Abstract
The vulnerability of cancer cells to nutrient deprivation and their dependency on specific metabolites are emerging hallmarks of cancer. Fasting or fasting-mimicking diets (FMDs) lead to wide alterations in growth factors and in metabolite levels, generating environments that can reduce the capability of cancer cells to adapt and survive and thus improving the effects of cancer therapies. In addition, fasting or FMDs increase resistance to chemotherapy in normal but not cancer cells and promote regeneration in normal tissues, which could help prevent detrimental and potentially life-threatening side effects of treatments. While fasting is hardly tolerated by patients, both animal and clinical studies show that cycles of low-calorie FMDs are feasible and overall safe. Several clinical trials evaluating the effect of fasting or FMDs on treatment-emergent adverse events and on efficacy outcomes are ongoing. We propose that the combination of FMDs with chemotherapy, immunotherapy or other treatments represents a potentially promising strategy to increase treatment efficacy, prevent resistance acquisition and reduce side effects.



Similar content being viewed by others
References
Lanier, A. P., Bender, T. R., Blot, W. J., Fraumeni, J. F. Jr & Hurlburt, W. B. Cancer incidence in Alaska natives. Int. J. Cancer 18, 409–412 (1976).
Henderson, B. E. et al. Cancer incidence in the islands of the Pacific. Natl Cancer Inst. Monogr. 69, 73–81 (1985).
Ziegler, R. G. et al. Migration patterns and breast cancer risk in Asian-American women. J. Natl Cancer Inst. 85, 1819–1827 (1993).
Le, G. M., Gomez, S. L., Clarke, C. A., Glaser, S. L. & West, D. W. Cancer incidence patterns among Vietnamese in the United States and Ha Noi, Vietnam. Int. J. Cancer 102, 412–417 (2002).
Hemminki, K. & Li, X. Cancer risks in second-generation immigrants to Sweden. Int. J. Cancer 99, 229–237 (2002).
Kushi, L. H. et al. American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 62, 30–67 (2012).
Calle, E. E., Rodriguez, C., Walker-Thurmond, K. & Thun, M. J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U. S. adults. N. Engl. J. Med. 348, 1625–1638 (2003).
Emmons, K. M. & Colditz, G. A. Realizing the potential of cancer prevention - the role of implementation science. N. Engl. J. Med. 376, 986–990 (2017).
Kerr, J., Anderson, C. & Lippman, S. M. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 18, e457–e471 (2017).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Lee, C. et al. Fasting cycles retard growth of tumors and sensitize a range of cancer cell types to chemotherapy. Sci. Transl Med. 4, 124ra27 (2012).
Raffaghello, L. et al. Starvation-dependent differential stress resistance protects normal but not cancer cells against high-dose chemotherapy. Proc. Natl Acad. Sci. USA 105, 8215–8220 (2008).
Laviano, A. & Rossi Fanelli, F. Toxicity in chemotherapy—when less is more. N. Engl. J. Med. 366, 2319–2320 (2012).
DeVita, V. T. Jr, Eggermont, A. M., Hellman, S. & Kerr, D. J. Clinical cancer research: the past, present and the future. Nat. Rev. Clin. Oncol. 11, 663–669 (2014).
Jaffee, E. M. et al. Future cancer research priorities in the USA: a Lancet Oncology commission. Lancet Oncol. 18, e653–e706 (2017).
Cleeland, C. S. et al. Reducing the toxicity of cancer therapy: recognizing needs, taking action. Nat. Rev. Clin. Oncol. 9, 471–478 (2012).
Caffa, I. et al. Fasting potentiates the anticancer activity of tyrosine kinase inhibitors by strengthening MAPK signaling inhibition. Oncotarget 6, 11820–11832 (2015).
Arends, J. et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 36, 11–48 (2017).
Arends, J. et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin. Nutr. 36, 1187–1196 (2017).
Pelt, A. C. (ed.) Glucocorticoids: Effects, Action Mechanisms, and Therapeutic Uses (Nova Science Publishers, Inc. 2011).
Khurana, I. Essentials of Medical Physiology (ed. India, E.) (Elsevier, 2008).
Brandhorst, S. et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan. Cell Metab. 22, 86–99 (2015).
Brennan, A. M. & Mantzoros, C. S. Drug insight: the role of leptin in human physiology and pathophysiology—emerging clinical applications. Nat. Clin. Pract. Endocrinol. Metab. 2, 318–327 (2006).
Kubota, N. et al. Adiponectin stimulates AMP-activated protein kinase in the hypothalamus and increases food intake. Cell Metab. 6, 55–68 (2007).
Cheng, C. W. et al. Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cell-based regeneration and reverse immunosuppression. Cell Stem Cell 14, 810–823 (2014).
Di Biase, S. et al. Fasting regulates EGR1 and protects from glucose- and dexamethasone-dependent sensitization to chemotherapy. PLOS Biol. 15, e2001951 (2017).
Fabrizio, P. et al. SOD2 functions downstream of Sch9 to extend longevity in yeast. Genetics 163, 35–46 (2003).
Fabrizio, P., Pozza, F., Pletcher, S. D., Gendron, C. M. & Longo, V. D. Regulation of longevity and stress resistance by Sch9 in yeast. Science 292, 288–290 (2001).
Lee, C. et al. Reduced levels of IGF-I mediate differential protection of normal and cancer cells in response to fasting and improve chemotherapeutic index. Cancer Res. 70, 1564–1572 (2010).
Levine, M. E. et al. Low protein intake is associated with a major reduction in IGF-1, cancer, and overall mortality in the 65 and younger but not older population. Cell Metab. 19, 407–417 (2014).
Wei, M. et al. Life span extension by calorie restriction depends on Rim15 and transcription factors downstream of Ras/PKA, Tor, and Sch9. PLOS Genet. 4, e13 (2008).
van der Horst, A. & Burgering, B. M. Stressing the role of FoxO proteins in lifespan and disease. Nat. Rev. Mol. Cell Biol. 8, 440–450 (2007).
Cheng, Z. et al. Foxo1 integrates insulin signaling with mitochondrial function in the liver. Nat. Med. 15, 1307–1311 (2009).
Converso, D. P. et al. HO-1 is located in liver mitochondria and modulates mitochondrial heme content and metabolism. FASEB J. 20, 1236–1238 (2006).
Hurley, R. L. et al. Regulation of AMP-activated protein kinase by multisite phosphorylation in response to agents that elevate cellular cAMP. J. Biol. Chem. 281, 36662–36672 (2006).
Berasi, S. P. et al. Inhibition of gluconeogenesis through transcriptional activation of EGR1 and DUSP4 by AMP-activated kinase. J. Biol. Chem. 281, 27167–27177 (2006).
Chalkiadaki, A. & Guarente, L. The multifaceted functions of sirtuins in cancer. Nat. Rev. Cancer 15, 608–624 (2015).
Zhu, Y., Yan, Y., Gius, D. R. & Vassilopoulos, A. Metabolic regulation of Sirtuins upon fasting and the implication for cancer. Curr. Opin. Oncol. 25, 630–636 (2013).
Gao, Z. et al. Neurod1 is essential for the survival and maturation of adult-born neurons. Nat. Neurosci. 12, 1090–1092 (2009).
Olguin, H. C., Yang, Z., Tapscott, S. J. & Olwin, B. B. Reciprocal inhibition between Pax7 and muscle regulatory factors modulates myogenic cell fate determination. J. Cell Biol. 177, 769–779 (2007).
Cheng, C. W. et al. Fasting-mimicking diet promotes Ngn3-driven β-cell regeneration to reverse diabetes. Cell 168, 775–788.e12 (2017).
Galluzzi, L., Pietrocola, F., Levine, B. & Kroemer, G. Metabolic control of autophagy. Cell 159, 1263–1276 (2014).
Mizushima, N., Yamamoto, A., Matsui, M., Yoshimori, T. & Ohsumi, Y. In vivo analysis of autophagy in response to nutrient starvation using transgenic mice expressing a fluorescent autophagosome marker. Mol. Biol. Cell 15, 1101–1111 (2004).
Morselli, E. et al. Caloric restriction and resveratrol promote longevity through the Sirtuin-1-dependent induction of autophagy. Cell Death Dis. 1, e10 (2010).
Fernandez, A. F. et al. Disruption of the beclin 1-BCL2 autophagy regulatory complex promotes longevity in mice. Nature 558, 136–140 (2018).
Rybstein, M. D., Bravo-San Pedro, J. M., Kroemer, G. & Galluzzi, L. The autophagic network and cancer. Nat. Cell Biol. 20, 243–251 (2018).
Liang, X. H. et al. Induction of autophagy and inhibition of tumorigenesis by beclin 1. Nature 402, 672–676 (1999).
Yue, Z., Jin, S., Yang, C., Levine, A. J. & Heintz, N. Beclin 1, an autophagy gene essential for early embryonic development, is a haploinsufficient tumor suppressor. Proc. Natl Acad. Sci. USA 100, 15077–15082 (2003).
Yang, H. et al. Nutrient-sensitive mitochondrial NAD+ levels dictate cell survival. Cell 130, 1095–1107 (2007).
Bianchi, G. et al. Fasting induces anti-Warburg effect that increases respiration but reduces ATP-synthesis to promote apoptosis in colon cancer models. Oncotarget 6, 11806–11819 (2015).
Brandhorst, S., Wei, M., Hwang, S., Morgan, T. E. & Longo, V. D. Short-term calorie and protein restriction provide partial protection from chemotoxicity but do not delay glioma progression. Exp. Gerontol. 48, 1120–1128 (2013).
de Groot, S. et al. The effects of short-term fasting on tolerance to (neo) adjuvant chemotherapy in HER2-negative breast cancer patients: a randomized pilot study. BMC Cancer 15, 652 (2015).
Dorff, T. B. et al. Safety and feasibility of fasting in combination with platinum-based chemotherapy. BMC Cancer 16, 360 (2016).
Lo Re,O. et al. Fasting inhibits hepatic stellate cells activation and potentiates anti-cancer activity of Sorafenib in hepatocellular cancer cells. J. Cell. Physiol. 233, 1202–1212 (2018).
Lu, Z. et al. Fasting selectively blocks development of acute lymphoblastic leukemia via leptin-receptor upregulation. Nat. Med. 23, 79–90 (2017).
Pietrocola, F. et al. Caloric restriction mimetics enhance anticancer immunosurveillance. Cancer Cell 30, 147–160 (2016).
Safdie, F. et al. Fasting enhances the response of glioma to chemo- and radiotherapy. PLOS ONE 7, e44603 (2012).
Safdie, F. M. et al. Fasting and cancer treatment in humans: a case series report. Aging (Albany NY) 1, 988–1007 (2009).
Shi, Y. et al. Starvation-induced activation of ATM/Chk2/p53 signaling sensitizes cancer cells to cisplatin. BMC Cancer 12, 571 (2012).
Sun, P. et al. Fasting inhibits colorectal cancer growth by reducing M2 polarization of tumor-associated macrophages. Oncotarget 8, 74649–74660 (2017).
Bauersfeld, S. P. et al. The effects of short-term fasting on quality of life and tolerance to chemotherapy in patients with breast and ovarian cancer: a randomized cross-over pilot study. BMC Cancer 18, 476 (2018).
Wei, M. et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci. Transl Med. 9, eaai8700 (2017).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT01802346?term=NCT01802346&rank=1 (2013).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT01954836?term=NCT01954836&rank=1 (2013).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT02126449?term=NCT02126449&rank=1 (2014).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT02710721?term=NCT02710721&rank=1 (2016).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT03340935?term=NCT03340935&rank=1 (2017).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT03595540?term=NCT03595540&rank=1 (2018).
Martin, K., Jackson, C. F., Levy, R. G. & Cooper, P. N. Ketogenic diet and other dietary treatments for epilepsy. Cochrane Database Syst. Rev. 2, CD001903 (2016).
Oliveira, C. L. P. et al. A nutritional perspective of ketogenic diet in cancer: a narrative review. J. Acad. Nutr. Diet 118, 668–688 (2018).
Urbain, P. et al. Impact of a 6-week non-energy-restricted ketogenic diet on physical fitness, body composition and biochemical parameters in healthy adults. Nutr. Metab. (Lond.) 14, 17 (2017).
Hopkins, B. D. et al. Suppression of insulin feedback enhances the efficacy of PI3K inhibitors. Nature 560, 499–503 (2018).
Abdelwahab, M. G. et al. The ketogenic diet is an effective adjuvant to radiation therapy for the treatment of malignant glioma. PLOS ONE 7, e36197 (2012).
Allen, B. G. et al. Ketogenic diets enhance oxidative stress and radio-chemo-therapy responses in lung cancer xenografts. Clin. Cancer Res. 19, 3905–3913 (2013).
Aminzadeh-Gohari, S. et al. A ketogenic diet supplemented with medium-chain triglycerides enhances the anti-tumor and anti-angiogenic efficacy of chemotherapy on neuroblastoma xenografts in a CD1-nu mouse model. Oncotarget 8, 64728–64744 (2017).
Gluschnaider, U. et al. Long-chain fatty acid analogues suppress breast tumorigenesis and progression. Cancer Res. 74, 6991–7002 (2014).
Hao, G. W. et al. Growth of human colon cancer cells in nude mice is delayed by ketogenic diet with or without omega-3 fatty acids and medium-chain triglycerides. Asian Pac. J. Cancer Prev. 16, 2061–2068 (2015).
Klement, R. J., Champ, C. E., Otto, C. & Kammerer, U. Anti-tumor effects of ketogenic diets in mice: a meta-analysis. PLOS ONE 11, e0155050 (2016).
Lussier, D. M. et al. Enhanced immunity in a mouse model of malignant glioma is mediated by a therapeutic ketogenic diet. BMC Cancer 16, 310 (2016).
Mavropoulos, J. C. et al. The effects of varying dietary carbohydrate and fat content on survival in a murine LNCaP prostate cancer xenograft model. Cancer Prev. Res. (Phila) 2, 557–565 (2009).
Morscher, R. J. et al. Inhibition of neuroblastoma tumor growth by ketogenic diet and/or calorie restriction in a CD1-nu mouse model. PLOS ONE 10, e0129802 (2015).
Otto, C. et al. Growth of human gastric cancer cells in nude mice is delayed by a ketogenic diet supplemented with omega-3 fatty acids and medium-chain triglycerides. BMC Cancer 8, 122 (2008).
Rieger, J. et al. ERGO: a pilot study of ketogenic diet in recurrent glioblastoma. Int. J. Oncol. 44, 1843–1852 (2014).
Stemmer, K. et al. FGF21 is not required for glucose homeostasis, ketosis or tumour suppression associated with ketogenic diets in mice. Diabetologia 58, 2414–2423 (2015).
Tisdale, M. J., Brennan, R. A. & Fearon, K. C. Reduction of weight loss and tumour size in a cachexia model by a high fat diet. Br. J. Cancer 56, 39–43 (1987).
Woolf, E. C. et al. The ketogenic diet alters the hypoxic response and affects expression of proteins associated with angiogenesis, invasive potential and vascular permeability in a mouse glioma model. PLOS ONE 10, e0130357 (2015).
Liskiewicz, A. et al. Sciatic nerve regeneration in rats subjected to ketogenic diet. Nutr. Neurosci. 19, 116–124 (2016).
Linard, B., Ferrandon, A., Koning, E., Nehlig, A. & Raffo, E. Ketogenic diet exhibits neuroprotective effects in hippocampus but fails to prevent epileptogenesis in the lithium-pilocarpine model of mesial temporal lobe epilepsy in adult rats. Epilepsia 51, 1829–1836 (2010).
Berrigan, D., Perkins, S. N., Haines, D. C. & Hursting, S. D. Adult-onset calorie restriction and fasting delay spontaneous tumorigenesis in p53-deficient mice. Carcinogenesis 23, 817–822 (2002).
Chen, Y. et al. Effect of intermittent versus chronic calorie restriction on tumor incidence: a systematic review and meta-analysis of animal studies. Sci. Rep. 6, 33739 (2016).
Dirx, M. J., Zeegers, M. P., Dagnelie, P. C., van den Bogaard, T. & van den Brandt, P. A. Energy restriction and the risk of spontaneous mammary tumors in mice: a meta-analysis. Int. J. Cancer 106, 766–770 (2003).
Engelman, R. W., Day, N. K. & Good, R. A. Calorie intake during mammary development influences cancer risk: lasting inhibition of C3H/HeOu mammary tumorigenesis by peripubertal calorie restriction. Cancer Res. 54, 5724–5730 (1994).
Fernandes, G., Chandrasekar, B., Troyer, D. A., Venkatraman, J. T. & Good, R. A. Dietary lipids and calorie restriction affect mammary tumor incidence and gene expression in mouse mammary tumor virus/v-Ha-ras transgenic mice. Proc. Natl Acad. Sci. USA 92, 6494–6498 (1995).
Harvey, A. E. et al. Calorie restriction decreases murine and human pancreatic tumor cell growth, nuclear factor-kappaB activation, and inflammation-related gene expression in an insulin-like growth factor-1-dependent manner. PLOS ONE 9, e94151 (2014).
Huffman, D. M. et al. Cancer progression in the transgenic adenocarcinoma of mouse prostate mouse is related to energy balance, body mass, and body composition, but not food intake. Cancer Res. 67, 417–424 (2007).
Hursting, S. D., Dunlap, S. M., Ford, N. A., Hursting, M. J. & Lashinger, L. M. Calorie restriction and cancer prevention: a mechanistic perspective. Cancer Metab. 1, 10 (2013).
Hursting, S. D., Perkins, S. N., Brown, C. C., Haines, D. C. & Phang, J. M. Calorie restriction induces a p53-independent delay of spontaneous carcinogenesis in p53-deficient and wild-type mice. Cancer Res. 57, 2843–2846 (1997).
Hursting, S. D., Perkins, S. N. & Phang, J. M. Calorie restriction delays spontaneous tumorigenesis in p53-knockout transgenic mice. Proc. Natl Acad. Sci. USA 91, 7036–7040 (1994).
King, J. T., Casas, C. B. & Visscher, M. B. The influence of estrogen on cancer incidence and adrenal changes in ovariectomized mice on calorie restriction. Cancer Res. 9, 436 (1949).
Lashinger, L. M. et al. Starving cancer from the outside and inside: separate and combined effects of calorie restriction and autophagy inhibition on Ras-driven tumors. Cancer Metab. 4, 18 (2016).
Mai, V. et al. Calorie restriction and diet composition modulate spontaneous intestinal tumorigenesis in Apc(Min) mice through different mechanisms. Cancer Res. 63, 1752–1755 (2003).
Olivo-Marston, S. E. et al. Effects of calorie restriction and diet-induced obesity on murine colon carcinogenesis, growth and inflammatory factors, and microRNA expression. PLOS ONE 9, e94765 (2014).
Rogozina, O. P., Nkhata, K. J., Nagle, E. J., Grande, J. P. & Cleary, M. P. The protective effect of intermittent calorie restriction on mammary tumorigenesis is not compromised by consumption of a high fat diet during refeeding. Breast Cancer Res. Treat. 138, 395–406 (2013).
Rossi, E. L. et al. Energy balance modulation impacts epigenetic reprogramming, ERalpha and ERbeta expression, and mammary tumor development in MMTV-neu transgenic mice. Cancer Res. 77, 2500–2511 (2017).
Shang, Y. et al. Cancer prevention by adult-onset calorie restriction after infant exposure to ionizing radiation in B6C3F1 male mice. Int. J. Cancer 135, 1038–1047 (2014).
Yoshida, K., Inoue, T., Hirabayashi, Y., Nojima, K. & Sado, T. Calorie restriction and spontaneous hepatic tumors in C3H/He mice. J. Nutr. Health Aging 3, 121–126 (1999).
Yoshida, K., Inoue, T., Nojima, K., Hirabayashi, Y. & Sado, T. Calorie restriction reduces the incidence of myeloid leukemia induced by a single whole-body radiation in C3H/He mice. Proc. Natl Acad. Sci. USA 94, 2615–2619 (1997).
Colman, R. J. et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science 325, 201–204 (2009).
Mattison, J. A. et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature 489, 318–321 (2012).
Maddocks, O. D. et al. Serine starvation induces stress and p53-dependent metabolic remodelling in cancer cells. Nature 493, 542–546 (2013).
Sheen, J. H., Zoncu, R., Kim, D. & Sabatini, D. M. Defective regulation of autophagy upon leucine deprivation reveals a targetable liability of human melanoma cells in vitro and in vivo. Cancer Cell 19, 613–628 (2011).
Hens, J. R. et al. Methionine-restricted diet inhibits growth of MCF10AT1-derived mammary tumors by increasing cell cycle inhibitors in athymic nude mice. BMC Cancer 16, 349 (2016).
Fontana, L. & Partridge, L. Promoting health and longevity through diet: from model organisms to humans. Cell 161, 106–118 (2015).
Holloszy, J. O. & Fontana, L. Caloric restriction in humans. Exp. Gerontol. 42, 709–712 (2007).
Dirks, A. J. & Leeuwenburgh, C. Caloric restriction in humans: potential pitfalls and health concerns. Mech. Ageing Dev. 127, 1–7 (2006).
Das, S. K. et al. Body-composition changes in the Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy (CALERIE)-2 study: a 2-y randomized controlled trial of calorie restriction in nonobese humans. Am. J. Clin. Nutr. 105, 913–927 (2017).
Fontana, L., Weiss, E. P., Villareal, D. T., Klein, S. & Holloszy, J. O. Long-term effects of calorie or protein restriction on serum IGF-1 and IGFBP-3 concentration in humans. Aging Cell 7, 681–687 (2008).
Yilmaz, O. H. et al. mTORC1 in the Paneth cell niche couples intestinal stem-cell function to calorie intake. Nature 486, 490–495 (2012).
Yousefi, M. et al. Calorie restriction governs intestinal epithelial regeneration through cell-autonomous regulation of mTORC1 in reserve stem cells. Stem Cell Rep. 10, 703–711 (2018).
Jarde, T., Perrier, S., Vasson, M. P. & Caldefie-Chezet, F. Molecular mechanisms of leptin and adiponectin in breast cancer. Eur. J. Cancer 47, 33–43 (2011).
Pollak, M. The insulin and insulin-like growth factor receptor family in neoplasia: an update. Nat. Rev. Cancer 12, 159–169 (2012).
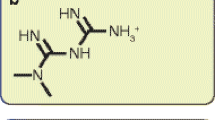
Newman, J. C. & Verdin, E. Ketone bodies as signaling metabolites. Trends Endocrinol. Metab. 25, 42–52 (2014).
Xia, S. et al. Prevention of dietary-fat-fueled ketogenesis attenuates BRAF V600E tumor growth. Cell Metab. 25, 358–373 (2017).
Di Biase, S. et al. Fasting-mimicking diet reduces HO-1 to promote T cell-mediated tumor cytotoxicity. Cancer Cell 30, 136–146 (2016).
Yakar, S. et al. Normal growth and development in the absence of hepatic insulin-like growth factor I. Proc. Natl Acad. Sci. USA 96, 7324–7329 (1999).
Lin, S. J. et al. Calorie restriction extends Saccharomyces cerevisiae lifespan by increasing respiration. Nature 418, 344–348 (2002).
Shim, H. S., Wei, M., Brandhorst, S. & Longo, V. D. Starvation promotes REV1 SUMOylation and p53-dependent sensitization of melanoma and breast cancer cells. Cancer Res. 75, 1056–1067 (2015).
D’Aronzo, M. et al. Fasting cycles potentiate the efficacy of gemcitabine treatment in in vitro and in vivo pancreatic cancer models. Oncotarget 6, 18545–18557 (2015).
Strickaert, A. et al. Cancer heterogeneity is not compatible with one unique cancer cell metabolic map. Oncogene 36, 2637–2642 (2017).
Chan, L. N. et al. Metabolic gatekeeper function of B-lymphoid transcription factors. Nature 542, 479–483 (2017).
Chen, G. G. et al. Heme oxygenase-1 protects against apoptosis induced by tumor necrosis factor-alpha and cycloheximide in papillary thyroid carcinoma cells. J. Cell. Biochem. 92, 1246–1256 (2004).
Postow, M. A., Callahan, M. K. & Wolchok, J. D. Immune checkpoint blockade in cancer therapy. J. Clin. Oncol. 33, 1974–1982 (2015).
Galluzzi, L., Buque, A., Kepp, O., Zitvogel, L. & Kroemer, G. Immunological effects of conventional chemotherapy and targeted anticancer agents. Cancer Cell 28, 690–714 (2015).
Stafford, P. et al. The ketogenic diet reverses gene expression patterns and reduces reactive oxygen species levels when used as an adjuvant therapy for glioma. Nutr. Metab. (Lond.) 7, 74 (2010).
Morscher, R. J. et al. Combination of metronomic cyclophosphamide and dietary intervention inhibits neuroblastoma growth in a CD1-nu mouse model. Oncotarget 7, 17060–17073 (2016).
Shields, B. A., Engelman, R. W., Fukaura, Y., Good, R. A. & Day, N. K. Calorie restriction suppresses subgenomic mink cytopathic focus-forming murine leukemia virus transcription and frequency of genomic expression while impairing lymphoma formation. Proc. Natl Acad. Sci. USA 88, 11138–11142 (1991).
Stewart, J. W. et al. Prevention of mouse skin tumor promotion by dietary energy restriction requires an intact adrenal gland and glucocorticoid supplementation restores inhibition. Carcinogenesis 26, 1077–1084 (2005).
Yoshida, K. et al. Radiation-induced myeloid leukemia in mice under calorie restriction. Leukemia 11 (Suppl. 3), 410–412 (1997).
Pugh, T. D., Oberley, T. D. & Weindruch, R. Dietary intervention at middle age: caloric restriction but not dehydroepiandrosterone sulfate increases lifespan and lifetime cancer incidence in mice. Cancer Res. 59, 1642–1648 (1999).
Al-Wahab, Z. et al. Dietary energy balance modulates ovarian cancer progression and metastasis. Oncotarget 5, 6063–6075 (2014).
Galet, C. et al. Effects of calorie restriction and IGF-1 receptor blockade on the progression of 22Rv1 prostate cancer xenografts. Int. J. Mol. Sci. 14, 13782–13795 (2013).
Fontana, L. & Klein, S. Aging, adiposity, and calorie restriction. JAMA 297, 986–994 (2007).
Paoli, A., Rubini, A., Volek, J. S. & Grimaldi, K. A. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur. J. Clin. Nutr. 67, 789–796 (2013).
Willcox, B. J. et al. Caloric restriction, the traditional Okinawan diet, and healthy aging: the diet of the world’s longest-lived people and its potential impact on morbidity and life span. Ann. NY Acad. Sci. 1114, 434–455 (2007).
Descamps, O., Riondel, J., Ducros, V. & Roussel, A. M. Mitochondrial production of reactive oxygen species and incidence of age-associated lymphoma in OF1 mice: effect of alternate-day fasting. Mech. Ageing Dev. 126, 1185–1191 (2005).
Arezzo di Trifiletti, A. et al. Comparison of the performance of four different tools in diagnosing disease-associated anorexia and their relationship with nutritional, functional and clinical outcome measures in hospitalized patients. Clin. Nutr. 32, 527–532 (2013).
Kilgour, R. D. et al. Handgrip strength predicts survival and is associated with markers of clinical and functional outcomes in advanced cancer patients. Support Care Cancer 21, 3261–3270 (2013).
Muscaritoli, M. et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin. Nutr. 29, 154–159 (2010).
Mourtzakis, M. et al. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl. Physiol. Nutr. Metab. 33, 997–1006 (2008).
Prado, C. M., Birdsell, L. A. & Baracos, V. E. The emerging role of computerized tomography in assessing cancer cachexia. Curr. Opin. Support. Palliat. Care 3, 269–275 (2009).
Laconi, E. et al. The enhancing effect of fasting/refeeding on the growth of nodules selectable by the resistant hepatocyte model in rat liver. Carcinogenesis 16, 1865–1869 (1995).
Premoselli, F., Sesca, E., Binasco, V., Caderni, G. & Tessitore, L. Fasting/re-feeding before initiation enhances the growth of aberrant crypt foci induced by azoxymethane in rat colon and rectum. Int. J. Cancer 77, 286–294 (1998).
Choi, I. Y. et al. A diet mimicking fasting promotes regeneration and reduces autoimmunity and multiple sclerosis symptoms. Cell Rep. 15, 2136–2146 (2016).
Acknowledgements
This work was supported in part by the Associazione Italiana per la Ricerca sul Cancro (AIRC) (IG#17736 to A.N. and IG#17605 to V.D.L.), the Seventh Framework Program ATHERO-B-CELL (#602114 to A.N.), the Fondazione Umberto Veronesi (to A.N. and V.D.L.), the Italian Ministry of Health (GR-2011-02347192 to A.N.), the 5 × 1000 2014 Funds to the Istituto di Ricovero e Cura a Carattere Scientifico per l’Oncologia (IRCCS) Ospedale Policlinico San Martino (to A.N.), the BC161452 and BC161452P1 grants of the Breast Cancer Research Program (US Department of Defense) (to V.D.L. and to A.N., respectively) and the US National Institute on Aging–National Institutes of Health (NIA–NIH) grants AG034906 and AG20642 (to V.D.L.).
Reviewer information
Nature Reviews Cancer thanks O. Yilmaz, C. C. Zhang and the anonymous reviewer for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
V.D.L. substantially contributed to discussion of content, wrote the manuscript and reviewed and/or edited it before submission. A.N. researched data for the manuscript, substantially contributed to discussion of content and wrote the manuscript. I.C. and S.C. researched data for the manuscript and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
A.N. and I.C. are inventors on three patents of methods for treating cancer by fasting-mimicking diets that are currently under negotiation with L-Nutra Inc. V.D.L. is the founder of L-Nutra Inc.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nencioni, A., Caffa, I., Cortellino, S. et al. Fasting and cancer: molecular mechanisms and clinical application. Nat Rev Cancer 18, 707–719 (2018). https://doi.org/10.1038/s41568-018-0061-0
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41568-018-0061-0
- Springer Nature Limited
This article is cited by
-
Exploring dietary changes and supplement use among cancer patients in Norway: prevalence, motivations, disclosure, information, and perceived risks and benefits: a cross sectional study
BMC Nutrition (2024)
-
Caloric restriction and metformin selectively improved LKB1-mutated NSCLC tumor response to chemo- and chemo-immunotherapy
Journal of Experimental & Clinical Cancer Research (2024)
-
Nanoparticles for inducing Gaucher disease-like damage in cancer cells
Nature Nanotechnology (2024)
-
Fasting-mimicking diet causes hepatic and blood markers changes indicating reduced biological age and disease risk
Nature Communications (2024)
-
Effects of dietary intervention on human diseases: molecular mechanisms and therapeutic potential
Signal Transduction and Targeted Therapy (2024)