Abstract
While chronic limb-threatening ischemia is a serious peripheral artery disease, the lack of an appropriate stent significantly limits the potential of interventional treatment. In spite of much progress in coronary stents, little is towards peripheral stents, which are expected to be both long and biodegradable and thus require a breakthrough in core techniques. Herein, we develop a long and biodegradable stent with a length of up to 118 mm based on a metal-polymer composite material. To achieve a well-prepared homogeneous coating on a long stent during ultrasonic spraying, a magnetic levitation is employed. In vivo degradation of the stent is investigated in rabbit abdominal aorta/iliac arteries, and its preclinical safety is evaluated in canine infrapopliteal arteries. First-in-man implantation of the stent is carried out in the below-the-knee artery. The 13 months’ follow-ups demonstrate the feasibility of the long and biodegradable stent in clinical applications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Peripheral arterial disease (PAD) is one of the most prevalent diseases in the world, resulting in around a quarter million of amputations in United States and Europe annually, and millions worldwide1. Claudication, ischemic rest pain, non-healing ulcer, focal gangrene and tissue loss in lower limb are the early symptoms before amputation, and the classification of Rutherford class about symptoms relevant to low limb artery is schematically presented in Fig. S1. Most of these clinical symptoms can be remitted by re-opening the occluded lower limb artery2. The main endovascular-first therapy for PAD is percutaneous transluminal angioplasty with bare balloon, which results in high incidence of restenosis due to limited acute lumen gain, elastic recoil and dissections2,3. The below-the-knee (BTK) lesion with chronic limb-threatening ischemia (CLTI) is the most difficult disease to treat due to complex anatomy such as long diffuse stenosis, chronic total occlusion (CTO) and serious calcification; the patency of percutaneous transluminal angioplasty was 50%-80% after one year4.
Stents play a crucial role in interventional treatment of cardiovascular diseases5,6. During the latest score years, various coronary stents have been developed7,8, and either long or biodegradable cardiovascular stents are dependent upon cutting-edge techniques9. However, there is so far no stent compatible with both biodegradability and long length, which is demanded for millions PAD patients and challenging in science and technology10. Although many coronary stents have been applied off-label in PAD treatment, the development of a long & biodegradable peripheral stents are still critical.
Conventional stenting was ever tried to improve the patency issue in BTK. Bare metal stents (BMS) have failed to prove its superior over percutaneous transluminal angioplasty, and drug eluting stents (DES) have only been successful in short infrapopliteal lesions according to some randomized controlled trials11,12,13. But in the real world, the majority of PAD treated lesions are long CTO (>40 mm) and seriously calcified14. The DES is normally non-biodegradable and short (8–38 mm), and thus it is inevitable to use two or more stents to cover the entire long BTK lesion, which raises uncertain prognosis results for the interventional lesions15. Another main issue of a permanent stent applied in BTK lesions is of high target lesion failure (TLF), which leads to higher rates of in-stent restenosis (ISR) or occlusion, and more seriously it is difficult to re-canalize or re-dilate an ISR lesion due to the cage of the original stent16. Thus, no permanent DES has been approved by US food and drug administration (FDA) in the treatment of BTK lesion and only for bail-out as off-label use. Other technologies, such as debulking/atherectomy equipment, score/ultrasonic balloon, and drug-coated balloon were tried for infrapopliteal lesion, but failed to be a mainstream therapy over percutaneous transluminal angioplasty with limited comparative data2.
A biodegradable stent (BDS) is expected to not only keep the lumen away from recoil and dissection in the early stage, but also avoid long term side effects of permanent implants, and thus promising as an ideal solution for PAD intervention in the future17. Polymer-based BDS has a satisfactory patency in short lesions of infrapopliteal artery. However, its small stent length (≤38 mm) and large strut thickness (>100 μm) have confined its clinical application for long lesion18. Metal-based BDS is another option for the treatment of BTK lesions19,20. Such BDSs may be magnesium-based21,22, zinc-based23 or iron-based24,25,26,27,28. Among all the BDSs, iron-based one can provide the strongest mechanical performance, which is comparable to the gold-standard permanent cobalt chromium (CoCr) alloy stent, namely, the Xience PrimeTM stent. The rest BDSs have to compromise their strut thickness to achieve equal mechanical performance. However, iron degrades slowly in human body (more than five years). If one technique can speed up iron degradation to an appropriate degradation period in human body, an iron-based stent with long length and high mechanical strength might revolutionize the interventional treatment of BTK diseases, which frequently accompany with the long and seriously calcified infrapopliteal lesion.
The present study reports a long & biodegradable stent (LBS) with metal-polymer composite technique to treat infrapopliteal artery disease. While an LBS is much required for PAD treatment, research and development (R & D) of LBS is faced with three key problems — how to maintain early stenting with degradation until vessel remodeling, how to achieve homogeneous coating, and how to access its safety and effectiveness after implantation, as schematically presented in Fig. 1. To resolve these difficulties towards fabricating the first long and biodegradable peripheral stent is the theme of the work reported in this article.
Schematic presentation of the current situation of percutaneous transluminal intervention in arteriosclerosis obliterans of lower limb artery, the motivation and difficulties to develop a biodegradable long stent, the rational to design a long & biodegradable stent (LBS) based on metal-polymer composite, and the main tests of the LBS in vitro and in vivo. Here, the term “TLF” denotes target lesion failure.
In this work, we introduced appropriate nitriding of iron to enhance the mechanical performance of the metal, a zinc layer to prevent early corrosion of iron, and a poly(D, L-lactide) (PDLLA or simply denoted as PLA) coating to speed up the corrosion of iron with the metal-polymer composite technique. The term “composite” to describe the polymer-coated metal comes from the unexpected “accelerating” of iron corrosion by the PLA layer instead of “protection”, which has been elaborated in our previous study of coronary stents29,30,31. However, we found that it was hard to prepare the homogeneous PLA coating on a long stent simply by traditional ultrasonic spraying, the standard technique to coat short stents.
Eventually, we introduced a magnetic levitation (Maglev) technique into the field of biomedical engineering to improve the homogeneity in coating a long stent. Here, the Maglev technique is not identical to, and in fact more convenient than that used in high-speed train in the field of transportation vehicles32. The state-of-the-art technique to fabricate a long composite stent achieved by the Maglev principle will be revealed in this article. The resultant LBS with the length of 118 mm and the total strut thickness of 70 μm is suitable for infrapopliteal complex anatomy lesions, which are of small diameter (2–4 mm), serious calcification, CTO lesion or long and diffuse stenosis lesion. The present paper reports the core technique and the underlying principle of the LBS, its fabrication, and the corresponding in vitro and in vivo performances.
Results
Strengthening iron raw material via nitriding
Pure iron has higher strength, ductility, and formability than zinc and magnesium, which allows iron stents with thinner struts and more delicate patterns. Nevertheless, its tensile strength, ranging 230∼345 MPa, is still lower than that of CoCr alloy for permanent stents, ∼1000 MPa. In order to further increase the tensile strength of iron without sacrificing its biological performance, we tried to add trace nitrogen into iron matrix. A schematic diagram of the nitriding process is given in the left of Fig. S2.
While the nitriding technique has been widely applied to improve surface performances of metal such as hardness, fatigue strength and corrosion resistance, the present technique is unique because the nitriding technique was employed as bulk alloying instead of surface modification and could enhance the performance of the whole metal. The tensile strength of the iron tube increased with nitrogen content till 1000 MPa when nitrogen concentration reached 0.08 % as shown in the right of Fig. S2, which is far larger than the tensile strength of the pure iron tube of 315 MPa.
Achieving a homogeneous PLA coating on a long stent via Maglev
The evenness of the polymer coating is critical for a metal-polymer composite based stent, which is particularly important and yet difficult for an LBS. A long stent is expected to be flexible to match the curved vessels and avoid additional mechanical stimulation to vessel walls. However, one end of the stent must be fixed to enable another one exposed to the spayed solution and then the two ends are altered in order to avoid the blank of coating on any end. Thus a long stent was bent and woggled during the spraying blow and stent gravity, as demonstrated in the left of Supplementary Video S1. This is harmful for a homogeneous coating.
In order to improve the uniformity and integrity of the coating on a long stent, the technique must be contactless and compatible with fixing the end of the stent. It has eventually achieved by us after introducing a Maglev technique. A non-contact magnet was exerted to the free end, as schematically presented in Fig. 2. The otherwise floated stent was then stabilized, as shown in the right of Supplementary Video S1.
The measurement of coating thicknesses in Fig. 2 confirmed the homogeneity of the resultant PLA coating on a long stent surface after introduction of the columnar magnet. We further carried out in vitro bench tests of our Maglev-fabricated LBS, and the results are shown in Fig. S3. The iron-based LBS exhibited comparable mechanical performances to the non-biodegradable Xience composed of CoCr alloy and another biodegradable stent Absorb composed of hydrolysable polymer PLA33. Our LBS is of the thinnest thickness with 70 µm versus 96 µm (Xience) and 150 µm (Absorb) in 3.0 diameter specification. Moreover, the foreshortening rate and elastic recoil rate of LBS were as small as 1.7% and 3.8%, respectively.
Confirming the tuned in vitro degradation of LBS in Hank’s solution and in vivo degradation profile in small animals
The most important bottleneck of iron as a biodegradable material for a cardiovascular stent is its slow in vivo degradation. The content of iron in the LBS can be significantly reduced due to great mechanical performance by nitriding, and the less iron usage may contribute partially to less degradation time of the stent. To further accelerate the degradation of the nitrided iron, we applied a PLA coating on the iron. In vitro testing in plasma-mimetic Hank’s solution demonstrated the faster mass loss of iron in the Fe-PLA composite. Nevertheless, an ideal design of a biodegradable stent provides sufficient radial strength until remodeling of the damaged vessel, and thus overly rapid degradation of a stent will lead to its early collapse. So we further introduced a zinc layer, making use of the more active zinc to delay the early degradation of iron.
We carried out in vitro degradation in Hank’s solution at 37 °C (Fig. S4) and in vivo degradation in the rabbit model (Fig. 3). The results illustrated that our LBS of Fe-Zn-PLA is capable of both early supporting and in-time degradation. In the rabbit model, the LBS degraded mostly within 24 months after implantation, maintained intact in the first 2 months, the Zn buffer layer completely degraded in about 3 months. The 70% sirolimus was released in the first three months, and the remaining part was later slowly released along with degradation of PLA.
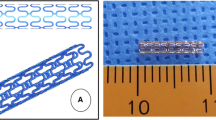
A Degradation profiles of each component. The left is a schematic presentation of the degradation profiles of nitrided Fe, Fe-PLA and Fe-Zn-PLA. Here, Fe means the bare nitrided iron stent, Fe-PLA means the bare nitrided iron stent coating with a PLA layer loaded with sirolimus, and Fe-Zn-PLA means the bare nitrided iron stent coating with a zinc layer and a PLA layer loaded with sirolimus. The right shows the degradation profiles of Fe (the number of animals N = 9, the number of stents for each group n = 11 at the time point of month 2; N = 7, n = 11 at month 3; N = 9, n = 11 at month 6; N = 6, n = 11 at month 9; N = 9, n = 11 at month 12; N = 7, n = 11 at month 24), Zn (N = 10, n = 11 at month 1; N = 10, n = 11 at month 2; N = 7, n = 11 at month 3) and PLA (N = 3, n = 9 at month 3; N = 3, n = 9 at month 6; N = 1, n = 3 at month 12; N = 1, n = 3 at month 18) in the LBS in rabbits, and the release curve of the drug (N = 3, n = 6 on day 7; N = 3, n = 6 on day 14; N = 3, n = 6 on day 30; N = 3, n = 6 on day 60; N = 3, n = 6 on day 90; N = 5, n = 10 on day 180; N = 1, n = 2 on day 360). For each group, the data are shown in mean ± standard deviation. B The sirolimus-eluting biodegradable LBS. The top shows an LBS stent system before balloon inflation and after balloon inflation; the bottom shows a scanning electron microscopy (SEM) image of the cross section of the stent and the cross section of the strut. Three samples were repeated independently with similar results. C The typical micro-computed tomography (micro-CT) images of implanted LBS till 24 months and the histopathology image at 24th month. Five samples were repeated independently with similar results.
An LBS in a balloon delivery system is demonstrated in Fig. 3B. When the balloon was inflated, the pattern of the stent can be evenly expanded. The SEM image of the cross-section also confirmed the uniform expansion and coating evenness of the LBS, and the strut thickness of the LBS was 70 μm including the metal skeleton and polymer coating.
Figure 3C presents the typical micro-CT images and the histological observations of our LBS in rabbit aorta/lilac. The stent struts kept clear and intact at 1 month, then the struts turned to obscure and partially degraded at 12 months, and most of the stent degraded at 24 months. No stent collapse was observed during the degradation, demonstrating that the duration of stent stenting was sufficient for vessel remodeling. The histopathology image shows the section of the rabbit abdominal aorta at 24 months. Neither pronounced neointimal proliferation nor significant inflammatory responses of the stented vessel were found.
Confirming biocompatibility of LBS in vitro and in vivo
We carried out a series of in vitro biocompatibility tests following the regulation of international standard organization (ISO) including Ames test, mouse lymphoma gene mutation test, micronucleus test, hemolysis test-direct contact, hemolysis test-extraction, complement activation test, partial thromboplastin time, and cytotoxicity test. The results are summarized in Table S1. All of the tests confirm that our LBS met the biocompatibility requirements by ISO for implanted medical devices.
We also perform the comparative histological evaluations of the LBS stent and Xience stent in the 1-month and 6-month follow-ups of the canine model. The representative images of the histological evaluation are demonstrated in Fig. S5, the score criteria are listed in Table S2 and the resultant scores for all of groups are summarized in Table S3. While there were statistical differences in macrophages, phagocytosis and degradation between LBS and Xience groups (p < 0.05), no statistical differences in the inflammatory response of polymorphonuclear cells, lymphocytes, plasma cells, giant cells, necrosis and fibrosis were observed between the two groups. Combination of the in vitro and in vivo assessments illustrates good biocompatibility of the metal-polymer composite LBS.
Another issue indirectly pertinent to biocompatibility of a medical device is its physiochemical stability during sterilization. All of the LBS used for testing experienced sterilization by ethylene oxide (EO). Although EO sterilization has been reported to affect molecule weight (MW) of polymer34, this effect can be mitigated by optimizing the sterilization parameters such as lowering temperature, decreasing reduced sterilization time, reducing EO sterilization concentration and exposure time. As a result, MW of PLA changed little under our experimental conditions, as evidenced from Table S4. In order to further evaluate the potential effects of sterilization on the encapsulated drug in the PLA coating, we also quantified drug contents before and after EO sterilization. The drug recovery rate was then determined from the amount of the remained drug in stents over the amount of added drug in stents. The calculated drug recovery rate of LBS before EO sterilization was 96.8%, and that after EO sterilization was as high as 96.9%.
Rational to select canine as large animal model to access BTK stent & confirmation of operability and safety of LBS
FDA recommends minipig coronary model and rabbit iliac model for preclinical animal study of bioresorbable coronary stents, and a large amount of historical data has been accumulated. However, those animals have not a blood vessel well suitable for mimicking the human infrapopliteal artery. Herein, we select the model of canine BTK vessels to access peripheral-vessel stents, considering their similar vessel dimension, location, movement, and physiological indicators such as body temperature, blood pH, blood pressure and blood flow velocity.
In order to create an injury model, we generated an injury of over-expansion (1.1–1.2 folds of vessel diameter) to stimulate the proliferation in healthy canine infrapopliteal artery. Our LBSs as well as the gold standard interventional stents Xience were implanted into the posterior tibial arteries in the left and right hind legs. Optical coherence tomography (OCT) measurements were performed immediately after stent implantation and at the expected angiographic follow-up time windows. According to Fig. 4, no stent discontinuity or collapse was observed at the examined time points. In the group of LBS, the shadow behind the struts became obscure after 6 months, indicating the corrosion of the stent struts; in contrast, there was no change of struts in Xience stents with time. The corresponding values of neointimal thickness of LBS and Xience are summarized in Fig. S6. The evaluation of neointimal hyperplasia illustrated no significant difference between LBS and Xience at each follow up period.
The upper are follow-up OCT images after 0, 1, 3, and 6 months of LBS and Xience stent implantation. The lower right image illustrates the calculation for percentage luminal area stenosis, and the lower left summarizes the calculated values of both LBS and Xience in each follow-up point, where the dotted line indicates the allowance criterion of area stenosis. For each group, n = 5 independent samples in individual animals. The data are shown in mean ± standard deviation. Two-sided student’s t test with no adjustments was used.
Area stenosis is usually defined as smallest lumen area at time t over the initial value at time zero35,36. However, we found that the above traditional calculation would mislead the evaluation of the BTK vessels due to the anatomy of canine BTK artery. The stents would be recoiled in accompany with degradation in canine peripheral arteries, which does not occur in human infrapopliteal arteries possibly because of sufficient muscle protection in human legs. Thus, we propose to separate the stenosis into two parts: one is the percent lumen area stenosis, the other one is stent recoil rate. The data of stent recoil are summarized in Fig. S7. During the first three months of implantation, the stent recoiled similarly to Xience. Afterwards, our stents began to degrade significantly, leading to significant higher recoil of LBS than Xience stents at 6 months. In this canine study, we evaluated the histological response of BTK artery to LBS mainly from percent luminal area stenosis, which is decoupled with recoil rate. The calculated values of percent luminal area stenosis are presented in Fig. 4, exhibiting no significant difference between LBS and Xience at all of the examined time points, 1 month, 3 months and 6 months.
First-in-human evaluation of LBS and its follow-ups
The initial subject of our study in the first-in-human or first-in-man (FIM) examination was an octogenarian male with a six-decade history of managed hypertension, absent of any diabetic complications. The patient had experienced bilateral lower extremity claudication for a duration of two years, constrained to a limping distance of approximately 20 meters. Notably, symptoms were more pronounced in the left lower extremity compared to the right. Clinical evaluation yielded a diagnosis of lower extremity arteriosclerosis with Rutherford class 3, denoting severe intermittent claudication. To ameliorate functional impairment and enhance life quality of the patient, percutaneous transluminal angioplasty was initially conducted. Angiographic assessment revealed occlusions in the tibio-peroneal trunk (TPT) and peroneal artery (PA) of the left leg; only the posterior tibial artery (PTA) remained patent. Subsequently, BTK interventional therapy was executed, following informed consent from the patient and ethical committee approval. The interventional process is shown in Supplementary Video S2, and the typical procedures are demonstrated in Fig. 5.
Firstly, an angioplasty was made to find the target lesion with occlusion of TPT; secondly, a pre-dilatation balloon was used to reopen the occluded lesion, and then an angioplasty was performed to check the pre-dilatation result; thirdly, as the lesion was partially patent with dissection and recoil that need further treatment, an LBS (Φ3.0 × 38 mm) was deployed by balloon dilatation. After the implantation of the stent, the patient exhibited no residual restenosis of his vessel, as seen in the last angioplasty image.
Additional diagnostic data, including preoperative computed tomography (CT) and ultrasonography, are presented in Fig. 6. CT revealed an infrapopliteal disease with a patent P3 (popliteal artery, from the center of knee joint space to the origin of anterior tibial artery) and PTA, while PA and TPT were not well visualized. According to the ultrasonography evaluation, the P3 segment was patent and the preoperative flow rate was 29.3 cm/s, but the TPT was occluded with an almost zero flow rate. In order to achieve at least one direct flow to the foot, his TPT should be re-canalized. After the interventional treatment, the occluded TPT was stented, resulting in a significant increase of blood flow from 0.0 cm/s to approximately 98.4 cm/s, showcasing the effective lumen maintenance by our LBS. The long-term follow-up at 13 months confirmed the enduring functionality of the stent and sustained arterial patency (Rutherford class 0).
The left upper image comes from the preoperative CT of the left leg. The right shows the ultrasonography images at the indicated time points. Based on preoperative ultrasonography, the diameter of the occluded lesion was 0.23 cm, and the lesion was measured 2.7 cm in length. The P3 segment was patent with 29.3 cm/s flow rate, but the TPT was occluded with 0 cm/s flow rate. After the implantation of LBS, postoperative ultrasonography illustrated increased flow rates in both P3 and TPT, which were 49.4 cm/s and 98.4 cm/s, respectively. After 13 months, the flow rates of PA and TPT read 29.7 cm/s and 56.6 cm/s respectively, which remain satisfied as the blood supply to the foot.
The second case is a 69-year-old male of Rutherford class 5 with a non-healing ulcer, focal gangrene, and small tissue loss. According to preoperative angioplasty, there were a patent TPT, a diffuse-stenosis PTA, and an occluded PA (Fig. 7). Assisted by a guidewire to cross the PTA lesion and PA lesion, we used a balloon of Φ2 × 80 mm for the PTA; subsequently, an LBS (Φ2.75 × 78 mm) was strategically positioned at the site of the PTA lesion and successfully expanded using nominal inflation pressure. For comparison, long-segment occlusive lesions in PA were treated with a Φ2.5 × 170 mm balloon dilatation. Post-angioplasty imaging revealed fully patent PTA and PA, correlating with immediate symptom alleviation (Rutherford class 2) after the intervention. The 6-month follow-up angiography of this case showed that the stenosis rate of the PTA lesion was 30% while that of the PA lesion was 80%.
The preoperative angiography showed that the target lesion was the PTA, and the length of the lesion was approximately 60 mm. As indicated by the postoperative angiography, an LBS (Φ2.75 × 78 mm) was successfully implanted and the target lesion was well stented without residual stenosis. By contrast, there was a long-segment occlusive lesion in the PA, which was treated with balloon dilation. After the interventional treatment, the residual stenosis was approximately 10%. The six-month follow up angiography showed that the PTA target lesion remained patent without obvious restenosis and the LBS profile maintained well without collapse. The raw image and the schematic image of the LBS profile under X-ray without the contrast agent are presented in the bottom right in order to visualize the whole stent in the leg site, indicating no significant recoil of the stent. The target lesion stenosis rate of PTA was 30%, whereas the lesion stenosis rate of PA has increased to 80%.
Case three is also a 69-year-old male but with a Rutherford classification 3 with severe claudication. The patient involved an LBS (Φ2.75 × 58 mm) implanted in his PA. The six-month follow up demonstrated that the PA lesion was patent and the LBS stented well, as presented in Fig. S8. It is satisfactory that Rutherford classifications improved from class 5 to class 2 in the second patient (with mild claudication) and from class 3 to class 0 in the third patient (asymptomatic) after six months after LBS implantation.
Cumulatively, all of the cases presented herein validate the operability, safety, and potential effectiveness of the LBS technology. We are currently in the clinical trial phase. Comprehensive statistics from multi-center trials will be reported by clinical teams in the future.
Discussion
The latest decade has witnessed much progress in biomaterials for medical devices and pharmaceutics etc.37,38,39,40,41,42,43. Among various biomaterials44,45,46, a cardiovascular stent is technically faced with much difficulty. An ideal stent appropriate for interventional treatment is expected to be highly deliverable with a thin-strut, low profile, flexible design and high radial strength47. The current commercialized permanent stents for infrapopliteal artery are only for bail-out failing balloon angioplasty, such as elastic recoil due to recanalize CTO lesion, as schematically presented in Fig. S9. The long lesions prevalence in peripheral artery and the scruple for ISR have hindered the stent application as a primary treatment. Repair of a long lesion needs to implant more than one stent. Then, either a gap area or an overlapping area of two stents leads to an intrinsic risk of local in-stent restenosis, while one long stent can avoid such dilemma, as schematically presented in Fig. S10. A biodegradable stent theoretically would improve the “caged vessel” and eliminate the scruple of ISR, as presented in Fig. S11. Hence, an LBS is an ideal and more customized for infrapopliteal artery.
A biodegradable long stent is reported in this article. The biomaterial innovations supporting the advantages of our metal-polymer composite based LBS over other BRSs and permanent stents are summarized from the following three main aspects.
(1) The bulk-alloy nitriding iron to strengthen the backbone material of the stent. We applied nitriding followed by thermal treatment and drawing of the iron tubes to strengthen iron. During the whole nitriding process, no other metallic or toxic element but nitrogen was incorporated into the LBS matrix. Bulky alloying of the iron stent through nitriding elevates the tensile strength by dispersive precipitates of Fe4N and over-saturated solution of nitrogen in iron lattices without formulation of any white nitriding layer on the surface. Moreover, nitrided iron degrades faster than pure iron owing to the additional galvanic corrosion between iron matrix and dispersive scattered Fe4N precipitations48. The first pure iron stent, NOR-I, reported for the preclinical study by Matthias Peuster et al. is of thickness 100-120 μm, Φ3 × 16 mm weighed 41 mg49. In contrast, our LBS is of 53 μm iron strut with the thickness excluding the PLA layer, and a much longer Φ3 × 118 mm LBS contains about 74 mg of iron. Owing to the enhanced mechanical properties after alloying, the amount of iron has been reduced 76% under a given stent length, which shortens the degradation period of the stent as well as enhancing the compliance of the mini-invasive device significantly. The resultant thin stent affords a sufficient mechanical stenting in BTK artery as a balloon-expandable stent like the Xience prime stent approved for BTK by Communate Europpene (CE).
(2) Magnetic levitation to enable a homogeneous polymer coating on a long metal stent. Fabrication of a long peripheral biodegradable stent is faced with difficulties such as mitigating the deviation of the dimension and homogeneity of a long stent in axial direction. Herein we introduced a magnetic levitation to fix the free end of the long stent in a contactless way. This technique avoids stent bending and fluctuating during the coating process, and thus significantly improves the coating homogeneity (Fig. 2, Supplementary Video S1). Based on characteristics of the iron materials and the infrapopliteal lesion (long and seriously calcified), the longest Maglev-fabricated LBS was 118 mm, three times of the longest balloon-expandable peripheral stents (38 mm) in the global market.
(3) Combination of a microscale PLA coating and a nanoscale Zn layer to adjust the profile of iron corrosion. There are many advantages of iron stents as peripheral stents, such as high mechanical performance, good biocompatibility and established absorption mechanism. A challenge of iron as a biodegradable material for a BTK stent is how to mediate its degradation in arterial blood under a weak alkaline environment (pH 7.4). Early in 1924, Whitman et al. from the Massachusetts Institute of Technology found that the local pH and thus hydrogen-ion concentration could influence metal corrosion significantly50. It is also known that polyester hydrolysis can lead to an acidic environment51. Herein, we introduced a PLA coating to create a local acid environment, taking advantage of hydrolysis of aliphatic polyester. In order to avoid early stent collapse while speeding up iron degradation, we applied a polyester of 200 kDa MW for the PLA coating, where the relatively high-MW PLA would hydrolyze and create acid local environment in a sustained manner. Another critical design of our LBS as the BTK stent is the addition of a Zn buffer layer on iron surface to prevent overly early iron degradation. To this end, we prepared a zinc layer of 600 nm thickness by electroplating on iron as a sacrifice anode to delay the onset of iron corrosion owing to a galvanic effect. This Zn layer was found to prevent iron from degradation for the first three months after implantation, as reflected from the in vivo biodegradation in rabbit aorta/lilac (Fig. 3). Eventually, the Fe-Zn-PLA design matches with both stenting at the early stage and remodeling at the late stage.
In order to evaluate the operability and safety of the stent in interventional treatment, we implanted an LBS and a gold standard non-biodegradable stent (Xience) into canine infrapopliteal arteries of each hind legs for control. Our LBS was transcatheter implanted smoothly as well as Xience. No stent thrombosis was found in both groups according to the OCT observations on 1, 3, and 6 months after implantation. Both groups had a trend of less neointimal hyperplasia along with time, which might be influenced by the early fibrosis deposition. It is worthy of mentioning that the abnormal stent recoil was observed in both groups in the canine model, especially when LBS started to degrade after 3 months. This might be relevant to lacking peripheral muscle to protect the BTK artery in the canine model. After eliminating the stent recoil and calculation of percent lumen area stenosis up to 6 months of follow ups, we confirmed the safety and effectiveness of LBS in large animals. For the long-term study of iron degradation and absorption, we ever evaluated the bare nitrided Fe stent in porcine coronary arteries for 7 years, iron based biodegradable stents in porcine coronary arteries for 5 years and in human coronary arteries for 3 years; no aneurysms or significant neointimal hyperplasia were observed during the degradation process of iron materials in all of these cases52,53,54.
In this article, we also demonstrate the clinical cases of the LBS (Figs. 5–7, Fig. S8). According to the quantitative BTK vessel angioplasty of the first patient, there is a chronic total occlusion of 25 mm length in TPT. Other main artery such as anterior and peroneal arteries are with even longer CTO to the footage. In order to relieve the ischemic, this operation was to acquire at least one patent artery directly to the foot. Thus, a pre-dilatation balloon was applied to reanalyze the tibio-peroneal CTO lesion. Angioplasty demonstrated a limited dissection that needed further treatment. An LBS was thus used to settle the dissection, and a desired lumen gain was achieved. Both the flow rates of PA and TPT vessels were significantly improved. The long-term follow-up of TPT lesion up to 13 months (Fig. 6) illustrated the feasibility of LBS applied in BTK application.
According to the quantitative vessel angioplasty of the second patient (Fig. 7), there is a severe BTK stenosis of 60 mm length in the PTA. Other main artery such as the middle segment of the peroneal artery and the anterior tibial artery are with even longer CTO to the footage. In order to relieve the ischemic, this operation was to acquire at least one patent artery directly to the foot. Thus, a pre-dilatation balloon was applied to reanalyze the PTA lesion, followed by angioplasty and implantation of an LBS. The PTA vessel kept patent till the longest follow-up (6 months). The third case (Fig. S8) further strengthened the operability, safety, and potential effectiveness of the LBS.
Basically, there are two fashions of stents for interventional treatments of cardiovascular diseases, self-expandable and balloon-expandable. Recently, a long self-expandable DES (Φ3.5 × 80 mm) named SAVAL was compared with balloon angioplasty, and according to the outcome of the clinical trial published in December, 202355, the self-expandable DES showed no benefit of one-year patency compared with the classical percutaneous transluminal angioplasty. As usual, all of the commercializable self-expandable stents are, just like examined in this reference, made of nitinol, taking advantage of the superelasticity of this marvelous alloy. Unfortunately, this metal is of low modulus and thus as indicated the Discussion of this important clinical paper “nitinol stents, as used in this trial, have greater wall thickness and other geometric differences compared with balloon-expandable metallic coronary stents used below the knee, which may affect endothelialization and thus clinical outcomes”55. The valuable 2023 clinical article releases objectively a failure result, and suggests that “continued innovation to provide optimal treatments for CLTI is needed” in the end of its abstract55. Our invention of a balloon-expandable LBS is just a demonstration of “innovation for CLTI”.
As balloon-expandable stents are concerned, a polymer-based biodegradable stent named Esprit BTK with its strut thicker than the gold standard nonbiodegradable stent Xience were approved by FDA at April 2024. The maximum length of Esprit BTK was 38 mm, and thus abutting and overlapping of more than two stents are inevitable in dealing with long peripheral lesion; its ISR rate was less than that of balloon angioplasty. An appropriate stent applied in infrapopliteal artery should care the decrease ISR as well as the increase of the stent length. In our FIM study (Fig. 7), case two is so special that the doctor implanted LBS to one of the main BTK vessels and dealt with another parallel BTK vessel using only balloon. The follow-ups indicate that the ISR after 6 months was 30% for the vessel with LBS and 80% for the vessel only expanded by a balloon. In spite of only one clinical case, the data have preliminarily indicated the benefit of our LBS compared with PTA in a long infrapopliteal artery lesion.
While long lesions frequently occur in the case of BTK artery, the longest approved balloon-expandable stent is of 38 mm length owing to engineering difficulty56. It is even more challenging to prepare a stent which is both long and biodegradable. Hence, our biodegradable and long (up to 118 mm) balloon-expandable stent is of significant technological advance, as compared with other stents summarized in Table S5.
In conclusion, this paper reports the core technique of a long biodegradable stent. The LBS of 70 µm strut thickness is based on a metal-polymer composite, which is mainly composed of nitrided iron and PLA. The PLA coating was found not to protect iron from degradation but to speed up its degradation. Inspired by the Maglev train, we employed this remote-control technique to achieve a stable and homogeneous ultrasonic spray of a PLA solution to a long stent. Furthermore, this study demonstrates the feasibility of LBS applied in BTK lesion based on in vitro tests, rabbit and canine in vivo experiments, and the FIM clinical study. The three clinical cases have covered all of the main BTK arteries, namely, TPT, PTA, and PA. While stent-based interventional treatment is currently not the first-line therapy due to lack of an appropriate stent, the present report might revolutionize the first-line surgical method to deal with diseases of peripheral vessels. The clinical implantation of our LBS is the first case for a biodegradable long stent to be applied in interventional therapy of not only infrapopliteal artery disease but also in other indication with stent-like medical treatment. Therefore, the present study which covers from the fundamental research of biomaterials to the FIM implantation in BTK arteries has shed new insight to develop various long & biodegradable medical devices.
Methods
Fabrication of nitrided-iron tubes and LBS stents
A pure iron tube (Φ6.0 mm, wall thickness 0.5 mm) was cut into segments with 25–35 cm length. The tube segments were put into an in-house-design nitriding furnace to be nitrided with a gas method. We carried out the initial nitriding at 500 °C with nitrogen for 30 min, then started vacuuming. The samples were heated at 950 °C for 30 min, and finally annealed at 500 °C for 30 min. The semi-finished nitride tube was drawn into nitride iron tubes of desired sizes (Φ1.6 mm, wall thickness 0.11 mm).
The finished nitride-iron tube was laser-cut into multiple stents. All the stents were polished to accurate dimensions. A nitride-iron stent was eletroplated with a pure zinc layer with 600 nm thickness. We then used a Sono-Tek system (2012 Route 9W, Milton, N.Y. 12547 USA) to spray a solution of PLA (Evonik Industries, Germany) on the surface of stent. The injection flow rate of spraying was 0.05 mL/min, and the rotation speed of the stent was 500 rpm/s. The ethyl acetate solution was used to dissolve PLA and sirolimus.
To maintain sample consistency, all LBS stents used in in vitro and in vivo experiments were EO sterilized prior to characterization.
Characterization of nitrogen content and PLA coating
Nitrogen content was measured with an ONH analyzer (ONH-2000, ELTRA Inc., Germany). Nitrogen-permeable semi-finished iron pipe (500 mg) was used to determine the nitrogen content of the stent (wt. %).
The PLA coating thickness was measured by spectroscopic reflectometry with a 3D optical profilometer (Q six, Sensofar Medical, Spain).
Mechanical measurements
The tensile strength of the finished iron tube of 100 mm was measured with a universal test machine (C43.504, MTS Inc., USA) at room temperature. The measurement standard follows ASTM E8.
A radial strength tester (RX550-100, Machine Solution Inc., USA) was applied to detect the radial force of LBS with a 0.1 mm/s of compression rate. The strength at 10% compression of the outer diameter of the initial stent was defined as the radial strength in units of kilopascal. The measurement standard follows ASTM 3067-14.
Crush resistance was evaluated by compression between two parallel plates perpendicular to the longitudinal axis of the stent following ISO 25539-1. The measurement was done in an electromechanical universal testing machine (C43.504, MTS, USA) with a 0.1 mm/s of compression rate. The force per unit length at 50% compression of outer diameter of the original stent was defined as crush resistance in units of N/mm according to ISO 25539-1.
We also determined local compression resistance (CR), which is important to deal with the case of calcified plaque. As such, we implanted the stent with nominal pressure into a mock vessel (inner diameter 2.7 ± 0.2 mm, radial compliance 5-7% per 100 mmHg@72 bpm, Dynatec Labs, Inc., Galena, MO, USA) with a simulated plaque and record the resist distance. The height, width and length of the simulated plaque in the experiment read 6.8 mm, 2.8 mm and 1.7 mm, respectively. CR is defined as
Here, d presents the diameter of the LBS under a simulated plaque, and D represents the diameter of the normally expanded stent. The measurement standard follows ISO 25539-1.
Animal models and stent implantation
The preclinical study was approved by the Ethics Committee of Shenzhen Advanced Medical Services Corporation in China. Small animals were used to evaluate the in vivo drug release and individual content degradation profile of the LBS. New Zealand rabbits of an average weight of 2.5 kg ranging from 1.9 to 3.2 kg experienced a standard diet without cholesterol or lipid supplements. The implantation sites were abdominal aorta and iliac arteries. We first punctured the right femoral artery of the rabbit and introduced a 5F guide catheter over a 0.014-inch guidewire. Then, a Φ3 × 8 mm LBS was introduced and positioned in the vessel segments avoiding the main branch of aorta under the fluoroscopic control. The stent was deployed under 8–10 inflation pressure at a target balloon to artery ratio of 1.1∼1.2 to 1.0 over 30 s. Then we deflated the balloon, withdrew the guidewire, and sutured the puncture site.
Large animals were used to evaluate the operability, safety and effectiveness of the BTK stent. Labrador dogs were chosen with weight between 20-35 kg. The preclinical study of LBS was made in canine BTK arteries. The control device was Xience Prime™ stents (Abbott Vascular, Santa Clara, CA, USA), which has obtained CE mark for additional infrapopliteal indication. Imaging of infrapopliteal artery OCT (C7 XR Fourier-Domain System, Light Lab Imaging, Westford, Massachusetts) was performed before and after implantation, at 1, 3, and 6 months follow ups.
The recovery of a damaged vessel lasts usually for 3-6 months, and later stenting may no longer profit the recover vessel but cage it. Additionally, 3-6 months is a crucial period, because majority of the drug sirolimus was released in 3 months and LBS started to degrade significantly. Hence, we set follow ups of the LBS at 1 month, 3 months and 6 months. Our follow ups to 6 months well evaluated the capability of our LBS to provide a sufficient support to the vessel and meanwhile evaluated the potential risk along with biodegradation.
Qualitative characterization of in vivo degradation of LBS through micro-CT analysis
We implanted LBSs into rabbit iliac arteries. At given follow-up periods, animals were sacrificed, and the stented artery segments were dissected. We then scanned the stents with vessel tissues through high-resolution micro-CT (Skyscan1172, Bruker, Germany) to acquire images and conducted 3D reconstruction to analyze the degradation extent of the LBS.
Quantitative characterization of in vivo material degradation and drug release of nitrided iron, Zn, PLA, and sirolimus in LBS
At given follow up periods, rabbits were sacrificed and the stented artery segments were dissected. We quantified the in vivo degradation of LBS via atomic absorption spectroscopy and the mass loss method. The stents were carefully separated from the vessel tissues and dissolved through microwave nitrification. The Zn concentration in the tissues was determined with an atomic absorption spectroscope (AA240FS, Agilent, USA).
We first used tweezers to remove the vessel tissues, and then immersed the stents in ethyl acetate (CH3COOC2H5) under ultrasound for 20 min to separate the PLA coating from the matrix. The PLA-CH3COOC2H5 solution was used to identify MW of the polymer via gel permeation chromatography coupled with multiangle laser light scattering (GPC-MALLS) combined with the molecular weight testing system of Wyatt Company. The test system included a liquid phase pump and injector from Agilent Company, an Agilent PL MIXED-C GPC column (Agilent, United States of American), a multi-angle laser light scattering instrument and a differential detector (Wyatt Corporation of America). The mobile phase during testing was tetrahydrofuran; the pump flow rate was set as 1 mL/min; the injection volume was 100 μL. The GPC data were processed using the software ASTRA 6.1.
The stents were immersed in tartaric acid (3 wt. %) under ultrasound for 20 minutes to remove the biodegradation products. The remaining stent struts were cleaned with NaOH, deionized water, and absolute ethyl alcohol, in sequence. Then we weighed the dried metal and calculated the biodegradation rate via the mass loss method.
After removing the tissues, we also immersed the LBS into a bottom of acetonitrile to quantify the drug content. The drug-eluted LBS was ultrasonically treated for 20 minutes to extract the residual sirolimus, which was further measured with high-performance liquid chromatography using Agilent 1260 with C18 column and a flow rate of 1 mL/min at room temperature. Sirolimus was analyzed at 278 nm with the mixture of acetonitrile and purified water (65:35 v/v) as the mobile phase. The cumulative drug release of each LBS was calculated from the residual drug amount on the LBS over the initial total drug amount.
Histological analysis
Samples fixed with 10% formalin for 48 hours were trimmed to remove excess tissues and rinsed with running water for over 10 minutes, followed by gradient dehydration with alcohol at concentration of 70%, 80%, 90% and 100%. The samples then underwent vitrification with xylol and were placed into a glass tube containing a proper amount of solution I (60 mL methyl methacrylate, 35 mL methyl butyl acrylate, 4.5 mL methyl benzoate, and 0.5 mL poly(glycolic diol) per 100 mL), vacuumed for 1 hour, and soaked for 2–3 d at 4 °C to make the polymer solution fully penetrate into deep tissues and to remove the gas in the tissue and polymer solution. After that, the samples were transferred to the polymer solution II (100 ml polymer solution I + 0.4 g/100 ml benzoyl peroxide) to have samples impregnated and were then placed in solution III (100 mL solution II + 150 µL N, N-dimethyl-p-toluidine and 150 µL decane-1-thiol), vacuumed for 1 hour, and preserved at 4 °C till solidification. The glass tube was broken to take out the embedded specimen, which was then sectioned with the precise cutting machine (BUEHLER Lsomet5000) into about 150 μm thickness, and was ground into slices of 10–20 μm thickness with the polish-grinding machine (BUEHLER Ecomet250). The slices were stained with hematoxylin and eosin (H&E) prior to optical observations. The local tissue response and the biodegradation products were observed with an optical microscope (DM2500, Leica, Germany).
FIM implantation
The FIM study of the LBS implantation for infrapopliteal lesions was approved by the Institutional Review Board of Chinese PLA General Hospital with approval number S2020-184-01. All procedures in this article were performed at the First Medical Center of Chinese PLA General Hospital (Beijing, China). Patients received dual antiplatelet therapy (100 mg aspirin and 75 mg clopidogrel once daily) for at least 3 days in advance. During the procedures, 5000 IU (50 IU/kg) of unfractionated heparin was administrated after 6 French sheath was placed. Written informed consent was obtained from all of patients. An 80-year-old man presented with left foot rest pain was first enrolled in this study. The target lesion in the first case was TPT of the left leg. The lesion was pre-dilated by plain old balloon angioplasty (Φ2 × 40 mm), and then LBS (Φ3 × 38 mm) was implanted to cover the lesion.
In the second case, the targeted lesion was situated in the PTA of the left lower extremity. A balloon catheter with dimensions Φ2 × 80 mm was deployed for pre-dilatory measures, followed by the implantation of LBS (Φ2.75 × 78 mm). In the third case, the lesion was localized in the left PA. A pre-dilation procedure employed a Φ2.5 × 60 mm balloon catheter, and subsequently, an LBS (Φ2.75 × 58 mm) was implanted. Both interventions serve to augment the cumulative evidence regarding the operability and effectiveness of the LBS technology in the management of lower extremity arterial occlusions.
Prior to stent implantation, peripheral arterial assessments were conducted via CT imaging systems (GE Company, USA). Digital subtraction angiography based on X-ray imaging (Angiostar, Siemens, Germany) was performed both pre- and post-implantation to evaluate vascular patency. Follow-up ultrasonography evaluations were carried out using an EPIQ 7 system (Philips, Netherlands) at immediate post-procedure intervals, and then at 6- or 13-month time point. Subsequent to the interventional procedures, patients were prescribed a daily regimen of 100 mg aspirin and 75 mg clopidogrel, to be maintained for a duration of 6- or 13-month. These comprehensive diagnostic and therapeutic protocols serve to reinforce the evidentiary basis for the effectiveness and safety of the LBS technology in the treatment of PAD.
Statistical analysis
Minitab 17 software was used for data analysis. Results are expressed as mean ± standard deviation. The experimental data were examined first for normality using the Anderson-Darling test; then, Student’s t-test was applied to evaluate the extent of stent restenosis, and p < 0.05 was considered statistically significant.
The percent luminal area stenosis in the canine BTK artery was defined as the ratio of the lumen area at the follow-up time to the reference stent area at the same time. A total of 15 dogs were implanted with 15 LBS (Φ2.5 × 18 mm/Φ2.5 × 8 mm) and 15 Xience Prime (Φ2.5 × 18 mm/Φ2.25 × 8 mm) and divided into three groups. In each group, 5 dogs were chosen for analysis, and the sample size was set considering that animals for histological analysis should contain at least 3-4 individuals. Every dog received one LBS and one Xience in each of the two hind legs and followed up by X-ray imaging & OCT immediately after implantation. Five dogs followed up at 1 month, 3 months, and 6 months.
We carried out in vivo degradation of LBS in rabbit abdominal aorta/iliac model. Since the drug content of a single LBS was too small to detect, we combined the stents collected from each rabbit as one sample. The mass loss of The PLA coating, nitrided-iron, zinc and sirolimus were analyzed by pooled date collecting from follow-up date. We denote the number of animals as N and the number of stents for each group as n. In tests of the mass loss of the PLA coating, we examined 3 months (N = 3, n = 9), 6 months (N = 3, n = 9), 12 months (N = 1, n = 3), and 18 months (N = 1, n = 3) after implantation of the stents; in tests of mass loss of the Zn sacrificial layer, we examined 1 month (N = 10, n = 11), 2 months (N = 10, n = 11), and 3 months (N = 7, n = 11); in test of mass loss of the nitride Fe, we examined 2 months (N = 9, n = 11), 3 months (N = 7, n = 11), 6 months (N = 9, n = 11), 9 months (N = 6, n = 11), 12 months (N = 9, n = 11), and 24 months (N = 7, n = 11); in tests of release of the sirolimus, we examined 7 days (N = 3, n = 6), 14 days (N = 3, n = 6), 1 month (N = 3, n = 6), 2 months (N = 3, n = 6), 3 months (N = 3, n = 6), 6 months (N = 5, n = 10), and 12 months (N = 1, n = 2).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The main data supporting the results of this study are available within the paper and its Supplementary Information. Any additional requests for information can be directed to, and will be fulfilled by, the corresponding authors. Source data are provided with this paper.
References
Uccioli, L. et al. Critical limb ischemia: current challenges and future prospects. Vasc. Health Risk. Manag. 14, 63–74 (2018).
Conte, M. S. et al. The GVG Writing Group, Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur. J. Vasc. Endovasc. Surg. 58, S1–S109 (2019).
Gerhard-Herman, M. D. et al. AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 69, 1465–1508 (2017).
Matsuoka, E. K. et al. Comparative performance analysis of interventional devices for the treatment of ischemic disease in below-the-knee lesions: a systematic review and meta-analysis. Circ. Cardiovasc. Interv. 37, 145–157 (2022).
Serruys, P. W. et al. M. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. N. Eng. J. Med. 331, 489–495 (1994).
Kereiakes, D. J., Onuma, Y., Serruys, P. W. & Stone, G. W. Bioresorbable vascular scaffolds for coronary revascularization. Circulation 134, 168–182 (2016).
Sharma, U. et al. The development of bioresorbable composite polymeric implants with high mechanical strength. Nat. Mater. 17, 96–103 (2018).
Hu, S. et al. Exosome-eluting stents for vascular healing after ischaemic injury. Nat. Biomed. Eng. 5, 1174–1188 (2021).
Borhani, S., Hassanajili, S., Hossein, S., Tafti, A. & Rabbani, S. Cardiovascular stents: overview, evolution, and next generation. Prog. Biomater. 7, 175–205 (2018).
Hiramoto, J. S., Teraa, M., de Borst, G. J. & Conte, M. S. Interventions for lower extremity peripheral artery disease. Nat. Rev. Cardiol. 15, 332–350 (2018).
Spreen, M. I. et al. Long-term follow-up of the PADI trial: Percutaneous transluminal angioplasty versus drug-eluting stents for infrapopliteal lesions in critical limb ischemia. J. Am. Heart Assoc. 6, e004877 (2017).
Varcoe, R. L. et al. Drug-Eluting Resorbable scaffold versus angioplasty for infrapopliteal artery disease. N. Engl. J. Med. 390, 9–19 (2024).
Iglesias, J. F. et al. Long-term outcomes with biodegradable polymer sirolimus-eluting stents versus durable polymer everolimus-eluting stents in ST-segment elevation myocardial infarction: 5-year follow-up of the BIOSTEMI randomised superiority trial. Lancet 402, 1979–1990 (2023).
Gray, B. H., Diaz-Sandoval, L. J., Dieter, R. S., Jaff, M. R. & White, C. J. SCAI expert consensus statement for infrapopliteal arterial intervention appropriate use. Catheter. Cardiovasc. Interv. 84, 539–545 (2014).
Konstantinos, K., Dimitris, K., Athanasios, D., Stavros, S. & Dimitris, S. Cost-effectiveness analysis of infrapopliteal drug-eluting stents. Cardiovasc. Interv. Radiol. 36, 90–97 (2012).
Varcoe, R. L., Paravastu, S. C., Thomas, S. D. & Bennett, M. H. The use of drug-eluting stents in infrapopliteal arteries: An updated systematic review and meta-analysis of randomized trials. Int. Angiol. 38, 121–135 (2019).
Jinnouchi, H. et al. Fully bioresorbable vascular scaffolds: lessons learned and future directions. Nat. Rev. Cardiol. 16, 286–304 (2019).
Dia, A. R. et al. Two-year follow-up of bioresorbable vascular scaffolds in severe infra-popliteal arterial disease. Vascular 29, 355–362 (2020).
Bowen, P. K. et al. Biodegradable metals for cardiovascular stents: from clinical concerns to recent Zn-alloys. Adv. Healthc. Mater. 5, 1121–1140 (2016).
Ryu, H., Seo, M.-H. & Rogers, J. A. Bioresorbable metals for biomedical applications: from mechanical components to electronic devices. Adv. Healthc. Mater. 10, e2002236 (2021).
Bosiers, M. et al. AMS INSIGHT-absorbable metal stent implantation for treatment of below-the-knee critical limb ischemia: 6-month analysis. Cardiovasc. Interv. Radiol. 32, 424–435 (2009).
Ozaki, Y., Garcia-Garcia, H. M., Shlofmitz, E., Hideo-Kajita, A. & Waksman, R. Second-Generation Drug-eluting resorbable magnesium scaffold: Review of the clinical evidence. Cardiovasc. Revasc. Med. 21, 127–136 (2020).
Yang, H. et al. Evolution of the degradation mechanism of pure zinc stent in the one-year study of rabbit abdominal aorta model. Biomaterials 145, 92–105 (2017).
Zheng, J. et al. Preclinical evaluation of a novel sirolimus-eluting iron bioresorbable coronary scaffold in porcine coronary artery at 6 months. JACC Cardiovasc. Interv. 12, 245–255 (2019).
Shen, D. et al. PLA-Zn-nitrided Fe bioresorbable scaffold with 53-μm-thick metallic struts and tunable multistage biodegradation function. Sci. Adv. 7, eabf0614 (2021).
Lin, W. et al. In vivo degradation and endothelialization of an iron bioresorbable scaffold. Bioact. Mater. 6, 1028–1039 (2021).
Zhang, H. et al. A biodegradable metal-polymer composite stent safe and effective on physiological and serum-containing biomimetic conditions. Adv. Healthc. Mater. 11, 2201740 (2022).
Sun, G. et al. A novel iron-bioresorbable sirolimus-eluting scaffold device for infrapopliteal artery disease. Circ. Cardiovasc. Interv. 15, e57–e59 (2022).
Qi, Y. et al. Strategy of metal-polymer composite stent to accelerate biodegradation of iron-based biomaterials. ACS Appl. Mater. Interfaces 10, 182–192 (2018).
Qi, Y., Li, X., He, Y., Zhang, D. & Ding, J. Mechanism of acceleration of iron corrosion by a polylactide coating. ACS Appl. Mater. Interfaces 11, 202–218 (2019).
Li, X. et al. Long-term efficacy of biodegradable metal-polymer composite stents after the first and the second implantations into porcine coronary arteries. ACS Appl. Mater. Interfaces 12, 15703–15715 (2020).
Lee, H.-W., Kim, K.-C. & Lee, J. Review of maglev train technologies. IEEE Trans. Magn. 42, 1917–1925 (2006).
Oberhauser, J. P., Hossainy, S. & Rapoza, R. J. Design principles and performance of bioresorbable polymeric vascular scaffolds. EuroInter 5, F15–F22 (2009).
Lambert, B. J., Mendelson, T. A. & Craven, M. D. Radiation and ethylene oxide terminal sterilization experiences with drug eluting stent products. AAPS PharmSciTech. 12, 1116–1126 (2011).
Samuels, O. B., Joseph, G. J., Lynn, M. J., Smith, H. A. & Chimowitz, M. I. A standardized method for measuring intracranial arterial stenosis. AJNR Am. J. Neuroradiol. 21, 643–646 (2000).
Shiono, Y. et al. Optical coherence tomography-derived anatomical criteria for functionally significant coronary stenosis assessed by fractional flow reserve. Circ. J. 76, 2218–2225 (2012).
Ali, Z. A. et al. 2-year outcomes with the absorb bioresorbable scaffold for treatment of coronary artery disease: a systematic review and metaanalysis of seven randomised trials with an individual patient data substudy. Lancet 390, 760–772 (2017).
Shen, Y. et al. Surface modification to enhance cell migration on biomaterials and its combination with 3D structural design of occluders to improve interventional treatment of heart diseases. Biomaterials 279, 121208 (2021).
Wang, L. et al. Rapid and ultrasensitive electromechanical detection of ions, biomolecules and SARS-CoV-2 RNA in unamplified samples. Nat. Biomed. Eng. 6, 276–285 (2022).
Wang, G. et al. Research and clinical translation of trilayer stent-graft of expanded polytetrafluoroethylene for interventional treatment of aortic dissection. Regen. Biomater. 9, rbac049 (2022).
Maselli, D. et al. Porcine organotypic epicardial slice protocol: A tool for the study of epicardium in cardiovascular research. Front. Cardiovasc. Med. 9, 920013 (2022).
Huang, J. et al. Identification of top-performance antimicrobial peptides from whole combinatorial libraries via a sequential model ensemble machine learning pipeline. Nat. Biomed. Eng. 7, 797–810 (2023).
Kwon, K. et al. A battery-less wireless implant for the continuous monitoring of vascular pressure, flow rate and temperature. Nat. Biomed. Eng. 7, 1215–1228 (2023).
Cao, D. & Ding, J. Recent Advances in regenerative biomaterials. Regen. Biomater. 9, rbac098 (2022).
Choi, Y. S. et al. Stretchable, dynamic covalent polymers for soft, long-lived bioresorbable electronic stimulators designed to facilitate neuromuscular regeneration. Nat. Commun. 11, 5990 (2020).
Liu, A. P. et al. The living interface between synthetic biology and biomaterial design. Nat. Mater. 21, 390–397 (2022).
Kolandaivelu, K. et al. Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings. Circulation 123, 1400–1409 (2011).
Lin, W. et al. Long-term in vivo corrosion behavior, biocompatibility and bioresorption mechanism of a bioresorbable nitrided iron scaffold. Acta Biomater. 54, 454–468 (2017).
Peuster, M. et al. A. novel approach to temporary stenting: degradable cardiovascular stents produced from corrodible metal results 6-18 months after implantation into new zealand white rabbits. Heart 86, 563–569 (2001).
Whitman, G. W., Russell, R. P. & Altieri, V. J. Effect of hydrogen-ion concentration on the submerged corrosion of steel. Ind. Eng. Chem. 16, 665–670 (1924).
Wu, L. & Ding, J. In vitro degradation of three-dimensional porous poly (D, L-lactide-co-glycolide) scaffolds for tissue engineering. Biomaterials 25, 5821–5830 (2004).
Zheng, J. et al. Long-term safety and absorption assessment of a novel bioresorbable nitrided iron scaffold in porcine coronary artery. Bioact. Mater. 17, 496–505 (2022).
Gao, Y. N. et al. Long-term efficacy, safety and biocompatibility of a novel sirolimus eluting iron bioresorbable scaffold in a porcine model. Bioact. Mater. 39, 135–146 (2024).
Gao, R. L. et al. First-in-human evaluation of a novel ultrathin sirolimus-eluting iron bioresorbable scaffold: 3-year outcomes of the IBS-FIM trial. EuroInter 19, 222–231 (2023).
Van Overhagen, H. et al. J. A. Primary results of the SAVAL randomized trial of a paclitaxel-eluting nitinol stent versus percutaneous transluminal angioplasty in infrapopliteal arteries. Vasc. Med. 28, 571–580 (2023).
Siablis, D., Kitrou, P. M., Spiliopoulos, S., Katsanos, K. & Karnabatidis, D. Paclitaxel-coated balloon angioplasty versus drug-eluting stenting for the treatment of infrapopliteal long-segment arterial occlusive disease: the IDEAS randomized controlled trial. JACC Cardiovasc. Inter. 7, 1048–1056, (2014).
Acknowledgements
This study was supported by National Natural Science Foundation of China (grant No. 52130302), and National Key R&D Program of China (grants number 2016YFC1100300 and 2023YFC2410300).
Author information
Authors and Affiliations
Contributions
J.D., W.G. and D.Z. conceived the concept. J.D., W.G., D.Z. and W.Z. designed the experiments. W.Z., X.G., H.Z, G.S, G.Z., X.L. and H.Q. did most of the experiments and collected most of data. J.D., W.G., D.Z., and W.Z. carried out most of data analysis. All of the authors (W.Z., X.G., H.Z., G.S., G.Z., X.L., H.Q., J.G., L.Q., D.S., X.S., H.L., D.Z., W.G., and J.D.) partially joined in pertinent experiments and manuscript writing. J.D., W.Z. and X.G. prepared the manuscript with devotion from all co-authors.
Corresponding authors
Ethics declarations
Competing interests
It is declared that W.Z., X.G., G.Z., H.Q., L.Q., X.S., H.L. and D.Z., are employees of Biotyx Medical (Shenzhen) Co., Ltd. The other authors declare no conflict of interest.
Peer review
Peer review information
Nature Communications thanks Eoin O’Cearbhaill and Tre Welch for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, W., Gao, X., Zhang, H. et al. Maglev-fabricated long and biodegradable stent for interventional treatment of peripheral vessels. Nat Commun 15, 7903 (2024). https://doi.org/10.1038/s41467-024-52288-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-52288-4
- Springer Nature Limited