Abstract
Traumatic brain injury (TBI) commonly results in cognitive and psychiatric problems. Cognitive impairments occur in approximately 30% of patients suffering from mild TBI (mTBI), and correlational evidence from clinical studies indicates that substance abuse may be increased following mTBI. However, understanding the lasting cognitive and psychiatric problems stemming from mTBI is difficult in clinical settings where pre-injury assessment may not be possible or accurate. Therefore, we used a previously characterized blast model of mTBI (bTBI) to examine cognitive- and addiction-related outcomes. We previously demonstrated that this model leads to bilateral damage of the medial prefrontal cortex (mPFC), a region critical for cognitive function and addiction. Rats were exposed to bTBI and tested in operant learning tasks several weeks after injury. bTBI rats made more errors during acquisition of a cue discrimination task compared to sham treated rats. Surprisingly, we observed no differences between groups in set shifting and delayed matching to sample, tasks known to require the mPFC. Separate rats performed cocaine self-administration. No group differences were found in intake or extinction, and only subtle differences were observed in drug-primed reinstatement 3–4 months after injury. These findings indicate that bTBI impairs acquisition of a visual discrimination task and that bTBI does not significantly increase the ability of cocaine exposure to trigger drug seeking.
Similar content being viewed by others
Introduction
Recent estimates indicate that over two million Americans suffer a traumatic brain injury (TBI) each year1. Two of the most prevalent chronic outcomes of TBI are cognitive and psychiatric problems, and these are cited as the major contributor to long-term disability2,3,4. Substance abuse is one of the most common psychiatric problems following TBI, with estimated prevalence rates of 5–28%5,6,7,8 and relative risk of 1.8 for substance abuse at 13–24 months following injury9.
Among TBIs, approximately 75% are categorized as mild (mTBI)10. The American Congress of Rehabilitation Medicine has defined mild TBI as head trauma resulting in one of the following: loss of consciousness for less than 30 min, alteration of mental state for up to 24 h with a Glasgow coma score ≥13, or pre- or post-traumatic amnesia11. This definition roughly coincides with categorizations of mild head injury and concussion12,13. mTBI symptoms commonly resolve within a few weeks or months following injury, and many studies report 30% or fewer patients exhibit cognitive or behavioral problems that persist longer than three months14,15,16. However, a recent scoping review suggests that approximately 50% of mTBI patients may exhibit cognitive problems beyond three months17. Cognitive difficulties are one of the most commonly reported persistent symptoms in mTBI sufferers14,17. In a study of 122 mTBI patients, 26% reported cognitive impairment three months post-injury, and neuropsychological testing revealed impairment in 30% of patients18. Meta-analysis of 39 studies including over 2600 cases found that the overall effect of mTBI on cognitive function three months post-injury was low (d = 0.04), however the effect was much larger (d = 0.74) when analysis was restricted to clinic-based studies19. Among cognitive impairments reported, executive dysfunction is one of the most commonly reported persistent symptoms in mild and non-mild TBI20,21. Executive dysfunction can manifest in problems with adaptability, problem solving, and mental flexibility, which commonly disrupts interpersonal relationships and other aspects of quality of life20.
There is also evidence of increased substance abuse following mTBI, although interpretation is complicated by the fact that many studies either combine injuries of varying severity or do not report injury severity9,22. Nonetheless, compelling evidence comes from studies specifically studying mTBI. In a study of nearly two million discharged military personnel, the relative risk of discharge for alcoholism or drug use was 2.6 higher for those suffering from mTBI23. A longitudinal study of subjects who suffered an mTBI at five years of age or younger found an odds ratio of 3.6 for likelihood of substance abuse during adolescence, several years following the injury24.
Blast-related TBIs are commonly sustained in modern combat, urban terrorist attacks, and industrial accidents25. Blast is the leading cause of TBI in recent military conflicts; a 2010 report noted that 69% of TBIs occurring in operation enduring freedom/operation Iraqi freedom, now operation new dawn (OEF/OIF/OND), were from blast exposure26, and the estimated prevalence of blast-related TBI in OEF/OIF/OND personnel is approximately 20%27,28,29. Like non-blast mTBI, cognitive problems are among the most frequently self-reported enduring symptoms following blast mTBI29,30. Despite the high prevalence of self-reported cognitive problems following blast injury in military personnel, neuropsychological testing has not always shown mTBI-associated deficiencies, or that deficiencies may be confounded by comorbid Axis I psychopathologies such as PTSD or depression31,32,33,34. As with non-blast TBI (described above), there is evidence that executive dysfunction may be specifically altered in blast mTBI35.
Many factors complicate our understanding of cognitive and addiction-related sequelae of brain injury. In clinical studies, factors such as pre-injury cognitive performance or substance use history are often unclear36. Outcomes following injury are often self-reported, and cognitive function may not be rigorously tested following injury. On the other hand, biases such as the “nocebo effect” (outcomes associated with expectations of negative outcomes37), diagnosis threat (outcomes shaped by negative expectations associated with diagnosis38), and the potential for secondary gain from injury-related disability may overestimate rates of chronic impairment39. Furthermore, cognitive dysfunction and psychostimulant abuse are common co-morbidities40,41, and this relationship has been modeled in preclinical studies42. Preclinical studies can address many of these problems by controlling pre-injury factors and removing biases inherent in human studies.
Our blast model of mTBI (bTBI) has been demonstrated to produce cognitive and behavioral alterations several weeks following injury43,44,45. We have demonstrated that this injury model leads to bilateral alterations in the medial prefrontal cortex (mPFC), revealed by diffusion tensor imaging (DTI) and elevated glial fibrillary acidic protein (GFAP), a marker of astrogliosis43. Altered DTI outcomes (e.g., fractional anisotropy, mean diffusivity) have been extensively reported in the prefrontal cortex and associated white matter tracts in human mTBI46,47,48. Furthermore, lower fractional anisotropy values in prefrontal cortex have been correlated with greater executive dysfunction46. The rodent mPFC is an ortholog of the human medial and dorsolateral prefrontal cortices49,50,51, areas implicated in executive dysfunction and drug craving/seeking in both species49,52,53,54,55. We used sophisticated behavioral models to test the hypothesis that bTBI would disrupt performance in complex mPFC-dependent cognitive tasks and elevate drug seeking following cocaine self-administration.
Materials and Methods
Animals
Male Sprague Dawley rats (n = 54; Harlan) were used in this study. Rats arrived at the Zablocki Veterans Affairs Medical Center (ZAMC) at approximately 8 weeks of age and were initially housed in pairs. Rats were transferred from the ZAMC to the Medical College of Wisconsin (~5 miles away) three days after blast exposure or sham treatment. Upon arrival at the Medical College of Wisconsin, rats were singly housed for the remainder of the study. Food and water were provided ad libitum until 3 days prior to onset of cognitive testing, at which point food intake was restricted to 5.5 g of food per 100 g body weight per day until behavioral testing was complete. Rats were housed under reverse light cycle conditions (lights off 0730–1930), and experiments were performed during the dark period. Experimenters were blind to group assignment in all experiments. All experiments done in accordance with The Guide for the Care and Use of Laboratory Animals (8th ed.) and were approved by the Institutional Animal Care and Use committee at the Medical College of Wisconsin.
Blast Exposure
Rats were exposed to either a blast overpressure or sham conditions as described previously43,44,45. In brief, all rats were maintained under anesthesia with a continuous delivery of 1.5% isoflurane and had the torso shielded with a metal cylinder while the head was restrained to prevent rotational acceleration injury. Blast-exposed rats were placed 17 cm from the end of a custom shock tube (3.6 cm inner diameter, 3.0 m driven section, and 0.3 m driver section with mylar membrane between the driver and driven sections). Blast overpressure (450 kPa peak, 80 kPa*msec) was then produced by pressurizing the driver section with helium until the membrane ruptured. Sham-exposed rats were subjected to the same procedures except shockwave overpressure. Following exposure, rats were observed until return of righting reflex, returned to home cage, and observed periodically for 6 hours. Experimenters were blind to group assignment (sham or bTBI).
Injury Assessment
The time taken to regain righting reflex following isoflurane termination was used as a metric for initial recovery from blast injury. At post-injury day 9, a composite neuroscore motor assessment was used to look for post-traumatic gross neurological dysfunction. This test assessed nine neurologically-related responses. Scores between 0 (severely impaired) and 2 (normal) were used for the first six tasks: left and right forelimb flexion during tail suspension, left and right hind limb flexion with forelimbs flat on surface and hind limbs elevated by tail suspension, and resistance to lateral pulsion from the left and right. Additionally, an inclined plane was used to test the rat’s ability to stabilize on an angled platform at three body positions: right side facing down the plane, left side facing down the plane, and rear end facing down the plane. A score was assigned to each body position depending on ability to stabilize: 0 (no stabilization); 1 (stabilization at 37.5°); 2 (stabilization at 40°); 3 (stabilization at 42.5°); 4 (stabilization at 45°). The composite score was the sum of all tests.
Apparatus
Cognitive and drug self-administration experiments were conducted in an operant conditioning chamber (31.8 × 25.4 × 26.7 cm, Med Associates) enclosed in a sound-attenuating box. The right wall was equipped with two retractable levers on either side of a central food receptacle. A pellet dispenser delivered 45 mg sucrose tablets (cat#1811255, Test Diet) to the food receptacle. Chambers were also equipped with a house light and stimulus lights located above each lever. Commercially available software (MED-PC, Med Associates) was used for chamber programming and data collection.
Experiment 1: Effects of bTBI on cognitive function
A total of 24 rats (n = 12 sham, n = 12 bTBI) underwent experiment 1. A timeline of experimental procedures is depicted in Fig. 1.
Operant Set-Shifting and Reversal Experiments
The design of the task was adapted from56,57. Sessions were conducted daily. Rats began food restriction three days prior to the onset of the pre-training phase and at one day prior, rats were given 20 sucrose tablets in their home cage as exposure to the food reward.
Lever Press Training
The initial pre-training phase consisted of lever press training in which a single lever (left or right, counterbalanced across groups) was extended, and a press resulted in the delivery of a single reinforcer (sucrose tablet). After a criterion of at least 50 reinforcers in a given 30 min session was met, rats were then trained on the opposite lever using the same procedure.
Retractable Lever Training
The next pre-training phase consisted of sessions of 90 individual trials in which a single lever (either left or right, randomly selected without replacement within each pair of trials) was extended for a maximum of 10 sec. A lever press within this time period resulted in delivery of a single reinforcer, retraction of the lever, and a 10-sec time out period with the house light extinguished. Each new trial began with illumination of house light and extension of a lever. If a rat failed to press the lever within the 10 sec, the lever was retracted, an omission was counted, and the next trial began 10 sec later. Rats had a minimum of 4 sessions with this training and remained at this phase until a criterion of fewer than 15 omissions in a session was met.
Determination of Potential Side Bias
The end of the pre-training phase was marked with a single session to determine each rat’s potential side bias as described58. The session consisted of 7 individual trials with two phases to each trial. The first phase consisted of an illuminated house light and both levers extended. A lever press on either side resulted in delivery of a single reinforcer and retraction of levers. The second phase consisted of a “correct” and “incorrect” lever response. Both levers were again extended, but only a press on the lever opposite to the lever chosen in the first phase resulted in delivery of a reinforcer and beginning of new trial. This was a “correct” response. If the same lever from the first phase was chosen in the second phase (“incorrect”), the levers were retracted without reinforcer delivery, house light turned off, and then the second phase would be repeated until the rats made a “correct” response. The biased side was then determined by the greater number of lever presses in the first phase.
Visual-Cue Discrimination
The visual-cue discrimination training phase required the rat to identify the correct lever by following a visual cue light that was illuminated over the reinforced lever. Each session consisted of 20-sec trials in which both levers were extended and a single cue light was presented (left or right, randomly selected without replacement within each pair of trials). A correct lever press on the cue-presented side resulted in delivery of a single reinforcer, cue light turned off, and retraction of the levers. After a 10-sec time out, the next trial began. An incorrect lever press (side opposite the cue light) resulted in retraction of levers, cue light turned off, and no reinforcer delivery. If the rat failed to press a lever within 10 sec, an omission was recorded, the levers were retracted, and cue light extinguished. Rats were given the criterion of 10 consecutive correct trials (and at least 30 total trails, excluding omissions), with a maximum number of trials of 150 per session. If rats failed to meet criterion in a single session, they received additional sessions on subsequent days. Rats continued this task until they met criterion.
Shift-to-Response Discrimination
After meeting the criterion for the visual discrimination task, rats were tested the next day on a shift-to-response discrimination. The response (position) discrimination phase forced the rat to shift selection strategy from the visual-cue rule to a spatial rule in which the correct lever was independent of the cue light (e.g., always the left lever). A lever side was assigned to each rat opposite to their previously determined side bias. The session began with 20 “reminder” trials of the visual-cue rule then shifted to the new rule which was to ignore the cue and instead press only the right or left lever. These trials tested 24-hour recall of the visual discrimination and established performance on the visual-cue rule immediately prior to the shift58. Besides reward contingencies, trials were identical in presentation to those in the visual-cue discrimination phase. After the 20 “reminder” trials, the cue light continued to illuminate in randomized fashion but had no bearing on which lever was correct. Rats were given the criterion of 10 consecutive correct trials once the spatial rule was introduced and a maximum number of trials of 200 (including “reminder trials”) per session. If rats failed to meet criterion in a single session, they received additional sessions on subsequent days. Errors were classified as “perseverative”, “regressive”, or “never reinforced” if they occurred before meeting an intermediate acquisition criterion of 75% correct responses per block of 16 trials, after meeting this intermediate criterion, or if the incorrect response was not associated with the cue light56.
Response reversal test
Once rats met criterion, a response discrimination reversal test was given the following day. This test began with 20 “reminder” trails of the previously learned spatial rule then shifted to a new spatial rule in which the correct lever was on the opposite side. Rats were again given the criterion of 10 consecutive correct trials once the new spatial rule was introduced and a maximum number of trials of 200 (including “reminder trials”) per session. If rats failed to meet criterion in a single session, they received additional sessions on subsequent days until they met criterion.
Progressive Ratio
To determine the motivation to obtain the sucrose reinforcer, a progressive ratio test was conducted the day following response discrimination reversal. A single lever was extended (using the lever that was assigned to the rat in reversal test) for 1 hr in which rats freely pressed the lever on a progressive ratio schedule of reinforcement, where each ratio was calculated based on the formula described by59, using j = 0.18. The house light remained on for the entirety of the session, and no cue lights were used.
Operant Delayed Matching to Sample (DMTS)
Immediately following the completion of the set-shifting experiment, working memory was tested using a DMTS experiment adapted from60,61. Delayed matching to sample was conducted in the same operant chambers with the same sucrose tablets as reinforcers. Because of the rat’s familiarity with pressing retractable levers, no initial lever press training was conducted. Each session consisted of 140 trials. A trial consists of three phases: sample, delay, and choice. A trial began with extension of single “sample” lever into the chamber (either left or right, randomly selected without replacement within each pair of trials). A lever press resulted in retraction of the lever and the delay period timer to start. During the delay phase, rats were required to nosepoke into the food receptacle to initiate the choice phase. This required rats to move away from the sample lever so they could not simply remain near the correct lever during the delay phase. Once the delay expired and a nosepoke was performed, both levers were extended giving the rat a choice of which lever to press. A response on the same lever as the sample phase (a correct choice) resulted in delivery of a single reinforcer, retraction of levers, and a 5 sec intertrial interval. A response on the opposite lever as the sample phase (an incorrect choice) resulted in retraction of levers, house light turned off, and a 5 sec time out before the next trial. In the trial following an incorrect response, a correction procedure was used to mitigate side bias. The correction procedure assigned the same lever as the previous trial instead of random assignment.
With initial learning sessions, no delay was used between sample and choice phases. Once the sample lever was pressed, rats could immediately initiate the choice phase by nosepoking into the food receptacle. Once the criterion of 80% correct choices for two consecutive sessions was met, sessions with delay sets were introduced. In delay set sessions, trials were split into blocks of 7, in which the delay durations were randomly presented once within each block. Three delay set sessions were used, and rats were required to meet the criterion of 80% correct choices for two consecutive sessions to advance from delay set 1 to 2 and delay set 2 to 3. Delay set 1 consisted of 0, 1, 2, 3, 4, 5, and 6 sec delays. Delay set 2 consisted of 0, 1, 2, 4, 8, 12, and 16 sec delays. Delay set 3 consisted of 0, 2, 4, 8, 12, 18, and 24 sec delays. Rats were tested for 10 consecutive days on delay set 3 and data from the all sessions was used for analysis. Due to inability to meet criterion on the DMTS task, 3 rats were removed from this experiment leaving a total of 21 rats with reported data (n = 11 blast injury, n = 10 sham).
Experiment 2: Effects of bTBI on cocaine self-administration and drug seeking
A separate group of rats (n = 12 sham, n = 18 bTBI) underwent experiment two. A timeline of experimental procedures is depicted in Fig. 1.
Jugular Catheterization Surgery
Rats underwent jugular catheter surgery similar to that described62,63,64. Rats were anesthetized with isoflurane (3–5% induction, 1–3% maintenance) and were implanted with a silicone catheter (Silastic, ID: 0.51 mm, OD: 0.94 mm, Dow Corning, Auburn, MI) into the right jugular vein, which exited through the intrascapular region and was connected to a cannula assembly. The cannula assembly consisted of a 22 gauge stainless steel cannula (Plastics One, Roanoke, VA) mounted on a base made from dental acrylic and nylon mesh (similar to that described in65), which was implanted subcutaneously. Rimadyl (carprofen, 5 mg/kg s.c.) was administered immediately following surgery and 24 h later. Catheters were flushed five days per week with 0.2 ml of heparinized saline (30 units/ml) and cefazolin (100 mg/ml).
Food self-administration
After ≥5 days recovery from surgery, rats acquired food self-administration without food restriction. Sessions were 30 min in duration and began with turning on the fan (houselight remained off), extension of the two levers, and non-contingent delivery of a 45-mg sucrose tablet. Rats underwent fixed ratio-1 (FR-1) sessions, where a single press on the active lever (side of active lever counterbalanced between animals) resulted in delivery of a 45-mg sucrose tablet and illumination of a cue lamp above the active lever. The cue lamp remained lit for 5 sec, and a timeout period lasted 5 additional sec (10 sec total timeout period). During timeout, responses were counted but had no consequence. Responses on the inactive lever had no consequence. FR-1 sessions were 30 min in length but terminated early if 64 infusions were earned. FR-1 sessions continued until criteria were met (three consecutive sessions of ≥50 reinforcers and ≥2:1 ratio of active to inactive lever presses, minimum 5 sessions).
Cocaine self-administration, extinction, and reinstatement
Rats self-administered cocaine in the same conditions as food self-administration, with the exception that intravenous infusion of cocaine (0.5 mg/kg) was the reinforcer and sessions were three hours in length. The infusion volume and time varied to deliver the appropriate dose from a 3.75 mg/ml stock solution infused at 17.4 ul/sec (e.g., 300 g rat received a 40 ul infusion over 2.3 sec). Rats were allowed to self-administer in 15 daily 2-hour sessions, then 10 daily 6-hour sessions. Catheter patency was determined after completion of the self-administration sessions using Brevital (methohexital, 10 mg/kg, i.v., JHP Pharmaceuticals, Rochester, MI) and any rat not meeting criteria for patency (sedation within 10 sec) was removed from the study. Nine total rats (n = 3 sham, n = 6 bTBI) were removed from the study due to loss of catheter patency and data were not included in analysis. The remaining rats then underwent abstinence for 5–11 days before extinction tests. Extinction tests were conducted in the same conditions as self-administration with the exception that no infusions were delivered. Following acquisition of extinction criteria (≤20 active lever presses for two consecutive days), rats were tested for cocaine primed reinstatement66. Reinstatement took place in three separate tests, and rats were required to meet extinction criteria again before the next test. Cocaine doses (0, 5, 10 mg/kg) were given according to a Latin squares design.
Statistical Analysis
Data were analyzed by two-tailed Student’s t test and ANOVA (repeated measures when appropriate) followed by Holm-Sidak multiple comparisons. D’Agonstino and Pearson normality tests were performed, and Mann-Whitney U tests were conducted when normality tests failed (in which case data are represented as box plots). Statistical tests were performed using Prism 6.0 (Graphpad) or SPSS 21.0 (for 3-way ANOVAs). Significance was set at p = 0.05.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Results
Experiment 1: Cognitive testing following bTBI
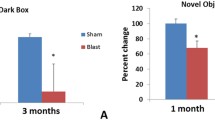
Following the bTBI procedure, there was no significant difference in recovery time between sham and bTBI rats (t(22) = 0.65, n.s.). Injury assessment with the composite neuroscore showed a trend for impairment nine days post-injury (t(22) = 1.8, p = 0.08), although our previous study using this found no significant effect of bTBI44. Despite this trend, no motor impairment was apparent in pre-training tests, which required numerous lever press responses each day of testing. Specifically, there was no difference between sham and bTBI rats in the number of days to meet criteria for FR-1 phase 1 (U = 68, n.s.), phase 2 (U = 72, n.s.), or retractable lever training (U = 66, n.s.). Conversely, there was a significant impairment in bTBI rats in acquisition of a visual discrimination rule. In the visual-cue discrimination task, there was a significant increase in the numbers of errors committed (U = 36, p < 0.05; Fig. 2A) and the number of trials required to reach criteria (U = 37, p < 0.05; data not shown). There was also a trend for bTBI rats to have impaired recall of the task 24 hours following acquisition (U = 41, p = 0.07; Fig. 2B). There were no significant differences between sham and bTBI rats in omissions (U = 66.5, n.s.; Fig. S1A), latency to lever press (t(22) = 0.1, n.s.; Fig. S1B), difference in lever bias (t(22) = 0.3, n.s.; Fig. S1C) during the visual-cue discrimination task, nor in motivation to obtain sucrose in the progressive ratio self-administration task (t(22) = 0.6, n.s.; Fig. S1D). These findings suggest that none of these potential confounds were responsible for the impairment in acquisition of the visual-cue discrimination task observed in the bTBI group.
Acquisition and recall of the visual-cue discrimination task. (A) Number of errors committed during acquisition of task. (B) Number of errors committed in a 20-trial recall test performed 24 hours following acquisition criteria were met. (C) Proportion of errors during acquisition that were initial (not preceded by an incorrect trial) and sequential (preceded by an incorrect trial). (D) Proportion of initial errors that were committed on the same side as the previous trial. (E) Proportion of sequential errors during acquisition that were committed on the same side as the previous trial. Boxes represent median and quartiles, whiskers represent range, symbols are individual values. Bars represent mean ± SEM. N = 12/group. *p ≤ 0.05.
To determine if there were qualitative differences in errors during acquisition of the visual discrimination task, errors were categorized into initial errors (those preceded by a correct trial) or sequential errors (those preceded by an incorrect trial). There was no significant effect of bTBI on the proportion of sequential errors relative to total errors (Fig. 2C), suggesting that errors committed by both groups were similarly distributed between these two categories. Initial and sequential errors were further analyzed by measuring the proportion which resulted from the same response as the previous trial. In the case of initial errors, responding on the same lever can reflect local proactive interference, a phenomenon where memory of the previously reinforced trial interferes with performance on the current trial67,68. In the case of sequential errors, responding on the same lever can reflect local choice perseveration, a failure to adapt response selection strategy following a previously unreinforced trial. Among initial errors, there was no difference in same lever responding between bTBI and sham rats (Fig. 2D). Among sequential errors, there was a significant increase in the proportion of same responses exhibited by bTBI rats (t(19) = 2.1, p = 0.05; Fig. 2E). This suggests that after an incorrect response, bTBI rats were more likely than shams to have another error due to the same response. Despite the deficits in acquisition of the visual-cue discrimination task, all bTBI rats ultimately met acquisition criteria. Combined, these data suggest that bTBI rats are not impaired in a simple instrumental task (i.e., in FR-1 and retractable lever training), but require additional training to acquire a task that requires flexible response selection based on location of a visual cue.
Next, rats were tested in a set-shift task. Acquisition of the set-shift task requires a shift from the visual discrimination rule to a location (response)-based rule56. We hypothesized that bTBI rats would be impaired in this task because inactivation of the mPFC results in set-shift deficits56,69, and we have previously characterized bTBI-associated changes in the mPFC that endure for at least 1 month43. Surprisingly, there was no difference between sham and bTBI rats in the errors committed during acquisition (Fig. 3A) or recall (Fig. 3B) of the set-shift task. We further analyzed errors into perseverative, regressive, or never reinforced (see Methods and56). These types of errors are thought to reflect suppression of the previously acquired strategy, maintenance of the newly acquired strategy, and acquisition of a new strategy, respectively58,69. There were also no differences in the number of any specific error types committed during acquisition (Fig. 3C–E). Thus, bTBI rats were able to shift their response strategy in a similar manner to sham rats. After acquisition of the set-shift, rats were tested in a reversal task. Response reversal is another measure of cognitive flexibility but requires reversal of the previous location rule as opposed to the extradimensional shift (shifting to a different type of rule) required for the set-shift. This reversal is impaired by disruption of transmission in orbitofrontal cortex, but not the mPFC70,71. Similar to the set-shift task, there were no differences between sham and bTBI rats in the number of errors to criteria or the number of perseverative or regressive errors in the reversal task (Fig. 4).
Performance in shift to response discrimination. (A) Number of errors committed during acquisition of set shift. (B) Number of errors committed in a 20-trial recall test performed 24 hours following acquisition criteria were met. (C–E) Analysis of error type during acquisition of set shift: (C) Perseverative errors, (D) Regressive errors, (E) Never reinforced errors. Bars represent mean ± SEM. N = 12/group.
Performance in reversal of response discrimination. (A) Number of errors committed during acquisition of reversal. (B,C) Analysis of error type during acquisition of reversal: (B) Perseverative errors, (C) Regressive errors. Boxes represent median and quartiles, whiskers represent range. N = 12/group.
Problems with working memory have also been reported in mTBI patients72. To test for deficits in working memory in our bTBI model, rats were next tested in an operant DMTS task, an mPFC-dependent working memory task73,74. There was no difference in the number of sessions required to acquire the task (Fig. 5A), nor was there a main effect of bTBI or interaction with delay period in the DMTS task (Fig. 5B).
Experiment 2: Effects of bTBI on cocaine self-administration and drug seeking
As in Experiment one, there were no significant differences in recovery time (t(27) = 0.95, n.s.) or composite neuroscore (t(27) = 0.74, n.s.) after injury. Unlike acquisition of the visual-cue discrimination task, there were no differences between sham and bTBI in acquisition of food self-administration (Fig. S2). There was also no main effect of bTBI or interaction with lever and/or sessions in 2- or 6-hour sessions when analyzing lever presses (Fig. 6A,C). Analysis of the number of infusions earned during these sessions also failed to find a significant effect of bTBI on drug intake or interaction with session (Fig. 6B,C). Extended access drug self-administration such as that in the 6-hour sessions can lead to an escalation of drug intake during the initial period of access75,76. To determine if bTBI altered escalation, we measured intake during the first hour of each 6-hour session (Fig. 6D inset). First hour responding was similar between groups throughout the sessions. Thus, bTBI had no significant effect on cocaine self-administration under short or extended access conditions. Based on the previous demonstration that our bTBI model leads to chronic changes in mPFC43 and extensive evidence that the mPFC regulates drug seeking77,78, we next measured extinction and reinstatement of drug seeking. There was no effect of bTBI on drug seeking in the initial four days of cued extinction sessions (Fig. 6E), nor on the number of days required to meet extinction criteria (Fig. 6F). In cocaine primed reinstatement, 5 mg/kg cocaine resulted in a significant increase in active lever presses in bTBI (p = 0.013, d = 0.94), but not sham rats (p = 0.11, d = 0.53). 10 mg/kg cocaine significantly reinstated drug seeking in both groups of rats (p < 0.001), but between group comparisons did not reveal significant differences between bTBI and sham rats at any dose. These data suggest that bTBI rats are not significantly more sensitive to the effects of cocaine to trigger drug seeking.
Cocaine self-administration and subsequent drug seeking. (A,B) Active (large symbols) and inactive (small symbols) lever responses during the (A) 15 days of 2-hour and (B) 10 days of 6-hour cocaine self-administration sessions. (C,D) Number of infusions earned and corresponding total cocaine intake during (C) 15 days of 2-hour and (D) 10 days of 6-hour cocaine self-administration sessions. Inset in panel D shows cocaine intake during the first hour of the 6-hour sessions. (E) Active lever responses during the initial four days of cued extinction sessions. (F) Number of days required to meet criteria for extinction prior to the first reinstatement test. (G) Active lever responses in cocaine primed reinstatement tests. Symbols represent mean ± SEM. N = 9 sham and 12 bTBI rats. *p ≤ 0.05 compared to 0 mg/kg cocaine in same group.
Discussion
In this study, we found that a single exposure bTBI event led to impairment of learning that was dependent on experimental conditions (i.e., Experiment one vs. Experiment two). Despite the initial impairment in Experiment one, which was assessed 5 weeks after injury, there were no apparent differences in measures of cognitive flexibility. Once a visual discrimination rule was learned, bTBI rats successfully performed an extradimensional shift (ignore visual cue rule and acquire place rule) and reversal of the new rule (ignore old place and go to opposite place) within the same week. There was also no deficit in working memory as assessed by the operant DMTS task 11 weeks following injury. In contrast to Experiment one, bTBI had no effect on acquisition of food self-administration, which was assessed 3 weeks after injury. In cocaine self-administration, there was no difference between sham and bTBI rats in lever pressing or drug intake under short or extended access conditions 4–8 weeks after injury. When cocaine was unavailable, drug seeking (the first week of extinction responding) was similar between sham and bTBI groups 10 weeks following injury. When drug seeking was reinstated with priming injections of cocaine between 12 and 15 weeks after injury, bTBI rats significantly increased responding with the lower dose of cocaine, while sham rats did not. This difference was not confirmed by between-group measurements, suggesting that differences in the power to detect within-group effects (arising from minor differences in sample size, baseline responding, and variance) are responsible for the findings. Following higher dose of cocaine, both groups of rats had a similar magnitude of reinstatement, although there was a trend for bTBI rats to have lower responding than shams.
The finding that bTBI impaired learning in the visual-cue discrimination task (Experiment one) but not in the food self-administration task (Experiment two) is not surprising considering the differences in task requirements. In the visual-cue discrimination task, bTBI had an increased number of errors required to meet the acquire criterion. This task required flexible response selection based on location of a visual cue and had a stringent criterion for acquisition. In experiment two, bTBI had no significant effect on performance of FR-1 food self-administration. This simpler task involved static response selection guided by spatial and egocentric cues (e.g., the lever in the back-left quadrant was always correct) and had less stringent acquisition criteria. Further analysis of the visual-cue discrimination data did not reveal differences in the number of omissions, latency to lever press, or overt bias to one lever. Moreover, there was no significant difference between bTBI and sham rats in operant learning during the pre-training phase of operant set shifting or during food or cocaine self-administration. Thus, bTBI did not result in performance deficits due to general attentional deficits that could have reduced recognition of trial initiation or altered the latency to response, nor did it produce a non-specific bias in overall lever preference, impair operant conditioning, or reduce motivation to obtain food reward. The finding that bTBI impaired acquisition of a visual-cue discrimination task but did not affect set shift or reversal of this task is consistent with a previous report by Vonder Haar et al.79. In this study, frontal controlled cortical impact injury delayed re-acquisition of an operant-based auditory cue discrimination task, but reversal of the task was unimpaired79. Frontal cortical impact injury has also been demonstrated to impair re-acquisition of an olfactory cue discrimination, although reversal of the task was also impaired80. Thus, the finding of impaired cue discrimination has been reported across sensory modalities and tests with different task requirements, although response flexibility after discrimination learning may be specific to cue type and/or task requirements.
It is notable that despite significant group differences in the number of errors committed during visual-cue discrimination, several bTBI rats were in the range of shams (Fig. 2A). We have previously reported heterogeneity in alcohol drinking following the same injury, where median split analysis revealed that the upper 50% of bTBI rats drank significantly more than the upper 50% of shams44. In the current study, bTBI rats did not fit an apparent bimodal distribution, so median split was not performed. However, the heterogeneity in performance on the visual-cue discrimination task is reminiscent of that reported in clinical studies of cognitive recovery following mTBI14,15,16,17,81.
Analysis of error types revealed that bTBI rats had a significantly greater proportion of local perseverative responses in errors that were sequential in nature. Thus, bTBI rats more commonly failed to adapt their behavior in response to the negative feedback during the previous incorrect trial. However, there was no difference in perseverative errors observed during the set shift, and within the bTBI rats, perseverative errors committed during visual-cue discrimination was not correlated with perseverative errors committed during the set shift (F(1,8) = 0.001, n.s.). Following acquisition of the visual-cue discrimination, there was no difference in strategy set shifting between sham and bTBI rats. This was a surprising finding, as our previous work demonstrated differences in fractional anisotropy (FA) in the mPFC 30 days following bTBI43. We have previously found significant correlations between differences in FA within the hippocampus and motor cortex with performance in the Morris water maze, and FA within the frontal cortex has been shown to correlate with impairment in executive function following blast injury in humans46). Because set shift from visual cue to response has been demonstrated to be altered by mPFC infusion of bicuculline (GABA-A antagonist) or bupivacaine (voltage-gated sodium channel blocker)56,69, we hypothesized that bTBI rats would either commit more errors during acquisition of the shift-to-response discrimination, or that acquisition criteria would not be met.
Rats in Experiment one were also tested in an operant DMTS task to assess working memory function. bTBI had no effect on acquisition of this task and did not alter performance in delays up to 24 seconds. In contrast, delayed non-matching to sample and delayed alternation were disrupted ~30 days following mTBIs that used weight drop82 or controlled cortical impact83. An operant version of the delayed non-matching to sample was impaired for over 30 days in a cortical impact model, but the injury was severe enough to result in significant cavitation of the frontal cortex84. Our finding that DMTS was unaffected by bTBI is consistent with the lack of effect in the set-shifting task, as both of these tasks are disrupted by pharmacological inhibition of the mPFC56,69,73,74. It is possible that other factors underlie the lack of effect in DMTS. For example, rats were tested in visual cue discrimination, set-shifting, and reversal prior to DMTS. This prior training on relatively complex tasks could have altered performance on DMTS and masked potential group differences. DMTS was also conducted between 6–11 weeks following injury, and potential deficits may have resolved during this time.
We also found that cocaine self-administration did not differ between bTBI and sham treated rats. To our knowledge, this is the first study of intravenous drug self-administration in a preclinical model of TBI. In fact, despite evidence of increased substance abuse following TBI5,6,7,8,9, there are very few preclinical studies of addiction liability following TBI85. Mayeux et al. found that TBI increased alcohol intake in rats with a previous history of alcohol drinking86. Furthermore, the authors found that the amount of increase was associated with pre-injury intake, a phenomenon described in human injury87,88,89. In alcohol naïve mice, cortical impact TBI increased alcohol intake and conditioned reward in female mice that were injured early in life (P21), but not females that were injured at P60 or males that were injured at P21 or P60 when tested at P80~P10090. We previously reported a modest effect of bTBI increasing alcohol intake ~30 days post-injury in adult rats that were alcohol naïve pre-injury44. Thus, preclinical data suggests that TBI can increase subsequent alcohol intake, but age, sex, and prior alcohol history are all factors that can modify this relationship. There is also evidence that TBI can increase the conditioned rewarding effects of cocaine. In juvenile mice exposed to a cortical impact injury, conditioned place preference for cocaine was elevated when measured three weeks following injury91. It is unclear if the discrepancy between our findings and this study is due to age of injury, species difference, or known inconsistencies between conditioned place preference and self-administration studies92,93,94. In drug seeking tests following cocaine abstinence, we found no effect of bTBI on extinction responding or cocaine-primed reinstatement.
We found that acquisition of a learned discrimination following voluntary intake may be particularly sensitive to the effects of mTBI. Our bTBI model is a closed-head model of mTBI that does not result in significant changes in unconscious time or gross neurological function43,44,45, suggesting that it resembles very mild injury. This model was used previously to determine behavioral and brain structural changes following exposure to shockwave overpressures simulating mild blast TBI43,45, although no injury assessment was made in the current study. The parameters of blast used here are the same as those we used to characterize the model using MRI43, and the blast exposures are highly consistent (mean peak overpressure = 450.8 kPa, coefficient of variation = 11.2%). Rodent injuries produced using this model are solely attributable to head exposure to shockwave overpressure as the body is protected using a metal cylinder, head movements are minimized to limit head rotational accelerations well below the threshold for injury43, and rodents are placed off axis from the shock tube to avoid exposure to exhaust gases43,95. Whereas peak overpressure magnitudes from this model are somewhat greater than other models that incorporate shockwave exposure inside the shock tube96,97,98,99,100, peak shockwave overpressure is not the most appropriate injury metric. Shockwave duration also influences injury onset and severity and should be accounted for in assessments of shockwave exposure101. Accordingly, the area under the positive overpressure versus time curve, also known as impulse magnitude, is often used to assess shockwave exposure severity. As such, impulse magnitude in the current study (80 kPa*ms) is in line with other studies incorporating shockwave exposures inside the shock tube. For example, Perez-Garcia exposed rats to 74.5-kPa with 4.8-ms duration shockwaves inside the shock tube and reported an impulse magnitude of 175.8 kPa*ms99. That study characterized their exposure severities as ‘low-level’. Another recent study produced 207-kPa shockwaves with 2.5-ms durations inside the shock tube96. Assuming a Friedlander waveform shape, calculated impulse magnitude for those exposures would be 190 kPa*ms. Those exposures produced brain and lung edema, which were absent in the current model. Therefore, based on the severity of shockwave exposure in terms of impulse magnitude, a lack of significant pathological changes such as brain edema or hemorrhage, and modest behavioral changes demonstrated previously43,45, the present injury severity was graded as mild.
A possible limitation of this injury model includes the incorporation of shockwave exposure outside the shock tube, whereas a majority of recent studies have incorporated shockwave exposures with the animal positioned inside the tube. However, as indicated above, our focus on placement of the rat lateral to the shock tube axis to avoid exhaust gases from the shock tube partially minimizes this effect. Likewise, our fully-characterized shockwaves are consistent with Friedlander waveforms. Overpressure rise times are an average of 6 microseconds from ambient pressure to peak overpressure and our waveform represents the Friedlander waveform shape associated with a blast wave (Fig. 7). Therefore, this injury model, which has been well-accepted in the literature43,45,95, produces shockwave exposures representative of open field blast and consistent with previous studies from other groups.
Importantly, acquisition of a simple discrimination task (food self-administration in Experiment 2) was not impaired, supporting clinical findings that more advanced cognitive testing may reveal cognitive deficits in mTBI17,18. If changes in drug seeking are particularly vulnerable to injury, this could have important clinical implications for susceptibility to drug craving in individuals who sustain a brain injury. Further studies will be needed to determine if drug craving induced by other types of stimuli are also increased following injury and if environmental enrichment can improve the cognitive and addiction-related outcomes reported here as it has with other TBI-related outcomes102,103,104,105. Our findings also raise important questions regarding the generalizability to other drugs of abuse, effects of repeated injury, and effects on drug seeking if injury occurred during abstinence.
References
Taylor, C. A., Bell, J. M., Breiding, M. J. & Xu, L. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. MMWR Surveill Summ 66, 1–16, https://doi.org/10.15585/mmwr.ss6609a1 (2017).
Koponen, S. et al. Axis I and II psychiatric disorders after traumatic brain injury: a 30-year follow-up study. The American journal of psychiatry 159, 1315–1321, https://doi.org/10.1176/appi.ajp.159.8.1315 (2002).
Fleminger, S. & Ponsford, J. Long term outcome after traumatic brain injury. BMJ 331, 1419–1420, https://doi.org/10.1136/bmj.331.7530.1419 (2005).
Vaishnavi, S., Rao, V. & Fann, J. R. Neuropsychiatric problems after traumatic brain injury: unraveling the silent epidemic. Psychosomatics 50, 198–205, https://doi.org/10.1176/appi.psy.50.3.198 (2009).
Ashman, T. A. et al. Psychiatric challenges in the first 6 years after traumatic brain injury: cross-sequential analyses of Axis I disorders. Archives of physical medicine and rehabilitation 85, S36–42 (2004).
Fedoroff, J. P. et al. Depression in patients with acute traumatic brain injury. The American journal of psychiatry 149, 918–923, https://doi.org/10.1176/ajp.149.7.918 (1992).
Kraus, J. F. & Sorenson, S. B. In Textbook of Traumatic Brain Injury (eds Silver, J. M., Yudofsky, S. C. & Hales, R. E.) 3–41 (American Psychiatric Pub., 1994).
Kreutzer, J. S., Wehman, P. H., Harris, J. A., Burns, C. T. & Young, H. F. Substance abuse and crime patterns among persons with traumatic brain injury referred for supported employment. Brain injury: [BI] 5, 177–187 (1991).
Fann, J. R. et al. Psychiatric illness following traumatic brain injury in an adult health maintenance organization population. Archives of general psychiatry 61, 53–61, https://doi.org/10.1001/archpsyc.61.1.53 (2004).
National Center for Injury Prevention and Control. Report to Congress on mild traumatic brain injury in the United States: steps to prevent a serious public health problem (Centers for Disease Control and Prevention, Atlanta, Ga., 2003).
American Congress of Rehabilitation Medicine. Definition of mild traumatic brain Injury. The Journal of head trauma rehabilitation 8, 86-87 (1993).
Rao, V. & Lyketsos, C. G. Psychiatric aspects of traumatic brain injury. Psychiatr Clin North Am 25, 43–69 (2002).
West, T. A. & Marion, D. W. Current recommendations for the diagnosis and treatment of concussion in sport: a comparison of three new guidelines. Journal of neurotrauma 31, 159–168, https://doi.org/10.1089/neu.2013.3031 (2014).
Rabinowitz, A. R. & Levin, H. S. Cognitive sequelae of traumatic brain injury. Psychiatr Clin North Am 37, 1–11, https://doi.org/10.1016/j.psc.2013.11.004 (2014).
Rutherford, W. H., Merrett, J. D. & McDonald, J. R. Symptoms at one year following concussion from minor head injuries. Injury 10, 225–230 (1979).
Hall, R. C., Hall, R. C. & Chapman, M. J. Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics 46, 195–202, https://doi.org/10.1176/appi.psy.46.3.195 (2005).
McInnes, K., Friesen, C. L., MacKenzie, D. E., Westwood, D. A. & Boe, S. G. Mild Traumatic Brain Injury (mTBI) and chronic cognitive impairment: A scoping review. PLoS One 12, e0174847, https://doi.org/10.1371/journal.pone.0174847 (2017).
de Boussard, C. N. et al. S100 and cognitive impairment after mild traumatic brain injury. J Rehabil Med 37, 53–57, https://doi.org/10.1080/16501970410015587 (2005).
Belanger, H. G., Curtiss, G., Demery, J. A., Lebowitz, B. K. & Vanderploeg, R. D. Factors moderating neuropsychological outcomes following mild traumatic brain injury: a meta-analysis. J Int Neuropsychol Soc 11, 215–227, https://doi.org/10.1017/S1355617705050277 (2005).
McDonald, B. C., Flashman, L. A. & Saykin, A. J. Executive dysfunction following traumatic brain injury: neural substrates and treatment strategies. NeuroRehabilitation 17, 333–344 (2002).
Bigler, E. D. Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc 14, 1–22, https://doi.org/10.1017/S135561770808017X (2008).
West, S. L. Substance use among persons with traumatic brain injury: a review. NeuroRehabilitation 29, 1–8, https://doi.org/10.3233/NRE-2011-0671 (2011).
Ommaya, A. K. et al. Outcome after traumatic brain injury in the U.S. military medical system. J Trauma 41, 972–975 (1996).
McKinlay, A., Grace, R., Horwood, J., Fergusson, D. & MacFarlane, M. Adolescent psychiatric symptoms following preschool childhood mild traumatic brain injury: evidence from a birth cohort. The Journal of head trauma rehabilitation 24, 221–227, https://doi.org/10.1097/HTR.0b013e3181a40590 (2009).
Rosenfeld, J. V. et al. Blast-related traumatic brain injury. Lancet Neurol 12, 882–893, https://doi.org/10.1016/S1474-4422(13)70161-3 (2013).
Fischer, H. United States Military Casualty Statistics: Operation Iraqi Freedom and Operation Enduring Freedom (2010).
Tanielian, T. & Jaycox, L. H. Vol. MG-720-CCF (Rand Corportation, 2008).
Polusny, M. A. et al. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Archives of general psychiatry 68, 79–89, https://doi.org/10.1001/archgenpsychiatry.2010.172 (2011).
Terrio, H. et al. Traumatic brain injury screening: preliminary findings in a US Army Brigade Combat Team. The Journal of head trauma rehabilitation 24, 14–23, https://doi.org/10.1097/HTR.0b013e31819581d8 (2009).
Lippa, S. M., Pastorek, N. J., Benge, J. F. & Thornton, G. M. Postconcussive symptoms after blast and nonblast-related mild traumatic brain injuries in Afghanistan and Iraq war veterans. J Int Neuropsychol Soc 16, 856–866, https://doi.org/10.1017/S1355617710000743 (2010).
Verfaellie, M., Lafleche, G., Spiro, A. & Bousquet, K. Neuropsychological outcomes in OEF/OIF veterans with self-report of blast exposure: associations with mental health, but not MTBI. Neuropsychology 28, 337–346, https://doi.org/10.1037/neu0000027 (2014).
Nelson, N. W. et al. Neuropsychological outcomes of U.S. Veterans with report of remote blast-related concussion and current psychopathology. J Int Neuropsychol Soc 18, 845–855, https://doi.org/10.1017/S1355617712000616 (2012).
Miller, D. R., Hayes, J. P., Lafleche, G., Salat, D. H. & Verfaellie, M. White matter abnormalities are associated with chronic postconcussion symptoms in blast-related mild traumatic brain injury. Human brain mapping 37, 220–229, https://doi.org/10.1002/hbm.23022 (2016).
Neipert, L. et al. Effect of clinical characteristics on cognitive performance in service members and veterans with histories of blast-related mild traumatic brain injury. Brain injury: [BI] 28, 1667–1674, https://doi.org/10.3109/02699052.2014.947623 (2014).
Pagulayan, K. F. et al. Retrospective and Prospective Memory Among OEF/OIF/OND Veterans With a Self-Reported History of Blast-Related mTBI. J Int Neuropsychol Soc, 1-11, https://doi.org/10.1017/S1355617717001217 (2017).
Taylor, L. A., Kreutzer, J. S., Demm, S. R. & Meade, M. A. Traumatic brain injury and substance abuse: A review and analysis of the literature. Neuropsychological rehabilitation 13, 165–188, https://doi.org/10.1080/09602010244000336 (2003).
Hahn, R. A. The nocebo phenomenon: concept, evidence, and implications for public health. Prev Med 26, 607–611, https://doi.org/10.1006/pmed.1996.0124 (1997).
Suhr, J. A. & Gunstad, J. “Diagnosis Threat”: the effect of negative expectations on cognitive performance in head injury. J Clin Exp Neuropsychol 24, 448–457, https://doi.org/10.1076/jcen.24.4.448.1039 (2002).
Cole, W. R. & Bailie, J. M. In Translational Research in Traumatic Brain Injury. Available from: https://www.ncbi.nlm.nih.gov/books/NBK326715/ (eds Laskowitz, D. & Grant, G.) (CRC Press/Taylor and Francis Group, Boca Raton (FL), 2016).
Noel, X., Brevers, D. & Bechara, A. A neurocognitive approach to understanding the neurobiology of addiction. Curr Opin Neurobiol 23, 632–638, https://doi.org/10.1016/j.conb.2013.01.018 (2013).
Sofuoglu, M., DeVito, E. E., Waters, A. J. & Carroll, K. M. Cognitive Function as a Transdiagnostic Treatment Target in Stimulant Use Disorders. J Dual Diagn 12, 90–106, https://doi.org/10.1080/15504263.2016.1146383 (2016).
Bernheim, A., See, R. E. & Reichel, C. M. Chronic methamphetamine self-administration disrupts cortical control of cognition. Neurosci Biobehav Rev 69, 36–48, https://doi.org/10.1016/j.neubiorev.2016.07.020 (2016).
Budde, M. D. et al. Primary blast traumatic brain injury in the rat: relating diffusion tensor imaging and behavior. Frontiers in neurology 4, 154, https://doi.org/10.3389/fneur.2013.00154 (2013).
Lim, Y. W. et al. Voluntary Alcohol Intake following Blast Exposure in a Rat Model of Mild Traumatic Brain Injury. PLoS One 10, e0125130, https://doi.org/10.1371/journal.pone.0125130 (2015).
Stemper, B. D. et al. Behavioral Outcomes Differ Between Rotational Acceleration and Blast Mechanisms of Mild TraumaticBrain Injury. Frontiers in neurology 7, https://doi.org/10.3389/fneur.2016.00031 (2016).
Lipton, M. L. et al. Diffusion-tensor imaging implicates prefrontal axonal injury in executive function impairment following very mild traumatic brain injury. Radiology 252, 816–824, https://doi.org/10.1148/radiol.2523081584 (2009).
Aoki, Y. & Inokuchi, R. A voxel-based meta-analysis of diffusion tensor imaging in mild traumatic brain injury. Neurosci Biobehav Rev 66, 119–126, https://doi.org/10.1016/j.neubiorev.2016.04.021 (2016).
Eierud, C. et al. Neuroimaging after mild traumatic brain injury: review and meta-analysis. Neuroimage Clin 4, 283–294, https://doi.org/10.1016/j.nicl.2013.12.009 (2014).
Fuster, J. M. The prefrontal cortex. 4th edn, (Academic Press, 2008).
Seamans, J. K., Lapish, C. C. & Durstewitz, D. Comparing the prefrontal cortex of rats and primates: insights from electrophysiology. Neurotox Res 14, 249–262, https://doi.org/10.1007/BF03033814 (2008).
Kesner, R. P. & Churchwell, J. C. An analysis of rat prefrontal cortex in mediating executive function. Neurobiol Learn Mem 96, 417–431, https://doi.org/10.1016/j.nlm.2011.07.002 (2011).
Goldstein, R. Z. & Volkow, N. D. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci 12, 652–669, https://doi.org/10.1038/nrn3119 (2011).
Kalivas, P. W. & Volkow, N. D. The neural basis of addiction: a pathology of motivation and choice. The American journal of psychiatry 162, 1403–1413, https://doi.org/10.1176/appi.ajp.162.8.1403 (2005).
Gourley, S. L. & Taylor, J. R. Going and stopping: dichotomies in behavioral control by the prefrontal cortex. Nat Neurosci 19, 656–664, https://doi.org/10.1038/nn.4275 (2016).
Miller, E. K. & Cohen, J. D. An integrative theory of prefrontal cortex function. Annu Rev Neurosci 24, 167–202, https://doi.org/10.1146/annurev.neuro.24.1.167 (2001).
Floresco, S. B., Block, A. E. & Tse, M. T. Inactivation of the medial prefrontal cortex of the rat impairs strategy set-shifting, but not reversal learning, using a novel, automated procedure. Behavioural brain research 190, 85–96, https://doi.org/10.1016/j.bbr.2008.02.008 (2008).
Cox, B. M. et al. Chronic methamphetamine self-administration alters cognitive flexibility in male rats. Psychopharmacology 233, 2319–2327, https://doi.org/10.1007/s00213-016-4283-0 (2016).
George, S. A. et al. Alterations in cognitive flexibility in a rat model of post-traumatic stress disorder. Behavioural brain research 286, 256–264, https://doi.org/10.1016/j.bbr.2015.02.051 (2015).
Richardson, N. R. & Roberts, D. C. Progressive ratio schedules in drug self-administration studies in rats: a method to evaluate reinforcing efficacy. J Neurosci Methods 66, 1–11 (1996).
Beas, B. S., Setlow, B. & Bizon, J. L. Distinct manifestations of executive dysfunction in aged rats. Neurobiol Aging 34, 2164–2174, https://doi.org/10.1016/j.neurobiolaging.2013.03.019 (2013).
Sloan, H. L., Good, M. & Dunnett, S. B. Double dissociation between hippocampal and prefrontal lesions on an operant delayed matching task and a water maze reference memory task. Behavioural brain research 171, 116–126, https://doi.org/10.1016/j.bbr.2006.03.030 (2006).
Ikegami, A., Olsen, C. M., D’Souza, M. S. & Duvauchelle, C. L. Experience-dependent effects of cocaine self-administration/conditioning on prefrontal and accumbens dopamine responses. Behavioral neuroscience 121, 389–400, https://doi.org/10.1037/0735-7044.121.2.389 (2007).
Olsen, C. M. & Duvauchelle, C. L. Prefrontal cortex D1 modulation of the reinforcing properties of cocaine. Brain research 1075, 229–235, https://doi.org/10.1016/j.brainres.2006.01.003 (2006).
D’Souza, M. S., Ikegami, A., Olsen, C. M. & Duvauchelle, C. L. Chronic D1 agonist and ethanol coadministration facilitate ethanol-mediated behaviors. Pharmacology, biochemistry, and behavior 76, 335–342 (2003).
Thomsen, M. & Caine, S. B. Chronic intravenous drug self-administration in rats and mice. Curr Protoc Neurosci Chapter 9, Unit 9 20, https://doi.org/10.1002/0471142301.ns0920s32 (2005).
Shaham, Y., Shalev, U., Lu, L., De Wit, H. & Stewart, J. The reinstatement model of drug relapse: history, methodology and major findings. Psychopharmacology 168, 3–20, https://doi.org/10.1007/s00213-002-1224-x (2003).
Edhouse, W. V. & White, K. G. Cumulative proactive interference in animal memory. Anim Learn Behav 16, 461–467, https://doi.org/10.3758/bf03209387 (1988).
White, K. G., Parkinson, A. E., Brown, G. S. & Wixted, J. T. Local proactive interference in delayed matching to sample: the role of reinforcement. J Exp Psychol Anim Behav Process 30, 83–95, https://doi.org/10.1037/0097-7403.30.2.83 (2004).
Enomoto, T., Tse, M. T. & Floresco, S. B. Reducing prefrontal gamma-aminobutyric acid activity induces cognitive, behavioral, and dopaminergic abnormalities that resemble schizophrenia. Biological psychiatry 69, 432–441, https://doi.org/10.1016/j.biopsych.2010.09.038 (2011).
Ghods-Sharifi, S., Haluk, D. M. & Floresco, S. B. Differential effects of inactivation of the orbitofrontal cortex on strategy set-shifting and reversal learning. Neurobiol Learn Mem 89, 567–573, https://doi.org/10.1016/j.nlm.2007.10.007 (2008).
Izquierdo, A., Brigman, J. L., Radke, A. K., Rudebeck, P. H. & Holmes, A. The neural basis of reversal learning: An updated perspective. Neuroscience 345, 12–26, https://doi.org/10.1016/j.neuroscience.2016.03.021 (2017).
McAllister, T. W. et al. Differential working memory load effects after mild traumatic brain injury. NeuroImage 14, 1004–1012, https://doi.org/10.1006/nimg.2001.0899 (2001).
McQuail, J. A. et al. NR2A-Containing NMDARs in the Prefrontal Cortex Are Required for Working Memory and Associated with Age-Related Cognitive Decline. J Neurosci 36, 12537–12548, https://doi.org/10.1523/JNEUROSCI.2332-16.2016 (2016).
Banuelos, C. et al. Prefrontal cortical GABAergic dysfunction contributes to age-related working memory impairment. J Neurosci 34, 3457–3466, https://doi.org/10.1523/JNEUROSCI.5192-13.2014 (2014).
Ahmed, S. H. & Koob, G. F. Transition from moderate to excessive drug intake: change in hedonic set point. Science 282, 298–300 (1998).
Edwards, S. & Koob, G. F. Escalation of drug self-administration as a hallmark of persistent addiction liability. Behavioural pharmacology 24, 356–362, https://doi.org/10.1097/FBP.0b013e3283644d15 (2013).
Peters, J., Kalivas, P. W. & Quirk, G. J. Extinction circuits for fear and addiction overlap in prefrontal cortex. Learning & memory 16, 279–288, https://doi.org/10.1101/lm.1041309 (2009).
Perry, J. L. et al. Prefrontal cortex and drug abuse vulnerability: translation to prevention and treatment interventions. Brain Res Rev 65, 124–149, https://doi.org/10.1016/j.brainresrev.2010.09.001 (2011).
Vonder Haar, C. et al. Simple tone discriminations are disrupted following experimental frontal traumatic brain injury in rats. Brain injury: [BI] 28, 235–243, https://doi.org/10.3109/02699052.2013.860473 (2014).
Martens, K. M., Vonder Haar, C., Hutsell, B. A. & Hoane, M. R. A discrimination task used as a novel method of testing decision-making behavior following traumatic brain injury. Journal of neurotrauma 29, 2505–2512, https://doi.org/10.1089/neu.2012.2388 (2012).
Rosenbaum, S. B. & Lipton, M. L. Embracing chaos: the scope and importance of clinical and pathological heterogeneity in mTBI. Brain Imaging Behav 6, 255–282, https://doi.org/10.1007/s11682-012-9162-7 (2012).
Milman, A., Rosenberg, A., Weizman, R. & Pick, C. G. Mild traumatic brain injury induces persistent cognitive deficits and behavioral disturbances in mice. Journal of neurotrauma 22, 1003–1010, https://doi.org/10.1089/neu.2005.22.1003 (2005).
Briones, T. L., Woods, J. & Rogozinska, M. Decreased neuroinflammation and increased brain energy homeostasis following environmental enrichment after mild traumatic brain injury is associated with improvement in cognitive function. Acta Neuropathol Commun 1, 57, https://doi.org/10.1186/2051-5960-1-57 (2013).
Lindner, M. D. et al. Dissociable long-term cognitive deficits after frontal versus sensorimotor cortical contusions. Journal of neurotrauma 15, 199–216, https://doi.org/10.1089/neu.1998.15.199 (1998).
Bjork, J. M. & Grant, S. J. Does traumatic brain injury increase risk for substance abuse? Journal of neurotrauma 26, 1077–1082, https://doi.org/10.1089/neu.2008-0849 (2009).
Mayeux, J. P., Teng, S. X., Katz, P. S., Gilpin, N. W. & Molina, P. E. Traumatic brain injury induces neuroinflammation and neuronal degeneration that is associated with escalated alcohol self-administration in rats. Behavioural brain research 279, 22–30, https://doi.org/10.1016/j.bbr.2014.10.053 (2015).
Bombardier, C. H., Temkin, N. R., Machamer, J. & Dikmen, S. S. The natural history of drinking and alcohol-related problems after traumatic brain injury. Archives of physical medicine and rehabilitation 84, 185–191, https://doi.org/10.1053/apmr.2003.50002 (2003).
Kreutzer, J. S., Witol, A. D. & Marwitz, J. H. Alcohol and drug use among young persons with traumatic brain injury. J Learn Disabil 29, 643–651, https://doi.org/10.1177/002221949602900608 (1996).
Ponsford, J., Whelan-Goodinson, R. & Bahar-Fuchs, A. Alcohol and drug use following traumatic brain injury: a prospective study. Brain injury: [BI] 21, 1385–1392, https://doi.org/10.1080/02699050701796960 (2007).
Weil, Z. M., Karelina, K., Gaier, K. R., Corrigan, T. E. & Corrigan, J. D. Juvenile Traumatic Brain Injury Increases Alcohol Consumption and Reward in Female Mice. Journal of neurotrauma 33, 895–903, https://doi.org/10.1089/neu.2015.3953 (2016).
Merkel, S. F. et al. Adolescent Traumatic Brain Injury Induces Chronic Mesolimbic Neuroinflammation with Concurrent Enhancement in the Rewarding Effects of Cocaine in Mice during Adulthood. Journal of neurotrauma 34, 165–181, https://doi.org/10.1089/neu.2015.4275 (2017).
Bardo, M. T. & Bevins, R. A. Conditioned place preference: what does it add to our preclinical understanding of drug reward? Psychopharmacology 153, 31–43 (2000).
Muelbl, M. J. et al. Responses to drugs of abuse and non-drug rewards in leptin deficient ob/ob mice. Psychopharmacology 233, 2799–2811, https://doi.org/10.1007/s00213-016-4323-9 (2016).
Tzschentke, T. M. Measuring reward with the conditioned place preference (CPP) paradigm: update of the last decade. Addict Biol 12, 227–462, https://doi.org/10.1111/j.1369-1600.2007.00070.x (2007).
Shah Ms, A. S., Stemper Phd, B. D. & Pintar Phd, F. A. Development and characterization of an open-ended shock tube for the study of blast mtbi. Biomedical sciences instrumentation 48, 393–400 (2012).
Toklu, H. Z. et al. Overpressure blast injury-induced oxidative stress and neuroinflammation response in rat frontal cortex and cerebellum. Behavioural brain research 340, 14–22, https://doi.org/10.1016/j.bbr.2017.04.025 (2018).
DeMar, J. et al. Effects of Primary Blast Overpressure on Retina and Optic Tract in Rats. Frontiers in neurology 7, 59, https://doi.org/10.3389/fneur.2016.00059 (2016).
Sajja, V. S. et al. Blast neurotrauma impairs working memory and disrupts prefrontal myo-inositol levels in rats. Mol Cell Neurosci 59, 119–126, https://doi.org/10.1016/j.mcn.2014.02.004 (2014).
Perez-Garcia, G. et al. Exposure to a Predator Scent Induces Chronic Behavioral Changes in Rats Previously Exposed to Low-level Blast: Implications for the Relationship of Blast-Related TBI to PTSD. Frontiers in neurology 7, 176, https://doi.org/10.3389/fneur.2016.00176 (2016).
Wang, Y. et al. Cerebrospinal Fluid Chemokine (C-C Motif) Ligand 2 Is an Early-Response Biomarker for Blast-Overpressure-Wave-Induced Neurotrauma in Rats. Journal of neurotrauma 34, 952–962, https://doi.org/10.1089/neu.2016.4465 (2017).
Bass, C. R. et al. Brain injuries from blast. Annals of biomedical engineering 40, 185–202, https://doi.org/10.1007/s10439-011-0424-0 (2012).
Nithianantharajah, J. & Hannan, A. J. Enriched environments, experience-dependent plasticity and disorders of the nervous system. Nat Rev Neurosci 7, 697–709, https://doi.org/10.1038/nrn1970 (2006).
Kline, A. E., Leary, J. B., Radabaugh, H. L., Cheng, J. P. & Bondi, C. O. Combination therapies for neurobehavioral and cognitive recovery after experimental traumatic brain injury: Is more better? Prog Neurobiol 142, 45–67, https://doi.org/10.1016/j.pneurobio.2016.05.002 (2016).
Hannan, A. J. Environmental enrichment and brain repair: harnessing the therapeutic effects of cognitive stimulation and physical activity to enhance experience-dependent plasticity. Neuropathol Appl Neurobiol 40, 13–25, https://doi.org/10.1111/nan.12102 (2014).
Alwis, D. S. & Rajan, R. Environmental enrichment and the sensory brain: the role of enrichment in remediating brain injury. Front Syst Neurosci 8, 156, https://doi.org/10.3389/fnsys.2014.00156 (2014).
Acknowledgements
This research was supported by NIH DA039276 (C.M.O., M.D.B., B.D.S.), Veterans Affairs Medical Research (M.D.B., B.D.S.), and the Research and Education Initiative Fund, a component of the Advancing a Healthier Wisconsin Endowment at the Medical College of Wisconsin (C.M.O.). The authors wish to thank the NIDA drug supply program for providing cocaine. Behavioral studies were performed using equipment from investigator laboratories and the MCW Neuroscience Research Center Rodent Behavior Core. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
C.M.O., B.D.S. and M.D.B. designed the experiments; B.D.S. and A.S.S. supervised and performed blast procedure; M.J.M., M.L.S., N.N.N. and C.H.G. performed the behavioral experiments; C.M.O., B.D.S. and A.S.S. analyzed the data; C.M.O. wrote the manuscript with help from all the authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Muelbl, M.J., Slaker, M.L., Shah, A.S. et al. Effects of Mild Blast Traumatic Brain Injury on Cognitive- and Addiction-Related Behaviors. Sci Rep 8, 9941 (2018). https://doi.org/10.1038/s41598-018-28062-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28062-0
- Springer Nature Limited