Abstract
Migraine is a common, chronic, disorder that is typically characterized by recurrent disabling attacks of headache and accompanying symptoms, including aura. The aetiology is multifactorial with rare monogenic variants. Depression, epilepsy, stroke and myocardial infarction are comorbid diseases. Spreading depolarization probably causes aura and possibly also triggers trigeminal sensory activation, the underlying mechanism for the headache. Despite earlier beliefs, vasodilation is only a secondary phenomenon and vasoconstriction is not essential for antimigraine efficacy. Management includes analgesics or NSAIDs for mild attacks, and, for moderate or severe attacks, triptans or 5HT1B/1D receptor agonists. Because of cardiovascular safety concerns, unreliable efficacy and tolerability issues, use of ergots to abort attacks has nearly vanished in most countries. CGRP receptor antagonists (gepants) and lasmiditan, a selective 5HT1F receptor agonist, have emerged as effective acute treatments. Intramuscular onabotulinumtoxinA may be helpful in chronic migraine (migraine on ≥15 days per month) and monoclonal antibodies targeting CGRP or its receptor, as well as two gepants, have proven effective and well tolerated for the preventive treatment of migraine. Several neuromodulation modalities have been approved for acute and/or preventive migraine treatment. The emergence of new treatment targets and therapies illustrates the bright future for migraine management.





Similar content being viewed by others
References
Goadsby, P. J., Lipton, R. B. & Ferrari, M. D. Migraine–current understanding and treatment. N. Engl. J. Med. 346, 257–270 (2002).
Terwindt, G. M. et al. The impact of migraine on quality of life in the general population: the GEM study. Neurology 55, 624–629 (2000).
Jensen, R. & Stovner, L. J. Epidemiology and comorbidity of headache. Lancet Neurol. 7, 354–361 (2008).
Stovner, L. J. et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 17, 954–976 (2018).
[No authors listed] Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd Edition. Cephalalgia 38, 1–211 (2018).
Ashina, M. Migraine. N. Engl. J. Med. 383, 1866–1876 (2020).
Steiner, T. J. et al. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J. Headache Pain. 21, 137 (2020).
Launer, L. J., Terwindt, G. M. & Ferrari, M. D. The prevalence and characteristics of migraine in a population-based cohort: the GEM study. Neurology 53, 537–542 (1999).
Salomon, J. A. et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet 380, 2129–2143 (2012).
Hansen, J. M., Goadsby, P. J. & Charles, A. C. Variability of clinical features in attacks of migraine with aura. Cephalalgia 36, 216–224 (2015).
Giffin, N. J. et al. Premonitory symptoms in migraine: an electronic diary study. Neurology 60, 935–940 (2003).
Schoonman, G. G., Evers, D. J., Terwindt, G. M., van Dijk, J. G. & Ferrari, M. D. The prevalence of premonitory symptoms in migraine: a questionnaire study in 461 patients. Cephalalgia 26, 1209–1213 (2006).
Karsan, N. & Goadsby, P. J. Biological insights from the premonitory symptoms of migraine. Nat. Rev. Neurol. 14, 699–710 (2018).
Giffin, N. J., Lipton, R. B., Silberstein, S. D., Olesen, J. & Goadsby, P. J. The migraine postdrome. Neurology 87, 309–313 (2016).
Ferrari, M. D., Klever, R. R., Terwindt, G. M., Ayata, C. & van den Maagdenberg, A. M. J. M. Migraine pathophysiology: lessons from mouse models and human genetics. Lancet Neurol. 14, 65–80 (2015).
van Oosterhout, W. P. J. et al. Female sex hormones in men with migraine. Neurology 91, e374–e381 (2018).
Stewart, W. F., Wood, C., Reed, M. L., Roy, J. & Lipton, R. B. Cumulative lifetime migraine incidence in women and men. Cephalalgia 28, 1170–1178 (2008).
Bigal, M. E. & Lipton, R. B. The epidemiology, burden, and comorbidities of migraine. Neurol. Clin. 27, 321–334 (2009).
Merikangas, K. R. Contributions of epidemiology to our understanding of migraine. Headache 53, 230–246 (2013).
Stovner, L. J. et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 27, 193–210 (2007).
Ashina, M., Hansen, J. M. & Olesen, J. Pearls and pitfalls in human pharmacological models of migraine: 30 years’ experience. Cephalalgia 33, 540–553 (2013).
Diener, H.-C. et al. Chronic migraine–classification, characteristics and treatment. Nat. Rev. Neurol. 8, 162–171 (2012).
Sun-Edelstein, C., Rapoport, A. M., Rattanawong, W. & Srikiatkhachorn, A. The evolution of medication overuse headache: history, pathophysiology and clinical update. CNS Drugs 35, 545–565 (2021).
Louter, M. A. et al. Cutaneous allodynia as a predictor of migraine chronification. Brain 136, 3489–3496 (2013).
Ottman, R. & Lipton, R. B. Is the comorbidity of epilepsy and migraine due to a shared genetic susceptibility? Neurology 47, 918–924 (1996).
Bauer, P. Headache in people with epilepsy. Nat. Rev. Neurol. 17, 529–544 (2021).
Modgill, G., Jette, N., Wang, J. L., Becker, W. J. & Patten, S. B. A population-based longitudinal community study of major depression and migraine. Headache 52, 422–432 (2011).
Breslau, N., Lipton, R. B., Stewart, W. F., Schultz, L. R. & Welch, K. M. A. Comorbidity of migraine and depression: investigating potential etiology and prognosis. Neurology 60, 1308–1312 (2003).
The Brainstorm Consortium. et al. Analysis of shared heritability in common disorders of the brain. Science 360, eaap8757 (2018).
Tietjen, G. E. et al. High prevalence of somatic symptoms and depression in women with disabling chronic headache. Neurology 68, 134–140 (2007).
Sacco, S. & Kurth, T. Migraine and the risk for stroke and cardiovascular disease. Curr. Cardiol. Rep. 16, 524 (2014).
Etminan, M. Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies. BMJ 330, 60–63 (2005).
Schürks, M. et al. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ 339, b3914 (2009).
Spector, J. T. et al. Migraine headache and ischemic stroke risk: an updated meta-analysis. Am. J. Med. 123, 612–624 (2010).
Kurth, T., Chabriat, H. & Bousser, M.-G. Migraine and stroke: a complex association with clinical implications. Lancet Neurol. 11, 92–100 (2012).
Kurth, T. et al. Association of migraine with aura and other risk factors with incident cardiovascular disease in women. JAMA 323, 2281–2289 (2020).
Gudmundsson, L. S. et al. Migraine with aura and risk of cardiovascular and all cause mortality in men and women: prospective cohort study. BMJ 341, c3966 (2010).
Peng, K.-P., Chen, Y.-T., Fuh, J.-L., Tang, C.-H. & Wang, S.-J. Migraine and incidence of ischemic stroke: a nationwide population-based study. Cephalalgia 37, 327–335 (2016).
Martinez‐Majander, N. et al. Association between migraine and cryptogenic ischemic stroke in young adults. Ann. Neurol. 89, 242–253 (2021).
Li, L., Schulz, U. G., Kuker, W. & Rothwell, P. M. Age-specific association of migraine with cryptogenic TIA and stroke. Neurology 85, 1444–1451 (2015).
Monteith, T. S., Gardener, H., Rundek, T., Elkind, M. S. V. & Sacco, R. L. Migraine and risk of stroke in older adults. Neurology 85, 715–721 (2015).
Tzourio, C. et al. Migraine and risk of ischaemic stroke: a case-control study. BMJ 307, 289–292 (1993).
Tzourio, C. et al. Case-control study of migraine and risk of ischaemic stroke in young women. BMJ 310, 830–833 (1995).
Sacco, S., Ornello, R., Ripa, P., Pistoia, F. & Carolei, A. Migraine and hemorrhagic stroke: a meta-analysis. Stroke 44, 3032–3038 (2013).
Adelborg, K. et al. Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. BMJ 360, k96 (2018).
Kruit, M. C. Migraine as a risk factor for subclinical brain lesions. JAMA 291, 427–434 (2004).
Kruit, M. C., Launer, L. J., Ferrari, M. D. & van Buchem, M. A. Brain stem and cerebellar hyperintense lesions in migraine. Stroke 37, 1109–1112 (2006).
Kurth, T. et al. Headache, migraine, and structural brain lesions and function: population based epidemiology of vascular ageing-MRI study. BMJ 342, c7357 (2011).
Scher, A. I. Migraine headache in middle age and late-life brain infarcts. JAMA 301, 2563–2570 (2009).
Palm-Meinders, I. H. et al. Structural brain changes in migraine. JAMA 308, 1889–1897 (2012).
Gaist, D. et al. Migraine with aura and risk of silent brain infarcts and white matter hyperintensities: an MRI study. Brain 139, 2015–2023 (2016).
Benedittis, G., Lorenzetti, A., Sina, C. & Bernasconi, V. Magnetic resonance imaging in migraine and tension-type headache. Headache 35, 264–268 (1995).
Takagi, H. & Umemoto, T., ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. A meta-analysis of case-control studies of the association of migraine and patent foramen ovale. J. Cardiol. 67, 493–503 (2016).
West, B. H. et al. Frequency of patent foramen ovale and migraine in patients with cryptogenic stroke. Stroke 49, 1123–1128 (2018).
Sen, S. et al. Migraine with visual aura is a risk factor for incident atrial fibrillation: a cohort study. Neurology 91, e2202–e2210 (2018).
Scher, A. I. et al. Cardiovascular risk factors and migraine: the GEM population-based study. Neurology 64, 614–620 (2005).
Kurth, T. et al. Migraine and risk of cardiovascular disease in women. JAMA 296, 283–291 (2006).
Kurth, T. Migraine and risk of cardiovascular disease in men. Arch. Intern. Med. 167, 795–801 (2007).
Bigal, M. E. et al. Migraine and cardiovascular disease: a population-based study. Neurology 74, 628–635 (2010).
Sacco, S. et al. Migraine and risk of ischaemic heart disease: a systematic review and meta-analysis of observational studies. Eur. J. Neurol. 22, 1001–1011 (2015).
Bushnell, C. D., Jamison, M. & James, A. H. Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. BMJ 338, b664 (2009).
Schürks, M., Winter, A., Berger, K. & Kurth, T. Migraine and restless legs syndrome: a systematic review. Cephalalgia 34, 777–794 (2014).
Scher, A. I., Stewart, W. F. & Lipton, R. B. The comorbidity of headache with other pain syndromes. Headache 46, 1416–1423 (2006).
Tietjen, G. E. et al. Allodynia in migraine: association with comorbid pain conditions. Headache 49, 1333–1344 (2009).
Fagherazzi, G. et al. Associations between migraine and type 2 diabetes in women: findings from the E3N cohort study. JAMA Neurol. 76, 257–263 (2019).
Ashina, M., Hansen, J. M., Á Dunga, B. O. & Olesen, J. Human models of migraine – short-term pain for long-term gain. Nat. Rev. Neurol. 13, 713–724 (2017).
Lashley, K. S. Patterns of cerebral integration indicated by the scotomas of migraine. Arch. Neurol. Psychiatry 46, 331–339 (1941).
Hansen, J. M., Baca, S. M., VanValkenburgh, P. & Charles, A. Distinctive anatomical and physiological features of migraine aura revealed by 18 years of recording. Brain 136, 3589–3595 (2013).
Charles, A. C. & Baca, S. M. Cortical spreading depression and migraine. Nat. Rev. Neurol. 9, 637–644 (2013).
Dreier, J. P. et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: review and recommendations of the COSBID research group. J. Cereb. Blood Flow. Metab. 37, 1595–1625 (2017).
Ayata, C. & Lauritzen, M. Spreading depression, spreading depolarizations, and the cerebral vasculature. Physiol. Rev. 95, 953–993 (2015).
Parker, P. D. et al. Non-canonical glutamate signaling in a genetic model of migraine with aura. Neuron 109, 611–628.e8 (2021).
Eikermann-Haerter, K. Neuronal plumes initiate spreading depolarization, the electrophysiologic event driving migraine and stroke. Neuron 109, 563–565 (2021).
Hadjikhani, N. et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc. Natl Acad. Sci. USA 98, 4687–4692 (2001).
Arngrim, N. et al. Heterogenous migraine aura symptoms correlate with visual cortex functional magnetic resonance imaging responses. Ann. Neurol. 82, 925–939 (2017).
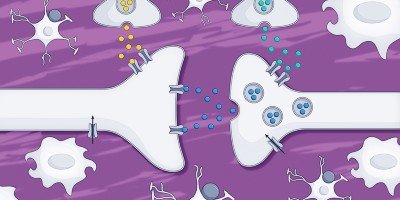
Ashina, M. et al. Migraine and the trigeminovascular system–40 years and counting. Lancet Neurol. 18, 795–804 (2019).
Goadsby, P. J. et al. Pathophysiology of migraine: a disorder of sensory processing. Physiol. Rev. 97, 553–622 (2017).
Burstein, R. & Jakubowski, M. Unitary hypothesis for multiple triggers of the pain and strain of migraine. J. Comp. Neurol. 493, 9–14 (2005).
Maniyar, F. H., Sprenger, T., Monteith, T., Schankin, C. & Goadsby, P. J. Brain activations in the premonitory phase of nitroglycerin-triggered migraine attacks. Brain 137, 232–241 (2013).
Noseda, R., Jakubowski, M., Kainz, V., Borsook, D. & Burstein, R. Cortical projections of functionally identified thalamic trigeminovascular neurons: implications for migraine headache and its associated symptoms. J. Neurosci. 31, 14204–14217 (2011).
Zhang, X. et al. Activation of central trigeminovascular neurons by cortical spreading depression. Ann. Neurol. 69, 855–865 (2011).
Zhang, X. et al. Activation of meningeal nociceptors by cortical spreading depression: implications for migraine with aura. J. Neurosci. 30, 8807–8814 (2010).
Noseda, R., Constandil, L., Bourgeais, L., Chalus, M. & Villanueva, L. Changes of meningeal excitability mediated by corticotrigeminal networks: a link for the endogenous modulation of migraine pain. J. Neurosci. 30, 14420–14429 (2010).
Schain, A. J. et al. Activation of pial and dural macrophages and dendritic cells by cortical spreading depression. Ann. Neurol. 83, 508–521 (2018).
Schain, A. J., Melo-Carrillo, A., Strassman, A. M. & Burstein, R. Cortical spreading depression closes paravascular space and impairs glymphatic flow: implications for migraine headache. J. Neurosci. 37, 2904–2915 (2017).
Karatas, H. et al. Spreading depression triggers headache by activating neuronal Panx1 channels. Science 339, 1092–1095 (2013).
Ayata, C. Cortical spreading depression triggers migraine attack: pro. Headache 50, 725–730 (2010).
Charles, A. Does cortical spreading depression initiate a migraine attack? Maybe not. Headache 50, 731–733 (2010).
Ayata, C., Jin, H., Kudo, C., Dalkara, T. & Moskowitz, M. A. Suppression of cortical spreading depression in migraine prophylaxis. Ann. Neurol. 59, 652–661 (2006).
Bogdanov, V. B. et al. Migraine preventive drugs differentially affect cortical spreading depression in rat. Neurobiol. Dis. 41, 430–435 (2011).
Ayata, C. Spreading depression: from serendipity to targeted therapy in migraine prophylaxis. Cephalalgia 29, 1095–1114 (2009).
Edvinsson, L., Haanes, K. A., Warfvinge, K. & Krause, D. N. CGRP as the target of new migraine therapies–successful translation from bench to clinic. Nat. Rev. Neurol. 14, 338–350 (2018).
Knight, Y. E., Edvinsson, L. & Goadsby, P. J. 4991W93 inhibits release of calcitonin gene-related peptide in the cat but only at doses with 5HT(1B/1D) receptor agonist activity? Neuropharmacology 40, 520–525 (2001).
Goadsby, P. J., Edvinsson, L. & Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 28, 183–187 (1990).
Goadsby, P. J. & Edvinsson, L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann. Neurol. 33, 48–56 (1993).
Olesen, J. et al. Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N. Engl. J. Med. 350, 1104–1110 (2004).
Tvedskov, J. F. et al. No increase of calcitonin gene-related peptide in jugular blood during migraine. Ann. Neurol. 58, 561–568 (2005).
Melo-Carrillo, A. et al. Fremanezumab — a humanized monoclonal anti-CGRP antibody — inhibits thinly myelinated (Aδ) but not unmyelinated (C) meningeal nociceptors. J. Neurosci. 37, 10587–10596 (2017).
Melo-Carrillo, A. et al. Selective inhibition of trigeminovascular neurons by fremanezumab: a humanized monoclonal anti-CGRP antibody. J. Neurosci. 37, 7149–7163 (2017).
Strassman, A. M., Raymond, S. A. & Burstein, R. Sensitization of meningeal sensory neurons and the origin of headaches. Nature 384, 560–564 (1996).
Burstein, R., Yamamura, H., Malick, A. & Strassman, A. M. Chemical stimulation of the intracranial dura induces enhanced responses to facial stimulation in brain stem trigeminal neurons. J. Neurophysiol. 79, 964–982 (1998).
Burstein, R., Yarnitsky, D., Goor-Aryeh, I., Ransil, B. J. & Bajwa, Z. H. An association between migraine and cutaneous allodynia. Ann. Neurol. 47, 614–624 (2000).
Burstein, R. The development of cutaneous allodynia during a migraine attack: clinical evidence for the sequential recruitment of spinal and supraspinal nociceptive neurons in migraine. Brain 123, 1703–1709 (2000).
Akerman, S., Holland, P. R. & Goadsby, P. J. Diencephalic and brainstem mechanisms in migraine. Nat. Rev. Neurosci. 12, 570–584 (2011).
Schulte, L. H., Mehnert, J. & May, A. Longitudinal neuroimaging over 30 days: temporal characteristics of migraine. Ann. Neurol. 87, 646–651 (2020).
Schulte, L. H. & May, A. The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain 139, 1987–1993 (2016).
Weiller, C. et al. Brain stem activation in spontaneous human migraine attacks. Nat. Med. 1, 658–660 (1995).
Goadsby, P. A review of paroxysmal hemicranias, SUNCT syndrome and other short-lasting headaches with autonomic feature, including new cases. Brain 120, 193–209 (1997).
Sprenger, T. & Goadsby, P. J. What has functional neuroimaging done for primary headache and for the clinical neurologist? J. Clin. Neurosci. 17, 547–553 (2010).
Andreou, A. P., Summ, O., Charbit, A. R., Romero-Reyes, M. & Goadsby, P. J. Animal models of headache: from bedside to bench and back to bedside. Expert Rev. Neurother. 10, 389–411 (2010).
Knight, Y. E., Bartsch, T., Kaube, H. & Goadsby, P. J. P/Q-type calcium-channel blockade in the periaqueductal gray facilitates trigeminal nociception: a functional genetic link for migraine? J. Neurosci. 22, RC213 (2002).
Bartsch, T., Knight, Y. E. & Goadsby, P. J. Activation of 5-HT1B/1D receptor in the periaqueductal gray inhibits nociception. Ann. Neurol. 56, 371–381 (2004).
Bergerot, A., Storer, R. J. & Goadsby, P. J. Dopamine inhibits trigeminovascular transmission in the rat. Ann. Neurol. 61, 251–262 (2007).
Charbit, A. R., Akerman, S. & Goadsby, P. J. Trigeminocervical complex responses after lesioning dopaminergic A11 nucleus are modified by dopamine and serotonin mechanisms. Pain 152, 2365–2376 (2011).
Lauritzen, M. & Olesen, J. E. S. Regional cerebral blood flow during migraine attacks by xenon-133 inhalation and emission tomography. Brain 107, 447–461 (1984).
Olesen, J., Burstein, R., Ashina, M. & Tfelt-Hansen, P. Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurol. 8, 679–690 (2009).
Charles, A. Vasodilation out of the picture as a cause of migraine headache. Lancet Neurol. 12, 419–420 (2013).
Schoonman, G. G. et al. Migraine headache is not associated with cerebral or meningeal vasodilatation–a 3T magnetic resonance angiography study. Brain 131, 2192–2200 (2008).
Amin, F. M. et al. Magnetic resonance angiography of intracranial and extracranial arteries in patients with spontaneous migraine without aura: a cross-sectional study. Lancet Neurol. 12, 454–461 (2013).
Khan, S. et al. Meningeal contribution to migraine pain: a magnetic resonance angiography study. Brain 142, 93–102 (2019).
Christensen, C. E. et al. Intradural artery dilation during experimentally induced migraine attacks. Pain 162, 176–183 (2021).
May, A. New insights into headache: an update on functional and structural imaging findings. Nat. Rev. Neurol. 5, 199–209 (2009).
Zielman, R. et al. Cortical glutamate in migraine. Brain 140, 1859–1871 (2017).
Russell, M. B. & Olesen, J. Increased familial risk and evidence of genetic factor in migraine. BMJ 311, 541–544 (1995).
Ulrich, V., Gervil, M., Fenger, K., Olesen, J. & Russell, M. B. The prevalence and characteristics of migraine in twins from the general population. Headache 39, 173–180 (1999).
Gormley, P. et al. Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nat. Genet. 48, 856–866 (2016).
de Vries, B. et al. Systematic re-evaluation of genes from candidate gene association studies in migraine using a large genome-wide association data set. Cephalalgia 36, 604–614 (2015).
Gormley, P. et al. Common variant burden contributes to the familial aggregation of migraine in 1,589 families. Neuron 98, 743–753.e4 (2018).
Oexle, K. & Winkelmann, J. Common grounds for family maladies. Neuron 98, 671–672 (2018).
Joutel, A. et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature 383, 707–710 (1996).
Chabriat, H. et al. Clinical spectrum of CADASIL: a study of 7 families. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Lancet 346, 934–939 (1995).
Richards, A. et al. C-terminal truncations in human 3′-5′ DNA exonuclease TREX1 cause autosomal dominant retinal vasculopathy with cerebral leukodystrophy. Nat. Genet. 39, 1068–1070 (2007).
Stam, A. H. et al. Retinal vasculopathy with cerebral leukoencephalopathy and systemic manifestations. Brain 139, 2909–2922 (2016).
Terwindt, G. Clinical and genetic analysis of a large Dutch family with autosomal dominant vascular retinopathy, migraine and Raynaud’s phenomenon. Brain 121, 303–316 (1998).
Pelzer, N. et al. Systemic features of retinal vasculopathy with cerebral leukoencephalopathy and systemic manifestations: a monogenic small vessel disease. J. Intern. Med. 285, 317–332 (2019).
Xu, Y. et al. Functional consequences of a CKIδ mutation causing familial advanced sleep phase syndrome. Nature 434, 640–644 (2005).
Brennan, K. C. et al. Casein kinase I mutations in familial migraine and advanced sleep phase. Sci. Transl. Med. 5, 183ra56 (2013).
Russell, M. B. & Ducros, A. Sporadic and familial hemiplegic migraine: pathophysiological mechanisms, clinical characteristics, diagnosis, and management. Lancet Neurol. 10, 457–470 (2011).
Zhao, H. et al. Gene-based pleiotropy across migraine with aura and migraine without aura patient groups. Cephalalgia 36, 648–657 (2015).
Pelzer, N., Stam, A. H., Haan, J., Ferrari, M. D. & Terwindt, G. M. Familial and sporadic hemiplegic migraine: diagnosis and treatment. Curr. Treat. Options Neurol. 15, 13–27 (2013).
Ophoff, R. A. et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 87, 543–552 (1996).
Fusco, M. D. et al. Haploinsufficiency of ATP1A2 encoding the Na+/K+ pump α2 subunit associated with familial hemiplegic migraine type 2. Nat. Genet. 33, 192–196 (2003).
Vanmolkot, K. R. J. et al. Novel mutations in the Na+,K+-ATPase pump gene ATP1A2 associated with familial hemiplegic migraine and benign familial infantile convulsions. Ann. Neurol. 54, 360–366 (2003).
Dichgans, M. et al. Mutation in the neuronal voltage-gated sodium channel SCN1A in familial hemiplegic migraine. Lancet 366, 371–377 (2005).
Pietrobon, D. Insights into migraine mechanisms and CaV2.1 calcium channel function from mouse models of familial hemiplegic migraine. J. Physiol. 588, 1871–1878 (2010).
Kahlig, K. M. et al. Divergent sodium channel defects in familial hemiplegic migraine. Proc. Natl Acad. Sci. USA 105, 9799–9804 (2008).
Cestele, S., Schiavon, E., Rusconi, R., Franceschetti, S. & Mantegazza, M. Nonfunctional NaV1.1 familial hemiplegic migraine mutant transformed into gain of function by partial rescue of folding defects. Proc. Natl Acad. Sci. USA 110, 17546–17551 (2013).
van den Maagdenberg, A. M. J. M. et al. A Cacna1a knockin migraine mouse model with increased susceptibility to cortical spreading depression. Neuron 41, 701–710 (2004).
van den Maagdenberg, A. M. J. M. et al. High cortical spreading depression susceptibility and migraine-associated symptoms in Cav2.1 S218L mice. Ann. Neurol. 67, 85–98 (2010).
Leo, L. et al. Increased susceptibility to cortical spreading depression in the mouse model of familial hemiplegic migraine type 2. PLoS Genet. 7, e1002129 (2011).
Eikermann-Haerter, K. et al. Genetic and hormonal factors modulate spreading depression and transient hemiparesis in mouse models of familial hemiplegic migraine type 1. J. Clin. Invest. 119, 99–109 (2009).
Eikermann-Haerter, K. et al. Androgenic suppression of spreading depression in familial hemiplegic migraine type 1 mutant mice. Ann. Neurol. 66, 564–568 (2009).
Eikermann-Haerter, K. et al. Enhanced subcortical spreading depression in familial hemiplegic migraine type 1 mutant mice. J. Neurosci. 31, 5755–5763 (2011).
Tottene, A. et al. Enhanced excitatory transmission at cortical synapses as the basis for facilitated spreading depression in CaV2.1 knockin migraine mice. Neuron 61, 762–773 (2009).
Capuani, C. et al. Defective glutamate and K+ clearance by cortical astrocytes in familial hemiplegic migraine type 2. EMBO Mol. Med. 8, 967–986 (2016).
Chanda, M. L. et al. Behavioral evidence for photophobia and stress-related ipsilateral head pain in transgenic Cacna1a mutant mice. Pain 154, 1254–1262 (2013).
Langford, D. J. et al. Coding of facial expressions of pain in the laboratory mouse. Nat. Methods 7, 447–449 (2010).
van Oosterhout, F. et al. Enhanced circadian phase resetting in R192Q Cav2.1 calcium channel migraine mice: circadian phase resetting. Ann. Neurol. 64, 315–324 (2008).
Eikermann-Haerter, K. et al. Migraine mutations increase stroke vulnerability by facilitating ischemic depolarizations. Circulation 125, 335–345 (2011).
Gao, Z. et al. Cerebellar ataxia by enhanced CaV2.1 currents is alleviated by Ca2+-dependent K+-channel activators in Cacna1aS218L mutant mice. J. Neurosci. 32, 15533–15546 (2012).
Pelzer, N. et al. Clinical spectrum of hemiplegic migraine and chances of finding a pathogenic mutation. Neurology 90, e575–e582 (2018).
Hiekkala, M. E. et al. The contribution of CACNA1A, ATP1A2 and SCN1A mutations in hemiplegic migraine: a clinical and genetic study in Finnish migraine families. Cephalalgia 38, 1849–1863 (2018).
Riant, F. et al. PRRT2 mutations cause hemiplegic migraine. Neurology 79, 2122–2124 (2012).
Pelzer, N. et al. PRRT2 and hemiplegic migraine: a complex association. Neurology 83, 288–290 (2014).
Bendtsen, L. et al. Guideline on the use of onabotulinumtoxinA in chronic migraine: a consensus statement from the European Headache Federation. J. Headache Pain. 19, 91 (2018).
Hoffmann, J. & Recober, A. Migraine and triggers: post hoc ergo propter hoc? Curr. Pain. Headache Rep. 17, 370 (2013).
Lipton, R. B., Pavlovic, J. M., Haut, S. R., Grosberg, B. M. & Buse, D. C. Methodological issues in studying trigger factors and premonitory features of migraine. Headache 54, 1661–1669 (2014).
Pavlovic, J. M., Buse, D. C., Sollars, C. M., Haut, S. & Lipton, R. B. Trigger factors and premonitory features of migraine attacks: summary of studies. Headache 54, 1670–1679 (2014).
Vollesen, A. L. H. et al. Effect of infusion of calcitonin gene-related peptide on cluster headache attacks: a randomized clinical trial. JAMA Neurol. 75, 1187–1197 (2018).
Vollesen, A. L. H. et al. The effect of pituitary adenylate cyclase-activating peptide-38 and vasoactive intestinal peptide in cluster headache. Cephalalgia 40, 1474–1488 (2020).
Chaitman, B. R. et al. A randomized, placebo-controlled study of the effects of telcagepant on exercise time in patients with stable angina. Clin. Pharmacol. Ther. 91, 459–466 (2012).
Brennan, K. C., Romero Reyes, M., López Valdés, H. E., Arnold, A. P. & Charles, A. C. Reduced threshold for cortical spreading depression in female mice. Ann. Neurol. 61, 603–606 (2007).
Lipton, R. B. et al. Reduction in perceived stress as a migraine trigger: testing the ‘let-down headache’ hypothesis. Neurology 82, 1395–1401 (2014).
Kelman, L. The triggers or precipitants of the acute migraine attack. Cephalalgia 27, 394–402 (2007).
Bigal, M. E. & Lipton, R. B. Modifiable risk factors for migraine progression. Headache 46, 1334–1343 (2006).
Schoonman, G. G. et al. Is stress a trigger factor for migraine? Psychoneuroendocrinology 32, 532–538 (2007).
Schulte, L. H., Menz, M. M., Haaker, J. & May, A. The migraineur’s brain networks: continuous resting state fMRI over 30 days. Cephalalgia 40, 1614–1621 (2020).
Borsook, D., Maleki, N., Becerra, L. & McEwen, B. Understanding migraine through the lens of maladaptive stress responses: a model disease of allostatic load. Neuron 73, 219–234 (2012).
Land, B. B. et al. The dysphoric component of stress is encoded by activation of the dynorphin κ-opioid system. J. Neurosci. 28, 407–414 (2008).
Bruchas, M. R., Land, B. B. & Chavkin, C. The dynorphin/kappa opioid system as a modulator of stress-induced and pro-addictive behaviors. Brain Res. 1314, 44–55 (2010).
Russell, M. B., Rasmussen, B. K., Fenger, K. & Olesen, J. Migraine without aura and migraine with aura are distinct clinical entities: a study of four hundred and eighty-four male and female migraineurs from the general population. Cephalalgia 16, 239–245 (1996).
Russell, M. B. & Olesen, J. A nosographic analysis of the migraine aura in a general population. Brain 119, 355–361 (1996).
Schott, G. D. Exploring the visual hallucinations of migraine aura: the tacit contribution of illustration. Brain 130, 1690–1703 (2007).
Yamani, N., Chalmer, M. A. & Olesen, J. Migraine with brainstem aura: defining the core syndrome. Brain 142, 3868–3875 (2019).
Do, T. P. et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology 92, 134–144 (2019).
Dodick, D. Pearls: headache. Semin. Neurol. 30, 74–81 (2010).
Vongvaivanich, K., Lertakyamanee, P., Silberstein, S. D. & Dodick, D. W. Late-life migraine accompaniments: a narrative review. Cephalalgia 35, 894–911 (2014).
Worthington, I. et al. Canadian Headache Society guideline: acute drug therapy for migraine headache. Can. J. Neurol. Sci. 40, S1–S3 (2013).
Roon, K. I. et al. No acute antimigraine efficacy of CP-122,288, a highly potent inhibitor of neurogenic inflammation: results of two randomized, double-blind, placebo-controlled clinical trials. Ann. Neurol. 47, 238–241 (2000).
Levy, D., Jakubowski, M. & Burstein, R. Disruption of communication between peripheral and central trigeminovascular neurons mediates the antimigraine action of 5HT1B/1D receptor agonists. Proc. Natl Acad. Sci. USA 101, 4274–4279 (2004).
Ferrari, M. D., Goadsby, P. J., Roon, K. I. & Lipton, R. B. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of a meta-analysis of 53 trials. Cephalalgia 22, 633–658 (2002).
Ferrari, M. D., Roon, K. I., Lipton, R. B. & Goadsby, P. J. Oral triptans (serotonin 5-HT1B/1D agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet 358, 1668–1675 (2001).
Subcutaneous Sumatriptan International Study Group Treatment of migraine attacks with sumatriptan. N. Engl. J. Med. 325, 316–321 (1991).
Thorlund, K. et al. Comparative efficacy of triptans for the abortive treatment of migraine: a multiple treatment comparison meta-analysis. Cephalalgia 34, 258–267 (2013).
Brandes, J. L. et al. Sumatriptan-naproxen for acute treatment of migraine. JAMA 297, 1443–1454 (2007).
Lipton, R. B. et al. Stratified care vs step care strategies for migraine: the Disability in Strategies of Care (DISC) Study: a randomized trial. JAMA 284, 2599–2605 (2000).
Pilgrim, A. J. Methodology of clinical trials of sumatriptan in migraine and cluster headache. Eur. Neurol. 31, 295–299 (1991).
Ferrari, M. D. Should we advise patients to treat migraine attacks early: methodologic issues. Eur. Neurol. 53, 17–21 (2005).
Bates, D. et al. Subcutaneous sumatriptan during the migraine aura. Neurology 44, 1587–1587 (1994).
Roberto, G. et al. Adverse cardiovascular events associated with triptans and ergotamines for treatment of migraine: systematic review of observational studies. Cephalalgia 35, 118–131 (2015).
Dodick, D. et al. Consensus statement: cardiovascular safety profile of triptans (5-HT1B/1D agonists) in the acute treatment of migraine. Headache 44, 414–425 (2004).
Roberto, G., Piccinni, C., D’Alessandro, R. & Poluzzi, E. Triptans and serious adverse vascular events: data mining of the FDA Adverse Event Reporting System database. Cephalalgia 34, 5–13 (2014).
Wammes-van der Heijden, E. A., Rahimtoola, H., Leufkens, H. G. M., Tijssen, C. C. & Egberts, A. C. G. Risk of ischemic complications related to the intensity of triptan and ergotamine use. Neurology 67, 1128–1134 (2006).
Ephross, S. A. & Sinclair, S. M. Final results from the 16-year sumatriptan, naratriptan, and treximet pregnancy registry. Headache 54, 1158–1172 (2014).
Orlova, Y., Rizzoli, P. & Loder, E. Association of coprescription of triptan antimigraine drugs and selective serotonin reuptake inhibitor or selective norepinephrine reuptake inhibitor antidepressants with serotonin syndrome. JAMA Neurol. 75, 566–572 (2018).
Tfelt-Hansen, P. Ergotamine in the acute treatment of migraine: a review and European consensus. Brain 123, 9–18 (2000).
Marmura, M. J., Silberstein, S. D. & Schwedt, T. J. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache 55, 3–20 (2015).
Rubio-Beltrán, E., Labastida-Ramírez, A., Villalón, C. M. & MaassenVanDenBrink, A. Is selective 5-HT1F receptor agonism an entity apart from that of the triptans in antimigraine therapy? Pharmacol. Ther. 186, 88–97 (2018).
Lipton, R. B. et al. Effect of ubrogepant vs placebo on pain and the most bothersome associated symptom in the acute treatment of migraine: the ACHIEVE II randomized clinical trial. JAMA 322, 1887–1898 (2019).
Lipton, R. B. et al. Rimegepant, an oral calcitonin gene-related peptide receptor antagonist, for migraine. N. Engl. J. Med. 381, 142–149 (2019).
Kuca, B. et al. Lasmiditan is an effective acute treatment for migraine: a phase 3 randomized study. Neurology 91, e2222–e2232 (2018).
Goadsby, P. J. et al. Phase 3 randomized, placebo-controlled, double-blind study of lasmiditan for acute treatment of migraine. Brain 142, 1894–1904 (2019).
Saengjaroentham, C. et al. Differential medication overuse risk of novel anti-migraine therapeutics. Brain 143, 2681–2688 (2020).
Chou, D. E. et al. Acute migraine therapy with external trigeminal neurostimulation (ACME): a randomized controlled trial. Cephalalgia 39, 3–14 (2019).
Schoenen, J. et al. Migraine prevention with a supraorbital transcutaneous stimulator: a randomized controlled trial. Neurology 80, 697–704 (2013).
Stanak, M., Wolf, S., Jagoš, H. & Zebenholzer, K. The impact of external trigeminal nerve stimulator (e-TNS) on prevention and acute treatment of episodic and chronic migraine: a systematic review. J. Neurol. Sci. 412, 116725 (2020).
Lipton, R. B. et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomised, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 9, 373–380 (2010).
Tassorelli, C. et al. Noninvasive vagus nerve stimulation as acute therapy for migraine: the randomized PRESTO study. Neurology 91, e364–e373 (2018).
Silberstein, S. D. et al. Chronic migraine headache prevention with noninvasive vagus nerve stimulation: the EVENT study. Neurology 87, 529–538 (2016).
Andreou, A. P. et al. Transcranial magnetic stimulation and potential cortical and trigeminothalamic mechanisms in migraine. Brain 139, 2002–2014 (2016).
Chen, S.-P. et al. Vagus nerve stimulation inhibits cortical spreading depression. Pain 157, 797–805 (2016).
Yarnitsky, D. et al. Nonpainful remote electrical stimulation alleviates episodic migraine pain. Neurology 88, 1250–1255 (2017).
Evers, S. et al. EFNS guideline on the drug treatment of migraine – revised report of an EFNS task force. Eur. J. Neurol. 16, 968–981 (2009).
Pringsheim, T. et al. Canadian Headache Society guideline for migraine prophylaxis. Can. J. Neurol. Sci. 39, S1–S59 (2012).
Silberstein, S. D. et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 78, 1337–1345 (2012).
Russell, F. A., King, R., Smillie, S.-J., Kodji, X. & Brain, S. D. Calcitonin gene-related peptide: physiology and pathophysiology. Physiol. Rev. 94, 1099–1142 (2014).
Forbes, R. B., McCarron, M. & Cardwell, C. R. Efficacy and contextual (placebo) effects of CGRP antibodies for migraine: systematic review and meta-analysis. Headache 60, 1542–1557 (2020).
Drellia, K., Kokoti, L., Deligianni, C. I., Papadopoulos, D. & Mitsikostas, D. D. Anti-CGRP monoclonal antibodies for migraine prevention: a systematic review and likelihood to help or harm analysis. Cephalalgia 41, 851–864 (2021).
Reuter, U. et al. Erenumab versus topiramate for the prevention of migraine – a randomised, double-blind, active-controlled phase 4 trial. SSRN Electron. J. https://doi.org/10.2139/ssrn.3791424 (2021).
Reuter, U. et al. Efficacy and tolerability of erenumab in patients with episodic migraine in whom two-to-four previous preventive treatments were unsuccessful: a randomised, double-blind, placebo-controlled, phase 3b study. Lancet 392, 2280–2287 (2018).
Ferrari, M. D. et al. Fremanezumab versus placebo for migraine prevention in patients with documented failure to up to four migraine preventive medication classes (FOCUS): a randomised, double-blind, placebo-controlled, phase 3b trial. Lancet 394, 1030–1040 (2019).
Mulleners, W. M. et al. Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol. 19, 814–825 (2020).
Goadsby, P. J. et al. Safety, tolerability, and efficacy of orally administered atogepant for the prevention of episodic migraine in adults: a double-blind, randomised phase 2b/3 trial. Lancet Neurol. 19, 727–737 (2020).
Croop, R. et al. Oral rimegepant for preventive treatment of migraine: a phase 2/3, randomised, double-blind, placebo-controlled trial. Lancet 397, 51–60 (2021).
MaassenVanDenBrink, A., Meijer, J., Villalón, C. M. & Ferrari, M. D. Wiping out CGRP: potential cardiovascular risks. Trends Pharmacol. Sci. 37, 779–788 (2016).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196 (2012).
Depre, C. et al. A randomized, double-blind, placebo-controlled study to evaluate the effect of erenumab on exercise time during a treadmill test in patients with stable angina. Headache 58, 715–723 (2018).
Ho, T. W. et al. Randomized, controlled study of telcagepant in patients with migraine and coronary artery disease. Headache 52, 224–235 (2012).
Maassen van den Brink, A., Rubio-Beltrán, E., Duncker, D. & Villalón, C. M. Is CGRP receptor blockade cardiovascularly safe? Appropriate studies are needed. Headache 58, 1257–1258 (2018).
Ashina, M. et al. Long-term tolerability and nonvascular safety of erenumab, a novel calcitonin gene-related peptide receptor antagonist for prevention of migraine: a pooled analysis of four placebo-controlled trials with long-term extensions. Cephalalgia 39, 1798–1808 (2019).
Holroyd, K. A. et al. Effect of preventive (β blocker) treatment, behavioural migraine management, or their combination on outcomes of optimised acute treatment in frequent migraine: randomised controlled trial. BMJ 341, c4871 (2010).
Carlsen, L. N. et al. Comparison of 3 treatment strategies for medication overuse headache: a randomized clinical trial. JAMA Neurol. 77, 1069–1078 (2020).
Evers, S. & Jensen, R. Treatment of medication overuse headache – guideline of the EFNS headache panel. Eur. J. Neurol. 18, 1115–1121 (2011).
Pijpers, J. A. et al. Acute withdrawal and botulinum toxin A in chronic migraine with medication overuse: a double-blind randomized controlled trial. Brain 142, 1203–1214 (2019).
Diener, H.-C. et al. Topiramate reduces headache days in chronic migraine: a randomized, double-blind, placebo-controlled study. Cephalalgia 27, 814–823 (2007).
Dodick, D. W. et al. OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache 50, 921–936 (2010).
Chiang, C.-C., Schwedt, T. J., Wang, S.-J. & Dodick, D. W. Treatment of medication-overuse headache: a systematic review. Cephalalgia 36, 371–386 (2015).
Charles, A. & Pozo-Rosich, P. Targeting calcitonin gene-related peptide: a new era in migraine therapy. Lancet 394, 1765–1774 (2019).
Ailani, J. et al. Positive response to galcanezumab following treatment failure to onabotulinumtoxinA in patients with migraine: post hoc analyses of three randomized double‐blind studies. Eur. J. Neurol. 27, 542–549 (2020).
Afridi, S. K., Giffin, N. J., Kaube, H. & Goadsby, P. J. A randomized controlled trial of intranasal ketamine in migraine with prolonged aura. Neurology 80, 642–647 (2013).
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
Linde, M. et al. The cost of headache disorders in Europe: the Eurolight project. Eur. J. Neurol. 19, 703–711 (2012).
Lancaster University Management School. Migraine costs EU economy €95bn per year (2019).
Burstein, R., Noseda, R. & Borsook, D. Migraine: multiple processes, complex pathophysiology. J. Neurosci. 35, 6619–6629 (2015).
Lauritzen, M. et al. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J. Cereb. Blood Flow. Metab. 31, 17–35 (2010).
Gupta, R. M. et al. A genetic variant associated with five vascular diseases is a distal regulator of endothelin-1 gene expression. Cell 170, 522–533.e15 (2017).
Tzourio, C. et al. Migraine and the risk of cervical artery dissection: a case-control study. Neurology 59, 435–437 (2002).
Rist, P. M., Diener, H.-C., Kurth, T. & Schürks, M. Migraine, migraine aura, and cervical artery dissection: a systematic review and meta-analysis. Cephalalgia 31, 886–896 (2011).
Tfelt-Hansen, P. C. & Tfelt-Hansen, J. Nitroglycerin headache and nitroglycerin-induced primary headaches from 1846 and onwards: a historical overview and an update. Headache 49, 445–456 (2009).
Kruuse, C., Thomsen, L. L., Birk, S. & Olesen, J. Migraine can be induced by sildenafil without changes in middle cerebral artery diameter. Brain 126, 241–247 (2003).
Asghar, M. S. et al. Evidence for a vascular factor in migraine. Ann. Neurol. 69, 635–645 (2011).
Amin, F. M. et al. Investigation of the pathophysiological mechanisms of migraine attacks induced by pituitary adenylate cyclase-activating polypeptide-38. Brain 137, 779–794 (2014).
Dickson, L., Aramori, I., McCulloch, J., Sharkey, J. & Finlayson, K. A systematic comparison of intracellular cyclic AMP and calcium signalling highlights complexities in human VPAC/PAC receptor pharmacology. Neuropharmacology 51, 1086–1098 (2006).
Guo, S., Olesen, J. & Ashina, M. Phosphodiesterase 3 inhibitor cilostazol induces migraine-like attacks via cyclic AMP increase. Brain 137, 2951–2959 (2014).
Al-Karagholi, M. A.-M., Hansen, J. M., Guo, S., Olesen, J. & Ashina, M. Opening of ATP-sensitive potassium channels causes migraine attacks: a new target for the treatment of migraine. Brain 142, 2644–2654 (2019).
Ashina, M. et al. Migraine: disease characterisation, biomarkers, and precision medicine. Lancet 397, 1496–1504 (2021).
Nieswand, V., Richter, M. & Gossrau, G. Epidemiology of headache in children and adolescents–another type of pandemia. Curr. Pain. Headache Rep. 24, 62 (2020).
Karsan, N., Prabhakar, P. & Goadsby, P. J. Characterising the premonitory stage of migraine in children: a clinic-based study of 100 patients in a specialist headache service. J. Headache Pain. 17, 94 (2016).
Gelfand, A. A., Reider, A. C. & Goadsby, P. J. Cranial autonomic symptoms in pediatric migraine are the rule, not the exception. Neurology 81, 431–436 (2013).
Gelfand, A. A. & Goadsby, P. J. Treatment of pediatric migraine in the emergency room. Pediatr. Neurol. 47, 233–241 (2012).
Gelfand, A. A. Pediatric and adolescent headache. Continuum 24, 1108–1136 (2018).
Gelfand, A. A., Thomas, K. C. & Goadsby, P. J. Before the headache: Infant colic as an early life expression of migraine. Neurology 79, 1392–1396 (2012).
Goadsby, P. J. in Oxford Textbook of Medicine 5th edn Ch. 24.8 (eds Warrell, D. A., Cox. T. M. & Firth, J. D.) (Oxford Univ. Press, 2018).
Author information
Authors and Affiliations
Contributions
Introduction (M.D.F., D.W.D. and P.J.G.); Epidemiology (T.K. and M.D.F.); Pathophysiology (C.A., M.A., R.B., A.C., P.J.G., M.D.F. and A.M.J.M.v.d.M.); Diagnosis, screening and prevention (D.W.D. and M.D.F.); Management (D.W.D., P.J.G. and M.D.F.); Quality of Life (T.K.); Outlook (A.C., P.J.G., D.W.D. and M.D.F.); Overview of the Primer (all authors).
Corresponding author
Ethics declarations
Competing interests
D.W.D. reports the following conflicts: consulting: AEON, Amgen, Clexio, Cerecin, Cooltech, Ctrl M, Allergan, Alder, Biohaven, GSK, Linpharma, Lundbeck, Promius, Eli Lilly, eNeura, Novartis, Impel, Satsuma, Theranica, WL Gore, Nocira, XoC, Zosano, Upjohn (Division of Pfizer), Pieris, Praxis, Revance, Equinox; honoraria: Clinical Care Solutions, CME Outfitters, Curry Rockefeller Group, DeepBench, Global Access Meetings, KLJ Associates, Academy for Continued Healthcare Learning, Majallin LLC, Medlogix Communications, MJH Lifesciences, Miller Medical Communications, Southern Headache Society (MAHEC), WebMD Health/Medscape, Wolters Kluwer, Oxford University Press, Cambridge University Press; research support: Department of Defense, National Institutes of Health, Henry Jackson Foundation, Sperling Foundation, American Migraine Foundation, Patient Centered Outcomes Research Institute (PCORI); stock options/shareholder/patents/boards of directors: Ctrl M (options), Aural Analytics (options), ExSano (options), Palion (options), Healint (options), Theranica (options), Second Opinion/Mobile Health (options), Epien (options/Board), Nocira (options), Matterhorn (shares/Board), Ontologics (shares/Board), King-Devick Technologies (options/Board), Precon Health (options/Board); patent 17189376.1-1466:v (title: Botulinum Toxin Dosage Regimen for Chronic Migraine Prophylaxis). M.A. is a consultant or scientific advisor for AbbVie, Allergan, Amgen, Eli Lilly, Lundbeck, Novartis and Teva; a primary investigator for ongoing Amgen, AbbVie/Allergan and Lundbeck trials; and has received grants from Lundbeck Foundation, Novo Nordisk Foundation and a research grant from Novartis. T.K. reports having contributed to an advisory board of CoLucid and a research project funded by Amgen, for which the Charité–Universitätsmedizin Berlin received an unrestricted compensation; he further reports having received honoraria from Lilly, Newsenselab, and Total for providing methodological advice, from Novartis and from Daiichi Sankyo for providing a lecture on neuroepidemiology and research methods, and from the BMJ for editorial services. P.J.G. reports, over the last 36 months, grants and personal fees from Amgen and Eli-Lilly and Company, a grant from Celgene, and personal fees from Alder Biopharmaceuticals, Aeon Biopharma, Allergan, Biohaven Pharmaceuticals Inc., Clexio, Electrocore LLC, eNeura, Epalex, GlaxoSmithKline, Impel Neuropharma, Lundbeck, MundiPharma, Novartis, Pfizer, Praxis, Sanofi, Santara Therapeutics, Satsuma, Teva Pharmaceuticals, Trigemina Inc., WL Gore, and personal fees for advice through Gerson Lehrman Group, and Guidepoint, fees for educational materials from Massachusetts Medical Society, Medery, Medlink, PrimeEd, UptoDate, WebMD, and publishing royalties from Oxford University Press, and Wolters Kluwer, and for medicolegal advice in headache, and a patent magnetic stimulation for headache (no. WO2016090333 A1) assigned to eNeura without fee. M.D.F. reports grants and consultancy or industry support from Electrocore, Medtronic, Eli Lilly, Amgen, Novartis, Satsuma, Lundbeck, and TEVA, and independent support from The Netherlands Organisation for Scientific Research (NWO), The Netherlands Organisation for Health Research and Development (ZonMW), The Dutch Brain Foundation, The Dutch Heart Foundation, The Dutch Ministry of Health, and The NutsOhra Foundation from the Dutch Insurance Companies. A.C. is a compensated consultant for Amgen, Biohaven, Eli Lilly, Lundbeck, and Satsuma; he is on the executive board of the American Headache Society. R.B. is the John Hedley-Whyte Professor of Anaesthesia and Neuroscience at the Beth Israel Deaconess Medical Center and Harvard Medical School; he has received research support from the NIH (R01 NS094198-01A1, R37 NS079678, R01NS095655, R01 NS104296, R21 NS106345), Allergan, Teva, Dr. Ready, Eli Lilly, Trigemina and the Migraine Research Foundation; he is a reviewer for NINDS; he holds stock options in AllayLamp, Theranica and Percept; he serves as consultant, advisory board member, or has received honoraria from: Alder, Allergan, Amgen, Autonomic Technologies, Avanir, Biohaven, Dr. Reddy’s Laboratory, electroCore, Eli Lilly, GlaxoSmithKline, Merck, Pernix, Theranica, Teva, and Trigemina; and has reveived CME fees from Healthlogix, Medlogix, WebMD/Medscape. A.M.J.M.v.d.M. reports grants and or industry support from Precision Medicine and Schedule 1 Therapeutics and independent support from The Netherlands Organisation for Scientific Research (NWO) and The Netherlands Organisation for Health Research and Development (ZonMW). C.A. declares no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks Hartmut Göbel, Andrew Hershey, Michel Lanteri-Minet, Cristina Tassorelli and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ferrari, M.D., Goadsby, P.J., Burstein, R. et al. Migraine. Nat Rev Dis Primers 8, 2 (2022). https://doi.org/10.1038/s41572-021-00328-4
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-021-00328-4
- Springer Nature Limited
This article is cited by
-
Postdromal symptoms in migraine: a REFORM study
The Journal of Headache and Pain (2024)
-
No causal association between allergic rhinitis and migraine: a Mendelian randomization study
European Journal of Medical Research (2024)
-
Microglia TREM1-mediated neuroinflammation contributes to central sensitization via the NF-κB pathway in a chronic migraine model
The Journal of Headache and Pain (2024)
-
Acute Treatment of Migraine: Expert Consensus Statements from the United Arab Emirates (UAE)
Neurology and Therapy (2024)
-
Migraine chronification as an allostatic disorder: a proof-of-concept study
Neurological Sciences (2024)