Abstract
Objectives
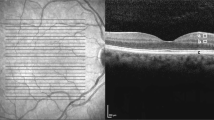
To comprehensively assess diabetic retinopathy neurodegeneration (DRN) as quantified by retinal neuronal and axonal layers measured with spectral-domain optical coherence tomography (SD-OCT) in subjects with diabetes mellitus (DM).
Methods
Articles on the topic of examining macular ganglion cell-inner plexiform layer (m-GCIPL), macular retinal nerve fibre layer (m-RNFL), macular ganglion cell complex (m-GCC), and peripapillary RNFL (p-RNFL) measured with SD-OCT in DM subjects without DR (NDR) or with non-proliferative DR (NPDR) were searched in PubMed and Embase up to November 31, 2019. Standardized mean difference (SMD) as effect size were pooled using random-effects model.
Results
Thirty-six studies searched from online databases and the CUHK DM cohort were included in the meta-analysis. In the comparison between NDR and control, macular measures including mean m-GCIPL (SMD = −0.26, p = 0.003), m-RNFL (SMD = −0.26, p = 0.046), and m-GCC (SMD = −0.28; p = 0.009) were significantly thinner in the NDR group. In the comparison between NPDR and NDR, only mean p-RNFL was significantly thinner in the NPDR group (SMD = −0.27; p = 0.03), but not other macular measures.
Conclusions
Thinning of retinal neuronal and axonal layers at macula as measured by SD-OCT are presented in eyes with NDR, supporting DRN may be the early pathogenesis in the DM patients without the presence of clinical signs of DR. In the future, these SD-OCT measures may be used as surrogates of DRN to stratify DM patients with a high risk of DR, and may be used as a therapeutic target if neuroprotection treatment for DR is available.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR), a common complication of diabetes mellitus (DM), remains the leading cause of blindness in working-age adults [1, 2]. Currently, available treatments, for example laser photocoagulation and anti-vascular endothelial growth factor (anti-VEGF) injection, are only targeting advanced stages of DR in which vision is threatened or has already been significantly affected. It is now increasingly evident that diabetic retinal neurodegeneration (DRN) plays a prominent role in the pathogenesis of DR [3,4,5,6]. For example, reactive gliosis, diminished retinal neuronal function, and neural cell apoptosis have been observed in both diabetic mouse models and eyes of diabetic donors [5, 7, 8]. Cross-sectional clinical studies also showed thinning of retinal neuronal and axonal layers as assessed by optical coherence tomography (OCT) in preclinical DR [9,10,11,12,13,14,15,16,17,18,19,20], and a recent longitudinal study has further demonstrated the progressive thinning of macular ganglion cell-inner plexiform layer (m-GCIPL) is associated with DR progression [21]. These studies have provided a better understanding of DR pathogenesis and may lead to the development of novel and more effective preventive treatment for early stages of DR [1, 3, 22,23,24,25].
However, the conclusions from current clinical studies are still not entirely consistent, with a few individual studies failing to find significant associations between the thicknesses of retinal layers and DR, and others reaching different conclusions based on different retinal layers assessment [11, 12, 17,18,19, 26, 27]. Only one meta-analysis has been performed thus far but with several limitations [28]. First, it has included studies with both time-domain OCT (TD-OCT) and spectral-domain OCT (SD-OCT), while the results of the two measuring methods are not interchangeable [28]. Second, the meta-analysis only included measurements of peripapillary retinal nerve fibre layer (p-RNFL), ignoring the retinal neuronal and axonal layers at macula (e.g. m-GCIPL, macular retinal nerve fibre layer (m-RNFL), macular ganglion cell complex (m-GCC)), which includes 50% of the retinal ganglion cells and were shown to become thinning in the clinical studies.
In this study, we conducted a systematic review and meta-analysis to comprehensively assess DRN as quantified by m-GCIPL, m-RNFL, m-GCC, and p-RNFL measured with SD-OCT in subjects with DM. We hypothesized that the thinning of SD-OCT measurements as surrogates of DRN could be observed in the preclinical or early stages of DR.
Materials and methods
Data sources and searches and study selection
Following the Meta-analysis of Observational Studies in Epidemiology (MOOSE) [29], we conducted a systematic review and meta-analysis to identify publications on evaluating m-GCIPL, m-RNFL, m-GCC, and p-RNFL measured by SD-OCT in subjects with DM without the DR (NDR) or non-proliferative DR (NPDR). Two investigators independently searched the potential records in PubMed and Embase up to November 31, 2019. The search was supplemented by manual bibliography searches of eligible studies. All potential records from electronic databases were merged in Zotero version 5.0.80 to go through titles and abstracts. The MOOSE checklist and search strategy are available in eTables 1 and 2.
All selected studies satisfied the following criteria: (1) studies with case-control, cross-sectional, or prospective design; (2) retinal neuronal and axonal layers measured with SD-OCT or Fourier-domain OCT measurements; (3) DR status was classified into no DR (NDR) and/or non-proliferative DR (NPDR); (4) only one eye of each subject selected for analysis in manuscript; (5) SD-OCT measurements reported as mean with standard deviation (SD), mean with 95% confidence interval (95% CI) or median with interquartile range (IQR); and (6) an English-language article with full text accessible published on or before November 31, 2019 in peer-reviewed journals. We excluded non-English records, conference abstracts, and case reports. All qualified studies were applied Newcastle-Ottawa Quality Assessment Form to examine the study quality [30]. In the whole search and selection process, any discrepancies were solved by further discussion with a senior reviewer (CYC).
Data collection
All retrieved records included: (1) study information: title of each study, authors’ name, publication year, type of OCT machine; (2) demographic information: type of DM, groups of DR status, numbers of eye, mean age of each group, DM duration, and HbA1c; and (3) SD-OCT measurements: the values of mean thicknesses and each sectoral thicknesses, if any. We also recorded the exclusion criteria of each study to ensure the potential confounders of SD-OCT measures were excluded. Eyes with diabetic macular oedema (DMO), previous related treatment (e.g. previous laser treatment, anti-VEGF, or vitrectomy) or other macular diseases were excluded. When any further information was demanded, the authors were contacted.
The CUHK DM cohort
We also included data from a DM cohort and healthy controls recruited from the CUHK Eye Centre, Hong Kong, in the current meta-analysis named as “CUHK 2019”. Data extraction followed the same classification described in the “Data Collection” above, among that, the thicknesses of m-GCIPL and p-RNFL were included in the current meta-analysis. The details of the study methodology were reported elsewhere [31, 32]. In brief, dilated biomicroscopic fundus examination was performed for assessing DR severity and DMO by retinal specialists, according to the International Clinical Diabetic Retinopathy and Diabetic Macular Oedema Disease Severity Scales [33]. Exclusion criteria for study eyes included: (1) DMO; (2) undergone related treatment; (3) eye pathology that interferes with image quality or retinal segmentation (e.g. dense cataract, and epiretinal membrane); (4) glaucoma; and (5) presence of other maculopathies not related to diabetes. Controls were defined as those without DM, and without any ocular abnormalities from the ocular examinations. M-GCIPL and p-RNFL thicknesses were obtained from all subjects with Cirrus HD-OCT (Carl Zeiss Meditec Inc., Dublin, CA, USA). Eyes with apparent failure in the automatic segmentation of the retinal layers, or with poor image quality were excluded. Right eyes from each subject were selected into analysis. Finally, for the m-GCIPL analysis, 84 eyes, 181 eyes, and 179 eyes were included for the control, NDR, and NPDR groups, respectively; whilst for the p-RNFL analysis, 86 eyes, 187 eyes, and 190 eyes were included for the control, NDR, and NPDR groups, respectively.
Data synthesis and analysis
In view of the differences in OCT model and segmentation algorithms used, standardized mean difference (SMD) were pooled using random-effects model with inverse variance method to investigate the relationship of DRN in two comparisons: (1) NDR group versus control group; (2) among subjects with DM, NPDR group versus NDR group. Heterogeneity and variability among the studies were examined by Higgins’ I2 test and Q test, respectively. To compare the strength of association among the SD-OCT measures in each group comparison, log odds ratio (Log OR) transformed from SMD, and OR was then calculated. Meta-regression analysis was performed based on mixed-effects models to examine whether age, type of DM, HbA1c, and duration of DM (explanatory variables) had any potential impact on SMD (outcome variable) in each comparison.
Subgroup analysis by type of DM was performed using mixed-effects model. To guarantee the sufficient power, subgroup analysis was only conducted in comparisons with the number of studies ≥ 10, and each covariate in the meta-regression should at least contain in 10 studies [34].
Publication bias was evaluated by Egger’s test. All statistical analyses were performed using R software (version 3.5.3, R Foundation for Statistical Computing) in the packages of “meta” and “metafor”. A p < 0.05 indicated statistically significant.
Results
Figure 1 summarized the selection process for 37 studies identified in the meta-analysis. Of 3534 records from PubMed and Embase screened the titles and abstracts for the eligibility, 74 records were potentially relevant to the topic of evaluating DRN in subjects with DM, which were full text reviewed by applying the inclusion criteria and exclusion criteria. After the review, we excluded studies that failed to meet our criteria: one study combined NPDR and PDR as one group; one study measured p-RNFL in a band of 2.4 mm thickness; one study reported SD-OCT measurement not including GCIPL, RNFL, or GCC; three studies were full-text unavailable; four studies were conference abstracts; four studies were uncategorized DR status; five studies were formats of results that could not be transformed for analysis; five studies used Stratus OCT; six studies included both eyes from each subject; seven studies did not report the exact mean values in the manuscript (i.e. only exhibited in figures). Since there was only one reported longitudinal study [35] that satisfied our criteria, we could not perform any meta-analysis and thus excluded it. The remaining 36 studies and the “CUHK 2019” cohort with a total of 6220 subjects were finally identified in the meta-analysis. No additional trials were established from a bibliography search of included studies. All identified studies were tested by Newcastle-Ottawa Quality Assessment Form, and had good or fair quality. eTable 3 exhibited the characteristics of the 37 eligible studies [9,10,11,12,13,14,15,16,17,18,19,20, 26, 36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. Publication bias was only observed in the SMD of mean p-RNFL between NPDR and NDR (p = 0.03).
Table 1 shows the SMDs of m-GCIPL, m-RNFL, m-GCC, and p-RNFL measurements for two comparisons in the meta-analysis: (1) NDR group versus control group; and (2) among subjects with DM, NPDR group versus NDR group.
m-GCIPL thickness
NDR eyes had significant thinning in the mean m-GCIPL thickness compared with control eyes among sixteen cohorts [9,10,11, 16,17,18,19, 36,37,38,39,40,41]. (SMD = −0.26; 95%CI = [−0.42, −0.11]; p = 0.003). In the sectoral analysis involving nine cohorts [9,10,11, 15,16,17,18,19], except for superotemporal quadrant, NDR eyes had significant thinning in all the remaining quadrants (all p < 0.05) (eFig. 1A). However, no significant differences were observed in the NPDR group compared with NDR group in both mean and sectoral m-GCIPL thicknesses (all p > 0.05) (eFig. 1B) [9, 10, 36,37,38,39, 41].
m-RNFL thickness
NDR eyes had significant thinning in mean m-RNFL compared with control among nine cohorts [9, 13, 37, 38, 40,41,42,43] (SMD = −0.26; 95%CI = [−0.51, −0.01]; p = 0.046) (eFig. 2A). No significant differences were observed in the comparison between NPDR and NDR among 8 studies (eFig. 2B) [9, 13, 37, 38, 41,42,43,44].
m-GCC thickness
NDR eyes showed significant thinner mean m-GCC than control group among 11 cohorts [12, 15, 20, 26, 40, 45,46,47,48] (SMD = −0.28; 95%CI = [−0.48, −0.09]; p = 0.009) (eFig. 3A). No significant differences were observed in the comparison between NPDR and NDR in mean m-GCC among five cohorts (eFig. 3B) [12, 26, 45, 46].
p-RNFL thickness
No significant differences were observed between NDR eyes and control eyes in the mean p-RNFL thickness among 26 cohorts [10,11,12, 14, 15, 17,18,19,20, 26, 36, 39, 41, 45,46,47,48,49, 51, 53,54,55,56, 58], as well as all sectors (all p > 0.05) (eFig. 4A). NPDR eyes had significant thinning in mean p-RNFL compared with NDR eyes among 16 cohorts [10, 12, 26, 36, 39, 42, 45, 46, 49,50,51,52,53] (SMD = −0.27; 95%CI = [−0.51, −0.03]; p = 0.03). In the sectoral analysis, similar finding was observed in the inferior quadrant among nine cohorts [10, 36, 42, 49, 51,52,53] (SMD = −0.35; 95%CI = [−0.64, −0.06]; p = 0.025), but not in other quadrants (eFig. 4B).
Strength of associations of SD-OCT measurement
We further compared the strength of associations of SD-OCT measurement in the two group comparisons as shown in Table 2. In the comparison between NDR and control, m-GCIPL (OR: 1.54, 95%CI = [1.21, 1.97]) showed stronger association, than that of m-RNFL (OR: 1.52, 95%CI = [1.06, 2.20]) and p-RNFL (OR: 1.21, 95%CI = [1.06, 2.20]). In the comparison between NPDR and NDR, p-RNFL showed stronger association (OR: 1.57, 95%CI = [1.09, 2.25]), than that of m-RNFL (OR: 1.38, 95%CI = [1.0, 1.89]) and m-GCIPL (OR: 1.21, 95%CI = [0.99, 1.62]).
Meta-regression
We did not observe any significant impact on SMD in m-GCIPL and p-RNFL from age, type of DM, HbA1c, and duration of DM in the group comparisons (eTable 4). The remaining SD-OCT measures with each covariate less than 10 cohorts didn’t have sufficient power to perform the meta-regression.
Subgroup analysis by type of DM
We did not observe any significant differences between type 1 DM (T1DM) and type 2 DM (T2DM) in mean GCIPL (p = 0.12), mean m-GCC (p = 0.89), and mean p-RNFL (p = 0.12) in NDR versus control, and in mean p-RNFL (p = 0.46) between NPDR and NDR (eTable 5). Other SD-OCT measures with less than 10 cohorts did not have sufficient power to perform the subgroup analysis.
Discussion
In this systematic review and meta-analysis, we demonstrated that there was significant thinning of retinal neuronal and axonal layers at macula in NDR eyes compared with control eyes, supporting the concept that such SD-OCT measures at macula, as surrogate markers for DRN, may indicate early pathogenesis of DR even before the presence of any microvascular abnormalities detected clinically.
Our meta-analysis firstly showed that m-GCIPL, m-RNFL, and m-GCC as measured by SD-OCT were thinner in NDR eyes than in control eyes. The accumulating evidences revealed that neuroretinal alterations begin sooner than the development of DR [7, 54, 55], and thus pathophysiology related to neurodegeneration in diabetic retina has been specifically emphasized in recent years [4, 25, 56, 57]. The structural consequence of DRN is evidenced by the thinning of retinal neuronal and axonal layers caused by neural apoptosis and reactive gliosis [5, 10, 44, 58]. Currently, numerous cross-sectional studies reported that the reduction in m-GCIPL thickness as measured by SD-OCT reflected structural neuroretinal alterations, in particular, some of the changes occurred in DM patients even without clinical signs of DR [9, 10, 15, 16, 20, 46]. Not only the reported cross-sectional studies, a longitudinal study also well documented that a progressive shrink of m-GCIPL and m-RNFL in DM without DR as well as retinal neuronal and axonal thinning in donors’ eyes without DR and diabetic mouse model [5]. Taken together, these findings and our data supported that DRN may be the early pathogenesis in DM individuals even before the appearance of any microvascular abnormalities detected clinically.
In addition, we observed that the association of NDR with thinner m-GCIPL was stronger than that of p-RNFL, suggesting that RGCs changes in the macular region are likely to be more susceptible and sensitive to neurodegenerative processes than p-RNFL axonal reduction in NDR eyes. One longitudinal study further demonstrated the progressive thinning of m-GCIPL thickness can contribute to the prediction of DR progression [21]. Since the macular region contains more than 50% of total RGCs and as the RGC cell body size is 10 to 20 times the diameter of their axons, RGCs at macular area may be more vulnerable to suffer an alteration than RGC axons at peripapillary region in face of neurodegenerative processes [59, 60]. Therefore, m-GCIPL thinning may be a better marker for tracking DRN in parallel with its potential predictive value on DR progression. In regard to p-RNFL, we did not detect any significant thinning in p-RNFL between NDR eyes and control eyes, inconsistent with a previous meta-analysis. [28]. Indeed, the studies included in the previous meta-analysis were comprised both SD-OCT and TD-OCT p-RNFL measures which were incomparable and interchangeable due to different image resolutions [61,62,63,64].
Compared with NDR, we noticed a significant reduction in p-RNFL in NPDR eyes. Lim et al recently examined the mean p-RNFL loss was −0.92 µm/y in the NDR group and −1.16 µm/y in the NPDR group which was 2.9-fold and 3.3-fold greater than that of the control group, respectively, evincing that the thinning of p-RNFL caused by neurodegeneration in the stage of NPDR may be more progressive than in NDR [35]. It is plausible that DRN may initially occur in RGC dendrites and cell bodies at macula (i.e., ganglion cell layer and inner-plexiform layer) in NDR eyes and then it may subsequently and mainly appear in RGC axons (i.e., p-RNFL layer) after DR is developed. Alternatively, the vascular leakage due to the disruption of the blood-retinal barrier and glial swelling within peripapillary vessels could mask the p-RNFL thinning. As a results, p-RNFL thinning may not be distinguished at very early stage of DR. It is noteworthy that the publication bias was presented in p-RNFL between NPDR and NDR, the interpretation should be cautious. Further studies are warranted to confirm.
In the subgroup analysis stratified by type of DM, we did not discern any significant differences in the associations of SD-OCT measurement in the two group comparisons between T1DM and T2DM, consonant with the earlier meta-analysis [28], suggesting that the extent of DRN may be similar in different types of DM. Previous studies have already reported that DRN is mainly caused by a cascade of metabolic processes, for instance, low-grade inflammation, immune cell activation, extracellular glutamate accumulation and an imbalance of local production of neurotrophic factors, which are indirectly triggered by hyperglycaemia regardless of resulting from T1DM or T2DM [25, 65, 66].
Our study may have several implications. First, SD-OCT measurement can be a surrogate or indicator of DRN. As SD-OCT has been piloted for screening DMO in different DR screening programs [67, 68], SD-OCT can potentially be used to screen for DRN simultaneously. Particularly, recent longitudinal studies showed that eyes with m-GCIPL thinning are at risk for DR progression [21]. Nevertheless, a threshold of retinal neuronal or axonal layer thinning for DRN should be established in the next stage. Second, the current management of earlier courses of DR relies almost exclusively on metabolic activities control. Research on experimental molecular targets and strategies for preserving neural retina is being conducted [69]. DRN measured by SD-OCT can be a therapeutic target or surrogate if neuroprotection treatment for earlier stages of DR is available. Third, the retina is composed of a neurovascular unit (NVU) [65]. A recent OCT-angiography study demonstrated that changes in retinal capillary network can be detected in NDR eyes and changes in retinal capillary network can predict DR progression and development of DMO [31]. Examining both retinal neuronal and axonal thinning as well as changes in retinal capillary network using the advanced OCT technology may facilitate the understanding of DR pathophysiology.
There are several strengths of our study. First, we only included studies using SD-OCT or Fourier-domain OCT to measure retinal neuronal and axonal thinning at both macular and peripapillary regions, eliminating studies using TD-OCT which are not comparable. Second, we performed subgroup analysis by type of DM. However, our study had some limitations. First, NDR was determined by fundus assessment only and some eyes with NDR may have detectable vascular abnormalities by fluorescein angiography or OCT-angiography which may confound our results. Second, our meta-analysis mainly focuses on SD-OCT measurements that broadly used for assessing glaucoma. Most of the reported studies did not include other retinal neuronal layers (e.g. inner nuclear layer, outer nuclear layer, and outer plexiform layer). Third, although there are three longitudinal studies to study the related field in the current literature [5, 21, 35], we cannot include it in the current meta-analysis as one used TD-OCT [5] and one divided DR groups into progression and non-progression group rather than by DR severity [21].
In conclusion, our findings showed that m-GCIPL, m-RNFL, and m-GCC thinning as measured by SD-OCT are present in eyes with NDR, supporting the concept that DRN may be the early pathogenesis in individuals with DM even before the onset of any microvascular abnormalities detected clinically. In the future, neuroretinal alterations as measured by SD-OCT may be used as surrogates of DRN to stratify DM patients at high risk for DR, and may be used as a therapeutic target or surrogate if neuroprotection treatment for earlier stages of DR is available.
Summary
What was known before
-
Diabetic retinal neurodegeneration happened in the early pathogenesis of diabetic retinopathy, but the results from the current clinical studies still not consistent.
What this study adds
-
In this meta-analysis, we found significant thinning of macular ganglion cell-inner plexiform layer, macular retinal nerve fibre layer, and macular ganglion cell complex in diabetes subjects without clinical retinopathy signs, compared with normal controls.
References
Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–36.
Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N. Engl J Med. 2012;366:1227–39.
Simó R, Hernández C, European Consortium for the Early Treatment of Diabetic R. Neurodegeneration in the diabetic eye: new insights and therapeutic perspectives. Trends Endocrinol Metab. 2014;25:23–33.
Sohn EH, van Dijk HW, Jiao C, Kok PHB, Jeong W, Demirkaya N, et al. Retinal neurodegeneration may precede microvascular changes characteristic of diabetic retinopathy in diabetes mellitus. Proc Natl Acad Sci USA. 2016;113:E2655–64.
Simo R, Hernandez C. Novel approaches for treating diabetic retinopathy based on recent pathogenic evidence. Prog Retin Eye Res. 2015;48:160–80.
Barber AJ, Lieth E, Khin SA, Antonetti DA, Buchanan AG, Gardner TW. Neural apoptosis in the retina during experimental and human diabetes. Early onset and effect of insulin. J Clin Invest. 1998;102:783–91.
Carrasco E, Hernández C, Miralles A, Huguet P, Farrés J, Simó R. Lower somatostatin expression is an early event in diabetic retinopathy and is associated with retinal neurodegeneration. Diabetes Care. 2007;30:2902–8.
Chhablani J, Sharma A, Goud A, Peguda HK, Rao HL, Begum VU, et al. Neurodegeneration in Type 2 Diabetes: Evidence From Spectral-Domain Optical Coherence Tomography. Invest Ophthalmol Vis Sci. 2015;56:6333.
Carpineto P, Toto L, Aloia R, Ciciarelli V, Borrelli E, Vitacolonna E, et al. Neuroretinal alterations in the early stages of diabetic retinopathy in patients with type 2 diabetes mellitus. Eye. 2016;30:673–9.
Lee H-J, Kang T-s, Kwak B-S, Jo Y-J, Kim J-Y. Long-term effect of panretinal photocoagulation on spectral domain optical coherence tomography measurements in diabetic retinopathy. Curr Eye Res. 2017;42:1169–73.
Srinivasan S, Dehghani C, Pritchard N, Edwards K, Russell AW, Malik RA, et al. Corneal and retinal neuronal degeneration in early stages of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2017;58:6365.
van Dijk HW, Verbraak FD, Kok PHB, Stehouwer M, Garvin MK, Sonka M, et al. Early Neurodegeneration in the Retina of Type 2 diabetic patients. Invest Ophthalmol Vis Sci. 2012;53:2715.
Sahin SB, Sahin OZ, Ayaz T, Karadag Z, Türkyılmaz K, Aktas E, et al. The relationship between retinal nerve fiber layer thickness and carotid intima media thickness in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2014;106:583–9.
Gundogan FC, Akay F, Uzun S, Yolcu U, Çağıltay E, Toyran S. Early neurodegeneration of the inner retinal layers in Type 1 diabetes mellitus. Ophthalmologica. 2015;235:125–32.
Chen Y, Li J, Yan Y, Shen X. Diabetic macular morphology changes may occur in the early stage of diabetes. BMC Ophthalmol. 2016;16:12.
Pekel E, Tufaner G, Kaya H, Kaşıkçı A, Deda G, Pekel G. Assessment of optic disc and ganglion cell layer in diabetes mellitus type 2. Medicine. 2017;96:e7556.
Pekel E, Altincik SA, Pekel G. Evaluation of optic disc, retinal nerve fiber and macular ganglion cell layers in pediatric diabetes. Int Ophthalmol. 2018;38:1955–61.
Karti O, Nalbantoglu O, Abali S, Ayhan Z, Tunc S, Kusbeci T, et al. Retinal ganglion cell loss in children with type 1 diabetes mellitus without diabetic retinopathy. Ophthalmic Surg Lasers Imaging Retin. 2017;48:473–7.
El-Fayoumi D, Badr Eldine NM, Esmael AF, Ghalwash D, Soliman HM. Retinal nerve fiber layer and ganglion cell complex thicknesses are reduced in children with type 1 diabetes with no evidence of vascular retinopathy. Invest Ophthalmol Vis Sci. 2016;57:5355.
Kim K, Kim ES, Yu S-Y. Longitudinal relationship between retinal diabetic neurodegeneration and progression of diabetic retinopathy in patients with Type 2 diabetes. Am J Ophthalmol. 2018;196:165–72.
Solomon SD, Chew E, Duh EJ, Sobrin L, Sun JK, VanderBeek BL, et al. Diabetic retinopathy: a position statement by the american diabetes association. Diabetes Care. 2017;40:412–8.
Duh EJ, Sun JK, Stitt AW. Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight. 2017;2:e93751.
Wong TY, Cheung CMG, Larsen M, Sharma S, Simó R. Diabetic retinopathy. Nat Rev Dis Prim. 2016;2:16012.
Simó R, Stitt AW, Gardner TW. Neurodegeneration in diabetic retinopathy: does it really matter? Diabetologia. 2018;61:1902–12.
Srinivasan S, Pritchard N, Sampson GP, Edwards K, Vagenas D, Russell AW, et al. Retinal thickness profile of individuals with diabetes. Ophthalmic Physiol Opt. 2016;36:158–66.
Lung JCY, Swann PG, Wong DSH, Chan HHL. Global flash multifocal electroretinogram: early detection of local functional changes and its correlations with optical coherence tomography and visual field tests in diabetic eyes. Doc Ophthalmol. 2012;125:123–35.
Chen X, Nie C, Gong Y, Zhang Y, Jin X, Wei S, et al. Peripapillary retinal nerve fiber layer changes in preclinical diabetic retinopathy: a meta-analysis. PLoS ONE. 2015;10:e0125919.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed 3 Feb 2020.
Sun Z, Tang F, Wong R, Lok J, Szeto SKH, Chan JCK, et al. OCT angiography metrics predict progression of diabetic retinopathy and development of diabetic macular edema: a prospective study. Ophthalmology. 2019;126:1675–84.
Tang FY, Ng DS, Lam A, Luk F, Wong R, Chan C, et al. Determinants of quantitative optical coherence tomography angiography metrics in patients with diabetes. Sci Rep. 2017;7:2575.
Wilkinson CP, Ferris FL 3rd, Klein RE, Lee PP, Agardh CD, Davis M, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–82.
Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 2004;23:1663–82.
Lim HB, Shin YI, Lee MW, Park GS, Kim JY. Longitudinal changes in the peripapillary retinal nerve fiber layer thickness of patients with type 2 diabetes. JAMA Ophthalmol. 2019;137:1125–32.
Carbonell M, Alonso N, Castelblanco E, Real J, Ramírez-Morros A, Simó R, et al. Assessment of inner retinal layers and choroidal thickness in type 1 diabetes mellitus: a cross-sectional study. J Clin Med. 2019;8:1412.
Chen Q, Tan F, Wu Y, Zhuang X, Wu C, Zhou Y, et al. Characteristics of retinal structural and microvascular alterations in early type 2 diabetic patients. Invest Ophthalmol Vis Sci. 2018;59:2110–8.
Li S-T, Wang X-N, Du X-H, Wu Q. Comparison of spectral-domain optical coherence tomography for intra-retinal layers thickness measurements between healthy and diabetic eyes among Chinese adults. PLoS ONE. 2017;12:e0177515.
Santos AR, Ribeiro L, Bandello F, Lattanzio R, Egan C, Frydkjaer-Olsen U, et al. Functional and structural findings of neurodegeneration in early stages of diabetic retinopathy: cross-sectional analyses of baseline data of the EUROCONDOR project. Diabetes. 2017;66:2503–10.
Vujosevic S, Muraca A, Alkabes M, Villani E, Cavarzeran F, Rossetti L, et al. Early microvascular and neural changes in patients with type 1 and type 2 diabetes mellitus without clinical signs of diabetic retinopathy. Retina. 2019;39:435–45.
Rodrigues EB, Urias MG, Penha FM, Badaró E, Novais E, Meirelles R, et al. Diabetes induces changes in neuroretina before retinal vessels: a spectral-domain optical coherence tomography study. Int J Retin Vitr. 2015;1:4.
Park HY-L, Kim IT, Park CK. Early diabetic changes in the nerve fibre layer at the macula detected by spectral domain optical coherence tomography. Br J Ophthalmol. 2011;95:1223–8.
Guha Mazumder A, Chatterjee S, Chatterjee S, Gonzalez JJ, Bag S, Ghosh S, et al. Spectropathology-corroborated multimodal quantitative imaging biomarkers for neuroretinal degeneration in diabetic retinopathy. Clin Ophthalmol. 2017;11:2073–89.
van Dijk HW, Verbraak FD, Kok PHB, Garvin MK, Sonka M, Lee K, et al. Decreased retinal ganglion cell layer thickness in patients with type 1 diabetes. Invest Ophthalmol Vis Sci. 2010;51:3660.
Li Z, Wen X, Zeng P, Liao Y, Fan S, Zhang Y, et al. Do microvascular changes occur preceding neural impairment in early-stage diabetic retinopathy? Evidence based on the optic nerve head using optical coherence tomography angiography. Acta Diabetol. 2019;56:531–9.
Pierro L, Iuliano L, Cicinelli MV, Casalino G, Bandello F. Retinal neurovascular changes appear earlier in type 2 diabetic patients. Eur J Ophthalmol. 2017;27:346–51.
Gołębiewska J, Olechowski A, Wysocka-Mincewicz M, Baszyńska-Wilk M, Groszek A, Czeszyk-Piotrowicz A, et al. Choroidal thickness and ganglion cell complex in pubescent children with type 1 diabetes without diabetic retinopathy analyzed by spectral domain optical coherence tomography. J Diabetes Res. 2018;2018:1–8.
Zeng Y, Cao D, Yu H, Yang D, Zhuang X, Hu Y, et al. Early retinal neurovascular impairment in patients with diabetes without clinically detectable retinopathy. Br J Ophthalmol. 2019;103:1747–52.
Shi R, Guo Z, Wang F, Li R, Zhao L, Lin R. Alterations in retinal nerve fiber layer thickness in early stages of diabetic retinopathy and potential risk factors. Curr Eye Res. 2018;43:244–53.
Srivastav K, Saxena S, Mahdi AA, Shukla RK, Meyer CH, Akduman L, et al. Increased serum level of homocysteine correlates with retinal nerve fiber layer thinning in diabetic retinopathy. Mol Vis. 2016;22:1352–60.
Vinuthinee-Naidu M-N, Zunaina E, Azreen-Redzal A, Nyi-Nyi N. Correlation of retinal nerve fibre layer and macular thickness with serum uric acid among type 2 diabetes mellitus. BMC Ophthalmol. 2017;17:91.
Vujosevic S, Muraca A, Gatti V, Masoero L, Brambilla M, Cannillo B, et al. Peripapillary microvascular and neural changes in diabetes mellitus: An OCT-angiography study. Invest Ophthalmol Vis Sci. 2018;59:5074–81.
Araszkiewicz A, Zozulińska‑Ziółkiewicz D, Meller M, Bernardczyk‑Meller J, Piłaciński S, Rogowicz‑Frontczak A, et al. Neurodegeneration of the retina in type 1 diabetic patients. Polish Arch Intern Med. 2012;122:464–70.
Martin PM, Roon P, Van Ells TK, Ganapathy V, Smith SB. Death of retinal neurons in streptozotocin-induced diabetic mice. Invest Ophthalmol Vis Sci. 2004;45:3330.
Abcouwer SF, Gardner TW. Diabetic retinopathy: loss of neuroretinal adaptation to the diabetic metabolic environment: Neuroretinal adaptation in diabetic retinopathy. Ann NY Acad Sci. 2014;1311:174–90.
Barber AJ. Diabetic retinopathy: recent advances towards understanding neurodegeneration and vision loss. Sci China Life Sci. 2015;58:541–9.
Sohn EH, Han IC, Abramoff MD. Diabetic retinal neurodegeneration—should we redefine retinopathy from diabetes? JAMA Ophthalmol. 2019;137:1132–3.
van Dijk HW, Kok PHB, Garvin M, Sonka M, Devries JH, Michels RPJ, et al. Selective loss of inner retinal layer thickness in type 1 diabetic patients with minimal diabetic retinopathy. Invest Ophthalmol Vis Sci. 2009;50:3404–9.
Tan O, Chopra V, Lu AT-H, Schuman JS, Ishikawa H, Wollstein G, et al. Detection of macular ganglion cell loss in glaucoma by fourier-domain optical coherence tomography. Ophthalmology. 2009;116:2305–14.e2.
Mwanza J-C, Durbin MK, Budenz DL, Sayyad FE, Chang RT, Neelakantan A, et al. Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology. 2012;119:1151–8.
Vizzeri G, Weinreb RN, Gonzalez-Garcia AO, Bowd C, Medeiros FA, Sample PA, et al. Agreement between spectral-domain and time-domain OCT for measuring RNFL thickness. Br J Ophthalmol. 2009;93:775–81.
Lange AP, Sadjadi R, Saeedi J, Lindley J, Costello F, Traboulsee AL. Time-domain and spectral-domain optical coherence tomography of retinal nerve fiber layer in ms patients and healthy controls. J Ophthalmol. 2012;2012:564627.
Leung CK-S, Cheung CY-L, Weinreb RN, Qiu Q, Liu S, Li H, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology. 2009;116:1257–63. 63.e1-2
den Haan J, Verbraak FD, Visser PJ, Bouwman FH. Retinal thickness in Alzheimer’s disease: a systematic review and meta-analysis. Alzheimers Dement (Amst). 2017;6:162–70.
Gardner TW, Davila JR. The neurovascular unit and the pathophysiologic basis of diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2017;255:1–6.
Lechner J, O’Leary OE, Stitt AW. The pathology associated with diabetic retinopathy. Vis Res. 2017;139:7–14.
Olson J, Sharp P, Goatman K, Prescott G, Scotland G, Fleming A, et al. Improving the economic value of photographic screening for optical coherence tomography-detectable macular oedema: a prospective, multicentre, UK study. Health Technol Assess. 2013;17:1–142.
Goh JKH, Cheung CY, Sim SS, Tan PC, Tan GSW, Wong TY. Retinal imaging techniques for diabetic retinopathy screening. J Diabetes Sci Technol. 2016;10:282–94.
Zafar S, Sachdeva M, Frankfort BJ, Channa R. Retinal neurodegeneration as an early manifestation of diabetic eye disease and potential neuroprotective therapies. Curr Diab Rep. 2019;19:17.
Funding
CUHK Direct Grant (Reference No. 2017.054).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2020_1020_MOESM8_ESM.pdf
eTable 4. Meta-regression analysis to examine the effect of age, type of DM, HbA1c and duration of DM on the Standardized Mean Difference in the group comparisons.
Rights and permissions
About this article
Cite this article
Tang, Z., Chan, M.Y., Leung, W.Y. et al. Assessment of retinal neurodegeneration with spectral-domain optical coherence tomography: a systematic review and meta-analysis. Eye 35, 1317–1325 (2021). https://doi.org/10.1038/s41433-020-1020-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1020-z
- Springer Nature Limited
This article is cited by
-
Early choroidal and retinal changes detected by swept-source oct in type 2 diabetes and their association with diabetic kidney disease: a longitudinal prospective study
BMC Ophthalmology (2024)
-
The cross-sectional and longitudinal relationship of diabetic retinopathy to cognitive impairment: a systematic review and meta-analysis
Eye (2023)
-
Retinal age gap as a predictive biomarker for future risk of clinically significant diabetic retinopathy
Acta Diabetologica (2023)
-
Diabetic retinal neurodegeneration as a form of diabetic retinopathy
International Ophthalmology (2021)