six portal tracts was required for diagnosis. Specimens were fixed, paraffin-embedded, and stained with hematoxylin-eosin, reticular fiber stain and Masson’s trichrome stain, and examined under a light microscope (Olympus, BX51). The liver biopsies were evaluated independently in a blinded fashion by the same pathologist as for the clinical data. Histological grading of inflammation and staging of liver fibrosis were determined according to Scheuer’s classification30: G0 = no activity, G1 = minimal activity, G2 = mild activity, G3 = moderate activity, and G4 = severe activity; S0 = no fibrosis, S1 = expansion of portal fibrotic area, S2 = fibrosis observed in and around portal area, may have formed fibrous septum, S3 = clear fibrosis and hepatic lobule structure disorder but no cirrhosis, and S4 = early cirrhosis.
Biochemical Measurements and Detection of Serum GP73 Levels
Demographic data were recorded for all patients. Biochemical and hematologic investigations were performed during the week before liver biopsy. Patients’ biochemical parameters including ALT, total bilirubin(TBIL), albumin(ALB), aspartate aminotransferase(AST), γ-glutamyltransferase(GGT), alkaline phosphatase(ALP), and cholinesterase(CHE) were detected using standard hospital-based laboratory procedures on a ROCHE Modular P800 Automatic Biochemical Analyzer (Roche Diagnostics, Mannheim, Germany). Platelet counts(PLT) were detected by an automatic blood cell analyzer (Sysmex XN-3000, Japan). Quantitative enzyme-linked immunosorbent assay (ELISA) kits (Hotgen Biotech Co. Ltd., Beijing, China) were used to detect the serum GP73 levels according to manufacturer’s instructions. Hepatitis B viral DNA (HBV DNA) levels were determined by quantitative PCR (Shenyou Biotec, Shanghai, China) using the Mx3000P System (Agilent Technologies, Santa Clara, CA, USA). Hepatitis B virus surface antigen (HBsAg), Hepatitis B virus e antigen (HBeAg) and hepatitis B virus e antibody (Anti-HBe) levels were determined by electrochemiluminescence immunoassay (Elecsys 2010; Roche Diagnostics, Indianapolis, IN, USA).
Statistical Analysis
Statistical analyses of the data were performed using SPSS 19.0 (SPSS, Chicago, IL, USA) and STATA 11.0 programs. Continuous variables were expressed as the median (centile 25; centile 75). Kolmogorov-Smirnov tests were used to assess for normality of the data. For continuous variables, the differences were assessed using independent samples t-tests in normal distribution data and Mann-Whitney U-test in abnormal distribution data. For categorical variables, the differences were assessed using Chi-square tests. Then, all variables were included in univariate and multivariate forward stepwise logistic regression analysis to determine the independent predictors of the absence or presence of significant inflammation or fibrosis. Mathematical models (inclusion criteria: P < 0.05, exclusion criteria: P > 0.05) were established by modeling the values of the independent predictors and their coefficients of regression. For each of the models, the diagnostic values were assessed using the area under the receiver operating characteristic (ROC) curves. Areas under the ROC (AUC) of different diagnostic methods were compared using the method of Hardey. Detailed diagnostic values were evaluated by sensitivity, specificity, positivepredictive value (PPV), negative predictive value (NPV), Youden index and accuracy.
References
McMahon, B. J. Natural history of chronic hepatitis B. Clin Liver Dis. 14, 381–96 (2010).
Busca, A. & Kumar, A. Innate immune responses in hepatitis B virus (HBV) infection. Virol J. 7(11), 22 (2014).
Yuen, M. F. & Lai, C. L. Treatment of chronic hepatitis B. Lancet Infect Dis. 1, 232–41 (2001).
European Association for the Study of the Liver. EASL2017 Clinical Practice Guidelines on the management of hepatitis B virusinfection. J Hepatol. 67, 370–398 (2017).
Wong, S. N. & Lok, A. S. Treatment of hepatitis B: who, when, and how? Arch InternMed. 166, 9–12 (2006).
Park, J. Y. et al. High prevalence of significant histology in asymptomatic chronic hepatitis B patients with genotype C and high serum HBV DNA levels. J Viral Hepat. 15, 615–21 (2008).
Cheong, J. Y. et al. Serum markers for necroinflammatory activity in patients with chronic viral hepatitis and normal or mildly elevated aminotransferase levels. Liver Int. 31, 1352–8 (2011).
Rockey, D. C., Caldwell, S. H., Goodman, Z. D., Nelson, R. C. & Smith, A. D. American Association for the Study of Liver Diseases. Liver biopsy. Hepatology. 49, 1017–44 (2009).
Tong, M. J., Hsien, C., Hsu, L., Sun, H. E. & Blatt, L. M. Treatment recommendations for chronic hepatitis B: an evaluation of current guidelines based on a natural history study in the United States. Hepatology. 48, 1070–8 (2008).
Kladney, R. D. et al. GP73, a novel Golgi-localized protein upregulated by viral infection. Gene. 249, 53–65 (2000).
Liu, X. et al. Golgi protein 73(GP73), a useful serum marker in liver diseases. Clin Chem Lab Med. 49, 1311–6 (2011).
Wright, L. M. et al. Hepatocyte GP73 expression in Wilson disease. J Hepatol. 51, 557–64 (2009).
Sun, Y. et al. Increased Golgi protein 73 expression in hepatocellular carcinoma tissue correlates with tumor aggression but not survival. J Gastroenterol Hepatol. 26, 1207–12 (2011).
Xu, Z. et al. Serum Golgi protein 73(GP73) is a diagnostic and prognostic marker of chronic HBV liver disease. Medicine (Baltimore). 94, e659 (2015).
Xu, Z. et al. Serum Golgi protein 73 levels and liver pathological grading in cases of chronic hepatitis B. Mol Med Rep. 11, 2644–52 (2015).
Sebagh, M. et al. Twenty-year protocol liver biopsies: Invasive but useful for the management of liver recipients. J Hepatol. 56, 840–7 (2012).
Zoulim, F., Perrillo, R. & Hepatitis, B. Reflections on the current approach toantiviral therapy. J Hepatol. 48 Suppl 1, S2–19 (2008).
Kladney, R. D., Cui, X., Bulla, G. A., Brunt, E. M. & Fimmel, C. J. Expression of GP73, a resident Golgi membrane protein, in viral and nonviral liver disease. Hepatology. 35, 1431–40 (2002).
Iftikhar, R. et al. Disease- and cell-specific expression of GP73 in human liver disease. Am J Gastroenterol. 99, 1087–95 (2004).
Wang, F. et al. Epithelium-Specific ETS (ESE)-1 upregulated GP73 expression in hepatocellular carcinoma cells. Cell Biosci. 4, 76 (2014).
Wei, H. et al. Serum GP73, a marker for evaluating progression in patients with chronic HBV infections. PLoSOne. 8, e53862 (2013).
Cao, Z. et al. Algorithm of Golgi protein 73 and liver stiffness accurately diagnoses significant fibrosis in chronic HBV infection. Liver Int. 37, 1612–1621 (2017).
Liang, H. et al. Interleukin-6 and oncostatin M are elevated in liver diseasein conjunction with candidate hepatocellular carcinoma biomarker GP73. CancerBiomark. 11, 161–71 (2012).
Wright, L. M., Yong, S., Picken, M. M., Rockey, D. & Fimmel, C. J. Decreased survival and hepato-renal pathology in mice with C-terminally truncated GP73 (GOLPH2). Int J ClinExpPathol. 2, 34–47 (2009).
Mignon, A. et al. LPS challenge in D-galactosamine-sensitized mice accounts forcaspase-dependent fulminant hepatitis, not for septic shock. Am J RespirCritCare Med. 159, 1308–15 (1999).
Sekiyama, K. D., Yoshiba, M. & Thomson, A. W. Circulating proinflammatory cytokines(IL-1 beta, TNF-alpha, and IL-6) and IL-1 receptor antagonist (IL-1Ra) infulminant hepatic failure and acute hepatitis. ClinExpImmunol. 98, 71–7 (1994).
Furuya, S. et al. Interleukin 17A plays a role in lipopolysaccharide/D-galactosamine-induced fulminant hepatic injury inmice. J Surg Res. 199, 487–93 (2015).
Bachert, C., Fimmel, C. & Linstedt, A. D. Endosomal trafficking and proprotein convertase cleavage of cis Golgi protein GP73 produces marker for hepatocellular carcinoma. Traffic. 8, 1415–23 (2007).
Meijuan, W., Xiaoman, Z. & Zhengju, X. Correlation of GP73 and cytokines before antiviral therapyin patients with chronic hepatitis B. Chin J ExpClin. Infect Dis (Electronic Edition). 11, 141–145 (2017).
Scheuer, P. J. The nomenclature of chronic hepatitis: time for a change. J Hepatol. 22, 112–4 (1995).
Acknowledgements
This research was supported by grant from the Science and Technology Project of Quanzhou (No. 2017Z018) to Dr. Zhengju Xu.
Author information
Authors and Affiliations
Contributions
Meijuan Wei and Zhengju Xu designed research and drafting of the manuscript: Yuxia Chen analysis and interpretation of data; Xingnan Pan revised Critical of the manuscript for important intellectual contentt: Bishuang Yang, LiGuan Liu and Xiaoman Zhang performed statistical analysis.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wei, M., Xu, Z., Pan, X. et al. Serum GP73 - An Additional Biochemical Marker for Liver Inflammation in Chronic HBV Infected Patients with Normal or Slightly Raised ALT. Sci Rep 9, 1170 (2019). https://doi.org/10.1038/s41598-018-36480-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-36480-3
- Springer Nature Limited