Abstract
Cortical excitation-inhibition (E/I) imbalance is a potential model for the pathophysiology of schizophrenia. Previous research using transcranial magnetic stimulation (TMS) and electromyography (EMG) has suggested inhibitory deficits in schizophrenia. In this meta-analysis we assessed the reliability and clinical potential of TMS-EMG paradigms in schizophrenia following the methodological recommendations of the PRISMA guideline and the Cochrane Handbook. The search was conducted in three databases in November 2022. Included articles reported Short-Interval Intracortical Inhibition (SICI), Intracortical Facilitation (ICF), Long-Interval Intracortical Inhibition (LICI) and Cortical Silent Period (CSP) in patients with schizophrenia and healthy controls. Meta-analyses were conducted using a random-effects model. Subgroup analysis and meta-regressions were used to assess heterogeneity. Results of 36 studies revealed a robust inhibitory deficit in schizophrenia with a significant decrease in SICI (Cohen’s d: 0.62). A trend-level association was found between SICI and antipsychotic medication. Our findings support the E/I imbalance hypothesis in schizophrenia and suggest that SICI may be a potential pathophysiological characteristic of the disorder.
Similar content being viewed by others
Introduction
Schizophrenia is a highly complex and severe psychiatric disorder characterized by great diversity in symptom profile, risk factors, treatment response, and prognosis1. Schizophrenia has been associated with various genetic and developmental risk factors, molecular and circuit-level impairments, as well as altered neurotransmission, such as striatal dopaminergic dysregulation2. However, the exact pathophysiology and the causal association between neural mechanisms and the course of the disorder remain unclear.
Symptoms of schizophrenia are clustered into three main domains of positive, negative, and disorganized/cognitive symptoms, of which the positive dimension responds relatively well to available dopaminergic antipsychotic treatments2. However, medication has limited efficacy over the negative and cognitive symptoms, which have been highlighted as core features of disease vulnerability3. Therefore, further exploration of the latent neural factors underlying the symptoms is inevitable.
An increasing body of evidence supports the role of γ-amino butyric acid (GABA) and glutamate in the pathophysiology of schizophrenia4,5, highlighting a disrupted cortical excitation-inhibition (E/I) imbalance as a neurobiological characteristic of the disorder6. E/I imbalance refers to the relative disproportion in the excitatory and inhibitory signaling in the brain, which is necessary for efficient information processing within and between circuits7. E/I balance can be studied locally on the synaptic level as well as globally on a network level8. Understanding how E/I imbalance defines the symptoms of schizophrenia could open up a new avenue for novel treatment and diagnostic targets6.
Disrupted cortical E/I imbalance is supported by postmortem9, genetic10, and electrophysiological11 evidence; furthermore, there is emerging evidence from non-invasive brain stimulation studies using Transcranial Magnetic Stimulation12.
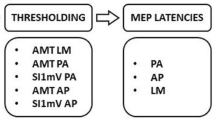
Transcranial magnetic stimulation (TMS) is a non-invasive brain stimulation method, which, combined with electromyography (EMG), can be used to assess motor cortical excitability in schizophrenia13. When a magnetic pulse (with an intensity reaching the threshold) is applied over the primary motor cortex, a motor-evoked potential (MEP) is elicited in the targeted contralateral peripheral muscle. The amplitude of the MEP can be recorded with EMG. Single- and paired-pulse TMS-EMG paradigms such as Short-Interval Intracortical Inhibition (SICI), Intracortical Facilitation (ICF), Long-Interval Intracortical Inhibition (LICI), and Cortical Silent Period (CSP) evoke excitatory and inhibitory MEP responses, allowing the neurophysiological probe of motor cortical excitability14.
Intracortical inhibition can be assessed using paired-pulse paradigms such as SICI and LICI and single-pulse paradigm CSP. SICI is a widely used standard method to elicit an inhibitory response. A subthreshold conditioning stimulus (CS) is followed by a suprathreshold test stimulus (TS) after a 1–4 ms interstimulus interval (ISI), resulting in a relative suppression of the second MEP amplitude15,16. Pharmacological studies indicate that SICI is mediated by cortical GABAA receptors, as GABAA agonists such as benzodiazepines enhance SICI17.
LICI is a less common inhibitory paired-pulse paradigm, where a suprathreshold CS and TS are delivered with a 100–200 ms ISI18. While SICI is mainly GABAA mediated, LICI is argued to be associated with GABAB receptors19,20.
CSP is elicited with a single suprathreshold TMS pulse while the individual maintains muscle contraction21. After the stimulation, the EMG activity is completely suppressed for a few hundred milliseconds. Although the early phase of CSP is thought to result from spinal inhibition, pharmacological evidence indicates that the later part of the silent period is mediated by GABAB receptors at the cortical level17.
Paired-pulse TMS paradigm ICF is a facilitatory response evoked by a similar technique to SICI. A subthreshold CS followed by a suprathreshold TS results in an increase in MEP amplitude when the two stimulations are given with a 10–25 ms ISI15. It has been suggested that ICF results from the combined mediation of GABAA and glutamatergic NMDA receptors, but the exact mechanism of intracortical facilitation is still unknown22,23.
Schizophrenia has been associated with impaired response in all of the aforementioned TMS-EMG paradigms, with deficits being particularly prominent in the inhibitory paradigms. Nevertheless, the results are inconsistent24,25. A previous meta-analysis by Radhu et al.26 confirmed a significant difference in SICI between schizophrenia patients and control group, however, the robustness of TMS-EMG paradigms in schizophrenia remains unclear. The aim of this meta-analysis is to fill this gap in the literature and examine the reliability and clinical potential of SICI, ICF, LICI and CSP in schizophrenia by providing a statistical summary of the results published in the literature. Additionally, we hypothesize that finding a disrupted inhibitory response in TMS-EMG paradigms could further support the importance of E/I imbalance as the pathophysiological mechanism behind schizophrenia.
To assess the reliability of TMS-EMG paradigms in schizophrenia we aim to study the association between excitability and antipsychotic medication, symptom severity, and illness duration.
Even though there are other TMS-EMG paradigms of cortical excitability (such as transcallosal inhibition or I-wave facilitation)27 here we focus on the four most widely used methods that have been associated with alterations in schizophrenia28. The aim of our study is to investigate the reliability of TMS-EMG paradigms in light of the E/I imbalance hypothesis in schizophrenia. Therefore, we did not focus on baseline resting motor threshold (RMT) or motor-evoked potential (MEP) amplitude, but rather on the inhibitory and excitatory responses.
Methods
The study protocol was predefined and registered on PROSPERO (CRD42022373330) and the meta-analysis was conducted following the recommendations of the Cochrane Handbook and reported according to the PRISMA 2020 guidelines.
Search and selection
Studies reporting TMS-EMG paradigms (SICI, CSP, ICF, and LICI) in schizophrenia-spectrum populations and healthy control groups were searched for. The systematic search was completed on the 5th of November 2022, using the following search engines: MEDLINE (via PubMed), Embase, and CENTRAL (The Cochrane Central Register of Controlled Trials). The search key used can be found in Supplementary Materials A.
Duplicate removal, title and abstract selection, and full-text selection were performed by two independent review authors (OL + DB and OL + BK, respectively), and disagreements were resolved by a third author (AS). Studies were included if they met the following eligibility criteria: (1) single- or paired-pulse TMS paradigms were applied in the primary motor cortex and the response was measured with EMG, (2) means and standard deviations for SICI, CSP, ICF, or LICI were reported for both patient and control groups, (3) all patients in the schizophrenia group met the DSM-IV or DSM-5 criteria for schizophrenia, schizoaffective disorder or first episode psychosis, (4) a detailed methodological description was provided with the calculation of the TMS-EMG outcome measures. Review articles, case reports, conference abstracts, and non-English language publications were excluded, as well as studies measuring TMS excitation with EEG.
Data synthesis
From the eligible articles, means and standard deviations of SICI, CSP, ICF, LICI, and resting motor threshold (RMT) were extracted, as well as group-level demographic data (sample size, age, sex) for both study populations. Diagnosis, PANSS scores, medication status (medicated/unmedicated), type of antipsychotic medication (atypical/typical or combination), CPZ-equivalent daily medication dose, and illness duration were extracted for the patient group. Most articles used a combined inclusion criteria for schizophrenia and schizoaffective disorder diagnoses therefore our pooled diagnostic categories are overlapping (Table 1). Interstimulus interval (ISI), stimulation intensity, type of TMS stimulator and coil, stimulation side, target muscle, and type of EMG electrode were collected for the TMS-EMG paradigms. Where available, data were also extracted separately for medicated and unmedicated patient groups. Where multiple ISI or intensity variations were available, or results for different medication groups were reported separately, total weighted averages were calculated for each article. Mean length of CSP was collected in milliseconds. The calculation of outcome measures for paired pulses varied across articles. SICI was reported, for example, as a ratio of [conditioned/unconditioned MEP] expressed raw number or percentage, as the reciprocal [unconditioned/conditioned MEP] or as the percentage of inhibition [1- conditioned/unconditioned MEP]. In this meta-analysis, all paired-pulse outcome measures are calculated as [conditioned/unconditioned MEP × 100] where SICI and LICI are ratios smaller than 100 whereas ICF is a ratio greater than 100. In our calculation, any number below 100 represents an inhibition, and smaller numbers represent increased inhibition. Numbers greater than 100 represent excitatory responses. Where results were reported differently, means were adjusted to match our calculation. WebPlotDigitizer29 was used for graphical data extraction. Data extraction was performed by OL and BK independently and disagreements were resolved by AS.
Statistical analysis
Data were analyzed with R (version 4.0.3)30 in RStudio31, using the meta32, metafor33, and dmetar34 packages. A random-effects model was applied to estimate the pooled mean difference with 95% confidence intervals. We anticipated variations in the true effect size across studies. To account for sampling error and such variances resulting from differences in experimental conditions, demographics and the heterogeneity of the patient population, we used a random-effects model. Between study variance of the true effect size was estimated with the Tau2 using the restricted maximum likelihood method (REML)35. The Hartung-Knapp adjustments36 were applied for the calculation of the confidence interval around the pooled effect size to compensate for small effect sizes reported in the articles. We used the I2 test to evaluate the amount of heterogeneity due to variability other than sampling error37. Forest plots were used to visualize mean differences and pooled effect sizes, and funnel plots were used to present publication bias.
In order to understand potential sources of heterogeneity, we first conducted exploratory analyses and assessed the distribution of data and evaluated the linear relationships between moderator variables such as demographics, disorder characteristics, experimental design and measurement details. When exploratory analyses revealed tendency-like associations (for example raw mean differences between medicated and unmedicated patients) or linear relationships (for example SICI of schizophrenia group and illness duration), we included all moderator variables in meta-regressions (metareg R function) and subgroup analyses.
Study risk of bias (ROB) assessment
Following the recommendations of the previous Cochrane Handbook on case-control studies, the Newcastle-Ottawa Scale (NOS)38 was used for risk of bias assessment. The checklist for TMS studies by Chipchase et al.39 was used to account for potential bias in the TMS methodology. The NOS was modified to include an additional point based on the outcome of the TMS score. Articles scoring above 70% on the TMS checklist were assigned an extra point in the NOS assessment, while those below 70% did not receive this adjustment. With the additional TMS score in the NOS, the scale ranged from 0–10. Without any published scoring guidelines, we used the following cutoff scores to determine ROB: 0–4 high risk, 5–7 moderate risk, and 8–10 low risk. ROB assessment was completed independently by two authors (OL and BK).
Results
Search and baseline characteristics
A total of 1715 case-control articles were identified by our search key and 80 reports were assessed for full-text selection. A final sample of 36 studies40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74 met the eligibility criteria and were included in the meta-analysis (flowchart of selection and reasons for exclusion in Supplementary Materials B).
The baseline characteristics of the included studies are presented in Table 1. Twenty-eight studies included SICI with 794 schizophrenia patients and 817 controls (mean age SCH = 32.25, min = 25.30, max = 38.5; mean age HC = 32.25, min = 20.93, max = 40.22). Eighteen studies reported SICI for medicated patients separately and 8 for unmedicated patients. Schizophrenia patients had a mean illness duration of 6.80 years (min = 0 in FEP, max = 16.40), a mean of 69.71 total PANSS score (min = 50.50, max = 92.40), and medicated patients were treated with a daily mean of 425.54 mg chlorpromazine (CPZ) equivalent antipsychotic dose (min = 283.97, max = 860.80).
Our second outcome measure, CSP was reported in 23 articles (total N control = 662, schizophrenia = 623), of which 17 reported data of medicated patients and 7 of unmedicated patients. The mean age of schizophrenia patients was 33.35 (min = 25.30, max = 42.60), and 31.81 for the control group (min = 20.93, max = 37.41). The patient population was characterized by an average of 7.07 years of illness duration (min = 0 in FEP, max = 18.30), a mean PANSS total of 71.76 (min = 50.50, max = 101) and a mean of 425.89 mg daily CPZ equivalent medication dose (min = 266.31, max = 860.80).
Twenty articles reported on ICF and only four articles reported on LICI, for descriptive statistics see the Supplementary Materials C.
Short-interval intracortical inhibition (SICI)
Results from the random-effects model revealed a robust (Cohen’s d: 0.62) and significant reduction in SICI in schizophrenia patients compared to healthy controls (Fig. 1). The pooled mean difference shows that the inhibitory response is 13.85% (95% CI: 9.19–18.51) smaller in schizophrenia. The results remained robust after sensitivity analysis (total mean difference after removing moderate to high ROB articles: 13.36%, 95% CI: 7.99–18.04). Between-study heterogeneity is moderate (I2 = 57%, p < 0.001), a part of which can be explained by moderate to high ROB (heterogeneity of the sensitivity analysis: I2 = 50%, p = 0.01). In addition to ROB75, experimental conditions such as the evaluation of task-related SICI41 and cannabis use55 could account for cases where SICI was found to be higher in schizophrenia.
Multiple subgroup analyses were conducted to further elucidate potential sources of heterogeneity and investigate the association between SICI and medication status. Exploratory analyses revealed a tendency-like association between SICI and medication status as well as SICI and CPZ equivalent antipsychotic dose (see Fig. 2D). Based on further exploratory analysis, the effect of medication status seems to be more defined than the effect of medication dose (Supplementary Materials D). However, subgroup analysis did not confirm that there is a difference in the extent to which medicated (N = 375) and unmedicated (N = 142) schizophrenia patients differ from the healthy population (Fig. 2E). Meta-regressions conducted with covariates such as symptom severity (PANSS total, positive, negative and general scores), illness duration, age and sex did not reveal a significant effect on the pooled effect size (Supplementary Material D). Exploratory analysis revealed a tendency-like association between the proportion of females and SICI, suggesting that inhibitory response was greater in samples with more males than females.
A Forest plot for SICI between unmedicated schizophrenia patients (SCH) and healthy control group (HC). B Forest plot for SICI between medicated SCH patients and HC. C, D Exploratory analysis of medication status and mean CPZ equivalent medication dose of SICI. E Summary of total effect sizes for subgroup analysis of SICI between medicated and unmedicated SCH and HC.
Additionally, subgroup analysis did not show any variance of SICI across different TMS conditions (stimulation side, device, target muscle, interstimulus interval), diagnoses or date of publication.
Cortical silent period (CSP)
Results for CSP did not show any difference between schizophrenia patients and control group (Fig. 3). The pooled effect size showed high heterogeneity between studies (I2 = 89%, p < 0.001) and a wide confidence interval around the pooled total effect size (6.69, CI: −6.16–19.54). Furthermore, the large inconsistency between published results is reflected in the range of CSP within the control group (83.6–195.7 ms), which could be the result of biological variability or measurement bias.
A Results of the random-effect meta-analysis showing the mean difference of CSP between schizophrenia patients (SCH) and healthy control groups (HC). CSP is measured in milliseconds, length of CSP is proportional to the extent of inhibition. Articles from 0 to left found shorter CSP in SCH whereas articles from 0 to right reported longer CSP in SCH. B Forest plot of CSP between unmedicated SCH patients and H. C Forest plot of CSP between medicated SCH patients and HC.
Subgroup analyses and meta-regressions of experimental conditions, demographic variables, and medical variables failed to identify any single moderator variable that could account for the variance found between studies. Nevertheless, a tendency-like association was found between medication status and CSP. Unmedicated patients exhibited a slightly shorter CSP (reduced inhibition), whereas medicated patients showed a slightly longer CSP compared to the control group (Fig. 3). However, these results are not significant and are highly heterogeneous.
Intracortical facilitation (ICF), long-interval intracortical inhibition (LICI), and resting motor threshold (RMT)
We found no clear difference between schizophrenia patients and control groups in terms of excitatory response ICF or the inhibitory response LICI (Fig. 4). Results of ICF are reliable, the relatively big sample size (SCH = 532, HC = 498) and the low between-study heterogeneity (I2 = 37%, p = 0.005) confirm that there is no clear difference between the two groups. Sensitivity analysis (excluding moderate to high ROB articles) did not improve or change the overall results of ICF (total mean difference = 0.45, 95% CI: −12.66–13.56). Subgroup analyses and meta-regressions (depending on the class of variables) did not account for heterogeneity in experimental conditions, medical conditions, demographic variables, or time of publication.
A Forest plot of ICF. Articles to the left of zero indicate decreased ICF in schizophrenia (SCH) while those to the right show increased ICF in SCH. No significant difference was found between the two groups. B Forest plot of LICI. Articles from zero to left reported increased inhibition in SCH whereas articles from zero to right found decreased inhibition in SCH. No significant difference was observed between the two groups, and a conclusion cannot be drawn from these results due to the small number of included articles.
Due to the small number of articles included (N = 4) and the relatively small pooled sample size (SCH = 170, HC = 201), the results of LICI are not sufficient to draw conclusions from.
A powerful analysis of RMT (Supplementary Materials E), which included 33 studies and an impressive sample size (SCH = 902, HC = 932), did not reveal any group differences in baseline excitability. A sensitivity analysis based on ROB did not change the overall effect (total mean difference = 1.69, 95% CI: −0.37–3.75).
Risk of bias, publication bias, and heterogeneity
Of the 36 articles included, 2 articles had a combined high risk of bias on the NOS and the TMS checklists, 13 had moderate risk and 21 articles received a low risk of bias score (results available online at https://osf.io/8cef3/). Funnel plots and Egger’s test were used to assess publication bias across the included studies. The funnel plots (Supplementary Materials F) revealed relative symmetry for all TMS-EMG paradigms except CSP, which raised some concerns about potential publication bias. No significant publication bias was detected with the Egger’s test (Supplementary Materials G).
Discussion
In this meta-analysis, we statistically pool data from 36 articles investigating cortical excitability with single- and paired-pulse TMS-EMG paradigms. The aim of our research was to find evidence for the disrupted E/I balance in schizophrenia and to determine the reliability and predictive value of TMS-EMG paradigms in schizophrenia.
To our knowledge, this is the first meta-analysis to statistically confirm the widely reported reduction in SICI in medicated and unmedicated schizophrenia patients. Our results confirmed the hypothesized difference between schizophrenia patients and healthy controls with a relatively large pooled sample (SCH = 794, HC = 817) and moderate to large effect size (Cohen’s d = 0.62). The pooled mean difference shows a 13.85% (95% CI = 9.19–18.51) between-group difference in the inhibitory response (Fig. 1), suggesting that intracortical inhibitory deficit in schizophrenia is indeed clinically relevant. Results for SICI remained unchanged after sensitivity analysis, confirming that the effect is stable. Furthermore, we only found three articles that contradicted our results41,55,70, and there are potential methodological explanations in all three cases (task-related SICI as opposed to resting state, cannabis use, and high risk of bias).
Although previous research suggested that SICI could be associated with antipsychotic medication45 and symptom severity46, our study was underpowered to confirm these results with subgroup analysis or meta-regression (Supplementary Material D). Nevertheless, exploratory analysis revealed a trend-level association between SICI and medication status as well as medication dose, suggesting that unmedicated patients might exhibit reduced SICI. Based on our exploratory analyses on medication dose, we propose that medication status itself rather than antipsychotic dose could be driving the effect. However, further research is needed to better understand these associations and how the different antipsychotic agents affect SICI.
There are several possible explanations for these ambiguous results on the effect of antipsychotics. First, we had a relatively small number of studies including unmedicated schizophrenia patients (N = 8), with a small pooled sample size (N = 142). Second, the patient population of the studies including unmedicated patients was small (N of patients: mean = 17.75, range: 6–43), and inclusion criteria varied across studies. Some studies included antipsychotic-naive patients50, whereas others included patients who had not been receiving antipsychotic treatment for the past 3 months51. The patient populations also differed in whether they received benzodiazepines, which has been confirmed to increase SICI24. Regrettably, data on benzodiazepine intake was not reported in the included articles therefore we were unable to control for its confounding effect. Lastly, medicated patients were treated with various types and combinations of antipsychotics with different receptor binding profiles76. We were only able to extract data and assess the moderator effect of clozapine directly, however, due to the small number of articles (N = 3) and the small sample size (N = 58), no conclusions could be drawn on its effect. Due to these limitations, our study lacked the statistical power to provide significant evidence on the impact of antipsychotic medication on SICI. Nevertheless, the notable correlation observed at a trend level between medication status, medication dose and SICI (Fig. 2C, D) suggests that antipsychotic medication could play an important role in reducing the magnitude of the SICI inhibitory deficit. This question should be targeted in future research to confirm the effect of medication on SICI.
The reliability of SICI is also supported by the fact that diversity in TMS conditions and experimental designs did not change the overall effect of SICI. Articles included in the present study applied a variety of experimental designs and TMS conditions (Table 1), with significant differences in stimulation intensity, used device, coil type, target muscle, direction of induced current, or pulse shape. The technical specifications within the TMS protocol may impact the evoked response75,77, nevertheless, adjusting for variations in experimental setup through subgroup analysis and meta-regression did not alter the overall effect.
Our results of SICI are in line with the previous meta-analysis published in 2013 by Radhu et al.26, further supporting the reliability of SICI in schizophrenia.
In contrast to SICI, our results showed no clear difference in CSP, ICF, or LICI between schizophrenia patients and healthy controls. This implies that the dysfunction in motor cortical excitability in schizophrenia may be specific to GABAA receptors involved in SICI17.
Limitations and heterogeneity
This study has several limitations that should be considered. Firstly, the number of studies included in the LICI analysis was too small, completely limiting the conclusions that can be drawn from this analysis. Secondly, there is high heterogeneity in the case of ICF and CSP, which has to be considered when interpreting the findings.
The high degree of heterogeneity found in CSP is in line with the meta-analysis by Miyazawa et al.78. We hypothesize that this heterogeneity might be due to several factors, including differences in TMS-EMG protocols (e.g., intensity, muscle contraction, pulse shape, determining the end of CSP)14, biological variability79, and the reporting of results with small sample sizes (SCH range: 9–81, HC range: 9–125) without accounting for the skewness of the data. Consequently, we suggest that future research should take such methodological considerations into account and report the distribution of the data when using the mean as an outcome.
There is considerably less heterogeneity underlying ICF. Our study was underpowered to account for this heterogeneity by testing the effect of clinical and methodological confounding factors.
The high heterogeneity observed in ICF and CSP may be due to confounding factors that we were not able to control for due to the small number of studies included when conducting a subgroup-analysis or meta-regression.
Therefore, the potential impact of clinical and methodological confounding variables should be further explored in future studies for all TMS-EMG paradigms. Larger samples are needed and the technical factors of TMS-EMG paradigms (such as stimulation intensity, pulse shape, ISI, direction of induced current, etc.) should be evaluated with more methodological rigor.
Moreover, there is a need for additional research on the impact of clinical variables (including diagnosis, medication type and dosage, and symptom severity) and demographic variables (such as age and sex) that were beyond our study’s capacity to thoroughly investigate.
Clinical and methodological implications
The results of the present meta-analysis have several clinical and methodological implications. Our results of SICI are in line with the gabaergic hypothesis of schizophrenia, and contribute to the growing evidence supporting the E/I imbalance in schizophrenia80,81. The E/I hypothesis is a promising model to link the neurodevelopmental and the dopaminergic hypotheses of schizophrenia. Understanding the role of E/I imbalance in the pathomechanism of schizophrenia could offer novel approaches for developing treatment targets within the GABA system to improve the cognitive and negative symptom domains of schizophrenia6.
Our results confirm that SICI is a reliable and robust TMS-EMG protocol showing a clear inhibitory deficit in schizophrenia regardless of experimental conditions and demographic variables. Therefore, our results raise the possibility that SICI, in combination with other reliable markers, may contribute to supporting current clinical diagnosis with physiological data. The diagnostic utility of TMS-EMG paradigms in the field of neurology is well established82, therefore we believe the results of this meta-analysis provide a foundation for future clinical research and confirm that the inhibitory deficits of SICI are robust enough to have a clinical potential.
The scope of this study limited us to assess the specificity and sensitivity of SICI in schizophrenia, therefore we argue that future research should further investigate the potential moderating factors of SICI in order to validate its clinical relevance and evaluate its diagnostic properties. Previous research comparing other psychiatric disorders such as OCD or depression to schizophrenia have found different patterns of excitability deficits in each disorder26,65, however, the specificity of SICI in schizophrenia have not been studied yet.
SICI might also have the potential to be investigated as a target for response prediction of pharmacological agents or neuromodulation. Non-invasive therapeutic brain stimulation techniques such as repetitive TMS (rTMS) or transcranial direct current stimulation (tDCS) have been shown to change the excitability of the stimulated circuits83, and studies confirm this by showing alterations in TMS-EMG paradigms in response to rTMS or tDCS51,54,58,61. In addition to response prediction, SICI may be further investigated as a measure of individual brain state to support the timing of state-dependent or closed-loop brain stimulation84,85.
Here we suggest that future studies should focus on investigating the diagnostic and prognostic value of SICI in larger patient samples and explore its potential use as a supportive biomarker or a marker for therapeutic response prediction. Future research should also further investigate the role of antipsychotic medication and its potential impact on SICI in schizophrenia.
Our results of CSP, ICF, and LICI have limited clinical relevance due to the high degree of heterogeneity and the smaller number of included studies.
In order to reduce heterogeneity and confounding due to methodological differences in the TMS-EMG paradigms, we suggest that future clinical research should consider some methodological aspects. First, we encourage the use of quality checklists (such as the one by Chipchase et al.39) to promote standardized reporting of results. In addition, to avoid misinterpretation, we believe that it is also of great importance to be consistent with the language used when referring to paired-pulse paradigms and to clearly state whether SICI or LICI refers to the amount of inhibition or to the ratio number calculated from the conditioned and unconditioned MEP amplitude.
TMS-EMG is a well-established tool to probe cortical excitability which fits well with other electrophysiological methods that have been suggested to be a marker of E/I imbalance12. For a better understanding of the E/I imbalance and the clinical potential of SICI, it would be worthwhile in the future to compare TMS-EMG paradigms to other electrophysiological methods such as EEG gamma-band power86, spectral slope87, event-related potentials88 or TMS-EEG89.
Conclusion
This meta-analysis provides evidence for a significant decrease in SICI in schizophrenia patients, supporting the hypothesis that gabaergic inhibitory dysfunctions play an important role in the pathophysiology of the disorder. Here we argue that the E/I imbalance is a robust physiological characteristic of the disorder which can be assessed with SICI. Our results suggest that SICI is a promising candidate as one of the potential physiological characteristics that could complement the observational diagnosis of schizophrenia with physiological data or serve as a marker for therapeutic response prediction.
Data availability
We have made all data for this meta-analysis publicly available. The data extraction table, the results of the risk of bias assessment and the R code for the statistical analysis can be found online in the OSF repository: https://osf.io/8cef3/.
References
van Os, J. & Kapur, S. Schizophrenia. Lancet 374, 635–645 (2009).
McCutcheon, R. A., Reis Marques, T. & Howes, O. D. Schizophrenia—an overview. JAMA Psychiatry 77, 201–210 (2020).
Gold, J. M. Cognitive deficits as treatment targets in schizophrenia. Schizophr. Res. 72, 21–28 (2004).
Coyle, J. T. Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell. Mol. Neurobiol. 26, 365–384 (2006).
Egerton, A., Modinos, G., Ferrera, D. & McGuire, P. Neuroimaging studies of GABA in schizophrenia: a systematic review with meta-analysis. Transl. Psychiatry 7, e1147 (2017).
Howes, O. D. & Shatalina, E. Integrating the neurodevelopmental and dopamine hypotheses of schizophrenia and the role of cortical excitation-inhibition balance. Biol. Psychiatry 92, 501–513 (2022).
Anticevic, A. & Lisman, J. How can global alteration of excitation/inhibition balance lead to the local dysfunctions that underlie schizophrenia? Biol. Psychiatry 81, 818–820 (2017).
Froemke, R. C. Plasticity of cortical excitatory-inhibitory balance. Annu. Rev. Neurosci. 38, 195–219 (2015).
Lewis, D. A., Curley, A. A., Glausier, J. R. & Volk, D. W. Cortical parvalbumin interneurons and cognitive dysfunction in schizophrenia. Trends Neurosci. 35, 57–67 (2012).
Pocklington, A. J. et al. Novel findings from CNVs implicate inhibitory and excitatory signaling complexes in schizophrenia. Neuron 86, 1203–1214 (2015).
Uhlhaas, P. J. & Singer, W. Abnormal neural oscillations and synchrony in schizophrenia. Nat. Rev. Neurosci. 11, 100–113 (2010).
Rogasch, N. C., Daskalakis, Z. J. & Fitzgerald, P. B. Cortical inhibition, excitation, and connectivity in schizophrenia: a review of insights from transcranial magnetic stimulation. Schizophr. Bull. 40, 685–696 (2014).
McClintock, S. M., Freitas, C., Oberman, L., Lisanby, S. H. & Pascual-Leone, A. Transcranial magnetic stimulation: a neuroscientific probe of cortical function in schizophrenia. Biol. Psychiatry 70, 19–27 (2011).
Reis, J. et al. Contribution of transcranial magnetic stimulation to the understanding of cortical mechanisms involved in motor control. J. Physiol. 586, 325–351 (2008).
Di Lazzaro, V. et al. Magnetic transcranial stimulation at intensities below active motor threshold activates intracortical inhibitory circuits. Exp. Brain Res. 119, 265–268 (1998).
Kujirai, T. et al. Corticocortical inhibition in human motor cortex. J. Physiol. 471, 501–519 (1993).
Ziemann, U. Pharmacology of TMS measures. in The Oxford Handbook of Transcranial Stimulation (eds Wassermann, E. M. et al.) (Oxford University Press, 2021).
Valls-Solé, J., Pascual-Leone, A., Wassermann, E. M. & Hallett, M. Human motor evoked responses to paired transcranial magnetic stimuli. Electroencephalogr. Clin. Neurophysiol. 85, 355–364 (1992).
McDonnell, M. N., Orekhov, Y. & Ziemann, U. The role of GABA(B) receptors in intracortical inhibition in the human motor cortex. Exp. Brain Res. 173, 86–93 (2006).
Werhahn, K. J., Kunesch, E., Noachtar, S., Benecke, R. & Classen, J. Differential effects on motorcortical inhibition induced by blockade of GABA uptake in humans. J. Physiol. 517, 591–597 (1999).
Fuhr, P., Agostino, R. & Hallett, M. Spinal motor neuron excitability during the silent period after cortical stimulation. Electroencephalogr. Clin. Neurophysiol. 81, 257–262 (1991).
Ziemann, U., Chen, R., Cohen, L. G. & Hallett, M. Dextromethorphan decreases the excitability of the human motor cortex. Neurology 51, 1320–1324 (1998).
Di Lazzaro, V. et al. Origin of facilitation of motor-evoked potentials after paired magnetic stimulation: direct recording of epidural activity in conscious humans. J. Neurophysiol. 96, 1765–1771 (2006).
di Hou, M., Santoro, V., Biondi, A., Shergill, S. S. & Premoli, I. A systematic review of TMS and neurophysiological biometrics in patients with schizophrenia. J. Psychiatry Neurosci. 46, E675–E701 (2021).
Kaskie, R. E. & Ferrarelli, F. Investigating the neurobiology of schizophrenia and other major psychiatric disorders with transcranial magnetic stimulation. Schizophr. Res. 192, 30–38 (2018).
Radhu, N. et al. A meta-analysis of cortical inhibition and excitability using transcranial magnetic stimulation in psychiatric disorders. Clin. Neurophysiol. 124, 1309–1320 (2013).
Bunse, T. et al. Motor cortical excitability assessed by transcranial magnetic stimulation in psychiatric disorders: a systematic review. Brain Stimul. 7, 158–169 (2014).
Kim, H. K., Blumberger, D. M. & Daskalakis, Z. J. Neurophysiological biomarkers in schizophrenia-P50, mismatch negativity, and TMS-EMG and TMS-EEG. Front. Psychiatry 11, 795 (2020).
Rohatgi, A. WebPlotDigitizer. (2022).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2022).
RStudio Team. RStudio: Integrated Development for R (RStudio, Inc., 2015).
Balduzzi, S., Rücker, G. & Schwarzer, G. How to perform a meta-analysis with R: a practical tutorial. Evid. Based Ment. Health 22, 153–160 (2019).
Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 36, 1–48 (2010).
Harrer, M., Cuijpers, P., Furukawa, T. & Ebert, D. D. dmetar: Companion R Package For The Guide ‘Doing Meta-Analysis in R’. (2019).
Viechtbauer, W. Bias and efficiency of meta-analytic variance estimators in the random-effects model. J. Educ. Behav. Stat. 30, 261–293 (2005).
Knapp, G. & Hartung, J. Improved tests for a random effects meta-regression with a single covariate. Stat. Med. 22, 2693–2710 (2003).
Higgins, J. P. T. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Peterson, J., Welch, V., Losos, M. & Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. Ottawa Hospital Research Institute. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [cited 2024 June 1].
Chipchase, L. et al. A checklist for assessing the methodological quality of studies using transcranial magnetic stimulation to study the motor system: an international consensus study. Clin. Neurophysiol. 123, 1698–1704 (2012).
Ahlgrén-Rimpiläinen, A., Lauerma, H., Kähkönen, S. & Rimpiläinen, I. Disrupted central inhibition after transcranial magnetic stimulation of motor cortex in schizophrenia with long-term antipsychotic treatment. ISRN Psychiatry 2013, 876171 (2013).
Bagewadi, V. I. et al. Diminished modulation of motor cortical reactivity during context-based action observation in schizophrenia. Schizophr. Res. 204, 222–229 (2019).
Bajbouj, M. et al. Abnormalities of inhibitory neuronal mechanisms in the motor cortex of patients with schizophrenia. Pharmacopsychiatry 37, 74–80 (2004).
Bridgman, A. C. et al. Deficits in GABAA receptor function and working memory in non-smokers with schizophrenia. Schizophr. Res. 171, 125–130 (2016).
Carment, L. et al. Neural noise and cortical inhibition in schizophrenia. Brain Stimul. 13, 1298–1304 (2020).
Daskalakis, Z. J. et al. Evidence for impaired cortical inhibition in schizophrenia using transcranial magnetic stimulation. Arch. Gen. Psychiatry 59, 347–354 (2002).
Daskalakis, Z. J. et al. Increased cortical inhibition in persons with schizophrenia treated with clozapine. J. Psychopharmacol. 22, 203–209 (2008).
Du, X. et al. The role of white matter microstructure in inhibitory deficits in patients with schizophrenia. Brain Stimul. 10, 283–290 (2017).
Du, X. & Hong, E. Aberrant prefronto-motor cortex connectivity explains inhibitory deficits in the motor cortex of patient with schizophrenia. Biol. Psychiatry 83, S324–S325 (2018).
Du, X. & Hong, L. E. Test-retest reliability of short-interval intracortical inhibition and intracortical facilitation in patients with schizophrenia. Psychiatry Res. 267, 575–581 (2018).
Eichhammer, P. et al. Cortical excitability in neuroleptic-naive first-episode schizophrenic patients. Schizophr. Res. 67, 253–259 (2004).
Fitzgerald, P. B. et al. Reduced plastic brain responses in schizophrenia: a transcranial magnetic stimulation study. Schizophr. Res. 71, 17–26 (2004).
Fitzgerald, P. B. et al. A transcranial magnetic stimulation study of abnormal cortical inhibition in schizophrenia. Psychiatry Res. 118, 197–207 (2003).
Fitzgerald, P. B., Brown, T. L., Daskalakis, Z. J. & Kulkarni, J. A transcranial magnetic stimulation study of inhibitory deficits in the motor cortex in patients with schizophrenia. Psychiatry Res. Neuroimaging 114, 11–22 (2002).
Frank, E. et al. Antipsychotic treatment with quetiapine increases the cortical silent period. Schizophr. Res. 156, 128–132 (2014).
Goodman, M. S. et al. Differential effects of cannabis dependence on cortical inhibition in patients with schizophrenia and non-psychiatric controls. Brain Stimul. 10, 275–282 (2017).
Hare, S. M. et al. Mapping local and long-distance resting connectivity markers of TMS-related inhibition reduction in schizophrenia. NeuroImage Clin. 31, 102688 (2021).
Hasan, A. et al. A similar but distinctive pattern of impaired cortical excitability in first-episode schizophrenia and ADHD. Neuropsychobiology 67, 74–83 (2013).
Hasan, A. et al. Impairments of motor-cortex responses to unilateral and bilateral direct current stimulation in schizophrenia. Front. Psychiatry 4, 121 (2013).
Hasan, A. et al. Impaired long-term depression in schizophrenia: a cathodal tDCS pilot study. Brain Stimul. 5, 475–483 (2012).
Hasan, A. et al. Deficient inhibitory cortical networks in antipsychotic-naive subjects at risk of developing first-episode psychosis and first-episode schizophrenia patients: a cross-sectional study. Biol. Psychiatry 72, 744–751 (2012).
Kaster, T. S. et al. Clozapine potentiation of GABA mediated cortical inhibition in treatment resistant schizophrenia. Schizophr. Res. 165, 157–162 (2015).
Lindberg, P. G. et al. Altered cortical processing of motor inhibition in schizophrenia. Cortex 85, 1–12 (2016).
Liu, S.-K., Fitzgerald, P. B., Daigle, M., Chen, R. & Daskalakis, Z. J. The relationship between cortical inhibition, antipsychotic treatment, and the symptoms of schizophrenia. Biol. Psychiatry 65, 503–509 (2009).
Mehta, U. M., Thirthalli, J., Basavaraju, R. & Gangadhar, B. N. Association of intracortical inhibition with social cognition deficits in schizophrenia: findings from a transcranial magnetic stimulation study. Schizophr. Res. 158, 146–150 (2014).
Mehta, U. M. et al. A transdiagnostic evaluation of cortical inhibition in severe mental disorders using transcranial magnetic stimulation. J. Psychiatr. Res. 143, 364–369 (2021).
Miyazawa, A. et al. Clozapine prolongs cortical silent period in patients with treatment-resistant schizophrenia. Psychopharmacol. Bull. 51, 20–30 (2021).
Oxley, T. et al. Repetitive transcranial magnetic stimulation reveals abnormal plastic response to premotor cortex stimulation in schizophrenia. Biol. Psychiatry 56, 628–633 (2004).
Pascual-Leone, A., Manoach, D. S., Birnbaum, R. & Goff, D. C. Motor cortical excitability in schizophrenia. Biol. Psychiatry 52, 24–31 (2002).
Roeh, A. et al. Effects of three months of aerobic endurance training on motor cortical excitability in schizophrenia patients and healthy subjects. Neuropsychobiology 79, 100–107 (2020).
Schecklmann, M., Weidler, C., Eichhammer, P., Hajak, G. & Langguth, B. Increased short-interval intracortical inhibition in un-medicated patients with schizophrenia. Brain Stimul. 11, 1080–1082 (2018).
Soubasi, E. et al. Cortical motor neurophysiology of patients with schizophrenia: a study using transcranial magnetic stimulation. Psychiatry Res. 176, 132–136 (2010).
Tang, Y. et al. Prolonged cortical silent period among drug-naive subjects at ultra-high risk of psychosis. Schizophr. Res. 160, 124–130 (2014).
Wobrock, T. et al. Motor circuit abnormalities in first-episode schizophrenia assessed with transcranial magnetic stimulation. Pharmacopsychiatry 42, 194–201 (2009).
Fitzgerald, P. B., Brown, T. L., Daskalakis, J. Z. & Kulkarni, J. A transcranial magnetic stimulation study of the effects of olanzapine and risperidone on motor cortical excitability in patients with schizophrenia. Psychopharmacology 162, 74–81 (2002).
Davila-Pérez, P., Jannati, A., Fried, P. J., Mazaira, J. C. & Pascual-Leone, A. The effects of waveform and current direction on the efficacy and test-retest reliability of transcranial magnetic stimulation. Neuroscience 393, 97–109 (2018).
Kaar, S. J., Natesan, S., McCutcheon, R. & Howes, O. D. Antipsychotics: mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacology 172, 107704 (2020).
Klomjai, W., Katz, R. & Lackmy-Vallée, A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Ann. Phys. Rehabil. Med. 58, 208–213 (2015).
Miyazawa, A. et al. The cortical silent period in schizophrenia: a systematic review and meta-analysis focusing on disease stage and antipsychotic medication. J. Psychopharmacol. 36, 479–488 (2022).
Zeugin, D. & Ionta, S. Anatomo-functional origins of the cortical silent period: spotlight on the basal ganglia. Brain Sci. 11, 705 (2021).
Tao, H. W., Li, Y. & Zhang, L. I. Formation of excitation-inhibition balance: inhibition listens and changes its tune. Trends Neurosci. 37, 528–530 (2014).
Jardri, R. et al. Are hallucinations due to an imbalance between excitatory and inhibitory influences on the brain? Schizophr. Bull. 42, 1124–1134 (2016).
Vucic, S. et al. Clinical diagnostic utility of transcranial magnetic stimulation in neurological disorders. Updated report of an IFCN committee. Clin. Neurophysiol. 150, 131–175 (2023).
Polanía, R., Nitsche, M. A. & Ruff, C. C. Studying and modifying brain function with non-invasive brain stimulation. Nat. Neurosci. 21, 174–187 (2018).
Bradley, C., Nydam, A. S., Dux, P. E. & Mattingley, J. B. State-dependent effects of neural stimulation on brain function and cognition. Nat. Rev. Neurosci. 23, 459–475 (2022).
Zrenner, C. & Ziemann, U. Closed-loop brain stimulation. Biol. Psychiatry 95, 545–552 (2024).
Grent-’t-jong, T. et al. Resting-state gamma-band power alterations in schizophrenia reveal e/i-balance abnormalities across illness-stages. eLife 7, e37799 (2018).
Martínez-Cañada, P. et al. Combining aperiodic 1/f slopes and brain simulation: an EEG/MEG proxy marker of excitation/inhibition imbalance in Alzheimer’s disease. Alzheimers Dement. 15, e12477 (2023).
de Wilde, O. M., Bour, L. J., Dingemans, P. M., Koelman, J. H. T. M. & Linszen, D. H. A meta-analysis of P50 studies in patients with schizophrenia and relatives: differences in methodology between research groups. Schizophr. Res. 97, 137–151 (2007).
Hill, A. T., Rogasch, N. C., Fitzgerald, P. B. & Hoy, K. E. TMS-EEG: a window into the neurophysiological effects of transcranial electrical stimulation in non-motor brain regions. Neurosci. Biobehav. Rev. 64, 175–184 (2016).
Takahashi S, Ukai S, Kose A, Hashimoto T, Iwatani J, Okumura M, Tsuji T, Shinosaki K (2013) Reduction of cortical GABAergic inhibition correlates with working memory impairment in recent onset schizophrenia. Schizophr. Res. 146, 238–243. https://doi.org/10.1016/j.schres.2013.02.033.
Acknowledgements
The study is supported by the Hungarian Research Foundation grants (OTKA FK 138385).
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
O.L.: conceptualization, search, selection, data extraction, analysis, ROB assessment, writing—original draft; B.K. and D.B.: search, selection, data extraction, ROB assessment; A.S. and M.E.: methodological guidance, review; P.H., Z.M., A.H., and Z.U.: methodological guidance, review; P.F.: statistical guidance; G.C.: conceptualization, methodology, analysis, writing, review. All authors certify that they have participated sufficiently in the work to take public responsibility for the content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lányi, O., Koleszár, B., Schulze Wenning, A. et al. Excitation/inhibition imbalance in schizophrenia: a meta-analysis of inhibitory and excitatory TMS-EMG paradigms. Schizophr 10, 56 (2024). https://doi.org/10.1038/s41537-024-00476-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-024-00476-y
- Springer Nature Limited