Abstract
Measurement of flow-mediated vasodilation (FMD) in the brachial artery by using ultrasound is a well-established technique for evaluating endothelial function. To make the measurement quicker and simpler than the measurements of conventional ultrasound FMD (uFMD), we have developed a new noninvasive method, plethysmographic FMD (pFMD), to assess vascular response to reactive hyperemia in the brachial artery. The aim of this study was to determine the accuracy of measurement of pFMD in comparison to that of measurement of conventional uFMD. This study was a multi-center, cross-sectional study. We compared pFMD by a new device using cuff pressure and volume with conventional uFMD using ultrasound in 50 men (mean age, 41 ± 9 years). pFMD significantly correlated with conventional uFMD (β = 0.59, P < 0.001). In Bland–Altman plot analysis of pFMD and conventional uFMD, the mean difference of pFMD and conventional uFMD was 0.78%, and limits of agreement (mean difference ±2 standard deviations of the difference) ranged from −4.53% to 6.11%. We demonstrated validity of the new method for measurement of pFMD, which can automate the evaluation of endothelial function in a short time. Measurement of pFMD is simpler than measurement of conventional uFMD and may have reduced artificial bias compared to that of conventional uFMD measurement (URL for Clinical Trial: https://ethics.hiroshima-u.ac.jp/site/wp-content/uploads/2022/12/eki_giji20221213.pdf. Registration Number for Clinical Trial: E2022-0131).

Similar content being viewed by others
Introduction
Endothelial dysfunction serves as an early stage in the development of atherosclerosis, ultimately leading to cardiovascular events [1, 2]. Endothelial function is assessed using strain-gauge plethysmography, in which a nitric oxide (NO) agonist or an NO antagonist such as acetylcholine, methacholine or bradykinin is intravascularly administered and subsequent blood flow in the forearm arteries is measured [3,4,5,6]. This method is regarded as the gold standard for evaluating endothelial function because it can yield specific insights into basal and stimulated NO release. However, measurement by strain-gauge plethysmography is difficult for clinical practice because it is an invasive and time-consuming procedure. Noninvasive assessment of endothelial function by measurement of flow-mediated vasodilation (FMD) in the brachial artery using ultrasound has been widely recognized and accepted in clinical practice [7,8,9]. Assessment of endothelial function through FMD independently predicts future cardiovascular events [10,11,12,13]. Furthermore, several treatments, including pharmaceutical treatment and lifestyle changes, have shown efficacy in improving endothelial function as assessed by FMD [14,15,16,17,18]. However, assessing ultrasound FMD (uFMD) necessitates a 5-minute forearm ischemia in the supine position, a component of the conventional uFMD measurement method that typically takes at least 15 min and demands specialized skills for vessel diameter measurement using ultrasound.
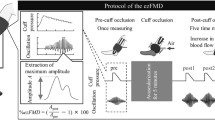
We have developed a new noninvasive method, plethysmographic FMD (pFMD), for assessing vascular response to reactive hyperemia in the brachial artery. This innovative approach relies on changes in vascular volume induced by ischemia, as measured through an automatic device using cuff pressure and volume. In this new method, a blood pressure cuff is placed around the upper arm and gradually deflated to 20 mmHg over a period of 30 s. The method of pFMD offers a less invasive and simpler means of assessing vascular function.
The aim of this study was to determine the accuracy of measurement of pFMD in comparison to that of measurement of conventional uFMD.
Methods
This study was a multi-center, cross-sectional study. A total of 51 men volunteers aged 25–60 years were recruited at two centers (Hiroshima University Hospital and Saraya Co.) between July 2022 and March 2023. One of the 51 subjects was excluded because of poor-quality images obtained by conventional uFMD measurement. pFMD was measurable in all subjects. Finally, 50 subjects were enrolled in this study. Hypertension was defined as systolic blood pressure equal to or exceeding 140 mm Hg and/or diastolic blood pressure equal to or exceeding 90 mm Hg measured at least three times in a seated position [19]. Diabetes mellitus was defined according to the American Diabetes Association recommendation [20]. Dyslipidemia was defined according to the third report of the National Cholesterol Education Program [21]. The estimated glomerular filtration rate was calculated using the Japanese estimated glomerular filtration rate equation [22]. Subjects fasted the previous night for at least 12 h. The subjects were kept in the supine position or the sitting position in a quiet, dark, air-conditioned room (constant temperature of 22–25 °C) throughout the study. A 23-gauge polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples. Thirty minutes after maintaining the supine position, conventional uFMD was measured, followed by measurement of pFMD at least one hour later. pFMD was measured 30 min after maintaining a sitting position. The observers were blind to the subjects’ clinical status. All methods followed the Declaration of Helsinki and relevant guidelines and regulations. The Ethics Review Board of Hiroshima University approved the study protocol (Registration Number for Clinical Trial: E2022-0131). All participants in this study provided written informed consent before their involvement.
Measurements of pFMD
The oscillometric method is often used for noninvasive blood pressure monitoring with a sphygmomanometer cuff tied around the upper arm. According to the theory, when the cuff pressure is equivalent to the arterial pressure, the arterial wall is assumed to be stress-free and the vessel experiences little distension [23, 24]. The cuff wave pressure is an indicator of the fluctuation in cuff pressure, which is caused by a change in the volume of the artery. The vascular response to reactive hyperemia in the brachial artery was assessed by cuff pressure variation and change in cuff volume of the pFMD. We assessed cuff pressure variation and change in cuff volume with a ViewWave (SARAYA, Osaka, Japan) (Supplementary Fig. 1). The cuff is inflated slowly to a level higher than 200 mmHg, and blood pressure is determined by analyzing oscillation signals obtained from the cuff pressure. This device requires a pre-set maximum cuff pressure. The maximum cuff pressure is set at 200 mmHg to achieve a systolic blood pressure of 50 mmHg or higher. We measured blood pressure in the upper arm in a resting sitting position during pressure elevation to 200 mmHg. The cuff pressure was maintained at 200 mmHg to cut off blood flow for 15 s, and then the cuff pressure was reduced to 20 mmHg for 30 s. Cuff pressure was maintained at 20 mmHg for 120 s, during which time changes in vascular volume were measured (Supplementary Fig. 2). In a preliminary study, there was a significant correlation between conventional uFMD, for which cuff pressure was maintained for 5 min, and short-time uFMD, for which cuff pressure was maintained for 40 s and then reduced for 30 s. Based on these results, pFMD also uses this protocol of reduced cuff pressure for 30 s. The cuff volume was measured based on the flow rate of gas supplied to and discharged from the cuff, as detected by the flow sensor. The cuff pressure-volume curve was used to create an approximate function F1 for the pressure-volume curve where the cuff pressure is higher than diastolic pressure (Supplementary Fig. 3). Arterial vessels are open when the cuff pressure is lower than diastolic pressure. Therefore, the pressure-volume curve will not approximate the approximate function F1 when the cuff pressure is lower than diastolic pressure. The difference between the cuff volume at the approximate function F1 when the cuff was 20 mmHg and the actual cuff volume at 20 mmHg is the volume that the arterial blood vessel opened, and this volume was defined as the baseline vessel volume. pFMD was calculated by the following equation: %pFMD = [(peak vessel volume − baseline vessel volume)/baseline vessel volume] × 1/2 × 100. The measurements were fully automated. Intra-coefficients were calculated from pFMD measured twice on different days under similar conditions, after 30 min while maintaining the sitting position. Intra-coefficients of variation for pFMD were 9.3% in our laboratory.
Measurements of conventional uFMD
Vascular response to reactive hyperemia in the brachial artery was used to assess endothelium-dependent conventional uFMD. A high-resolution linear artery transducer was coupled to computer-assisted analysis software (MISTPILOT, SARAYA Co, Osaka, Japan) that used an automated edge detection system for the measurement of brachial artery diameter [25]. A blood pressure cuff was placed around the forearm. The brachial artery was scanned longitudinally 5–10 cm above the elbow. When the clearest B-mode image of the anterior and posterior intimal interfaces between the lumen and vessel wall was obtained, the transducer was held at the same point throughout the scan by a special probe holder to ensure consistency of the image. Depth and gain settings were set to optimize the images of the arterial lumen wall interface. When the tracking gate was placed on the intima, the artery diameter was manually tracked, and the waveform of diameter changes over the cardiac cycle was displayed in real-time using the conventional uFMD mode of the tracking system. This allowed the ultrasound images to be optimized at the start of the scan and the transducer position to be adjusted immediately for optimal tracking performance throughout the scan. The baseline longitudinal image of the artery was acquired for 30 s, and then the blood pressure cuff was inflated to 50 mm Hg above systolic pressure for 5 min. The longitudinal image of the artery was recorded continuously until 3 min after cuff deflation. Changes in brachial artery diameter were immediately expressed as percentage changes relative to the vessel diameter before cuff inflation. Conventional uFMD was automatically calculated as the percentage change in peak vessel diameter from the baseline value. The percentage of conventional uFMD [(Peak diameter − Baseline diameter)/Baseline diameter] was used for analysis. Inter- and intra-coefficients of variation for the brachial artery diameter were 3.5% and 2.6%, respectively, in our laboratory.
Statistical analysis
Results are summarized as means ± SD for continuous variables and as percentages for categorical variables. Statistical significance was a probability value of <0.05. Relationships between variables were determined using Pearson’s correlation coefficients. Bland–Altman plot analysis was conducted to assess the level of agreement between pFMD and conventional uFMD [26]. To estimate the coefficient of correlation between pFMD and conventional uFMD, with a correlation coefficient equal to 0.4, it is necessary to sample size 47 subjects. The data were processed using JMP pro version 17 (SAS Institute. Cary, NC).
Results
The baseline clinical characteristics of the subjects are summarized in Table 1. Of the 50 subjects, eight (16.0%) had hypertension, eight (16.0%) had dyslipidemia, one (2.0%) had diabetes mellitus, and 11 (22.0%) were current smokers. The mean values were 5.2 ± 2.4% for conventional uFMD and 6.0 ± 2.9% for pFMD.
Relationships between pFMD and conventional uFMD
pFMD significantly correlated with conventional uFMD (β = 0.59, P < 0.001) (Fig. 1). In Bland–Altman plot analysis of pFMD and conventional uFMD, the mean difference between pFMD and conventional uFMD was 0.78%, and limits of agreement (mean difference ±2 standard deviations of the difference) ranged from −4.53% to 6.11% (Fig. 2).
Bland–Altman plot of conventional ultrasound flow-mediated vasodilation and plethysmographic flow-mediated vasodilation. The bold line represents the mean difference between conventional ultrasound flow-mediated vasodilation and plethysmographic flow-mediated vasodilation. The dotted lines represent the mean difference ±2 standard deviations of the differences
Discussion
The present study demonstrated that pFMD significantly correlated with conventional uFMD. Bland–Altman plot analysis showed a high level of concordance between pFMD and conventional uFMD. It is easier, more convenient, and more comfortable for the subjects to measure pFMD with a shorter cuff inflation time in the sitting position.
Measurement of pFMD has several advantages as outlined below. Measurement of pFMD is simpler than measurement of conventional uFMD since fully automated measurements can be performed in the same way as blood pressure measurement and it requires only a short time for cuff inflation. Measurement of conventional uFMD with an ultrasound system requires specialized skills, as the operator must accurately position the transducer to image the brachial artery and manually or automatically monitor changes in brachial artery diameter [7, 27,28,29]. Measurement of pFMD requires only the application of a cuff on the upper arm, similar to measuring blood pressure. In addition, pFMD is measured in 5 min, including a cuff inflation time of 45 s. In contrast, measurement of conventional uFMD requires at least 15 min, including a cuff inflation time of 5 min and time to place the transducer in the proper position before cuff inflation. An incremental reduction in pressure release from the cuff results in optimal shear stress on the arterial wall, leading to subsequent dilation of blood vessels depending on the endothelium, despite a brief period of reduced blood flow in the upper arm. Therefore, measurement of pFMD has the benefit of avoiding artificial bias, such as manipulation of the transducer and operation of the ultrasound system, thereby enhancing the operation effectiveness of the present invention and no inter-measurer variation.
This study has some limitations. First, the correlations between pFMD and cardiovascular risk factors were not established due to validation only in males with low cardiovascular risk profiles. Further studies are needed to assess the relationships of pFMD with cardiovascular risk factors and future cardiovascular disease. Second, a difference exists between pFMD and conventional uFMD regarding the scope of arterial assessment. pFMD evaluates volume alterations in the arteries over the whole of the upper arm, including the brachial artery and small vessels of the upper arm, while conventional uFMD focuses only on a single brachial artery, which is classified as a macrovasculature. The relationship between pFMD and conventional uFMD has been established via the conversion of volume changes to diameter. Therefore, pFMD mainly evaluates the macrovascular endothelial function, although pFMD includes the evaluation of volume alteration in the arteries over the whole of the upper arm. pFMD might provide a more representative assessment of vascular endothelial function by integrating the effects of several arteries in the upper arm. Third, while the recommendations for measurement of FMD suggest using the supine position for the measurement of FMD, the measurement of pFMD is carried out in the sitting position. pFMD in the sitting position significantly correlated with conventional uFMD in the supine position. In our previous study, we showed that measurement of FMD in both the supine and sitting positions is appropriate for evaluation of endothelial function in various populations, including those with cardiovascular diseases [30, 31]. These studies suggest that endothelial function in different body positions may not change. It is possible that the same correlation was observed in the present study. Future studies should verify whether there is a difference in pFMD results between different body positions. Fourth, it is technically difficult to change the maximum cuff pressure settings for each patient, the maximum cuff pressure is set at 200 mmHg. In the present study, subjects had systolic blood pressure under 150 mmHg. Therefore, maximum cuff pressure was at least 50 mmHg higher than systolic blood pressure in all subjects. It will be necessary to confirm the correlation between pFMD and conventional uFMD when the cuff pressure is 200 mmHg in hypertensive patients with systolic blood pressure greater than 150 mmHg. Fifth, measurements of pFMD and conventional uFMD were performed on the same day. Therefore, we cannot deny the possibility that the vasodilation during the first uFMD measurement affected the results of the next pFMD measurement. However, Inaba et al. [32] have shown that uFMD fully recovered after 60 min following the initial uFMD. This result indicates that one hour is a sufficient interval for continuous FMD measurement. In the present study, at least one hour was allowed between the measurement of pFMD and that of conventional uFMD.
Conclusion
We demonstrated the validity of a new method for measurement of pFMD, which can automate the evaluation of endothelial function in a short time. Measurement of pFMD is simpler than measurement of conventional uFMD and may have reduced artificial bias compared to that of conventional uFMD measurement. In further research, we should determine whether pFMD is a reliable predictor of cardiovascular outcomes and whether measurements of pFMD differ from measurements of conventional uFMD with respect to predicting cardiovascular outcomes.
Data availability
The data presented in this study are available on request from the corresponding author.
References
Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999;340:115–26.
Higashi Y, Noma K, Yoshizumi M, Kihara Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ J. 2009;73:411–8.
Panza JA, Quyyumi AA, Brush JE Jr., Epstein SE. Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension. N Engl J Med. 1990;323:22–7.
Gilligan DM, Sack MN, Guetta V, Casino PR, Quyyumi AA, Rader DJ, et al. Effect of antioxidant vitamins on low density lipoprotein oxidation and impaired endothelium-dependent vasodilation in patients with hypercholesterolemia. J Am Coll Cardiol. 1994;24:1611–7.
Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Oshima T, Chayama K. Endothelial function and oxidative stress in renovascular hypertension. N Engl J Med. 2002;346:1954–62.
Creager MA, Cooke JP, Mendelsohn ME, Gallagher SJ, Coleman SM, Loscalzo J, et al. Impaired vasodilation of forearm resistance vessels in hypercholesterolemic humans. J Clin Investig. 1990;86:228–34.
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002;39:257–65.
Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–5.
Anderson TJ, Elstein E, Haber H, Charbonneau F. Comparative study of ACE-inhibition, angiotensin II antagonism, and calcium channel blockade on flow-mediated vasodilation in patients with coronary disease (BANFF study). J Am Coll Cardiol. 2000;35:60–6.
Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, et al. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation. 2009;120:502–9.
Rossi R, Nuzzo A, Origliani G, Modena MG. Prognostic role of flow-mediated dilation and cardiac risk factors in post-menopausal women. J Am Coll Cardiol. 2008;51:997–1002.
Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr., et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation. 2004;109:613–9.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Endothelial Dysfunction, Increased Arterial Stiffness, and Cardiovascular Risk Prediction in Patients With Coronary Artery Disease: FMD-J (Flow-Mediated Dilation Japan) Study A. J Am Heart Assoc. 2018;7:e008588.
Wolfrum S, Jensen KS, Liao JK. Endothelium-dependent effects of statins. Arteriosclerosis Thrombosis Vasc Biol. 2003;23:729–36.
Ghiadoni L, Virdis A, Magagna A, Taddei S, Salvetti A. Effect of the angiotensin II type 1 receptor blocker candesartan on endothelial function in patients with essential hypertension. Hypertension. 2000;35:501–6.
Kishimoto S, Oki K, Maruhashi T, Kajikawa M, Hashimoto H, Takaeko Y, et al. A Comparison of Adrenalectomy and Eplerenone on Vascular Function in Patients with Aldosterone-producing Adenoma. J Clin Endocrinol Metabol. 2020;105:dgaa561.
Kishimoto S, Oki K, Maruhashi T, Kajikawa M, Matsui S, Hashimoto H, et al. Eplerenone improves endothelial function and arterial stiffness and inhibits Rho-associated kinase activity in patients with idiopathic hyperaldosteronism: a pilot study. J Hypertens. 2019;37:1083–95.
Goto C, Higashi Y, Kimura M, Noma K, Hara K, Nakagawa K, et al. Effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation. 2003;108:530–5.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
American Diabetes Association: clinical practice recommendations 1999. Diabetes Care. 1999;22:S1–114.
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Posey JA, Geddes LA, Williams H, Moore AG. The meaning of the point of maximum oscillations in cuff pressure in the indirect measurement of blood pressure. 1. Cardiovasc Res Cent Bull. 1969;8:15–25.
Drzewiecki G, Hood R, Apple H. Theory of the oscillometric maximum and the systolic and diastolic detection ratios. Ann Biomed Eng. 1994;22:88–96.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arteriosclerosis Thrombosis Vasc Biol. 2013;33:1401–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Thijssen DHJ, Bruno RM, van Mil A, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019;40:2534–47.
Flammer AJ, Anderson T, Celermajer DS, Creager MA, Deanfield J, Ganz P, et al. The assessment of endothelial function: from research into clinical practice. Circulation. 2012;126:753–67.
Alexander Y, Osto E, Schmidt-Trucksäss A, Shechter M, Trifunovic D, Duncker DJ, et al. Endothelial function in cardiovascular medicine: a consensus paper of the European Society of Cardiology Working Groups on Atherosclerosis and Vascular Biology, Aorta and Peripheral Vascular Diseases, Coronary Pathophysiology and Microcirculation, and Thrombosis. Cardiovasc Res. 2021;117:29–42.
Soga J, Nishioka K, Nakamura S, Umemura T, Jitsuiki D, Hidaka T, et al. Measurement of flow-mediated vasodilation of the brachial artery: a comparison of measurements in the seated and supine positions. Circ J. 2007;71:736–40.
Higashi Y. Assessment of Atherosclerosis - Vascular Imaging Tests and Vascular Function Tests. Circ J. 2017;81:304–5.
Inaba H, Takeshita K, Uchida Y, Hayashi M, Okumura T, Hirashiki A, et al. Recovery of flow-mediated vasodilatation after repetitive measurements is involved in early vascular impairment: comparison with indices of vascular tone. PloS One. 2014;9:e83977.
Acknowledgements
We thank Megumi Wakisaka, Ki-ichiro Kawano, and Satoko Michiyama for their excellent secretarial assistance.
Funding
This study was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898 to Higashi). Open Access funding provided by Hiroshima University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The Ethics Review Board of Hiroshima University approved the study protocol.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kishimoto, S., Hashimoto, Y., Maruhashi, T. et al. New device for assessment of endothelial function: plethysmographic flow-mediated vasodilation (pFMD). Hypertens Res (2024). https://doi.org/10.1038/s41440-024-01770-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41440-024-01770-z
- Springer Nature Singapore Pte Ltd.