Abstract
The cardiovascular diseases are the leading cause of mortality in end-stage renal disease (ESRD) patients. However, roles of statins are still controversial in dialysis-dependent ESRD patients regardless of having proven coronary artery occlusive disease. The aim of this study was to examine the benefit of statin following percutaneous coronary intervention (PCI) in ESRD patients who have proven coronary artery occlusive disease. This study was based on the National Health Insurance Service-National Sample Cohort in South Korea. We included 150 ESRD patients on chronic hemodialysis who underwent PCI with stenting between 2002 and 2013. The primary outcome was a composite of myocardial infarction, stroke, and all-cause mortality. Multivariate time-dependent Cox regression analysis were performed, and statin therapy after PCI was treated as a time-dependent variable. During 3.15 ± 2.71 (mean ± standard deviation) years of follow-up, there were 82 patients with primary outcome. The adjusted hazard ratio for statin use was 0.54 [0.33–0.90] compared to no statin use. This study showed that statin has significant benefit on reducing adverse events risk in dialysis-dependent ESRD patients after PCI.
Similar content being viewed by others
Introduction
Patients with end-stage renal disease (ESRD) have a poor prognosis, and their mortality rates are 6.7–8.5 fold greater than those of the general population1. Cardiovascular diseases are known as the leading cause of morbidity and mortality, accounting for almost 50 percent of deaths in the ESRD population1,2. ESRD patients commonly have coexisting cardiovascular risk factors, and emerging evidence show that kidney disease itself is a risk factor for atherosclerosis and cardiovascular events2,3. As a consequence, ESRD patients frequently undergo percutaneous coronary intervention (PCI) with stenting.
Statins are lipid-lowering agents and are widely prescribed for the primary and secondary prevention of cardiovascular events. The clinical benefit of statin use after PCI is well established by multiple clinical trials4,5,6,7. On the other hand, benefit of statin is still controversial in ESRD patients receiving dialysis8,9,10,11. It has recently been suggested that proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitors, new therapeutic option for the treatment of dyslipidemia, may would be beneficial in reducing cardiovascular risk in chronic kidney disease (CKD)12. Clinical prognosis after PCI is proportional to kidney function, and relatively poor in ESRD patients13. Therefore, optimal preventive medications after PCI are crucial for the high-risk patients with ESRD. We hypothesized that statin therapy following PCI would have beneficial effects on ESRD patients, and the aim of this study was to examine this hypothesis by conducting a cohort study using the nationwide health insurance claim data.
Results
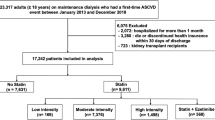
According to the inclusion and exclusion criteria, 150 chronic hemodialysis patients were finally included (Fig. 1). The median age at coronary artery implantation was 65–69 years old, and 56.7% was male (Table 1). During the first 30 days after PCI, 113 patients (75.3%) received statin therapy and 37 patients (24.7%) did not. Among 113 patients who received statin therapy, 80 patients were classified as good adherence (PDC ≥ 80%) and 33 patients were classified as poor adherence (PDC < 80%) during the first 30 days after PCI. Clinical characteristics were not significantly different between patient groups stratified by statin use during the first 30 days, except good adherence to aspirin and ADP receptor antagonist treatment, which was positively associated with good adherence to statin therapy (Table 1).
During the follow-up period of 3.15 ± 2.71 (mean ± standard deviation) years, there were 82 patients with primary outcomes (17 cases of MI, 13 cases of stroke, and 52 cases of all-cause death by counting only the earliest event per patient). Figure 2 illustrates a survival plot based on the use of statin during the follow-up period. In the multivariate time-dependent Cox regression analyses, the adjusted HR [95% CI] for the use of statin was 0.54 [0.33–0.90] compared to no statin use (Table 2, Model A). Good adherence to statin (PDC30day ≥ 0.8, PDCfu ≥ 0.8) was also significantly associated with lower risk of adverse events (Table 2, Model B,C).
Discussion
This study showed that statin therapy was significantly associated with reduced risk of adverse events in dialysis-dependent ESRD patients after PCI. This beneficial effect remained significant after adjusting for conventional risk factors and the use of antiplatelet agents. There was almost a 40% reduction in hazard for the primary outcome. Over the past decades, various effects of statins beyond lipid control have been reported in cardiovascular disease14. Statins play a role in improving vasomotor activity through promoting vasodilation, which is mediated by endothelial nitric oxide synthase15,16, and inhibiting vasoconstriction by the reduction of preproendothelin-1 transcription17. Statins are also immune modulators and impact various mechanisms, including inhibition of leukocyte adhesion to the endothelium, inhibition of inflammatory transcription factors, and reduction of serum inflammatory markers, such as C-reactive protein (CRP), tumor necrosis factor-α, and various cytokines and interleukins18. Indeed, several clinical trials have shown that statin therapy contributes to decreases in CRP levels19,20,21. In addition, inhibition of platelet aggregation and augmentation of thrombolysis have been suggested as other pleiotropic roles of statins18,22,23,24,25.
It has been demonstrated that CKD is associated with low-grade inflammation, endothelial dysfunction, and platelet activation, and thus, those alterations become worse as kidney function declines26,27. The Treating to New Targets (TNT) study on 3,107 patients with stable coronary artery disease and CKD found a significant benefit from high-dose atorvastatin (80 mg/day) on the reduction of coronary artery disease and stroke; however, patients who needed dialysis were not included28. The first large prospective trial of statin use in patients receiving chronic hemodialysis was conducted in Germany (the German Diabetes and Dialysis Study, 4D study)8. The results demonstrated that lowering LDL cholesterol with atorvastatin in 1,255 hemodialysis patients with type 2 diabetes but did not significantly reduce the incidence of primary outcomes (median 4 years)8. A few years later, the AURORA (A Study to Evaluate the Use of Rosuvastatin in Subjects on Regular Hemodialysis: An Assessment of Survival and Cardiovascular Events) Study Group examined the effects of rosuvastatin on patients undergoing regular hemodialysis treatment compared to a control group9. Rosuvastatin did not have a significant effect on the primary endpoint of nonfatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes9. The recent large SHARP (Study of Heart and Renal Protection) trial studied a wide range of patients with CKD11. Although there was a significant risk reduction in primary outcomes among the non-dialysis-dependent patients with CKD after treatment with statins plus ezetimibe, dialysis patients did not benefit from the treatment11. The results of these three randomized controlled studies are inconsistent with prior large observational reports showing that statin prescriptions are associated with reduced mortality in chronic dialysis patients29,30.
In our study, we focused on chronic hemodialysis patients undergoing PCI because they are at high risk of cardiovascular disease, but there is no clear evidence regarding statin treatment among this patient population31. In both the 4D and SHARP studies, subjects who had recently undergone coronary intervention or experienced a myocardial infarction were excluded8,11. In the AURORA study, only 6.2% of subjects had a history of coronary revascularization before enrollment9. The European Society of Cardiology and European Atherosclerosis Society categorized patients with history of previous PCI as very high risk, and they recommended this group to reduce LDL-cholesterol level lower than 70 mg/dL. They recommended that dialysis-dependent CKD also must be considered very high risk, but they suggested not to initiate statin in case of dialysis-dependent CKD and free of atherosclerotic cardiovascular disease32. The United States Preventive Service Task Force recently emphasized statin therapy based on the presence of cardiovascular disease risk factors and a 10-year risk of cardiovascular disease events33. The American College of Cardiology and the American Heart Association also recommended high intensity statin therapy in CKD patients similar to the European group34. However, they did not make recommendation of statin use in the specific subgroup undergoing maintenance hemodialysis because of considerable uncertainty regarding whether statins have a cardiovascular protective effect on this population8,9,11,34. The Kidney Disease Improving Global Outcomes Lipid Guideline Development Work Group recommended that statins or the statin/ezetimibe combination should not be initiated in dialysis-dependent CKD patients without mentioning specific subgroups, such as patients who underwent coronary artery intervention31. In our retrospective cohort study, statin therapy has beneficial effects on dialysis-dependent patients following PCI. The selection of patients who underwent PCI in this study might have influenced the observation of a significant benefit from statin therapy compared to the prior trials with ESRD patients. Our results suggest that we may consider statin therapy in dialysis patients who underwent coronary intervention.
This study had both strengths and limitations aside from the retrospective nature. We were able to collect prescription data as well as admission and mortality data during the long-term follow-up period based on the national health claim data. In clinical practice, statin use is dynamic; the discontinuation and resumption of statin therapy are frequent and can occur at any time. Unlike previous observational studies, which commonly determined statin use at baseline or exposure during hospitalization29,30, we investigated statin use during the follow-up period as a time-dependent variable with consideration for the dynamics. This approach could strengthen the associations between time-varying covariates, including individual drug use, with clinical outcome compared to the traditional model35. On the other hand, we should acknowledge that outcome detection in this study might have limited accuracy. Although the diagnostic accuracy of the ICD-10 code in NHIS has been validated in prior studies, adverse events without admission could not be captured36. Additionally, we lacked information that was not available from the health insurance database, such as cigarette smoking status, biochemical abnormalities, the duration of dialysis, and why some patients get prescription of statin and others do not; these factors may cause confounding effects. Prescription data in the NHIS-NSC database did not assure the actual compliance of patients to medication. This study had retrospective observational design; therefore, we could not conclude the casual relationship between favorable prognosis and statin therapy. Additional study is required to establish the beneficial effects of adherent statin therapy on ESRD patients undergoing PCI.
Methods
Data source
This study used data from the National Health Insurance Service-National Sample Cohort (NHIS-NSC)37. All individuals living in South Korea are eligible for coverage from the National Health Insurance Program. The NHIS-NSC database was constructed with the health claim data of 1,025,340 subjects (2.2% of the total eligible Korean population in 2002) who were selected by stratified random sampling based on gender, age, and household income. The NHIS-NSC contains data of all health services, including hospital visits (inpatient and outpatient), medical procedures, prescriptions of drugs, diagnosis at the hospital visit, and demographic information, including sex, age, household income, and mortality, during the study period of 2002–2013. The diagnostic code was based on the International Classification of Diseases, 10th revision (ICD-10). There are many published articles based on the NIHS health claim data38,39,40,41.
Study design
We conducted a retrospective cohort study using the NHIS-NSC database. The study subjects were patients on chronic hemodialysis who underwent PCI during 2002–2013. With the claim database of national health insurance program in Korea, we could find patients who underwent PCI with stenting (health claim code of ‘M6561’, ‘M6562’, ‘M6563’, and ‘M6564’) during the study period. Among them, we only included patients aged ≥20 years and who continued hemodialysis (health claim code of ‘O7020’ and ‘O9991’ in NHIS) for ≥3 months before PCI. As exclusion criteria, we excluded patients who underwent renal transplantation before PCI. Because too short follow-up period is inadequate to evaluate the adherence to statin, those followed-up <30 days were excluded. Figure 1 illustrates the inclusion and exclusion criteria. The index date was the first date of admission for PCI. Primary outcome was a composite of myocardial infarction (MI), stroke, and all-cause mortality, whichever occurred first after PCI. The development of MI (I21) and stroke (I60–I63) was defined as admission with a main diagnosis of the respective ICD-10 codes. In the validation studies based on the NHIS database, the diagnostic accuracy of MI was reported as 73–93%, and that for stroke was over 80%27,42,43,44. Patients were followed-up until the development of a primary outcome, renal transplantation, loss of eligibility for NHIS due to emigration, or Dec 31, 2013 (study end date). Data in the NHIS-NSC were fully anonymized and deidentified. This study was approved by the Institutional Review Board of CHA Bundang Medical Center, and informed consent was waived.
Use of statins as a time-dependent variable
Starting from the index date, we collected the prescription records for statins (atorvastatin, rosuvastatin, pitavastatin, pravastatin, simvastatin, and lovastatin) in each patient. We determined the use of statin on each day of the follow-up period based on whether the day is covered by the prescription of statins. For each day, we calculated 1) the current use of statin on that day, 2) the proportion of days covered (PDC) by statin over the prior 30 days (PDC30day), and 3) the PDC by statin over the follow-up period from index date to a given day (PDCfu). Additional explanations of the definitions are shown in the Supplementary Table. PDC ≥80% is considered as a responsible cut-off value for the good adherence45. To reflect the dynamic change of statin use during follow-up, these values on each day were included as time-dependent variables in the survival analyses. Use of aspirin and adenosine diphosphate (ADP) receptor antagonists (clopidogrel, prasugrel, ticlopidine, and ticagrelor) were also assessed as time-dependent covariates in the same manner.
Covariates as a time-fixed variable
We collected data on sex, age (grouped into five-year periods in the NHIS-NSC database), and household income (a marker of socioeconomic state at the time of PCI) as time-fixed covariates. The household income obtained from the NHIS-NSC was subdivided into tertile groups (Q1–Q3) for analysis. The presence of hypertension (I10–15), diabetes mellitus (DM; E08–11 and E13–14), and atrial fibrillation (AF; I48) was defined based on the presence of the diagnostic codes (ICD-10) in the NHIS-NSC before or at the time of discharge from the index admission. Hypertension and DM were recognized as relevant only if the subjects received anti-hypertensive (calcium-channel blockers, angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, diuretics, or beta-blockers) or anti-diabetic (sulfonylureas, biguanides, alpha-glucosidase inhibitors, thiazolidinediones, meglitinides, glucagon-like peptide-1 receptor agonists, dipeptidyl peptidase-4 inhibitors, or insulin) prescriptions along with the diagnostic code46. The presence of acute MI at PCI was determined by the presence of an ICD-10 code of I21 at the index admission.
Statistical analysis
Comparison of clinical characteristics were performed using the chi square test for categorical data and the Kruskal-Wallis test for age. To evaluate effects of statin therapy on the risk of adverse events, we constructed three Cox proportional hazards regression models with fixed and time-varying covariates; each model included current use, PDC30day ≥ 80%, and PDCfu ≥ 80% as time-dependent variables for statin therapy on each day of the follow-up period. Adjustments were made for sex, age (as continuous variable), the level of house income, and the presence of hypertension, DM, atrial fibrillation, and acute MI as time-fixed covariates. Adjustments were also made for the use of antiplatelet drugs (aspirin or ADP receptor antagonist) as time-dependent covariates. The assumption of proportional hazards for statin therapy in the Cox models was tested by evaluating scaled Schonfeld residuals, which were found to be satisfactory. The survival plot with a time-dependent variable was illustrated using the method established by Simon and Makuch47. Data manipulation and the statistical analyses were performed with PostgreSQL, version 9.6.1 (The PostgreSQL Global Development Group; https://www.postgresql.org/) and R software, version 3.4.1 (The R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org/). A two-sided P value of <0.05 was considered to be statistically significant.
References
Tonelli, M. et al. Chronic kidney disease and mortality risk: a systematic review. J. Am. Soc. Nephrol. 17, 2034–2047 (2006).
Saran, R. et al. US Renal Data System 2016 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 69, A7–a8 (2017).
Sarnak, M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension 42, 1050–1065 (2003).
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344, 1383–1389 (1994).
Toi, T. et al. Early effect of lipid-lowering therapy with pitavastatin on regression of coronary atherosclerotic plaque. Comparison with atorvastatin. Circ. J. 73, 1466–1472 (2009).
Takayama, T. et al. Effect of rosuvastatin on coronary atheroma in stable coronary artery disease: multicenter coronary atherosclerosis study measuring effects of rosuvastatin using intravascular ultrasound in Japanese subjects (COSMOS). Circ. J. 73, 2110–2117 (2009).
Nissen, S. E. et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 295, 1556–1565 (2006).
Wanner, C. et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N. Engl. J. Med. 353, 238–248 (2005).
Fellstrom, B. C. et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N. Engl. J. Med. 360, 1395–1407 (2009).
Marz, W. et al. Atorvastatin and low-density lipoprotein cholesterol in type 2 diabetes mellitus patients on hemodialysis. Clin. J. Am. Soc. Nephrol. 6, 1316–1325 (2011).
Baigent, C. et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet 377, 2181–2192 (2011).
Zheng-Lin, B. & Ortiz, A. Lipid Management in Chronic Kidney Disease: Systematic Review of PCSK9 Targeting. Drugs, https://doi.org/10.1007/s40265-017-0858-2 (2018).
Patel, A. D. et al. Five-year mortality outcomes in patients with chronic kidney disease undergoing percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 89, E124–E132 (2017).
Blum, A. & Shamburek, R. The pleiotropic effects of statins on endothelial function, vascular inflammation, immunomodulation and thrombogenesis. Atherosclerosis 203, 325–330 (2009).
Anderson, T. J. et al. The effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotion. N. Engl. J. Med. 332, 488–493 (1995).
Janssens, S. et al. Human endothelial nitric oxide synthase gene transfer inhibits vascular smooth muscle cell proliferation and neointima formation after balloon injury in rats. Circulation 97, 1274–1281 (1998).
Hernandez-Perera, O., Perez-Sala, D., Soria, E. & Lamas, S. Involvement of Rho GTPases in the transcriptional inhibition of preproendothelin-1 gene expression by simvastatin in vascular endothelial cells. Circ. Res. 87, 616–622 (2000).
Zhao, J., Zhang, X., Dong, L., Wen, Y. & Cui, L. The many roles of statins in ischemic stroke. Curr. Neuropharmacol. 12, 564–574 (2014).
Ridker, P. M., Rifai, N., Pfeffer, M. A., Sacks, F. & Braunwald, E. Long-term effects of pravastatin on plasma concentration of C-reactive protein. The Cholesterol and Recurrent Events (CARE) Investigators. Circulation 100, 230–235 (1999).
Plenge, J. K. et al. Simvastatin lowers C-reactive protein within 14 days: an effect independent of low-density lipoprotein cholesterol reduction. Circulation 106, 1447–1452 (2002).
de Lorgeril, M. et al. Cholesterol lowering, cardiovascular diseases, and the rosuvastatin-JUPITER controversy: a critical reappraisal. Arch. Intern. Med. 170, 1032–1036 (2010).
Sang, L. Q., H., K., Levenson, J., Megnien, J. L., Simon, A. & Devynck, M. A. Platelet cytosolic Ca2+ and membrane dynamics in patients with primary hypercholesterolemia. Effects of pravastatin. Arterioscler. Thromb. Vasc. Biol. 15, 759–764 (1995).
Obi, C. et al. Inhibition of platelet-rich arterial thrombus in vivo: acute antithrombotic effect of intravenous HMG-CoA reductase therapy. Arterioscler. Thromb. Vasc. Biol. 29, 1271–1276 (2009).
Essig, M. et al. 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors increase fibrinolytic activity in rat aortic endothelial cells. Role of geranylgeranylation and Rho proteins. Circ. Res. 83, 683–690 (1998).
Zhang, L. et al. Multitargeted effects of statin-enhanced thrombolytic therapy for stroke with recombinant human tissue-type plasminogen activator in the rat. Circulation 112, 3486–3494 (2005).
Landray, M. J. et al. Inflammation, endothelial dysfunction, and platelet activation in patients with chronic kidney disease: the chronic renal impairment in Birmingham (CRIB) study. Am. J. Kidney Dis. 43, 244–253 (2004).
Zoccali, C., Mallamaci, F. & Tripepi, G. Inflammation and atherosclerosis in end-stage renal disease. Blood Purif. 21, 29–36 (2003).
Shepherd, J. et al. Intensive lipid lowering with atorvastatin in patients with coronary heart disease and chronic kidney disease: the TNT (Treating to New Targets) study. J. Am. Coll. Cardiol. 51, 1448–1454 (2008).
Seliger, S. L. et al. HMG-CoA reductase inhibitors are associated with reduced mortality in ESRD patients. Kidney Int. 61, 297–304 (2002).
Mason, N. A. et al. HMG-coenzyme a reductase inhibitor use is associated with mortality reduction in hemodialysis patients. Am. J. Kidney Dis. 45, 119–126 (2005).
Tonelli, M. & Wanner, C. Lipid management in chronic kidney disease: synopsis of the Kidney Disease: Improving Global Outcomes 2013 clinical practice guideline. Ann. Intern. Med. 160, 182 (2014).
Catapano, A. L. et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur. Heart J. 37, 2999–3058 (2016).
Pagidipati, N. J. et al. Comparison of Recommended Eligibility for Primary Prevention Statin Therapy Based on the US Preventive Services Task Force Recommendations vs the ACC/AHA Guidelines. JAMA 317, 1563–1567 (2017).
Goff, D. C. Jr. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 63, 2935–2959 (2014).
Dekker, F. W., de Mutsert, R., van Dijk, P. C., Zoccali, C. & Jager, K. J. Survival analysis: time-dependent effects and time-varying risk factors. Kidney Int. 74, 994–997 (2008).
Kim, H. L. et al. Incidence and Risk Factors Associated With Hospitalization for Variant Angina in Korea. Medicine (Baltimore) 95, e3237 (2016).
Lee, J., Lee, J. S., Park, S. H., Shin, S. A. & Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 46, e15 (2017).
Park, S. J., Choi, N. K., Yang, B. R., Park, K. H. & Woo, S. J. Risk of stroke in retinal vein occlusion. Neurology 85, 1578–1584 (2015).
Shin, J. Y., Roughead, E. E., Park, B. J. & Pratt, N. L. Cardiovascular safety of methylphenidate among children and young people with attention-deficit/hyperactivity disorder (ADHD): nationwide self controlled case series study. BMJ 353, i2550 (2016).
Jee, S. H. et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open 4, e005025 (2014).
Rim, T. H. et al. Retinal Artery Occlusion and the Risk of Stroke Development: Twelve-Year Nationwide Cohort Study. Stroke 47, 376–382 (2016).
Chou, R., Dana, T., Blazina, I., Daeges, M. & Jeanne, T. L. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 316, 2008–2024 (2016).
Hou, W. et al. Effect of statin therapy on cardiovascular and renal outcomes in patients with chronic kidney disease: a systematic review and meta-analysis. Eur. Heart J. 34, 1807–1817 (2013).
Lim, S. Y. Role of statins in coronary artery disease. Chonnam Med. J. 49, 1–6 (2013).
Bansilal, S. et al. Assessing the Impact of Medication Adherence on Long-Term Cardiovascular Outcomes. J. Am. Coll. Cardiol. 68, 789–801 (2016).
Kang, Y. M., Kim, Y. J., Park, J. Y., Lee, W. J. & Jung, C. H. Mortality and causes of death in a national sample of type 2 diabetic patients in Korea from 2002 to 2013. Cardiovasc. Diabetol. 15, 131 (2016).
Snapinn, S. M., Jiang, Q. & Iglewicz, B. Illustrating the impact of a time-varying covariate with an extended Kaplan-Meier estimator. Am. Stat. 59, 301–307 (2005).
Acknowledgements
This study used NHIS-NSC data (NHIS-2017–2–389) made by NHIS.
Author information
Authors and Affiliations
Contributions
S.H.K., the co-first author, conceived and designed the study. H.Y.J. the co-first author, conceived and designed the study. D.H.Y. analyzed the data and drafted the manuscript. J.K., the co-corresponding author, acquired and analyzed the data. S.-Y.L., the co-corresponding author, analyzed the data and drafted the manuscript. J.K. and S.-Y.L. provided critical revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
This research was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Education [NRF-2017R1D1A1B03033382 and NRF-2016R1C1B1013814]. All authors declare no potential conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, S.H., Jeong, H.Y., Yang, D.H. et al. Beneficial effect of statins in patients receiving chronic hemodialysis following percutaneous coronary intervention: A nationwide retrospective cohort study. Sci Rep 8, 9692 (2018). https://doi.org/10.1038/s41598-018-27941-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-27941-w
- Springer Nature Limited