Abstract
Objectives
To determine spherical equivalent (SE) progression among children in the Shahroud School Children Eye Cohort Study.
Methods
A prospective cohort study recruited children aged 6 to 12 years in 2015 (baseline) with a follow-up in 2018. Cycloplegic autorefraction and axial length (AL) measurements were included. SE progression over 3 years was analysed in non-myopic (SE ≥ + 0.76 D), pre-myopic (PM; SE between +0.75 D and –0.49 D), low myopic (LM; SE between −0.5 D and −5.99 D), and high myopic (HM; SE ≤ − 6 D) eyes. Age, sex, near work, outdoor time, living place, parental myopia, mother’s education, and baseline SE were evaluated as risk factors for SE progression (≤ −0.50 D).
Results
Data were available for 3989 children (7945 eyes). At baseline, 40.3% (n = 3205), 3.4% (n = 274) and 0.1% (n = 7) eyes had PM, LM and HM, respectively. At the 3-year follow-up, 40.5% (n = 3216), 7.5% (n = 599) and 0.2% (n = 15) eyes had PM, LM, and HM, respectively. SE progression in eyes with LM and HM was −1.08 ± 0.76 D and −1.60 ± 1.19 D, respectively. SE progression was associated with age at baseline (Odds Ratio [OR] = 1.14; 95% confidence interval [CI], 1.08–1.21), female sex (OR = 1.80; 95% CI: 1.48–2.18), near work (OR = 1.08; 95% CI: 1.02–1.14), parental myopia (OR = 1.20; 95% CI: 1.01–1.42) and baseline SE (OR = 2.28; 95% CI: 1.88–2.78).
Conclusion
A myopic shift was associated with older age, female sex, near work, parental myopia and greater myopic baseline SE. These results help identifying children at risk of progression that may benefit from treatment and lifestyle counselling.
Similar content being viewed by others
Introduction
Myopia is an important public health problem with 50% of the world population expected to have myopia in 2050 [1]. Environmental risk factors such as reduced time outdoors, more intensive education and increased near work have been linked to the increased rates of myopia [2,3,4,5]. Preventing myopia progression during childhood is of paramount importance to reduce the incidence of high myopia and myopia-related complications such as myopic macular degeneration [6, 7].
Progression of myopia has been analysed in prior studies and was reported to be greater in East and Southeast Asian Countries compared with Western countries [8,9,10]. The mean myopia progression varied from −0.63 to −2.00 dioptres (D) per year in clinical trials performed in East Asia, such as in China and Hong Kong, and in Southeast Asia, in Singapore. [8, 11,12,13,14,15] Although ethnicity seems to be an important factor for myopia progression rates, risk factors for myopia progression appear to be similar between East Asian descents and Europeans. Faster myopia progression (≤ −0.50 D per year) was associated with younger age, female sex and greater myopic spherical equivalent (SE) at baseline among myopic (SE ≤ –4.00 D) European children aged 7 to 12 years [9]. Additionally, age of myopia onset and parental myopia were also identified as risks factors for myopia progression [16,17,18]. SE at 10 years of age may be an important prognostic indicator that can help determine myopia control treatment intensity, as those with faster progression before the age of 10 years were more likely to develop high myopia in adulthood [7]. Most existing data on myopia progression are from East Asian or Western Countries, with scarce data from Middle East [19, 20]. Greater understanding on risk factors of myopia progression in different populations is necessary to guide clinical management.
This study aimed to examine SE progression among children in the Shahroud School Children Eye Cohort Study (SSCECS) in Iran.
Methods
Study population and design
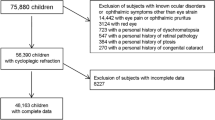
The SSCECS is a prospective cohort study where children aged 6 to 12 years were recruited from urban and rural areas in Shahroud, northeast Iran in 2015. The study methodology has been previously reported [21]. At baseline, children were excluded if they had a history of eye surgery or trauma, strabismus and amblyopia. Children who attended both the baseline and the 3-year follow-up visit in 2018 were included in this study (Supplementary Fig. 1). The protocol of this study was approved by the Ethics Committee of Shahroud University of Medical Sciences which adheres to the principles of the Declaration of Helsinki. All parents signed informed consents for the participation of their children in the study. All included schoolchildren were willing to participate.
Inclusion and exclusion criteria
Children who attended the baseline and the 3-year follow-up visit with available information on SE or axial length (AL) measures and environmental risks factors were analysed. They were included in the analysis if the following criteria were met: (1) availability of SE measured by cycloplegic refractometry and/or AL; and (2) availability of at least one of the following variables, the time spent on reading and writing, watching screen-based entertainment (screen time), total near work and time spent outdoors.
Refraction and biometry measurements
Cycloplegic autorefraction was performed with retinoscopy and the Nidek ARK-510A at least 30 min after instilling 2 drops of cyclopentolate 1% at an interval of 5 min. SE was calculated using the standard formula (SE = sphere + [cylinder/2]). AL (in mm) was measured with the Allegro Lenstar LS 900 (WaveLight AG, Erlangen, Germany).
Reading and writing, screen time, total near work and outdoor time
The time spent on reading and writing, digital screen-based entertainment, total time spent on near work and time spent outdoors were estimated by a questionnaire filled in by the parents. Total near work was defined as any activity such as reading and writing, colouring, drawing, reading for pleasure, doing homework/study, computer work and playing handheld devices. Digital screen time was defined as the time spent watching screen-based entertainment (computer and mobile devices). Outdoor time included physical activities and leisure activities. Reading and writing, screen time, total near work and outdoor time (computed as the number of hours per day [h/d]) from the questionnaires were aligned for each child.
Other measures
Detailed interviewer-administered questionnaires were used to collect demographic (age, sex and parents’ education and parents’ myopia status) data, general medical and ophthalmic history. Participants’ height was measured in the upright position without shoes, using a stadiometer with an accuracy of 0.1 cm [21].
Predictors of SE and AL progression
The outcome of interest was SE and AL progression over the 3-year period. Three-year mean SE and AL progression, defined as a progression over a period of 3 years, were calculated by subtracting baseline measurements from 3-year follow-up measurements. SE progression represents worsening of SE (in the negative direction), and AL progression represents axial elongation. SE progression was defined as having SE progression of at least −0.50 D over the 3-year period regardless of myopia status. Myopia progression was defined as having SE progression of at least −0.50 D over the 3-year period in myopic eyes. AL progression was defined as having AL progression exceeding the median cut of 0.28 mm over the 3-year period. In our study, there was a moderate inverse correlation between AL progression and SE progression (r = −0.56). The relationship between SE and AL is influenced by child’s age and the amount of myopia, with AL correlation with SE being stronger in older children and in eyes with longer AL. For example, a previous study, reported that 1 D of myopia was equivalent to 0.28 mm of axial length growth in the 6–7-year-olds and 0.32 mm in the 12–13-year-olds [22]. In another study, The Correction of Myopia Evaluation Trial (COMET) study, a 0.5 mm increase in axial length was associated with 1 D of myopia progression in myopic children 6 to 11 years [23]. Thus, the definition of AL progression in our study was based on the current evidence, the younger age of our cohort and the analysis of the median cut-off (0.28 mm).
SE progression over 3 years was analysed in non-myopic (SE ≥ + 0.76 D), pre-myopic (PM; SE between +0.75 D and –0.49 D), low myopic (LM; SE between −0.5 D and −5.99 D), and high myopic (HM; SE ≤ − 6 D) eyes [24].
Statistical analysis
The 3-year eye-specific incidence rate was calculated based on the development of myopia in eyes without myopia at baseline. To determine the risk factors associated with SE progression, eyes with SE progression (≤ −0.50 D) and eyes without SE progression over the 3-year period were compared. The outcomes ‘SE progression’ and ‘AL progression (defined by the median cut-off)’ were analysed as categorical variables (yes/no). Additionally, the outcomes ‘SE progression’ and ‘AL progression’ were analysed as continuous variables. ANOVA was used for comparisons of SE and AL progression over a 3-year period by age groups and SE categories at baseline. To evaluate the differences in participant characteristics by outcome status, the eye with higher SE or AL progression (worse eye) of each subject at the last follow-up was chosen. If progression was the same for both eyes, progression from the right eye was selected. To evaluate the differences in participant eye characteristics by outcome status both eyes were chosen.
Risk factors such as baseline SE and AL, and total near work, screen time and outdoor time were analysed as continuous variables (per unit change). Both eyes were included for analysis, thus Generalised Estimating Equation (GEE) was used to account for the correlation between the two eyes. The results were reported with adjustment for confounders, by including the following variables as covariates in the GEE models: age, gender, mothers’ education, parental myopia, baseline SE and residence place (rural/urban). Height and baseline AL were only included for the models using AL progression as outcomes. P < 0.05 was considered statistically significant. All statistical analyses were carried out with STATA software and SPSS (IBM, United States, version 26).
Results
A total of 3989 children (7945 eyes) were included in the analysis. The mean (± standard deviation) age was 9.6 ± 1.7 years, and 2042 (51.2%) were boys (Table 1). At baseline, 3205 (40.3%), 274 (3.4%) and 7 (0.1%) eyes had PM, LM, and HM, respectively. At the 3-year follow-up, 40.5% (n = 3216), 7.5% (n = 599) and 0.2% (n = 15) eyes had PM, LM, and HM, respectively. The 3-year incidence rate of myopia was 4.7% (95% confidence interval [CI], 3.7–5.7).
At the 3-year follow-up visit, the mean SE was 0.69 ± 0.98 D, ranging from −11.00 D to 5.25 D, and the mean AL was 23.29 ± 0.78 mm, ranging from 20.54 mm to 28.01 mm. The mean 3-year SE progression was −0.15 ± 0.47 D, and the 3-year AL progression was 0.31 ± 0.19 mm. In eyes with LM at follow-up (n = 599), the mean 3-year myopia progression was −1.08 ± 0.76 D, and the 3-year AL progression was 0.63 ± 0.30 mm. Myopia progression was significantly (both p < 0.001) higher in eyes with HM at follow-up (n = 15) with mean 3-year SE and AL progression at −1.60 ± 1.19 D and 0.79 ± 0.47 mm, respectively.
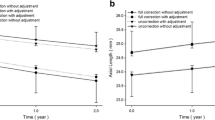
Figure 1 shows the 3-year SE and AL progression in all children stratified by age groups (Fig. 1, top panel) and SE categories at baseline (Fig. 1, bottom panel). Mean SE progression increased with age at baseline (ANOVA, p < 0.001), while mean AL progression decreased with age at baseline (ANOVA, p < 0.001). SE progression (r = −0.15) and AL progression (r = −0.31) were correlated with baseline age. Near work increased significantly (ANOVA, p < 0.001) with baseline age, with children aged 6 to 8 years (3.60 ± 1.55 h/d) spending less time on near work compared with 9- to 10-year-olds (3.77 ± 1.67 h/d) and 11- to 12-year-olds (3.94 ± 1.71 h/d). Reading and writing were only significantly different (p = 0.025) in 6- to 8-year-olds (1.12 ± 0.59 h/d) compared with 11- to 12-year-olds (1.18 ± 0.62 h/d). Outdoor time was only significantly different (p = 0.004) in 9- to 10-year-olds (1.56 ± 1.28 h/d) compared with 11- to 12-year-olds (1.68 ± 1.39 h/d). Mean AL progression increased significantly (ANOVA, p < 0.001) for all baseline SE categories, except for the HM group. The HM group only differed significantly from the LM group (p = 0.002). Mean SE progression was the highest for the LM and HM groups at baseline and differed significantly from the no myopia and PM groups at baseline (p < 0.05). SE progression (r = 0.20) and AL progression (r = −0.29) were correlated with baseline SE. A correlation was also detected between AL progression and baseline AL (r = 0.04). Near work time increased significantly (ANOVA, p < 0.002) with baseline SE categories, with children with no myopia (3.69 ± 1.60 h/d) spending less time on near work compared with children with PM (3.80 ± 1.66 h/d), LM (4.00 ± 1.88 h/d) and HM (4.37 ± 2.51 h/d). Outdoor time did not differ significantly (ANOVA, p = 0.22) by baseline SE categories. Girls had greater myopic SE progression (−0.19 ± 0.51 in girls versus −0.10 ± 0.42 in boys; p < 0.001) and faster AL progression (0.33 ± 0.19 in girls versus 0.29 ± 0.18 in boys; p < 0.001) over 3 years.
Of 4459 non-myopic eyes at baseline, 9 (0.2%) developed myopia over the 3-year period. Mean SE progression in those 9 eyes was −2.83 ± 2.31 D. Of 3205 pre-myopic eyes at baseline, 332 (10.4%) developed myopia over the 3-year period. Mean SE progression in those 332 eyes was −1.09 ± 0.57. Of 274 eyes with LM at baseline, 258 (94.2%) had persistent LM, 8 (2.9%) had developed HM, and 8 (2.9%) reverted to PM at 3-year follow-up. The 3-year mean SE progression in eyes with LM and HM at baseline was −1.04 ± 0.84 D and −0.64 ± 0.86 D, respectively.
A myopic shift of 0.50 D or greater occurred in 909 eyes (11.4%) and axial elongation of 0.28 mm or more occurred in 4001 eyes (50.4%). Compared with children without SE progression, children with SE progression were older, taller, more likely to be girls, from urban regions, with mothers having a greater number of years of education, with a higher number of non-myopic parents, and spent less time outdoors and more on near work (Table 2). Compared with children without AL progression, children with axial elongation of 0.28 mm or more were younger, shorter, more likely to be girls, with mothers having a greater number of years of education, with a higher number of non-myopic parents, and spent less time outdoors and more on near work. Compared with eyes without a myopic shift, eyes with a myopic shift had less hyperopic SE at baseline and were from no myopia and PM baseline categories (Table 3). Eyes from the lower AL quartiles, shorter AL, less hyperopic SE at baseline were more likely to have AL progression.
SE progression in all eyes was associated with older age at baseline (Odds Ratio [OR] = 1.14; 95% CI: 1.08–1.21), female sex (OR = 1.80; 95% CI: 1.48–2.18), near work (OR = 1.08; 95% CI: 1.02–1.14), parental myopia (OR = 1.20; 95% CI: 1.01–1.42) and higher myopic baseline SE (OR = 2.28; 95% CI: 1.88–2.78; Table 4) in the multivariable model. Conversely, AL progression in all eyes was associated with younger age at baseline (OR = 0.53; 95% CI: 0.49–0.57). Additionally, AL progression was also associated with mother’s education (OR = 1.03; 95% CI: 1.01–1.05), outdoor time (OR = 0.94; 95% CI: 0.89–0.99), and AL at baseline (OR = 1.63; 95% CI: 1.47–1.81) in the multivariable model. Myopic progression in myopic eyes at baseline was not significantly associated with any of the predictors in the multivariable model. There was a tendency, although non-significant, for children with no myopic and PM eyes at baseline to spend less time outdoors (1.39 ± 1.31 h/d and 1.42 ± 1.28 h/d) and more time on near work (4.50 ± 1.36 and 4.12 ± 1.68) compared with children with LM eyes (outdoor time: 1.52 ± 1.24 h/d; near work: 3.99 ± 1.88 h/d).
Discussion
This study describes SE and AL progression over a 3-year period in 3989 children aged 6 to 12 years from Iran (n = 7945 eyes). The 3-year incidence rate of myopia was low (4.6%, 95% CI: 4.1, 5.1). The mean 3-year SE and AL progression in eyes with LM at follow-up were −1.08 ± 0.76 D and 0.63 ± 0.30 mm, respectively. The progression was significantly higher in eyes with HM at follow-up. Factors associated with faster SE progression were female sex, more severe myopia level at baseline, older age, more time spent near work and a higher number of parents with myopia.
The mean SE progression (−1.08 ± 0.76 D) over 3 years in children with LM in this study was similar to African-American children with myopia onset at 7 years (−1.05 D, 95% CI −1.34, −0.76) from the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study [25]. Our mean AL progression (0.63 ± 0.30 mm) was also similar to the mean 3-year progression rate in children aged 8 to 12 years in the control group of the MiSight Lenses study at 0.62 ± 0.30 mm [26]. However, our mean 3-year SE progression was slightly lower than that of White children with myopia onset at 10 years (mean of −1.25 D; 95% CI: −1.43 to −1.06) from the CLEERE [25] study and that of the control group aged 8 to 12 years of the MiSight Lenses study (−1.24 ± 0.61 D) [26]. Our mean SE progression was more than double of that in the Northern Ireland Childhood Errors of Refraction (NICER) Study for the older cohort aged 12 to 13 years (mean of −0.33 D, 95% CI, −1.63 to −0.63) [27]. Compared to other Asian children, our progression results showed a much slower progression. For example, the 3-year progression in children aged 7 to 10 years was −2.11 D (95% CI, − 2.23 to −1.99) in children from Singapore [28], which may be related to differences in ethnicity, genetics and environmental factors, such as outdoor exposure or near work patterns.
In the present study, higher myopic baseline SE was associated with SE progression in all children. This finding is in line with other study results [7, 9] that showed faster myopic progression in children with higher myopic refractive error at baseline. SE progression rates may be useful as guidelines to identify fast progressors who may likely benefit from early or more intensive treatment. In our study, we found an inversion of the OR when we analysed myopia progression in myopes and baseline SE. This inversion seemed to be mainly influenced by the 3-year myopia progression in 9 non-myopic eyes at baseline that developed myopia and a very fast progression of −2.83 ± 2.31 D. We found that there was a tendency, although non-significant, for those children with no myopic eyes at baseline to spend less time and more time on near work compared with children with LM eyes. Although, those results may be related to differences in environmental factors, such as outdoor exposure or near-work patterns, other unknown factors cannot be excluded, and further research is necessary.
In the present study, older age was associated with greater SE progression, whereas axial length progression was associated with younger age. Although SE progression was significantly greater for children aged 11 to 12 years, the difference seems to be of low clinical significance, as it was only 0.04 D in 3 years compared with children aged 9 to 10 years. Nevertheless, several studies showed that SE progression is faster at younger ages [23, 25, 29]. Although the reason for the different findings is difficult to identify, one possibility is that the age of myopia onset was different, as it is expected that there would be greater myopia progression if the onset of myopia occurs at a younger age.
We also found that near work was associated with SE progression and less time outdoors with AL progression. This finding is different from the CLEERE study results where no association was found [25, 30]. However, children from the CLEERE study resided in the United States and might have been exposed to different environments. The findings related to near work and SE progression are mixed, with several studies reporting no association [30,31,32,33] and others reporting a positive association [34]. In our study, near work was measured subjectively using a questionnaire. Objective measures of near work may provide better information on the significance of this factor on progression rates.
Gender was associated with SE and AL progression; girls had both greater mean SE and AL progression. Although we observed a significant gender difference in progression rates, this difference was not clinically significant at 0.09 D for SE progression and 0.04 mm for AL progression over 3 years. This finding is in line with other studies and may be related to lifestyle [25, 29, 35, 36]. Different lifestyles, such as more near work or less outdoor time, may be related to this gender difference, but further research is necessary.
Parental myopia was associated with the rate of progression. This is similar to results reported by the COMET study, the Raine Study and a Singapore study including children aged 6 to 12 years, where increasing myopia progression was found in those with a greater number of myopic parents [25, 31, 36]. Parental myopia is a complex measure and may be a mix of genetic and environmental exposures.
Potential limitations of our study should also be mentioned. Age of myopia onset was not assessed in the study, and it is an important factor for myopia progression. Age of onset of myopia may differ from age at baseline or age at study entry. The use of 0.28 mm as the cut-off for AL progression for this study was not comparable with the definition of myopia progression (≤ −0.50 D). The number of eyes with 0.28 mm of AL progression were considerable higher (n = 4001 eyes) than the number of eyes with myopia progression ≤ −0.50 D (n = 909 eyes) during the 3-year period. Those results, warrant further research as 1714 eyes were classified in the pre-myopia group and may be predisposed to develop myopia in a near future. The study was limited by a restricted range of ages at baseline between 6 to 12 years. Follow-up was not sufficiently long to observe progression in late teens and adulthood. However, strengths include the examination of important risk factors such as outdoor time and near work, a large sample size with cycloplegic refraction and AL measurements.
Conclusions
We found that myopic shifts were associated with children who were older, female, engaged in more near work, with parental myopia, and more myopic baseline refractive error. These results may help identify children at risk of progression and determine the best time of treatment intervention or determine the children who may benefit from treatment to slow myopic progression. Further research is necessary, especially on preventive strategies that may combine pharmacological and optical treatment with counselling on lifestyle to avoid progression to high myopia in adulthood and related complications, such as myopic macular degeneration.
Summary
What was known before
-
Reduced time outdoors, more intensive education and increased near work have been linked to the increased rates of myopia.
-
Preventing myopia progression during childhood is of paramount importance.
What this study adds
-
The 3-year incidence rate of myopia was low (4.7%).
-
Female sex, more severe myopia level at baseline, older age, more time spent near work and myopic parents are associated factors with myopia progression.
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42. https://doi.org/10.1016/j.ophtha.2016.01.006.
Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, Smith W. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85. https://doi.org/10.1016/j.ophtha.2007.12.019.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J. et al. Effect of time spent outdoors at school on the development of myopia among children in China. JAMA. 2015;314:1142. https://doi.org/10.1001/jama.2015.10803.
Ip JM, Saw SM, Rose KA, Morgan IG, Kifley A, Wang JJ. et al. Role of near work in myopia: findings in a sample of Australian school children. Investig Opthalmology Vis Sci. 2008;49:2903. https://doi.org/10.1167/iovs.07-0804.
Nickels S, Hopf S, Pfeiffer N, Schuster AK. Myopia is associated with education: Results from NHANES 1999-2008. PLoS One. 2019;14:e0211196 https://doi.org/10.1371/journal.pone.0211196.
Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157:9–25.e12. https://doi.org/10.1016/j.ajo.2013.08.010.
Polling JR, Klaver C, Tideman JW. Myopia progression from wearing first glasses to adult age: the DREAM Study. Br J Ophthalmol. 2021; https://doi.org/10.1136/bjophthalmol-2020-316234.
Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY. et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Investig Opthalmology Vis Sci. 2004;45:1071. https://doi.org/10.1167/iovs.03-1151.
Tricard D, Marillet S, Ingrand P, Bullimore MA, Bourne RRA, Leveziel N. Progression of myopia in children and teenagers: a nationwide longitudinal study. Br J Ophthalmol. 2021. https://doi.org/10.1136/bjophthalmol-2020-318256.
Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL A, Holden B. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27–32. https://doi.org/10.1097/OPX.0b013e3182357f79.
Yam JC, Jiang Y, Tang SM, Law AKP, Chan JJ, Wong E. et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126:113–24. https://doi.org/10.1016/j.ophtha.2018.05.029.
Yen MY, Liu JH, Kao SC, Shiao CH. Comparison of the effect of atropine and cyclopentolate on myopia. Ann Ophthalmol. 1989;21:180–2, http://www.ncbi.nlm.nih.gov/pubmed/2742290.
Yi S, Huang Y, Yu SZ, Chen XJ, Yi H, Zeng XL. Therapeutic effect of atropine 1% in children with low myopia. J Am Assoc Pediatr Ophthalmol Strabismus. 2015;19:426–9. https://doi.org/10.1016/j.jaapos.2015.04.006.
Wang Y, Bian HL, Wang Q. Atropine 0.5% eyedrops for the treatment of children with low myopia. Med (Baltim). 2017;96:e7371 https://doi.org/10.1097/MD.0000000000007371.
Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL. et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91. https://doi.org/10.1016/j.ophtha.2006.05.062.
Ma Y, Zou H, Lin S, Xu X, Zhao R, Lu L. et al. Cohort study with 4-year follow-up of myopia and refractive parameters in primary schoolchildren in Baoshan District, Shanghai. Clin Exp Ophthalmol. 2018;46:861–72. https://doi.org/10.1111/ceo.13195.
Pärssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: a three-year follow-up study. Invest Ophthalmol Vis Sci. 1993;34:2794–802. http://www.ncbi.nlm.nih.gov/pubmed/8344801.
Loh KL, Lu Q, Tan D, Chia A. Risk factors for progressive myopia in the atropine therapy for myopia study. Am J Ophthalmol. 2015;159:945–9. https://doi.org/10.1016/j.ajo.2015.01.029.
Fotouhi A, Hashemi H, Khabazkhoob M, Mohammad K. The prevalence of refractive errors among schoolchildren in Dezful, Iran. Br J Ophthalmol. 2007;91:287–92. https://doi.org/10.1136/bjo.2006.099937.
Norouzirad R, Hashemi H, Yekta A, Nirouzad F, Ostadimoghaddam H, Yazdani N. et al. The prevalence of refractive errors in 6- to 15-year-old schoolchildren in Dezful, Iran. J Curr Ophthalmol. 2015;27:51–55. https://doi.org/10.1016/j.joco.2015.09.008.
Emamian MH, Hashemi H, Khabazkhoob M, Malihi S, Fotouhi A. Cohort Profile: Shahroud Schoolchildren Eye Cohort Study (SSCECS. Int J Epidemiol. 2019;48:27–27f. https://doi.org/10.1093/ije/dyy250.
Cruickshank FE, Logan NS. Optical ‘dampening’ of the refractive error to axial length ratio: implications for outcome measures in myopia control studies. Ophthalmic Physiol Opt. 2018;38:290–7. https://doi.org/10.1111/opo.12457.
Hyman L. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005;123:977. https://doi.org/10.1001/archopht.123.7.977.
Jong M, Jonas JB, Wolffsohn JS, Berntsen DA, Cho P, Clarkson-Townsend D. et al. IMI 2021 yearly digest. Investig Opthalmology Vis Sci. 2021;62:7 https://doi.org/10.1167/iovs.62.5.7.
Jones-Jordan LA, Sinnott LT, Chu RH, Cotter SA, Kleinstein RN, Manny RE. et al. Myopia progression as a function of sex, age, and ethnicity. Invest Ophthalmol Vis Sci. 2021;62:36. https://doi.org/10.1167/iovs.62.10.36.
Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year randomized clinical trial of MiSight lenses for myopia control. Optom Vis Sci. 2019;96:556–67. https://doi.org/10.1097/OPX.0000000000001410.
Breslin KMM, O’Donoghue L, Saunders KJ. A prospective study of spherical refractive error and ocular components among Northern Irish schoolchildren (The NICER study). Investig Opthalmology Vis Sci. 2013;54:4843. https://doi.org/10.1167/iovs.13-11813.
Khor WB, Aung T, Saw SM, Wong TY, Tambyah PA, Tan AL. et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. JAMA. 2006;295:2867–73. https://doi.org/10.1001/jama.295.24.2867.
Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT. et al. Incidence and progression of myopia in Singaporean school children. Investig Opthalmology Vis Sci. 2005;46:51. https://doi.org/10.1167/iovs.04-0565.
Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, Mutti DO. et al. Time outdoors, visual activity, and myopia progression in Juvenile-onset myopes. Investig Opthalmology Vis Sci. 2012;53:7169. https://doi.org/10.1167/iovs.11-8336.
Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77:549–54. http://www.ncbi.nlm.nih.gov/pubmed/11100893.
Li SM, Li H, Li SY, Liu LR, Kang MT, Wang YP. et al. Time outdoors and myopia progression over 2 years in Chinese children: the anyang childhood eye study. Investig Opthalmology Vis Sci. 2015;56:4734. https://doi.org/10.1167/iovs.14-15474.
Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080–5. https://doi.org/10.1016/j.ophtha.2012.11.009.
Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Gupta V, et al. Incidence and progression of myopia and associated factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS One. 2017;12:e0189774 https://doi.org/10.1371/journal.pone.0189774.
Zhou WJ, Zhang YY, Li H, Wu YF, Xu J, Lv S. et al. Five-year progression of refractive errors and incidence of myopia in school-aged children in western China. J Epidemiol. 2016;26:386–95. https://doi.org/10.2188/jea.JE20140258.
Lee SS, Lingham G, Sanfilippo PG, Hammond CJ, Saw SM, Guggenheim JA. et al. Incidence and progression of myopia in early adulthood. JAMA Ophthalmol. 2022;140:162–9. https://doi.org/10.1001/jamaophthalmol.2021.5067.
Funding
This work was supported by the Noor Ophthalmology Research Centre and Shahroud University of Medical Sciences (Grant Number: 960351).
Author information
Authors and Affiliations
Contributions
CL and MHE contributed to the conception and design of the study. CL and MHE performed the data analyses. CL wrote the manuscript. Manuscript revision: YL, MK, HH, AG, SSM and AF. Final approval of the manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
YLW is an employee of Essilor International, Singapore. Other authors have no conflict of interests to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lanca, C., Emamian, M.H., Wong, Y.L. et al. Three-year change in refractive error and its risk factors: results from the Shahroud School Children Eye Cohort Study. Eye 37, 1625–1632 (2023). https://doi.org/10.1038/s41433-022-02219-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02219-8
- Springer Nature Limited