Abstract
Central to understanding human behavior is a comprehensive mapping of brain-behavior relations within the context of lifespan development. Reproducible discoveries depend upon well-powered samples of reliable data. We provide to the scientific community two, 10-minute, multi-echo functional MRI (ME-fMRI) runs, and structural MRI (T1-MPRAGE), from 181 healthy younger (ages 18–34 y) and 120 older adults (ages 60–89 y). T2-FLAIR MRIs and behavioral assessments are available in a majority subset of over 250 participants. Behavioral assessments include fluid and crystallized cognition, self-reported measures of personality, and socioemotional functioning. Initial quality control and validation of these data is provided. This dataset will be of value to scientists interested in BOLD signal specifically isolated from ME-fMRI, individual differences in brain-behavioral associations, and cross-sectional aging effects in healthy adults. Demographic and behavioral data are available within the Open Science Framework project “Goal-Directed Cognition in Older and Younger Adults” (http://osf.io/yhzxe/), which will be augmented over time; neuroimaging data are available on OpenNeuro (https://openneuro.org/datasets/ds003592).
Measurement(s) | Magnetization-Prepared Rapid Gradient Echo MRI • Functional Magnetic Resonance Imaging • T2 and Fluid Attenuated Inversion Recovery MRI • Cognition |
Technology Type(s) | 3 Tesla Magnetic Resonance Imaging • Cognitive Assessment |
Sample Characteristic - Organism | Homo sapiens |
Sample Characteristic - Location | United States of America • Canada |
Similar content being viewed by others
Background & Summary
Comprehensive characterization, or deep phenotyping, is critically necessary to identify reliable patterns of coherence between brain structure, function and behavior, towards generating precision maps of brain-behavior associations. Here we report data collected from a two-site, cognitive neuroscience investigation involving samples of healthy younger and older adults. The design was cross-sectional, incorporating deep behavioral phenotyping, structural MRI and multi-echo fMRI (ME-fMRI) data acquisition. The central motivation of the study was to investigate differences across age cohorts in cognition and brain health, and how they intersect to shape late life development. The sample size for each age-cohort recruited into the study was calculated to provide sufficient statistical power for group-wise individual difference analyses of behavior-brain associations1. A correlation of individual differences between measures that do not share method variance is, on average, between 0.20 and 0.302,3,4, and n ≥ 120 provides 80% power to detect non-zero correlations r ≥ 0.20 with 95% confidence intervals.
In devising our behavioral protocol, we drew from research showing that cognitive aging proceeds along two overarching trajectories: fluid cognition steadily declines with age while crystallized cognition increases or remains stable5. To obtain reliable behavioral indices we included multiple measures for each cognitive domain including episodic memory, semantic memory, executive functioning and processing speed, as well as self-report measures of personality and socioemotional functioning.
In developing the functional brain imaging protocol, we adopted a lifespan network neuroscience approach6. This involves investigating neurocognitive aging through the lens of spatially distributed, large-scale brain networks. With advancing age, the network architecture of the brain shifts, as within-network connectivity declines, between-network connectivity increases, and network dedifferentiation emerges as a prominent feature of the aging connectome (see7, for in-depth preliminary examination of the dataset). We reasoned that the dual trajectories of cognitive aging would be reflected in these broad shifts in the functional architecture of the aging brain8,9.
Identifying reliable patterns of functional networks and associations with cognition imposes significant methodological challenges. Among the most pervasive of these involves the separation of neural from non-neural, or noise, components in resting-state BOLD signals. This is particularly problematic in cross-sectional studies of aging, where it can be difficult to attribute observed group differences to neural sources versus noise sources of non-interest. We adopted ME-fMRI data acquisition with multi-echo independent components analysis (ME-ICA) preprocessing10. This approach relies on the TE-dependence model of BOLD signal for denoising to reliably differentiate BOLD from non-BOLD signal in fMRI data10. Importantly, ME-ICA processing removes distant-dependent motion confounds in RSFC data11, possibly eliminating the need for multiple confound regression, including the global signal12, while allowing for valid between-group comparisons of the full range of positive and negative RSFC values. The approach has proven to be highly reliable for precision mapping13. Subsets of the data described here have provided novel insight into inter-regional BOLD signal variability properties in young adults14, and into large-scale network configuration differences between younger and older adults related to semantic autobiographical memory15 and moral cognition16. Despite the demonstrable advantages of ME-fMRI data and processing, there is currently a paucity of ME-fMRI data available in open access repositories (for task and naturalistic viewing exceptions, see17,18).
This release is the product of a multi-year, multi-site data collection initiative with the overarching objective to uncover parallels in the shifting architectures of brain and cognitive functioning from younger to older adulthood. In addition to resting-state ME-fMRI, we also collected a structural image (T1-MPRAGE) and a T2-FLAIR acquisition to quantify white matter hyperintensities. Our initial investigation into the older adults included in this dataset suggests that white matter hyperintensities, which accumulate with advancing age, are related to reduced network segregation19. This multi-modal protocol has resulted in an extensive neurocognitive aging dataset, including one of the first large-scale releases of ME-fMRI data in younger and older adults. We expect that the samples of healthy younger and older adults reported here, as well as the deep phenotyping and innovative neuroimaging approaches, will be of broad interest to the scientific community.
Methods
Participants
Participants were 181 younger (Mage = 22.59 y, SD = 3.27; 57% female) and 120 older (Mage = 68.63 y, SD = 6.44; 54% female) healthy adults from Ithaca, New York (N = 238) and Toronto, Canada (N = 63; Table 1), rendering a total sample size of 301 that passed quality assessment. Participants were screened to rule out individuals with a history of neurological or other medical illness known to impact cognition, acute or chronic psychiatric illness, those undergoing current or recent treatment with psychotropic medication, and those having recently experienced significant changes to health status at the time of the eligibility interview. Younger and older participants were screened for depressive symptoms using the Beck Depression Inventory20 and the Geriatric Depression Scale21, respectively. Two older adults were not included due to a rating of “moderate depression.” Participants were additionally administered the Mini-Mental State Examination (MMSE22). Participants with MMSE scores below 27/30 were excluded if fluid cognition scores23 also fell below an age-adjusted national percentile of 25% (two younger and two older adults). All participants were right-handed with normal or corrected-to-normal vision. Procedures were administered in compliance with the Institutional Review Board at Cornell University and the Research Ethics Board at York University, including written informed consent obtained from each study participant. The cost of data collection per participant was estimated to be approximately $3000 USD.
Cognitive, Behavioral and Personality Assessment
In the lab, 283 of 301 individuals (163/181 younger adults, 120/120 older adults) underwent extensive cognitive, behavioral and personality assessment over three to four days prior to brain scanning, and passed quality assessment.
In lab assessments included the NIH Toolboxes of Cognition and Emotion23 and auxiliary measures. The NIH Cognition Toolbox included the Rey Auditory Verbal Learning and Picture Sequence Memory, Flanker Inhibitory Control and Attention, Dimensional Change Card Sort, List Sort Working Memory, Picture Vocabulary, and Oral Reading Recognition tests. Composite scores of fluid and crystallized intelligence were also tabulated within the toolbox. The NIH Emotion Toolbox included surveys of Positive Affect, General Life Satisfaction, Meaning and Purpose, Emotional Support, Instrumental Support, Friendship, Perceived Rejection, Perceived Hostility, Perceived Stress, Self-Efficacy, Anger-Affect, Fear-Somatic Arousal, and Fear-Affect. Additionally, participants completed Verbal Paired Associates from the Wechsler Memory Scale-IV24, the Associative Recall Paradigm25, Shipley-2 Vocabulary26, Trail Making Test B-A27, the Reading Span Task28, and the Symbol Digit Modalities Test29.
Online, 253 of 301 individuals (142/181 younger adults, 111/120 older adults) completed self-report evaluations between lab visits in the days prior to brain scanning, and passed quality assessment. Measures included the Behavioral Inhibition System/Behavioral Activation System Scale30, Interpersonal Reactivity Index31, and Big Five Aspects Scale32.
Magnetic resonance imaging
Neuroimaging data were acquired from two sites with a 3T GE Discovery MR750 and 32-channel head coil at the Cornell Magnetic Resonance Imaging Facility or on a 3T Siemens TimTrio MRI scanner with a 32-channel head coil at the York University Neuroimaging Center in Toronto.
T1-MPRAGE
T1 anatomical scans on the GE were acquired using a T1-weighted volumetric magnetization prepared rapid gradient echo sequence (TR = 2530 ms; TE = 3.4 ms; 7° flip angle; 1 mm isotropic voxels, 176 slices, 5m25s) with 2x acceleration with sensitivity encoding. On the Siemens, anatomical scans were acquired using a T1-weighted volumetric magnetization prepared rapid gradient echo sequence (TR = 1900ms; TE = 2.52 ms; 9° flip angle; 1 mm isotropic voxels, 192 slices, 4m26s) with 2x acceleration and generalized auto calibrating partially parallel acquisition (GRAPPA) encoding at an iPAT acceleration factor of 2.
T2-FLAIR
A subset of 110 older adults and 148 younger adults have T2-FLAIR images. T2-weighted FLAIR sequences were acquired on a GE (TR = 12000 ms; TE = 95 ms; TI = 2712 ms; 160° flip angle; 42 slices of 1x1x3 mm; 2m36s) and Siemens (TR = 12000 ms; TE = 95 ms; TI = 2759.4 ms; 160° flip angle; 44 slices of 0.8 × 0.8 × 3 mm; 3m38s). 12 participants had FLAIR images with 46 slices acquired due to technician error, detailed in the README and participants.tsv files on OpenNeuro33.
Resting-state ME-fMRI
All participants completed two 10m06s resting-state multi-echo BOLD functional scans. Participants were instructed to keep their eyes open, blinking and breathing normally in the dimly lit scanner bay. Resting-state runs were acquired using a multi-echo (ME) EPI sequence on GE (TR = 3000 ms; TE1 = 13.7 ms, TE2 = 30 ms, TE3 = 47 ms; 83° flip angle; matrix size = 72 × 72; field of view (FOV) = 210 mm; 46 axial slices; 3 mm isotropic voxels; 204 volumes, 2.5x acceleration with sensitivity encoding) and Siemens (TR = 3000 ms; TE1 = 14 ms, TE2 = 29.96 ms, TE3 = 45.92 ms; 83° flip angle; matrix size = 64 × 64; FOV = 216 mm; 43 axial slices; 3.4 × 3.4 × 3mm voxels; 200 volumes, 3x acceleration and GRAPPA encoding) scanners. One participant (sub-149) had 206 volumes collected instead of 204: This discrepancy is detailed in the README and participants.tsv file on OpenNeuro33. For 233 participants scanned on the GE, pulse and respiration were monitored continuously during scanning using an integrated pulse oximeter and respiratory belt. Note that due to a software upgrade, physiological sampling varies between participants at 50 Hz or 40 Hz, as indicated in the Data Records.
Data collection quality assurance and control
A number of measures were taken to ensure reliable high quality behavioral and neuroimaging data collection.
In lab behavioral data were collected by a trained psychometrist. All behavioral data were then quality controlled before and after compilation. Paper and pencil measures were digitized by two researchers to ensure accuracy. Online data collection included multiple attention checks. Participants with incorrect responses to 4 or more checks were excluded. Participants who answered 3 or more different questionnaires uniformly (i.e., without variation in the Likert ratings) were excluded completely, along with participants missing more than 15% of total behavioral data. Participants missing more than 15% of any given measure were not included in any analysis with that measure.
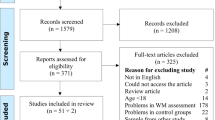
Prior to undergoing MRI scanning, all participants were informed about the importance of staying still during the MR scan. All scans at the Cornell Magnetic Resonance Imaging Facility and York University Neuroimaging Center were performed by a trained MR technician working with a standardized protocol. This ensured consistent data acquisition procedures, including visual checks for coverage, ongoing quality assessment, and confirmation of participant wakefulness between runs. Five participants were initially excluded after visual inspection of anatomical scans revealed anomalies. One younger participant had a hyperintensity in the posterior lateral ventricle. One younger and four older adults had extended basal ganglia lesions of unknown etiology resembling perivascular spaces34,35. As the cognitive consequences of perivascular spaces in cognitively healthy adults remain unknown (e.g.36,37), these participants were excluded from our sample. Image quality assessment was then performed on each functional run following preprocessing to exclude participants with unsuccessful coregistration, residual noise (framewise displacement > 0.50 mm coupled with denoised data with DVARS > 138), a temporal signal-to-noise ratio <50, or an insufficient amount of data retained after denoising (<10 BOLD components; see BOLD dimensionality below). Only participants with two functional runs that met these criteria were included in our final sample. 9 younger and 24 older adults were excluded on this basis.
Quality metrics on the final sample are discussed below.
Data Records
All demographic information, in addition to cognitive, behavioral and personality variables, is available within the Open Science Framework project “Goal-Directed Cognition in Older and Younger Adults” contributed by R.N.S. (https://doi.org/10.17605/OSF.IO/YHZXE; http://osf.io/yhzxe/39). All neuroimaging data are available on OpenNeuro following Brain Imaging Data Structure (BIDS) specification40 along with a detailed descriptor of acquisition parameters (https://doi.org/10.18112/openneuro.ds003592.v1.0.833). All data is shared under the Creative Commons license CC0.
Demographics, Cognitive, Behavioral and Personality Assessment
Location: ddbehav.csv
File format: plain text, comma-separated values
Basic demographic information including gender, age, race, and ethnicity is available.
All demographic information is available as a comma-separated value (CSV) file.
T1 Anatomical scans
Location: sub- <ID> /ses-1/anat/sub- <ID>_ses-1-T1w.nii.gz
File format: NIfTI, gzip-compressed
MRI data are available in NIfTI file format. All structural scans have been defaced as part of the de-identifying process.
T2-FLAIR scans
Location: sub- <ID> /ses-1/anat/sub- <ID>_ses-1_FLAIR.nii.gz
File format: NIfTI, gzip-compressed
Resting-state ME-fMRI
Location: sub- <ID> /ses- <SESSION> /func/sub- <ID>_ses- <SESSION>_task-rest_echo[1-3]_bold.nii.gz
File format: NIfTI, gzip-compressed
Physiological recordings
Location: sub- <ID> /ses- <SESSION> /func/sub- <ID>_ses- <SESSION>_task-rest_physio.tsv.gz
File format: plain text, tab-separated values
Physiological recordings for respiration and heart rate are provided as a tab-separated value (TSV) file. Accompanying meta-data in JSON format indicates the sampling frequency.
Technical Validation
Cognitive, Behavioral and Personality Assessment
Composite scores of episodic memory, semantic memory, and executive function were created from cognitive measures. Missing cells were first imputed with age group means (36 younger adults and 42 older adults had at least one cell missing). Latency scores on the Trail Making Task were reversed so that higher values on all measures reflected better performance. Scores were then z-scored and averaged for each composite. Episodic memory included scores on Verbal Paired Associates, Associative Recall, NIH Cognition Rey Auditory Verbal Learning, and NIH Cognition Picture Sequence Memory; Semantic memory included scores on Shipley Vocabulary, NIH Cognition Picture Vocabulary, and NIH Cognition Oral Reading Recognition; Executive function included scores on the Trail Making Task, NIH Cognition Flanker Inhibitory Control and Attention, NIH Cognition Dimensional Change Card Sort, and NIH Cognition List Sort Working Memory. Processing speed was additionally measured with the Symbol Digits Modalities Task.
Descriptive statistics for all cognitive measures are shown in Table 1. Overall, younger adults had higher episodic memory (t(281) = 17.51, p < 0.001, [1.10, 1.38], Cohen’s d = 2.11), executive function (t(281) = 12.67, p < 0.001, [0.71, 0.97], Cohen’s d = 1.52), and processing speed (t(281) = 15.03, p < 0.001, [1.17, 1.53], Cohen’s d = 1.81) scores than older adults. Older adults had higher semantic memory scores (t(281) = 9.18, p < 0.001, [−1.00, −0.65], Cohen’s d = 1.10) than younger adults. These results remained when controlling for site, gender, and education.
Table 2 contains descriptive statistics for all individual measures included in the index scores. Table 3 contains descriptive statistics for all self-report measures.
T1-MPRAGE
Cortical reconstruction and volumetric segmentation was performed with FreeSurfer version 6.0.141,42. All participant surfaces had a Euler number of 2, indicating that no holes or defects were detected across the entire sample. Estimated total intracranial volume (eTIV), grey matter, white matter, hippocampus, BA45, V1, and MT volumes were extracted. These regions were selected for divergent susceptibilities to age-related volume reductions. Heteromodal cortices (prefrontal BA 45) and hippocampus characteristically show significant age-related volume losses, while volumes in unimodal cortices (V1, MT) are comparatively preserved into older age (43,44,45,46,47and see8, for a review). Regional volumes were adjusted for head size by using the residuals of a linear regression between each volume, as output by FreeSurfer, and eTIV48,49,50. Adjusted volumes for each hemisphere were summed to yield a single adjusted volume for each region. Estimated whole brain volume (eWBV) was also calculated as (grey matter + white matter)/eTIV. A series of ANCOVAs were then conducted to test for age group differences on volume with site, gender, education, and eWBV (regional volumes only) as covariates. Inclusion of eWBV provides additional estimation of specificity, particularly given global atrophy that occurs with aging (e.g.51,). Education was not recorded for 14 young adult participants.
Volume distributions are plotted by age group in Fig. 1. Younger and older adults had comparable head sizes (Fig. 1A; F(1, 282) = 0.08, p = 0.784, ηp2 = 0.00), but younger adults had higher grey matter volume (Fig. 1B; F(1,282) = 165.58, p < 0.001, ηp2 = 0.37). Fig. 1C illustrates higher regional volumes in the hippocampus (F(1,281) = 12.60, p < 0.001, ηp2 = 0.04), BA45 (F(1,281) = 116.67, p < 0.001, ηp2 = 0.29), and MT (F(1,281) = 20.06, p < 0.001, ηp2 = 0.07) in younger adults compared to older adults. V1 volumes were similar in younger and older adults (F(1,281) = 0.54, p = 0.463, ηp2 = 0.00).
Structural MRI MPRAGE technical validation. (A) Estimated total intracranial volume (eTIV) in younger and older adults. (B) Grey matter volume in younger and older adults. (C) Hippocampal, lateral prefrontal (BA45), primary visual cortex (V1) and Motion Complex (MT) volumes in younger and older adults. Regional volumes were adjusted for eTIV. * indicates significant age group differences as determined by ANCOVAs controlling for site, gender, education, and eWBV (regional volumes only).
T2-FLAIR
T2-FLAIR sequences were used to evaluate white matter hyperintensities (WMH) in 105 healthy older adults (57% female; Mage = 68.35; age range = 60–83 y). WMH were segmented by the lesion prediction algorithm (Schmidt, 2017, Chapter 6.1) as implemented in the Lesion Segmentation Toolbox version 2.0.15 (www.statistical-modelling.de/lst.html) for Statistical Parametric Mapping. Each participant’s raw total lesion volume in cubic millimetres (mm3) was then divided by their eTIV derived from the T1 image in mm3 to correct for head size. Final total lesion volume and number of lesions data were converted to within-sample z-scores for subsequent analysis. We characterized white matter lesion load, indexed by total lesion volume and number of lesions, and examined the validity of these indices to confirm that estimates of white matter lesion load in our sample demonstrated patterns previously established in the literature43,52,53,54,55. This was accomplished by examining white matter lesion load associations with age and cognition. Consistent with expectation, total lesion volume and number of lesions were positively correlated (r(103) = 0.730, p < 0.001, [0.60, 0.83]). White matter lesion load was then examined for its associations with age and cognitive performance. Both total lesion volume and number of lesions were positively correlated with age (r(103) = 0.562, p < 0.001, [0.42, 0.68]; r(103) = 0.398, p < 0.001, [0.23, 0.55], respectively). Both total lesion volume and number of lesions were negatively associated with the NIH fluid IQ composite score (r(101) = −0.220, p = 0.013, [−0.36, −0.05]; r(101) = −0.227, p = 0.011, [−0.37, −0.07], respectively). The associations between white matter lesion load and fluid IQ held when controlling for site, gender, age and education (total lesion volume: pr(97) = −0.179, p = 0.038, [−0.34, 0.03]; number of lesions: pr(97) = −0.017, p = 0.046, [−0.32, −0.02]. See Fig. 2.
Technical validation of FLAIR images and white matter hyperintensities (A) Total lesion volume is associated with number of lesions. Increasing age is associated with (B) Total lesion volume, and, (C) Number of lesions. Fluid-IQ is negatively associated with (D) Total lesion volume, and, (E) Number of lesions. Total lesion volume is corrected for intracranial volume.
Resting-state ME-fMRI
To assess fMRI scan quality, quality metrics were calculated for each scan. Functional images were preprocessed with ME-ICA (version 3.2 beta56,57).
Framewise Displacement (FD)
A measure of the frame-to-frame movement, assessed in millimetres. FD was calculated on the second echo image for each resting-state scan using weighted scaling38. In younger adults, the average FD was 0.10 mm (SD = 0.05); in older adults, the average FD was 0.13 mm (SD = 0.05 mm).
Temporal Signal to Noise Ratio (tSNR)
A measure of signal strength at the voxel level, calculated as the mean signal intensity of a voxel across the timeseries divided by its standard deviation. tSNR was calculated on each run of ME-ICA denoised data in native space (see17 for a comparison of single-echo and multi-echo). Following Kundu and colleagues56, tSNR was quantified within the conjunction of grey matter and functional masks. Skull-stripped anatomical images were resampled to functional resolution and segmented with FSL FAST to create the grey matter mask. AFNI 3dAutomask was applied to the functional data to create the functional mask. The median of all voxels within this mask is used to characterize each run of resting-state fMRI, where higher tSNR values reflect clearer signal. Median tSNR values for younger adults ranged from 140.10–361.37, and for older adults from 129.59–418.90. For visualization purposes, tSNR spatial maps were separately derived in standard MNI space across the whole brain. Maps were averaged across all participants, thresholded at 50, and plotted in Fig. 3A. The results clearly demonstrate high tSNR throughout the cortical mantle in both cohorts.
Functional MRI technical validation. (A) Temporal signal-to-noise map across the full sample. (B) BOLD signal dimensionality across runs (left) and in younger and older adults. (C) Resting-state functional connectivity for younger (left) and older (middle) adults. (D) Age-related differences in connectivity between younger and older adults. Red color indicates significantly greater connectivity in younger adults, and blue color indicates significantly greater connectivity in older adults. (E) Resting-state functional connectivity across runs (sample mean edge-weights). VIS = visual, SOM = somatomotor, DAN = dorsal attention, VAN = ventral attention, LIM = limbic, FPC = frontoparietal control, DN = default, RSFC = resting-state functional connectivity.
BOLD dimensionality
A unique advantage of ME-fMRI and the ME-ICA processing framework is that BOLD and non-BOLD signals can be separated into independent components. A novel metric of “BOLD dimensionality”58, or the number of BOLD components identified in the ME-fMRI timeseries, may then be examined. We assessed test-retest reliability of BOLD dimensionality across two runs of data and compared BOLD dimensionality between younger and older adults. BOLD dimensionality was stable across resting-state fMRI runs (r(299) = 0.79, p < 0.001, [0.75, 0.83]; Fig. 3B left panel). Younger adults showed greater BOLD dimensionality than older adults (t(299) = 15.38, p < 0.001, [20.06, 25.95], Cohen’s d = 1.81; Fig. 3B right panel). This remained true when controlling for site, gender, education, and eWBV (F(1,281) = 97.07, p < 0.001; ηp2 = 0.26).
Connectomics
Whole-brain interregional functional connectivity was computed and compared between younger and older adults. Group mean connectivity matrices are in Fig. 3C. Age-related differences in the 79800 interregional connections (i.e., the lower triangle of the 400 × 400 functional connectivity matrix59; individualized with Group Prior Individualized Parcellations60) were quantitatively assessed with Partial Least Squares61,62. A significant latent variable (permuted p = 0.001) revealed a pattern of age differences in RSFC, with increases and decreases observed across the connectome (Fig. 3D). See Setton and Mwilambwe-Tshilobo et al.7 for in depth assessment.
Code availability
ME-ICA uses AFNI and python, both of which are open-source software. ME-ICA processing code is available at https://github.com/ME-ICA/me-ica. As the code base is unmaintained, readers are also directed to https://tedana.readthedocs.io/ for additional multi-echo de-noising options.
Change history
24 April 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41597-024-03265-5
References
Mar, R. A., Spreng, R. N. & Deyoung, C. G. How to produce personality neuroscience research with high statistical power and low additional cost. Cogn Affect Behav Neurosci 13, 674–685, https://doi.org/10.3758/s13415-013-0202-6 (2013).
Hemphill, J. F. Interpreting the magnitudes of correlation coefficients. Am. Psychol. 58, 78–79 (2003).
Frayley, R. C. & Marks, M. J. in Handbook of research methods in personality psychology (eds R.W. Robins, R.C. Frayley, & R.F. Krueger) 149-169 (The Guilford Press, 2007).
Gignac, G. E. & Szodorai, E. T. Effect size guidelines for individual differences researchers. Personality and Individual Differences 102, 74–78 (2016).
Park, D. C., Polk, T. A., Mikels, J. A., Taylor, S. F. & Marshuetz, C. Cerebral aging: integration of brain and behavioral models of cognitive function. Dialogues in clinical neuroscience 3, 151–165 (2001).
Damoiseaux, J. S. Effects of aging on functional and structural brain connectivity. NeuroImage 160, 32–40, https://doi.org/10.1016/j.neuroimage.2017.01.077 (2017).
Setton, R. et al. Age differences in the functional architecture of the human brain. Cereb. Cortex, https://doi.org/10.1093/cercor/bhac056 (in press).
Spreng, R. N. & Turner, G. R. in The aging brain (ed G. R. Samanez-Larkin) (American Psychological Association, 2019).
Spreng, R. N. & Turner, G. R. The shifting architecture of cognition and brain function in older adulthood. Perspect Psychol Sci, 14, 523–542, https://doi.org/10.1177/1745691619827511 (2019).
Kundu, P. et al. Multi-echo fMRI: A review of applications in fMRI denoising and analysis of BOLD signals. NeuroImage 154, 59–80, https://doi.org/10.1016/j.neuroimage.2017.03.033 (2017).
Power, J. D. et al. Ridding fMRI data of motion-related influences: Removal of signals with distinct spatial and physical bases in multiecho data. Proc. Natl. Acad. Sci. USA 115, E2105–E2114, https://doi.org/10.1073/pnas.1720985115 (2018).
Spreng, R. N., Fernandez-Cabello, S., Turner, G. R. & Stevens, W. D. Take a deep breath: Multiecho fMRI denoising effectively removes head motion artifacts, obviating the need for global signal regression. Proc. Natl. Acad. Sci. USA 116, 19241–19242, https://doi.org/10.1073/pnas.1909848116 (2019).
Lynch, C. J. et al. Rapid Precision Functional Mapping of Individuals Using Multi-Echo fMRI. Cell Rep 33, 108540, https://doi.org/10.1016/j.celrep.2020.108540 (2020).
Baracchini, G. et al. Inter-regional BOLD signal variability is an organizational feature of functional brain networks. NeuroImage 237, 118149, https://doi.org/10.1016/j.neuroimage.2021.118149 (2021).
Spreng, R. N. et al. Semanticized autobiographical memory and the default-executive coupling hypothesis of aging. Neuropsychologia 110, 37–43, https://doi.org/10.1016/j.neuropsychologia.2017.06.009 (2018).
Huang, S. et al. Age differences in intuitive moral decision-making: Associations with inter-network neural connectivity. Psychol. Aging 36, 902–916, https://doi.org/10.1037/pag0000633 (2021).
DuPre, E., Luh, W. M. & Spreng, R. N. Multi-echo fMRI replication sample of autobiographical memory, prospection and theory of mind reasoning tasks. Scientific data 3, 160116, https://doi.org/10.1038/sdata.2016.116 (2016).
Geerligs, L., Cam, C. A. N. & Campbell, K. L. Age-related differences in information processing during movie watching. Neurobiol. Aging 72, 106–120, https://doi.org/10.1016/j.neurobiolaging.2018.07.025 (2018).
Kantarovich, K. et al. White matter lesion load is associated with lower within- and greater between- network connectivity across older age. Neurobiol. Aging, https://doi.org/10.1016/j.neurobiolaging.2022.01.005 (in press).
Beck, A. T., Steer, R. A. & Brown, G. K. Manual for the Beck Depression Inventory-II. (Psychological Corporation, 1996).
Yesavage, J. A. et al. Development and validation of a geriatric depression screening scale: a preliminary report. J. Psychiatr. Res. 17, 37–49 (1982).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Gershon, R. C. et al. NIH toolbox for assessment of neurological and behavioral function. Neurology 80, S2–6, https://doi.org/10.1212/WNL.0b013e3182872e5f (2013).
Wechsler, D. (Pearson., San Antonio, TX., 2009).
Brainerd, C. J. et al. Dual-retrieval models and neurocognitive impairment. J. Exp. Psychol. Learn. Mem. Cogn. 40, 41–65, https://doi.org/10.1037/a0034057 (2014).
Shipley, W. C., Gruber, C. P., Martin, T. A. & Klein, A. M. (Western Psycholigical Services, Los Angeles, CA., 2009).
Reitan, R. M. Validity of the trail making test as an indicator of organic brain damage. Perceptual and Motor Skills 8, 271–276 (1958).
Daneman, M. & Carpenter, P. A. Individual differences in working memory and reading. Journal of Verbal Learning & Verbal Behavior. Journal of Verbal Learning and Verbal Behavior 19, 450–466 (1980).
Smith, A. (Western Psychological Services, Los Angeles, CA., 1982).
Carver, C. S. & White, T. L. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. J. Pers. Soc. Psychol. 67, 319–333 (1994).
Davis, M. H. A multidimensional approach to individual differences in empathy. JSAS Catalog of Selected Documents in Psychology 10, 85 (1980).
DeYoung, C. G., Quilty, L. C. & Peterson, J. B. Between facets and domains: 10 aspects of the Big Five. J. Pers. Soc. Psychol. 93, 880–896, https://doi.org/10.1037/0022-3514.93.5.880 (2007).
Spreng, R.N. et al. Neurocognitive aging data release with behavioral, structural and multi-echo functional MRI measures. OpenNeuro https://doi.org/10.18112/openneuro.ds003592.v1.0.3 (2021).
Doubal, F. N., MacLullich, A. M., Ferguson, K. J., Dennis, M. S. & Wardlaw, J. M. Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke 41, 450–454, https://doi.org/10.1161/STROKEAHA.109.564914 (2010).
Potter, G. M. et al. Enlarged perivascular spaces and cerebral small vessel disease. Int J Stroke 10, 376–381, https://doi.org/10.1111/ijs.12054 (2015).
Hilal, S. et al. Enlarged perivascular spaces and cognition: A meta-analysis of 5 population-based studies. Neurology 91, e832–e842, https://doi.org/10.1212/WNL.0000000000006079 (2018).
Huijts, M. et al. Accumulation of MRI Markers of Cerebral Small Vessel Disease is Associated with Decreased Cognitive Function. A Study in First-Ever Lacunar Stroke and Hypertensive Patients. Frontiers in aging neuroscience 5, 72, https://doi.org/10.3389/fnagi.2013.00072 (2013).
Power, J. D., Barnes, K. A., Snyder, A. Z., Schlaggar, B. L. & Petersen, S. E. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. NeuroImage 59, 2142–2154, https://doi.org/10.1016/j.neuroimage.2011.10.018 (2012).
Spreng, R. N. Goal-Directed Cognition in Older and Younger Adults. OSF https://doi.org/10.17605/OSF.IO/YHZXE (2022).
Gorgolewski, K. J. et al. The brain imaging data structure, a format for organizing and describing outputs of neuroimaging experiments. Scientific data 3, 160044, https://doi.org/10.1038/sdata.2016.44 (2016).
Fischl, B. et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33, 341–355 (2002).
Reuter, M., Schmansky, N. J., Rosas, H. D. & Fischl, B. Within-subject template estimation for unbiased longitudinal image analysis. NeuroImage 61, 1402–1418, https://doi.org/10.1016/j.neuroimage.2012.02.084 (2012).
Raz, N. et al. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb. Cortex 15, 1676–1689, https://doi.org/10.1093/cercor/bhi044 (2005).
Salat, D. H. et al. Thinning of the cerebral cortex in aging. Cereb. Cortex 14, 721–730, https://doi.org/10.1093/cercor/bhh032 (2004).
Shaw, M. E., Sachdev, P. S., Anstey, K. J. & Cherbuin, N. Age-related cortical thinning in cognitively healthy individuals in their 60s: the PATH Through Life study. Neurobiol. Aging 39, 202–209, https://doi.org/10.1016/j.neurobiolaging.2015.12.009 (2016).
Storsve, A. B. et al. Differential longitudinal changes in cortical thickness, surface area and volume across the adult life span: regions of accelerating and decelerating change. J. Neurosci. 34, 8488–8498, https://doi.org/10.1523/JNEUROSCI.0391-14.2014 (2014).
Yang, Z. et al. Age-associated differences on structural brain MRI in nondemented individuals from 71 to 103 years. Neurobiol. Aging 40, 86–97, https://doi.org/10.1016/j.neurobiolaging.2016.01.006 (2016).
Jack, C. R. Jr. et al. Anterior temporal lobes and hippocampal formations: normative volumetric measurements from MR images in young adults. Radiology 172, 549–554, https://doi.org/10.1148/radiology.172.2.2748838 (1989).
Buckner, R. L. et al. A unified approach for morphometric and functional data analysis in young, old, and demented adults using automated atlas-based head size normalization: reliability and validation against manual measurement of total intracranial volume. NeuroImage 23, 724–738, https://doi.org/10.1016/j.neuroimage.2004.06.018 (2004).
Voevodskaya, O. et al. The effects of intracranial volume adjustment approaches on multiple regional MRI volumes in healthy aging and Alzheimer’s disease. Frontiers in aging neuroscience 6, 264, https://doi.org/10.3389/fnagi.2014.00264 (2014).
Schmitz, T. W. & Spreng, R. N. Alzheimer’s Disease Neuroimaging, I. Basal forebrain degeneration precedes and predicts the cortical spread of Alzheimer’s pathology. Nature communications 7, 13249, https://doi.org/10.1038/ncomms13249 (2016).
Cook, I. A. et al. Longitudinal progression of subclinical structural brain disease in normal aging. Am. J. Geriatr. Psychiatry 12, 190–200 (2004).
Gunning-Dixon, F. M. & Raz, N. The cognitive correlates of white matter abnormalities in normal aging: a quantitative review. Neuropsychology 14, 224–232, https://doi.org/10.1037//0894-4105.14.2.224 (2000).
Kramer, J. H. et al. Longitudinal MRI and cognitive change in healthy elderly. Neuropsychology 21, 412–418, https://doi.org/10.1037/0894-4105.21.4.412 (2007).
Vernooij, M. W. et al. Incidental findings on brain MRI in the general population. N. Engl. J. Med. 357, 1821–1828, https://doi.org/10.1056/NEJMoa070972 (2007).
Kundu, P. et al. Integrated strategy for improving functional connectivity mapping using multiecho fMRI. Proc. Natl. Acad. Sci. USA 110, 16187–16192, https://doi.org/10.1073/pnas.1301725110 (2013).
Kundu, P., Inati, S. J., Evans, J. W., Luh, W. M. & Bandettini, P. A. Differentiating BOLD and non-BOLD signals in fMRI time series using multi-echo EPI. NeuroImage 60, 1759–1770, https://doi.org/10.1016/j.neuroimage.2011.12.028 (2012).
Kundu, P. et al. The Integration of Functional Brain Activity from Adolescence to Adulthood. J. Neurosci. 38, 3559–3570, https://doi.org/10.1523/JNEUROSCI.1864-17.2018 (2018).
Schaefer, A. et al. Local-Global Parcellation of the Human Cerebral Cortex from Intrinsic Functional Connectivity MRI. Cereb. Cortex 28, 3095–3114, https://doi.org/10.1093/cercor/bhx179 (2018).
Chong, M. et al. Individual parcellation of resting fMRI with a group functional connectivity prior. NeuroImage 156, 87–100, https://doi.org/10.1016/j.neuroimage.2017.04.054 (2017).
Krishnan, A., Williams, L. J., McIntosh, A. R. & Abdi, H. Partial Least Squares (PLS) methods for neuroimaging: a tutorial and review. NeuroImage 56, 455–475, https://doi.org/10.1016/j.neuroimage.2010.07.034 (2011).
McIntosh, A. R. & Misic, B. Multivariate statistical analyses for neuroimaging data. Annu. Rev. Psychol. 64, 499–525, https://doi.org/10.1146/annurev-psych-113011-143804 (2013).
Acknowledgements
This project was supported in part by grants to RNS from the Canadian Institute of Health Research and NIH (1S10RR025145) and to G.R.T from the Natural Sciences and Engineering Research Council of Canada (Discovery Grant). The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Thanks go to Juliana Garcia, Niloufar A. Lueke, Emily Qualls, and Roy Proper for assistance with data collection and Sara Fernández-Cabello for assistance processing the Flair images.
Author information
Authors and Affiliations
Contributions
R.N.S. and G.R.T. designed the study; W.-M. L. and P.K. provided data acquisition methods; U.A., B.N.C., B.D. and A.W.L. facilitated data collection, R.S., E.D., K.K., A.W.L., and L.M.-T. processed, analyzed and organized the data; R.N.S., R.S., and G.R.T. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spreng, R.N., Setton, R., Alter, U. et al. Neurocognitive aging data release with behavioral, structural and multi-echo functional MRI measures. Sci Data 9, 119 (2022). https://doi.org/10.1038/s41597-022-01231-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41597-022-01231-7
- Springer Nature Limited
This article is cited by
-
Increased MRI-based Brain Age in chronic migraine patients
The Journal of Headache and Pain (2023)