Abstract
The aim of this study was to investigate the relationship between endothelin-1, nitric oxide, insulin resistance, and blood pressure in young subjects with a high prevalence of excess weight and/or elevated blood pressure. In a cohort of 238 children (mean age = 11.1 years), height, weight, waist circumference, and blood pressure were assessed. Body mass index, waist-to-height ratio, and blood pressure percentiles were calculated, and the children were classified as having excess weight and elevated blood pressure according to the International Obesity Task Force and the US blood pressure nomograms specific for gender, age and height, respectively. Endothelin-1 and nitric oxide production were assessed, and the homeostatic model assessment index was calculated. Forty-three percent of children were male, 71% had excess weight, and 37% had systolic and/or diastolic values above the ninetieth percentile. Plasma endothelin-1 and nitric oxide production were independently correlated (p < 0.05). In multivariate analyses, the HOMA index was associated with systolic and diastolic blood pressure (p = 0.01), and nitric oxide was independently related to diastolic blood pressure (p = 0.04), even after adjustment for measures of body composition. By using the waist-to-height ratio instead of BMI in the statistical model, the association between the homeostatic model assessment index and blood pressure was attenuated, while the results remained similar for nitric oxide. No correlation was found between endothelin-1 and blood pressure. In our study population, the correlation between nitric oxide and blood pressure and the lack of a relationship between endothelin-1 and blood pressure could be explained by an increase in the vasodilator effect of local and systemic nitric oxide, which counteracts the possible hypertensive effect of endothelin-1.
Similar content being viewed by others
Introduction
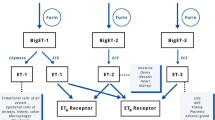
Among the three separately encoded isoforms constituting the endothelin superfamily, endothelin-1 (ET-1) is the dominant isoform in the cardiovascular system and is therefore the most often studied. ET-1 is synthesized predominantly in vascular endothelial cells, but it is also synthesized in vascular smooth muscle cells (VSMC) as well as in extravascular tissues such as the spleen, pancreas, lung, and nervous system, as well as in the glomerular and epithelial cells within the kidney [1,2,3,4].
In humans, the physiological action of ET-1 is mediated by ET-A and ET-B receptors. ET-1 contributes to a basal vasoconstrictor tone [5] that seems to be largely mediated by ET-A receptors [6]. In fact, the binding of ET-1 to ET-A and ET-B receptors in VSMCs results in vasoconstriction, whereas the predominant effect of ET-1 binding to ET-B receptors in the endothelium is an increase in nitric oxide (NO) and prostacyclin synthesis [7, 8]. The administration of ET-1 results in a biphasic response characterized by a transient depressor effect, followed by pronounced and persistent hypertension [6, 9]. It is noteworthy that the effects of ET-1 administration may not necessarily reproduce the effects of endogenous ET-1 since it is not presently clear whether endothelial ET-B receptors under physiological conditions “sense” quantities of ET-1 that are high enough to elicit vasodilation through a NO-dependent mechanism [10]. The nonunivocal behavior of the ET pathway underlies the differences between acute and chronic effects of ET-1 signaling and makes the study of this pathway particularly problematic.
In the presence of excess weight, the ET-1 system is increased; however, the mechanisms underlying this activation are unclear. Overweight (OW) and obesity (OB) are typically associated with hyperinsulinemia [11], and insulin has been shown to stimulate ET-1 production [12, 13]. Nevertheless, recent findings in humans have reported that hyperinsulinemia fails to augment ET-1 action in vivo [14]. It has been suggested that hyperinsulinemia interferes with the vasomotor balance in human skeletal muscle, favoring vasoconstrictive pathways, and eventually impairing arteriolar vasodilation [15]. While OW and OB have recently been described as being associated with the enhanced ET-1-mediated vasoconstriction that contributes to endothelial vasodilator dysfunction in adults [16], the balance of ET-1 and NO in children with excess weight has not been adequately investigated.
Nitric oxide is biosynthesized endogenously by various NO synthases (NOSs) from L-arginine, oxygen, and nicotinamide adenine nucleotide phosphate (NADPH). The reduction in inorganic nitrate may also lead to NO production. Through NO, the endothelium signals the surrounding smooth muscle to relax, thus resulting in vasodilation and increased blood flow. NO is highly reactive (having a half-life of a few seconds) but diffuses freely across membranes, making it an ideal transient paracrine (between adjacent cells) and autocrine (within a single cell) signaling molecule in the control of smooth muscle tone [17].
As natural counterparts in vascular function, ET-1 and NO are known to interact via both direct and indirect mechanisms [18, 19]. In fact, NO signaling in the systemic vasculature should be considered a vital component of ET-1 activity rather than a distinct pathway. While it is largely recognized that the function of NO is principally to maintain a tonic vasodilatory signal [20, 21], the mechanism by which NO inhibits ET-1-mediated vasoconstriction remains unknown. A contemporary hypothesis is that NO, under normal physiological conditions, inhibits ET-1 activity. In addition, it has been hypothesized that an important step in the progression of cardiovascular disease is the loss of endothelial-derived NO production resulting in increased ET-1 signaling [10]. It is becoming increasingly apparent that an imbalance between NO and ET-1 is important in numerous pathophysiological conditions, including hypertension and insulin resistance.
With the aim of better clarifying the relationship between ET-1, NO, insulin resistance, and blood pressure (BP) in a scenario in which irreversible vascular damage has not yet developed, we performed cross-sectional analyses on a study population of young subjects with a high prevalence of excess weight and/or elevated BP.
Methods
Study population
We studied a consecutive cohort of children referred by their primary care pediatricians to the Unit for Cardiovascular Risk Assessment in Children of the Istituto Auxologico Italiano, University of Milano-Bicocca, because of evidence of excess weight and/or elevated BP. None of the children were affected by impaired glucose tolerance, diabetes, or renal insufficiency. The specific diagnostic tests that were needed to rule out secondary hypertension were carried out in all children. Children with secondary forms of hypertension were excluded from the study. Informed consent was obtained from the children’s parents, and the local ethics committee approved the study protocol.
Anthropometric parameters and blood pressure
Height, weight, and waist circumference (WC) were measured. Weight was approximated to the nearest 100 grams, and height was approximated to the nearest 0.5 cm. Body mass index (BMI) was calculated as weight (kg)/height (m)2. Body mass index percentiles were calculated using the Centers for Disease and Control prevention charts available at http://www.cdc.gov/nchs/. Weight class was defined according to the International Obesity Task Force classification [22], distinguishing among normal weight (NW), OW, and OB classes. Waist circumference was measured to the nearest 0.5 cm by a nonelastic flexible tape while the child was in a standing position. The waist-to-height ratio (WtHr) was calculated by dividing WC by height. Blood pressure was measured while the child was in a seated position using an oscillometric device validated in children (Omron 705 IT) with the appropriate cuff for the child’s upper-arm size. Measurements were performed after at least 5 min of rest. Blood pressure was measured three times (at 1–2 min intervals), and systolic BP (SBP) and diastolic BP (DBP) percentiles were calculated according to the nomograms of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents [23]. The children were classified according to the mean of the three measurements as follows: normotensive (NT) if both SBP and DBP percentiles were below the ninetieth percentile; high normal (HN) if the SBP and/or DBP percentiles were at or above the ninetieth percentile but both SBP and DBP were below the ninety-fifth percentile; hypertensive (HT) if the SBP and/or DBP percentiles were at or above the ninety-fifth percentile. Children were stratified on the basis of the presence of excess weight (OW + OB) and/or elevated BP (HN + HT).
Pubertal stage was assessed by a medical examination, and children were classified into two categories: prepubertal and pubertal according to Tanner stage [24].
Biochemical parameters
At baseline, blood samples were taken after a 12-h fasting period for plasma glucose and insulin, ET-1, and NO assessment. Plasma glucose was measured by a glucose oxidase method, and insulin was evaluated by chemiluminescence immunometric assay. The HOMA index was calculated by dividing the product of plasma insulin (µU/ml) and plasma glucose (mmol/L) by 22.5 [25].
NO production was assessed in plasma samples using the Griess method [26]. The colorimetric Griess reaction for nitrite was used to determine the concentration of NO. Because the NO present in biological fluids is recovered in nitrate form, the plasma samples were treated with nitrate reductase (10 U/mL) and nicotinamide adenine dinucleotide phosphate oxidase (5 mM in Tris-Cl) for 3 h at room temperature to reduce nitrate to nitrite. Finally, the samples were mixed with an equal volume of freshly prepared Griess reagent (0.05% N-[1-naphthyl] ethylene diamine dihydrochloride and 0.5% sulfanilamide in 2.5% orthophosphoric acid) for 20 min. The absorbance of each sample was measured at 540 nm using a microplate reader (Victor3 1420 multilabelcounter, Perkin Elmer). Concentrations of NO in the samples were determined using a calibration curve generated with standard NaNO2 solutions (0.1–100 μM).
The ET-1 concentration in the plasma samples was detected by ELISA, which was carried out according to the manufacturer’s instructions (Clinisciences). Samples were measured in triplicate against known standards.
Statistical methods
Variables are reported as the mean (standard deviation). The differences among biochemical parameters in different subgroups of children (NT/NW, HN-HT/NW, NT/OW-OB, and HN-HT/OW-OB) were assessed by analysis of variance (ANOVA) and Fisher’s post hoc test. The associations among variables (age, puberty, ET-1, NO, HOMA index, BMI percentiles, SBP and DBP percentiles, WtHr) were assessed by simple and multiple regression analysis. A p-value <0.05 was considered significant.
Results
The anthropometric and clinical characteristics of the study population (n = 238) according to BP category and weight class are shown in Table 1. The mean age of the cohort was 11.1 (±2.4) years. Forty-three percent (n = 103) of children were male, and 54% (n = 128) of the children were pubertal. Seventy-one percent (n = 168) of the subjects had excess weight, and 58% (n = 137) had a WtHr greater than 0.5. The prevalence of BP values (SBP and/or DBP) above the ninetieth percentile was 37% (n = 88). Thirty-two percent of children (n = 76) had a family history of arterial hypertension (i.e., at least one hypertensive parent). The highest percentage of family history of hypertension was observed in the HT/NW subgroup, and the lowest was observed among the NT/NW children.
NO production did not differ among the four subgroups (NT/NW, HN-HT/NW, NT/OW-OB, and HN-HT/OW-OB). The endothelin-1 values were greater in children with excess weight (OW-OB) regardless of BP category (p < 0.05). The HOMA index progressively and significantly increased (p < 0.001) with increasing weight class and BP category (NT/NW vs HN-HT/NW p = NS; HN-HT/NW vs HT/OW-OB p < 0.001; NT/OW-OB vs HN-HT/OW-OB p = 0.034; NT/NW vs NT/OW-OB and vs HN-HT/OW-OB p < 0.001; HN-HT/NW vs HN-HT/OW-OB p < 0.001) (Fig. 1).
Determinants of NO and ET-1 plasma levels
In the univariate analysis, NO was slightly associated with age and puberty (p = 0.06 for both) and SBP percentile (p = 0.09) and significantly correlated with ET-1 and DBP percentile (p = 0.04 for both). There was a significant association between ET-1 and NO (p = 0.04), BMI percentile (p = 0.005) and WtHr (p = 0.02). The HOMA index was not related to NO or ET-1 values. The NO and ET-1 values were similar between children with and without a family history of arterial hypertension. A multiple regression model adjusted for age and puberty showed that the ET-1 and SBP percentiles were independently associated with NO levels. No variable was associated with NO when the DBP percentile was used in the statistical model instead of the SBP percentile (Table 2). Among all the variables studied in the multivariable analysis, the only variables that were independently associated with ET-1 values were NO and BMI percentile. The results did not change when the BMI percentile was replaced with WtHr (Table 3).
Determinants of SBP and DBP values
SBP and DBP percentiles were higher in children with excess weight than in NW children (p = 0.001, for SBP and p = 0.002, for DBP) and in subjects with a WtHr >0.5 (p = 0.015, for SBP and p = 0.014, for DBP). In the univariate analysis, the WtHr was strongly associated with BP (p < 0.001, for both SBP and DBP), and there was a significant correlation even between BMI percentile and BP values (p = 0.001, for SBP and p = 0.018, for DBP). Additionally, the HOMA index was significantly correlated with both SBP (p < 0.001) and DBP (p = 0.002).
When we investigated the determinants of BP percentiles with the multiple regression model, the HOMA index was associated with SBP and DBP values in the models adjusted for WtHr or BMI percentile. Nitric oxide was slightly correlated with SBP, while there was a significant association with DBP even when BMI was used in place of WtHr (Table 4, panels a and b, Model A and B). When NO was replaced by ET-1, the correlation between HOMA index and both SBP and DBP percentiles was confirmed in the model adjusted for BMI percentile (Table 4, panels c and d, Model B). By including the WtHr instead of BMI in the statistical model, the association between the HOMA index and the BP values was attenuated (Table 4, panels c and d, Model A).
Discussion
In our population, in which 70% of subjects were OW or obese and ~35% had elevated BP, NO levels were independently related to DBP, while no association was found between ET-1 and BP values. We observed a direct relationship between ET-1 and NO that might be the expression of their complex balance before the development of structural vascular modifications occurs. An increase in ET-1 was observed in children with excess weight. The HOMA index increased along with the BP category and weight class, and its relationship with BP values was independent of ET-1 and NO, even after adjustment for BMI, while it was weakened by the inclusion of central obesity in the model.
Endothelin-1/nitric oxide balance and blood pressure
ET-1 is involved in the regulation of vasoconstrictor tone and the pathogenesis of hypertension in humans [27]. It is possible that under normal physiological conditions, a fundamental role of NO in BP control is to deeply inhibit the vasoconstrictive actions of ET-1. However, under pathological conditions compromising NO bioavailability, the vasoconstrictor effects of ET-1 (and other potentially deleterious effects such as VSMC proliferation and migration) become disinhibited. This mechanism may lead to a form of hypertension with detrimental long-term effects on vascular structure and function, as described in adults [28].
In our sample, no relationship between ET-1 levels and BP values was found. In mice with one allele of the ET-1 gene deleted, BP values are slightly elevated compared to those of the controls, suggesting that ET-1 may play a role as a depressor rather than as a pressor in the physiological state [29]. In humans, some studies showed an increase in plasma ET-1 values in adult patients with hypertension [30,31,32], while other authors did not confirm these findings [33,34,35]. It has been shown that high ET-1 plasma levels are present mainly in HT patients with more advanced disease, in terms of target organ damage or higher BP values [36,37,38]. The transition condition, in which we believe the children in our study were, is also supported by data on 60 adolescents (5–6 years older than the children in our study sample), among whom, those with hypertension showed significantly higher levels of ET-1 and lower levels of NO than those with prehypertension [39]. It is possible that the lack of association between ET-1 and hypertension we observed in our sample might be due to the young age of the subjects and the absence of organ damage.
In general, laminar flow is associated with the upregulation of eNOS and NO production [40]. In small-for-gestational-age children with high BP and vascular resistance in the basal condition, Strambi et al. described that increased vascular response after ischemic stress at the brachial level leads to a greater decrease in BP and vascular resistance compared to that in control children [41]. These data support the hypothesis that, in children with increased BP values, the response induced by ischemic stress is greater than in that in NT subjects, suggesting that endothelial production of NO is chronically overstimulated in the early phases of hypertension. This pathophysiological condition may initially protect young organisms from the development of stable hypertension. In a second step, endothelial dysfunction due to the decrease in the synthesis and release of NO might favor early damage to the vascular wall.
In our study population, NO was significantly correlated with ET-1 and DBP percentile even after adjustment for measures of body composition; in contrast, no correlation was found between ET-1 and BP. Recent findings describe an inverse relationship between NO and ET-1 concentrations and show how endothelin imbalance seems to play a role in the development of hypertension and target organ damage in adolescents [42]. It is possible that in younger children without vascular structural damage, such as those included in our study, NO and ET-1 remain in a delicate balance, thereby maintaining the overall total peripheral resistance substantially unchanged.
As previously reported, our data show that central obesity is the strongest correlate of BP values in children [43, 44]. In both statistical models that take into account the role of NO or the role of ET-1 in the analyses of the predictors of SBP and DBP, the association between WtHr and both systolic and diastolic BP values is much stronger than the association with indexed BMI. It is interesting to note that the correlation between values of NO and BP percentiles was similar in the model adjusted for WtHr and in the one adjusted for BMI, indicating that NO may partially affect the blood pressure values regardless of the important role played by central obesity.
Endothelin-1 and excess weight
Although enhanced ET-1-mediated vasoconstriction has previously been demonstrated in obese adults with [45, 46] and without [16] comorbidities, this is the first study, to our knowledge, to demonstrate elevated ET-1 levels in OW or obese children, independent of BP levels or HT status (Fig. 1). The vasoconstrictor response to exogenous ET-1 has been found to be lower in OW and obese adults, suggesting that ET-1 bioavailability increases with increased adiposity [16]. Obese prepubertal children demonstrated higher flow-mediated dilation and lower arterial stiffness than their NW/NT counterparts [47]. The authors suggest the presence of an initial adaptive response, which ultimately, after a longer exposure to obesity, will fail and culminate in vascular damage.
The results of the present study significantly extend these previous findings by demonstrating that OW and OB are associated with elevated ET-1 levels and HOMA index but not with NO levels in children (Fig. 1, Tables 2 and 3). While enhanced ET-1-mediated vasoconstriction is supposed to play a role in the association between hypertension and increased adiposity in adults, our findings cannot support a role of ET-1 system activation in adiposity-related BP elevation in young subjects with excess weight.
Endothelin-1 and insulin resistance
In our study sample, the HOMA index was not related to NO or ET-1 values. Our findings with respect to insulin resistance are consistent with those of Lteif et al. [14], who recently reported that hyperinsulinemia failed to augment ET-1 action in vivo. Accordingly, while OW and obese adults had significantly higher plasma insulin concentrations and HOMA index values than the NW subjects, neither plasma insulin concentrations nor HOMA index was associated with forearm blood flow responses to either exogenous ET-1 or ETA receptor antagonist. These findings argue against an insulin-related effect [16] and suggest that other factors, including inflammation and oxidative stress, may contribute to the adiposity-related elevation in ET-1 system activity. It is interesting to note that in our population, the association between BP and the HOMA index lost its strength when the statistical model was corrected for a visceral obesity index (WtHr), suggesting that, in addition to insulin resistance, other factors such as cytokines produced by adipose tissue could collaborate to produce an increase in BP levels.
Conclusions
Our study has some limitations as well as several strengths that should be mentioned. Among the limitations, given the cross-sectional study design, we cannot exclude the possibility that genetic and/or lifestyle behaviors may have influenced our results. Undoubtedly, further studies with a different clinical approach might help to clarify the pathogenetic mechanisms underlying the reported associations. Second, due to the necessity to limit the invasive investigations, we did not assess ET-1 system activity in vivo as provided by intra-arterial infusion of exogenous ET-1 and ET-1 receptor antagonists. Circulating plasma concentrations of the peptide do not necessarily reflect local vascular production but rather variable spillover into and clearance from the bloodstream [48]. Moreover, because of the study design, only associations, but no cause-effect relationships, can be inferred. Nevertheless, we believe that the measurement of circulating plasma levels of ET-1, NO, and HOMA index provided interesting findings, making this study useful in the generation of a hypothesis of a pathophysiological model for hypertension. Therefore, further intervention studies, such as after a weight loss program, are warranted to better investigate these mechanisms. In particular, we believe that children are a model that allows us to explore the initial phase of hypertension development. Most likely, at this stage, the increased ET-1 activity has not yet caused vascular damage and is directly related to NO because the production of the latter is not yet reduced.
In our study population, the correlation between NO and BP levels and the lack of any relationship between ET-1 and BP could be explained by an increase in the vasodilatory effect of local and systemic NO that counteracts the possible hypertensive effect induced by ET-1. Further studies are encouraged to clarify the pathophysiological role of NO/endothelin imbalance in children with hypertension.
References
Barton M, Yanagisawa M. Endothelin: 20 years from discovery to therapy. Can J Physiol Pharmacol. 2008;86:498.
Chen M, Todd-Turla K, Wang WH, Cao X, Smart A, Brosius FC et al. Endothelin-1 mRNA in glomerular and epithelial cells of kidney. Am J Physiol Ren Fluid Electrolyte Physiol. 1993;265:F542–50.
Levin ER. Endothelins. N Engl J Med. 1995;333:356–63.
Ujiie K, Terada Y, Nonoguchi H, Shinohara M, Tomita K, Marumo F. Messenger RNA expression and synthesis of endothelin-1 along rat nephron segments. J Clin Invest. 1992;90:1043–8.
Hexum TD, Hoeger C, Rivier JE, Baird A, Brown MR. Characterization of endothelin secretion by vascular endothelial cells. Biochem Res Commun. 1990;167:294–300.
Verhaar MC, Strachan FE, Newby DE, Cruden NL, Koomans HA, Rabelink TJ et al. Endothelin-A receptor antagonist-mediated vasodilatation is attenuated by inhibition of nitric oxide synthesis and by endothelin-B receptor blockade. Circulation. 1998;97:752–6.
Rakugi H, Nakamaru M, Tabuchi Y, Nagano M, Mikami H, Ogihara T. Endothelin stimulates the release of prostacyclin from rat mesenteric arteries. Biochem Res Commun. 1989;160:924–8.
Warner TD, Mitchell JA, de Nucci G, Vane JR. Endothelin-1 and endothelin-3 release EDRF from isolated perfused arterial vessels of the rat and rabbit. J Cardiovasc. 1989;13 Suppl 5:S85–8.
de Nucci G, Thomas R, D’Orleans-Juste P, Antunes E, Walder C, Warner TD. et al. Pressor effects of circulating endothelin are limited by its removal in the pulmonary circulation and by the release of prostacyclin and endothelium-derived relaxing factor. Proc Natl Acad Sci USA. 1988;85:9797–800.
Bourque SL, Davidge ST, Adams MA. The interaction between endothelin-1 and nitric oxide in the vasculature: new perspectives. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1288–95.
Ferrannini E, Natali A, Bell P, Cavallo-Perin P, Lalic N, Mingrone G. Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J ClinInvest. 1997;100:1166–73.
Ferri C, Pittoni V, Piccoli A, Laurenti O, Cassone MR, Bellini C et al. Insulin stimulates endothelin-1 secretion from human endothelial cells and modulates its circulating levels in vivo. J Clin Endocrinol Metab. 1995;80:829–35.
Hu RM, Levin ER, Pedram A, Frank HJ. Insulin stimulates production and secretion of endothelin from bovine endothelial cells. Diabetes. 1993;42:351–8.
Lteif AA, Fulford AD, Considine RV, Gelfand I, Baron AD, Mather KJ. Hyperinsulinemia fails to augment ET-1 action in the skeletal muscle vascular bed in vivo in humans. Am J Physiol Endocrinol Metab. 2008;295:E1510–7.
Mahmoud AM, Szczurek MR, Blackburn BK, Mey JT, Chen Z, Robinson AT et al. Hyperinsulinemia augments endothelin-1 protein expression and impairs vasodilation of human skeletal muscle arterioles. Physiol Rep. 2016;4:e12895.
Weil BR, Westby CM, Van Guilder GP, Greiner JJ, Stauffer BL, DeSouza CA. Enhanced endothelin-1 system activity with overweight and obesity. Am J Physiol Heart Circ Physiol. 2011;301:H689–695. https://doi.org/10.1152/ajpheart.00206.2011
Stryer L. Biochemestry. 4th edn. Freeman and Company: New York, 1995.
Black SM, Fineman JR. Oxidative and nitrosative stress in pediatric pulmonary hypertension: roles of endothelin-1 and nitric oxide. Vascul Pharmacol. 2006;45:308–16.
Pollock JS, Pollock DM. Endothelin and NOS1/nitric oxide signaling and regulation of sodium homeostasis. Curr Opin Nephrol Hypertens. 2008;17:70–5.
Haynes WG, Noon JP, Walker BR, Webb DJ. Inhibition of nitric oxide synthesis increases blood pressure in healthy humans. J Hypertens. 1993;11:1375–80.
Wolzt M, Schmetterer L, Ferber W, Artner E, Mensik C, Eichler HG et al. Effect of nitric oxide synthase inhibition on renal hemodynamics in humans: reversal by L-arginine. Am J Physiol Ren Fluid Electrolyte Physiol. 1997;272:F178–82.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Brit Med J. 2000;320:1240–3.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114 2 Suppl 4th Report:555–76.
Oberfield SE, Levine LS, Firpo A, Lawrence D Sr., Stoner E, Levy DJ et al. Primary hyperaldosteronism in childhood due to unilateral macronodular hyperplasia. Case report. Hypertension. 1984;6:75–84.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Orlando A, Re F, Sesana S, Rivolta I, Panariti A, Brambilla D et al. CazzanigaE.Effect of nanoparticles binding β-amyloid peptide on nitric oxide production by cultured endothelial cells and macrophages. Int J Nanomed. 2013;8:1335–47.
Schiffrin EL. Vascular endothelin in hypertension. Vascul Pharmacol. 2005;43:19–29.
Goch A, Banach M, Mikhailidis DP, Rysz J, Goch JH. Endothelial dysfunction in patients with noncomplicated and complicated hypertension. Clin Exp Hypertens. 2009;31:20–30.
Kurihara Y, Kurihara H, Suzuki H, Kodama T, Maemura K, Nagai R et al. Elevated blood pressure and craniofacial abnormalities in mice deficient in endothelin-1. Nature. 1994;368:703–10.
Saito Y, Nakao K, Mukoyama M, Shirakami G, Itoh H, Yamada T et al. Application of monoclonal antibodiesfor endothelin to hypertensive research. Hypertension. 1990;15:734–8.
Fernandez-Cruz A, Martin P, Fernandez L, Sanchez J, Ibarra J, Moya J et al. Plasma endothelin is increased in young essential hypertensives but not in elderly essential or diabetic hypertensives. J Hypertens. 1993;11 suppl. 5:S146–147.
Lemne CE, Lundeberg T, Theodorsson E, de Faire U. Increased basal concentrations of plasma endothelin in borderline hypertension. J Hypertens. 1994;12:1069–74.
Veglio F, Bertello P, Pinna G, Mulatero P, Rossi A, Gurioli L et al. Plasma endothelin in essentialhypertension and diabetesmellitus. J Hum Hypertens. 1993;7:321–5.
Davenport AP, Ashby MJ, Easton P, Ella S, Bedford J, Dickerson C et al. A sensitive radioimmunoassay measuring endothelin-like immunoreactivity in human plasma: comparison of levels in patients with essential hypertension and normotensive control subjects. Clin Sci. 1990;78:261–4.
Sorensen SS, Egeblad M, Eiskjaer H, Madsen B, Nielsen CB, Sihm I et al. Endothelin in renovascular and essential hypertension. Blood Press. 1994;3:364–9.
Saito Y, Nakao K, Mukoyama M, Imura H. Increased plasma endothelin level in patients with essentialhypertension. New Engl J Med. 1990;322:205.
Naruse M, Kawana M, Hifumi S, Naruse K, Yoshihara I, Oka T et al. Plasma immunoreactiveendothelin,but not thrombomodulin, is increased in patients with essential hypertension and ischemic heart disease. J Cardiovasc Pharmacol. 1991;17 suppl. 7:S471–474.
Widimsky J Jr., Horky K, Dvorakova J. Plasma endothelin-1,2 levels in mild and severe hypertension. J Hypertens. 1991;9 suppl. 6:S194–195.
Aflyatumova GN, Nigmatullina RR, Sadykova DI, Chibireva MD, Fugetto F, Serra R. Endothelin-1, nitric oxide, serotonin and high blood pressure in male adolescents. Vasc Health Risk Manag. 2018;14:213–23.
Paravicini TM, Touyz RM. Redox signaling in hypertension. Cardiovasc Res. 2006;71:247–58.
Strambi M, Messa G, Berni S, Capitani S, Pammolli A, Iacoponi F et al. Basal and post-ischemic vascular compliance in children/adolescents born small for gestational age. Pediatr Nephrol. 2012;27:1541–6.
Katona E, Settakis G, Varga Z, Paragh G, Bereczki D, Fülesdi B et al. Target-organ damage in adolescent hypertension. Analysis of potential influencing factors, especially nitric oxide and endothelin-1. J Neurol Sci. 2006;247:138–43.
Genovesi S, Antolini L, Giussani M, Brambilla P, Barbieri V, Galbiati S et al. Hypertension, prehypertension, and transient elevated blood pressure in children: association with weight excess and waist circumference. Am J Hypertens. 2010;23:756–61.
Genovesi S, Antolini L, Giussani M, Pieruzzi F, Galbiati S, Valsecchi MG et al. Usefulness of waist circumference for the identification of childhood hypertension. J Hypertens. 2008;26:1563–70.
Cardillo C, Campia U, Iantorno M, Panza JA. Enhanced vascular activity of endogenous endothelin-1 in obese hypertensive patients. Hypertension. 2004;43:36–40.
Mather KJ, Mirzamohammadi B, Lteif A, Steinberg HO, Baron AD. Endothelin contributes to basal vascular tone and endothelial dysfunction in human obesity and type 2 diabetes. Diabetes. 2002;51:3517–23.
Charakida M, Jones A, Falaschetti E, Khan T, Finer N, Sattar N et al. Childhood obesity and vascular phenotypes: a population study. J Am Coll Cardiol. 2012;60:2643–50.
Cardillo C, Kilcoyne CM, Waclawiw M, Cannon RO 3rd, Panza JA. Role of endothelin in the increased vascular tone of patients with essential hypertension. Hypertension. 1999;33:753–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Orlando, A., Viazzi, F., Giussani, M. et al. Endothelin-1/nitric oxide balance and HOMA index in children with excess weight and hypertension: a pathophysiological model of hypertension. Hypertens Res 42, 1192–1199 (2019). https://doi.org/10.1038/s41440-019-0253-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0253-3
- Springer Nature Singapore Pte Ltd.