Abstract
Background
Idiopathic intracranial hypertension (IIH) is a condition of raised intracranial pressure (ICP). Obstructive sleep apnoea (OSA) has been shown to cause episodic rises in ICP and is frequently reported in patients with IIH. The aim of this study is to identify the prevalence of OSA in a cohort of IIH patients.
Methods
We conducted a retrospective case notes review as part of a service evaluation of newly diagnosed IIH patients who were all referred for OSA screening with overnight pulse oximetry. The 3% oxygen desaturation index (3% ODI) was used to evaluate the presence and severity of OSA. The clinical outcomes of patients who received continuous positive airway pressure (CPAP) therapy as treatment for OSA were reviewed.
Results
In our cohort of newly diagnosed IIH patients, the yield of overnight pulse oximetry as a screening tool was 48.6% for OSA and 15.3% for moderate to severe OSA. We found that age (p = 0.0008), BMI (p < 0.0001), vitamin B12 (p = 0.0183), and a higher Epworth Sleep Score (p = 0.0269) correlated with more severe OSA. Eleven (10%) patients had CPAP therapy and those with good adherence alongside weight loss or medical therapy found improvements in symptoms of raised ICP.
Conclusion
We report the largest series of consecutive IIH patients screened for OSA using overnight pulse oximetry. The high rate of OSA highlights a potential role for the recognition and management of OSA in the IIH patient cohort. Further studies on the potential contribution of OSA as a cause of raised ICP in the IIH cohort is warranted.
Similar content being viewed by others
Introduction
Idiopathic intracranial hypertension (IIH) is a condition of raised intracranial pressure (ICP). The current diagnostic criteria is defined by the modified Dandy criteria, which requires: (1) normal neuroimaging apart from evidence of raised ICP; (2) lumbar puncture (LP) opening pressure of > 25 cm CSF with normal cerebrospinal fluid (CSF) composition; (3) signs and symptoms of raised ICP; (4) no evidence of localising signs with the exception of sixth cranial nerve palsy; and (5) no secondary causes of raised ICP identified [1]. It occurs predominantly in women and has a striking association with obesity [2,3,4]. Patients with IIH commonly present with symptoms including headaches, pulsatile tinnitus and transient visual obscuration. Current treatments include weight loss, medical therapies such as acetazolamide or topiramate, and surgical intervention such as CSF diversion, optic nerve sheath fenestration, or bariatric surgery [5].
Obstructive sleep apnoea (OSA) is a condition in which episodes of hypopnoea and apnoea occur during sleep as a result of partial or complete obstruction of the upper airway. Signs and symptoms of OSA include disruptive snoring, witnessed apnoea or gasping, excessive daytime sleepiness and unrefreshing sleep. It is more common in men [6], postmenopausal women [7], obesity [8] and larger neck circumference (>42 cm in men; >37 cm in women) [9]. The prevalence of OSA in IIH patients has previously been reported to be between 4% and 60% [10,11,12,13]. OSA has been shown to cause episodic increases in ICP, relating to apnoeic episodes during sleep and its involvement in the pathophysiology of IIH in patients with concurrent OSA has been speculated [14]. The aim of this study was to identify the prevalence of OSA in a cohort of patients with IIH.
Methods
Study design and participants
Between February 2018 and July 2020, we conducted a retrospective case notes review of patients newly diagnosed with IIH in the Medical Eye Unit at Guy’s and St Thomas’ NHS Foundation Trust, all of whom were referred for overnight pulse oximetry as part of screening for OSA. This was conducted as part of a service evaluation to understand potential unmet clinical need. We excluded patients in whom overnight pulse oximetry could not be obtained (e.g., in those who did not attend appointment, insufficient sleep study data or already on CPAP therapy). This study received institutional approval as a service evaluation and quality improvement project (ID No: 9139).
Patient demographics including age, gender, BMI and neck size were collected. We obtained serum haemoglobin and serum haematinics including iron, ferritin, active vitamin B12, folate and 25-hydroxyvitamin D3 from the hospital database which were routinely collected as part of standard clinical care in our IIH patients. The prevalence of anaemia was obtained using a cut-off of serum haemoglobin levels <12.0 g/dL in women and <13.0 g/dL in men. The lumbar puncture opening pressure and presence of papilloedema on referral for oximetry studies were also recorded. Optical coherence tomography (OCT) images were reviewed to obtain the retinal nerve fibre layer (RNFL) thickness, where elevated RNFL thickness was used as a marker of severity of papilloedema. Note was also made of patients with optic atrophy and significantly thinned RNFL as a consequence of severe, chronic papilloedema.
The prevalence of OSA in this cohort was reported. We compared data between non-OSA, mild OSA and moderate to severe OSA groups. The effects of CPAP treatment on raised intracranial pressure (ICP) symptoms were described.
Overnight home pulse oximetry
All patients had pulse oximetry conducted over two nights. The 3% oxygen desaturation index (3% ODI) as defined by ODI ≥ 3% x60/TST was used to diagnose and stratify the severity of OSA. OSA was graded mild if 3% ODI was >5 and ≤15, moderate if >15 to <30, and severe if ≥30.
Statistical analysis
Distribution of variables were checked using the D’Agostino & Pearson normality test. The Kruskal-Wallis test (for non-normally distributed data), ordinary one-way ANOVA test (for normally distributed data) and Chi-square tests were used to calculate the difference in variables for the comparison groups. To adjust for multiple comparisons, Bonferroni’s or Dunn’s post hoc test was performed if one-way ANOVA or Kruskal-Wallis yielded a significant p-value. The Spearman Rank-Order Correlation Test was used to calculate the Spearman r correlation coefficient with two-tailed p values for patient demographics and clinical data against oximetry results. Missing variables were omitted from statistical analyses. All statistical calculations were done using the Prism 9.0.0 (86) for macOS software.
Results
Patient demographics and clinical data
One hundred and twenty-one patients were seen during the study period. Of these, 111 patients were included; 105 were female (95%) and 6 were male (5%). Ages ranged from 16 to 81 years (mean 36.4 ± SD 13.4 years). BMI ranged from 24.4 to 59.6 kg/m2 (mean 36.6 ± SD 7.9 kg/m2).
The mean lumbar puncture opening pressure was 31.7 cm CSF ± SD 9.1 cm CSF. 80/111 (72%) met the modified Dandy criteria for diagnosis of idiopathic intracranial hypertension. Six (5.4%) patients had CSF pressures under 25 cm CSF due to CSF leak, five (4.5%) did not have LP performed due to spinal malformations, nine (8.1%) declined and the remaining are awaiting LP, majority delayed secondary to the COVID-19 pandemic. All patients had neuroimaging to exclude secondary causes of raised ICP.
All 121 newly diagnosed IIH patients seen during the study period were referred for OSA screening with pulse oximetry. 111/121 (91.7%) were included; ten patients were excluded for the following reasons: one was already on CPAP and nine had overnight pulse oximetry results that were unavailable or incomplete for analysis.
All patients had papilloedema at time of diagnosis, which resolved with medical treatment or weight loss in 24.6% at the time of pulse oximetry, due to waiting times for the test. The mean average RNFL thickness on OCT taken prior to overnight pulse oximetry study was 132.7 ± SD 48.9 µm. Six patients had optic atrophy secondary to previous papilloedema and were excluded from statistical analyses where RNFL was used as a marker of severity of disease. The mean RNFL thickness for those who were excluded was 69.8 µm ± SD 12.9 µm. These six patients with optic atrophy had a long history of symptoms prior to their diagnosis at the MEU.
Thirty (27%) patients had anaemia or a history of anaemia. This was attributed to iron deficiency alone in 21/30 (70%), mixed iron and vitamin B12 deficiencies in 4/30 (13%), normocytic anaemia in 4/30 (13%) and sickle cell disease in one patient.
The Epworth Sleepiness Scale (ESS) was obtained for 67 patients (60%). Twenty (30%) reported a degree of excessive daytime sleepiness with ESS scores above ten. ESS ranged from 0 to 20 of 24 (mean 5 ± SD 7). Neck sizes were measured for 38 patients (34%), which ranged from 30.4 to 48.2 cm (mean 37.9 ± SD 3.9 cm). A summary of the patient demographics and clinical data are shown in Table 1.
Overnight pulse oximetry results
Mean 3% ODI obtained from overnight pulse oximetry ranged from 0.48 to 80.2 events/hour (mean ± SD, 9.4 ± 13.1 events/hour). Fifty-four patients (48.6%) had OSA; 37 (33.3%) had mild OSA, 11 (9.9%) had moderate OSA and six (5.4%) had severe OSA. Mean average peripheral oxygen saturation (SpO2) was 96.1% ± SD 2.5% and mean minimum SpO2 was 81.3% ± SD 8.8%. Fifty-two patients (46.8%) had an element of presumed REM related OSA and 38 patients (34.2%) had increased nocturnal pulse rate variability (PRV).
Using Spearman’s Rank-Order Correlation test, we found an association between 3% ODI and age (r = 0.31 [95% CI: 0.13–0.48], p = 0.0008), BMI (r = 0.47 [95% CI: 0.29–0.61], p < 0.0001), vitamin B12 (r = 0.32 [95% CI: 0.050–0.55], p = 0.0183) and ESS (r = 0.24 [95% CI: 0.022–0.44], p = 0.0269). The correlation data for 3% ODI against patient demographics and clinical data have been summarised in Table 2.
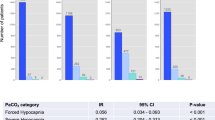
When comparing between non OSA, mild OSA and moderate to severe OSA groups, age, BMI and Vitamin B12 differed across groups, with a trend towards higher values in the moderate to severe group (Kruskal-Wallis p = 0.0204, <0.0001 and 0.0332 respectively). Dunn’s post hoc test for BMI showed significant difference between all three groups, whilst for age and vitamin B12, the difference was only significant between the non OSA and moderate to severe OSA group. This has been detailed in Fig. 1. Differences in lumbar puncture opening pressure and RNFL thickness on OCT were not statistically significant. Comparisons between the three groups are summarised in Table 3.
Effects of CPAP and OSA treatment
Current NICE guidance recommends CPAP as a treatment option for moderate or severe symptomatic OSA, and positioning of sleep or mandibular advancement device (MAD) for mild OSA [15]. In our cohort, 11/17 with moderate-to-severe OSA were treated with CPAP. Of the remaining six, two were offered CPAP and are awaiting commencement of treatment; four were referred for MAD on the basis that their 3% ODI was bordering on mild OSA.
For the eleven patients (five with moderate OSA; six with severe OSA) who went on to have CPAP therapy, adherence was mixed. CPAP was well tolerated in three patients, all describing improvement in symptoms of IIH and OSA. Two of three patients reported significantly lower ESS scores at annual follow-up. Weight loss of 4.7%, 11% and 10.2% respectively was observed. Papilloedema on fundus examination was noted to have improved for two of the three patients, one in conjunction with medical management.
Tolerability was poor in five patients, with two stopping CPAP therapy at two and six months. Where adherence was poor, symptoms were generally reported as unchanged or worsened. Three patients had weight gain ranging from 0.4% to 5.2%. Despite this, papilloedema improved for three of five patients with concurrent acetazolamide or topiramate.
A summary of the outcomes of CPAP therapy is illustrated in Table 4.
Discussion
This service evaluation highlights the high prevalence of OSA in a cohort of IIH patients and the importance of OSA as a common co-morbidity.
The implications of untreated OSA have been well established beyond poor sleep quality. Untreated OSA has been shown to increase cardiovascular risk and is independently associated with a large increased risk of all-cause mortality [16,17,18].
In our cohort of IIH patients, the yield of overnight pulse oximetry as a screening tool was 48.6% for OSA and 15.3% for moderate to severe OSA. We found that age, BMI, vitamin B12 and higher ESS correlated with more severe OSA. There is a trend of higher RNFL thickness in in the moderate to severe OSA group, but this did not reach statistical significance.
Eleven (10%) patients had CPAP therapy. Those who adhered to CPAP therapy, in conjunction with weight loss or medical therapy found improvements in both OSA and IIH symptoms, including resolution of papilloedema in some cases. This highlights a potential role for screening and treating OSA in this population.
To our knowledge, this is the largest study reporting the prevalence of OSA using overnight pulse oximetry as a screening tool in newly diagnosed IIH patients, as well as reporting the effects of CPAP therapy in conjunction with weight loss and medical therapies on the clinical course of IIH.
Other studies showed similar prevalence of OSA in IIH patients. Thurtell and colleagues [19] reported OSA in 18/30 (60%) and again in a case control study [11] 8/24 (33.3%) with no statistical difference to matched controls. Previous case series relying on medical history without systematic screening of OSA in IIH reported prevalence ranging from 0.7–33%. [12, 13, 20,21,22] This large range may indicate potential missed opportunities for the diagnosis and treatment of OSA without systematic screening.
In this study, 20/67 (30%) had a significant ESS score. Previous studies have utilised other OSA questionnaires including STOP-BANG and Berlin Questionnaire (BQ). Fraser and colleagues reported that men with IIH were significantly more likely to have a positive BQ compared to matched controls after adjustments for BMI. Thurtell also reported a BQ score indicating high risk of OSA in 20/30 (67.8%) of IIH patients [10]. In our study, only a proportion of patients had data available for ESS and neck circumference and therefore could not be compared with the yield of oximetry screening. The conclusions in this regard are limited and warrants further assessment in future studies.
We found a positive correlation between 3% ODI and active vitamin B12 levels. Although the pathophysiological link between vitamin B12 and OSA is unknown, it has previously been reported in mice [23]. Veasey et al. found low levels of plasma methylmalonic acid (MMA) in mice exposed to long-term intermittent hypoxia, a marker for vitamin B12 activity. It was speculated that low plasma MMA or high vitamin B12 activity may be indicative of myelin injury secondary to hypoxia.
This study lacked matched controls. It is possible that the high rates of OSA may be confounded by high BMI. Several cross-sectional studies have consistently found an association between increased BMI and risk of OSA [24, 25]. A previous study showed that up to 40% of obese men and 3% of obese women had significant OSA warranting intervention [26]. OSA has also been reported to cause raised ICP [27]. A case control study with systematic screening of OSA using home oximetry testing would therefore be important to shed further light on the significance of OSA in the pathophysiology of raised ICP in patients with IIH.
This study did not systematically screen for non-OSA sleep disturbances, which may be important to consider with regards to assessing the quality of sleep in patients with IIH. This is important to consider as sleep disturbances has been reported as a risk factor weight gain [28, 29].
In line with the exploratory nature of this study, type-1 statistical error from multiple comparisons should be considered and p-values should be interpreted as descriptive correlations rather than confirmatory claims.
In summary, we report the largest series of consecutive IIH patients screened for OSA using home pulse oximetry. This study highlights the importance of OSA as a common co-morbidity in the IIH patient cohort. Given the well-known implications of undiagnosed and untreated OSA in particular towards increased cardiovascular risk and all-cause mortality, there is a potential role of screening and treating OSA in this population. Further studies on the potential contribution of OSA as a cause of raised ICP in the IIH cohort as well as the effects of OSA treatment on IIH symptoms is warranted.
Summary
What was known before
-
OSA has been speculated to be involved in the pathophysiology of IIH.
-
The prevalence of OSA in IIH patients has previously been reported to be between 4–60% in small case control studies and case series with non systematic screening.
What this study adds
-
This study is the largest series of consecutive IIH patients screened for OSA using home pulse oximetry.
-
The high rates of OSA reported in our study highlights a potential role for the recognition and management of OSA in the IIH patient cohort.
References
Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 2013;81:1159–65.
Rowe FJ, Sarkies NJ. The relationship between obesity and idiopathic intracranial hypertension. Int J Obes. 1999;23:54–9.
Radhakrishnan K, Thacker AK, Bohlaga NH, Maloo JC, Gerryo SE. Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. J Neurological Sci. 1993;116:18–28.
Chen J, Wall M. Epidemiology and risk factors for idiopathic intracranial hypertension. Int. Ophthalmol. Clin. 2014;54:1–11.
Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR, et al. Idiopathic intracranial hypertension: Consensus guidelines on management. J Neurol Neurosurg Psychiatry. 2018;89:1088–100.
Pillar G, Malhotra A, Fogel R, Beauregard J, Schnall R, White DP. Airway mechanics and ventilation in response to resistive loading during sleep: Influence of gender. Am J Respiratory Crit Care Med. 2000;162:1627–32.
Young T. Menopause, hormone replacement therapy, and sleep-disordered breathing: Are we ready for the heat? Am J Respiratory Crit Care Med. 2001;163:597–8.
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respiratory Crit Care Med. 1998;157:144–8.
Davies RJ, Ali NJ, Stradling JR. Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax 1992;47:101–5.
Thurtell MJ, Bruce BB, Rye DB, Newman NJ, Biousse V. The Berlin questionnaire screens for obstructive sleep apnea in idiopathic intracranial hypertension. J Neuro-Ophthalmol. 2011;31:316–9.
Thurtell MJ, Trotti LM, Bixler EO, Rye DB, Bliwise DL, Newman NJ, et al. Obstructive sleep apnea in idiopathic intracranial hypertension: comparison with matched population data. J Neurol. 2013;260:1748–51.
Lee AG, Golnik K, Kardon R, Wall M, Eggenberger E, Yedavally S. Sleep apnea and intracranial hypertension in men. Ophthalmology 2002;109:482–5.
Bruce BB, Kedar S, Van Stavern GP, Monaghan D, Acierno MD, Braswell RA, et al. Idiopathic intracranial hypertension in men. Neurology 2009;72:304–9.
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiological Rev. 2010;90:797–8.
NICE guidelines: Continuous positive airway pressure for the treatment of obstructive sleep apnoea/hypopnoea syndrome. 2008. https://www.nice.org.uk/guidance/ta139/chapter/1-Guidance.
Knauert M, Naik S, Gillespie MB, Kryger M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol-Head Neck Surg. 2015;1:17–27.
Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. Jama 2012;307:2169–76.
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: The Busselton health study. Sleep 2008;31:1079–85.
Fraser JA, Bruce BB, Rucker J, Fraser LA, Atkins EJ, Newman NJ, et al. Risk factors for idiopathic intracranial hypertension in men: A case–control study. J Neurological Sci. 2010;290:86–9.
Szewka AJ, Bruce BB, Newman NJ, Biousse V. Idiopathic intracranial hypertension: Relation between obesity and visual outcomes. J Neuro-Ophthalmol: Off J North Am Neuro-Ophthalmol Soc. 2013;33:4.
Ardissino M, Moussa O, Tang A, Muttoni E, Ziprin P, Purkayastha S. Idiopathic intracranial hypertension in the British population with obesity. Acta Neurochirurgica. 2019;161:239–46.
Radojicic A, Vukovic-Cvetkovic V, Pekmezovic T, Trajkovic G, Zidverc-Trajkovic J, Jensen RH. Predictive role of presenting symptoms and clinical findings in idiopathic intracranial hypertension. J Neurological Sci. 2019;399:89–93.
Veasey SC, Lear J, Zhu Y, Grinspan JB, Hare DJ, Wang S, et al. Long-term intermittent hypoxia elevates cobalt levels in the brain and injures white matter in adult mice. Sleep 2013;36:1471–81.
Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: A population health perspective. Am J Respiratory Crit Care Med. 2002;165:1217–39.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl J Med. 1993;328:1230–5.
Vgontzas AN, Tan TL, Bixler EO, Martin LF, Shubert D, Kales A. Sleep apnea and sleep disruption in obese patients. Arch Intern Med. 1994;154:1705–11.
Jennum P, Børgesen SE. Intracranial pressure and obstructive sleep apnea. Chest 1989;95:279–83.
Theorell-Haglöw J, Berne C, Janson C, Sahlin C, Lindberg E. Associations between short sleep duration and central obesity in women. Sleep 2010;33:593.
Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36.
Author information
Authors and Affiliations
Contributions
Study conception: LTK, SW, VG, GL. Data collection: LTK, VG. Statistical analysis: LTK. All authors contributed to the critical review and final approval of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare that there are no conflicts of interest. The following authors have nothing to disclose: LTK, VG, RM, AN, GL. SHW has the following financial declarations which do not conflict with the work done for this paper: Research funding from Myaware, Eye Hope, Guys & St Thomas’ Charity, Visual Snow Initiative; honorarium for educational content (Neurodiem; Chiesi) and safety study (REN001); subsidy for Group Consultations Ltd training from Sir Jules Thorn Charitable Trust.
Ethics approval
As this study was deemed to be a service evaluation by the Guy’s and St Thomas’ Research and Development department and with the HRA decision tool, there was no requirement for ethical review. This study received institutional approval as a service improvement project (ID No: 9139).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kok, L.T., Gnoni, V., Muza, R. et al. Prevalence and utility of overnight pulse oximetry as a screening tool for obstructive sleep apnoea in newly diagnosed idiopathic intracranial hypertension. Eye 37, 537–542 (2023). https://doi.org/10.1038/s41433-022-01971-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-01971-1
- Springer Nature Limited
This article is cited by
-
Idiopathic intracranial hypertension: a step change in understanding the disease mechanisms
Nature Reviews Neurology (2023)
-
Topiramate
Reactions Weekly (2023)